Abstract
Studies have shown that sFlt-1 overproduction stimulated by excess VEGF of deciduous origin in trophoblasts can cause preeclampsia. However, the mechanism underlying how VEGF regulates sFtl-1 expression in trophoblasts remains unknown. To address this issue, JEG3 and HTR-8/SV neo (HTR8) trophoblast cell lines were used to investigate the signaling pathways involved in the regulation of sFlt-1 production via VEGF overexpression in vitro. JEG3 (VEGF–GFP–JEG3, V-J) and HTR8 (VEGF–GFP–HTR8, V-H) cells overexpressing VEGF165 were established by infecting the JEG3 and HTR8 cell lines with lentivirus expressing VEGF165. Both the mRNA and protein levels of VEGF and sFlt-1 were dramatically up-regulated in the V-J and V-H cells compared to the JEG3 and HTR8 cells, and they were significantly decreased after treatment with an Flt-1 receptor inhibitor (MK-2461), a KDR receptor inhibitor (XL-184), or an Flt-1 and KDR receptor inhibitor (ABT-869). The mRNA levels of sFlt-1, Flt-1, and KDR were increased in V-H cells after treatment, and the VEGF-A mRNA levels were also elevated. The migration and invasion abilities of JEG3 and HTR8 cells were decreased after VEGF overexpression, and this reduction could be reversed with VEGF receptor inhibitor treatment. In addition, after the different treatments, the cell migration rates of V-J cells were significantly increased compared with the control treatment. Taken together, these results indicate that sFlt-1 up-regulation by VEGF may be mediated by the VEGF/Flt-1 and/or VEGF/KDR signaling pathways. However, elucidating which pathway plays this key role requires further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preeclampsia (PE) is a severe pregnancy-related complication which is a leading cause of maternal and perinatal morbidity and mortality and is mainly characterized by maternal hypertension and proteinuria after 20 weeks of gestation [1]. Although a series of PE risk factors have been identified, the underlying pathogenic mechanism of PE is not completely understood. However, PE is primarily a consequence of an imbalance between proangiogenic growth factors (such as VEGF-A) and antiangiogenic factors (such as sFlt-1) [2]. The concentration of sFlt-1 in maternal circulation is relatively low during early pregnancy and begins to rise during the middle and late periods [3]. SFlt-1 e15a has been identified as a primate-specific sFlt-1 splice variant that is abundant in the placenta [4]. SFlt-1 plays an important role in the pathogenesis of PE. Previous studies have reported that sFlt-1 expression is significantly elevated in preeclamptic placentas at 11 weeks of pregnancy and that it begins to increase 5 weeks prior to the onset of clinical PE symptoms [3]. Moreover, a placenta-specific lentivirus overexpressing sFlt-1 in rats could induce hypertension, proteinuria, and glomerular endothelial cell proliferation, which are similar to PE symptoms [5]. Additionally, a recent study showed that removing sFlt-1 from extracorporeal circulation by dialysis could improve the conditions of PE patients and prolong their pregnancies [6].
There have been many studies on the regulation of sFlt-1 expression. One recent study observed that heterogeneous nuclear ribonucleoprotein D (hnRNP D) could bind Flt-1 pre-mRNA and that hnRNP D overexpression could decrease the sFlt-1 mRNA levels in human microvascular endothelial cells (HMVECs) [7]. In addition, nitrite-derived nitric oxide (NO) has been shown to prevent hypertension during pregnancy and to concomitantly reduce the circulating plasma levels of sFlt-1 and VEGF [8], and sFlt-1 has been identified as an antagonist of VEGF and PIGF [9]. Notably, placental vascular defects and early embryonic death in VEGF-knockout or VEGF-overexpressing mice have been observed in previous studies [10, 11]. Increasing evidence has shown that VEGF expression is significantly increased in PE, and importantly, the severity of PE is associated with elevated VEGF expression [12]. Exogenous VEGF121 has been administered to experimental animals in attempts to neutralize excess sFlt-1, revealing that exogenous VEGF121 could alleviate the symptoms of PE [3].
A previous study observed that HIF-1α overexpression in pregnant mice results in elevated sFlt-1 levels and leads to a wide range of pregnancy complications [13]. Meanwhile, another study observed that human trophoblast cells administered a low dose of nicotine which could promote VEGF secretion by increasing HIF-1α-mediated VEGF transcription under hypoxic conditions [14]. Importantly, one study showed that VEGF induced a concentration-dependent release of sFlt-1 into cultured placental villous explants [15]. Previous studies in our laboratory showed that VEGF overexpression in endometrial decidual cells could directly stimulate sFlt-1 overexpression in the placenta, which may induce similar PE symptoms in pregnant mice [16]. In the present study, we hypothesized that sFlt-1 up-regulation is regulated by the VEGF-A/Flt-1 or VEGF-A/KDR signaling pathways. To confirm this hypothesis, we examined the expression levels of sFlt-1 and VEGF-A after administering VEGF-A receptor inhibitors to HTR-8/SV neo and JEG3 cells expressing exogenous VEGF165 to block the VEGF-A/Flt-1 or VEGF-A/KDR signaling pathways separately.
Materials and methods
Cell lines and culture conditions
The human choriocarcinoma cell line JEG3 (TCHu195, from Shanghai Cell Bank, China) and the trophoblast cell line HTR-8/SV neo (referred to as HTR8 herein, kindly provided by Dr. Charles H. Graham, Queen’s University, Canada) were grown in Dulbecco’s modified Eagle’s medium/nutrient mixture F12 (DMEM/F12) (HyClone, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, USA) and 1% v/v penicillin/streptomycin (10,000 units/mL penicillin and 10,000 µg/mL streptomycin, Gibco) at 37 °C with 5% CO2.
Establishing the VEGF–GFP–HTR8 and VEGF–GFP–JEG3 cell lines
Stable VEGF165 overexpression in the HTR8 and JEG3 cell lines was achieved by transduction with lentivirus encoding GFP and VEGF165 (LV–GFP–VEGF) [16]. Briefly, cells at approximately 70% confluency were transduced with 10 µL of LV–GFP–VEGF in 250 µL of DMEM/F12 in 24-well plates. After 24 h, 500 µL of fresh DMEM/F12 was added to each well, and the medium was refreshed every day. Pure VEGF–GFP–HTR8 and VEGF–GFP–JEG3 cell lines (V-H and V-J cells, respectively) were acquired by sorting GFP-positive cells after lentiviral transduction and then amplifying them for subsequent experiments.
Grouping and treatments
Cells were grown in a 25-cm2 flask until confluency. After 24 h of serum starvation, HTR8 and JEG3 cells were maintained in DMEM/F12 supplemented with 1% FBS; the control HTR8 and JEG3 cell lines were maintained in FBS-free media. V-H and V-J cells were divided into the following treatment groups and compared with JEG3 and HTR8 cells: a VEGF overexpression group (V-H or V-J) in DMEM/F12 and VEGF-overexpressing cells with an Flt-1 receptor inhibitor (10 nM MK-2461, Selleck, USA), a KDR receptor inhibitor (4 nM XL-184, Selleck), or an Flt-1 and KDR receptor inhibitor (0.035 nM ABT-869, Selleck). Doses of these inhibitors were determined in a dose-dependent experiment, and all the inhibitors were diluted in DMEM/F12. After 24 h of incubation, the cell culture supernatants were collected for enzyme-linked immunosorbent assays (ELISAs) of VEGF and sFlt-1 expression, and cells were collected to analyze VEGF and its receptors at the RNA and protein levels.
RNA extraction, cDNA synthesis, and qPCR
Total cellular RNA was isolated with RNAiso Plus (TAKARA, China), and cDNA was then synthesized from the extracted RNA using Rever Tra qPCR RT Master Mix (TOYOBO, Japan) and gDNA remover (TOYOBO, Japan). The samples were further processed for qPCR using PCR mixtures that contained 1 µL of cDNA, 1 µL of each primer, 10 µL of SYBR Premix Ex Taq II (TOYOBO, Japan), and 7 µL of DNase-free water in a final volume of 20 µL. The cycling conditions were adopted as published previously: 10 s at 95 °C followed by 45 cycles at 95 °C for 5 s, 30 s at 60 °C, and 30 s at 72 °C. The appropriate primers have been published previously (Table 1). Amplification reactions were performed on either a LightCycler 480 Instrument II (Roche Diagnostics, USA) or a CFX96 Optics Module (BIO-RAD, Singapore) and utilized SYBR Green (Qiagen, USA). The 2−ΔCT method, where CT is the cycle threshold, was used to calculate the RNA levels [17]. All the RT-PCR results were normalized to the expression of the reference gene GAPDH.
ELISA
The levels of sFlt-1 and VEGF-A in the supernatants from the abovementioned treatment groups were separately evaluated with sFlt-1 (F13478-A96T, FUDEAN Inc., China) and VEGF (BMS277/2, eBioScience, USA) ELISA kits according to the manufacturer’s instructions. The levels of VEGF-A and sFlt-1 in the supernatants are expressed in terms of pg/mL and ng/L, respectively.
Western blot
The cells were lysed using a lysis buffer containing protease inhibitor, and the total protein content was determined using a BCA kit (Thermo Fisher) after centrifugation at 4 °C and 12,000 rpm for 30 min. The extracts were boiled in loading buffer for 10 min, and then, the total protein extracts were separated via 10% SDS-PAGE and transferred onto polyvinylidene difluoride (PVDF) membranes. After blocking nonspecific binding with 5% BSA at room temperature for 2 h, the membranes were incubated overnight at 4 °C with primary antibodies against sFlt-1 (1:1000; 36-1100, Invitrogen) and GAPDH (1:4000; 2118, Cell Signaling Technology). Then, the membranes were washed with TBST and incubated with horseradish peroxidase-conjugated goat anti-rabbit secondary antibodies (1:4000; ab97051, Abcam) for 1 h at room temperature. Finally, the washed membranes were incubated with ECL solution for 5 min and detected with a Molecular Imager® Gel Doc™ XR System (Bio-Rad, USA), and the western blot images were analyzed with ImageJ software.
Wound healing assay
The wound healing assay was performed following a previously published method [18]. Briefly, cells were grown in 24-well plates until confluency. After 24 h of serum starvation, a central linear wound area was created by scraping the cell monolayers with a sterile 200-µL pipette tip. The wounded cell monolayers were then washed twice with Dulbecco’s phosphate buffered saline (DPBS, HyClone) to remove floating cells or debris and then allowed to heal for 24 h in DMEM/F12 conditioned for the different treatment groups as described above. The widths of the wound areas were monitored and photographed with an inverted microscope (OLYMPUS, Japan) at 0, 12, and 24 h. Cell migration was assessed by quantifying the width of wound closure relative to the initial wound area at 12 and 24 h.
Transwell insert invasion assay
The transwell assay was performed according to methods established in a previous study [19]. In brief, a transwell insert chamber coated with Matrigel (BD Biosciences, Israel) was used according to the manufacturer’s instructions. The cells were seeded into transwell inserts pre-coated with 1 mg/mL Matrigel (Matrigel:media = 1:7) at 1 × 105 cells per insert in serum-free DMEM/F12, and the lower chambers were loaded with DMEM/F12 supplemented with 10% FBS. The invaded cells on the bottom side of the inserts were fixed with 4% polyoxymethylene 24 h later and stained with 0.1% crystal violet. Images of the invaded cells were captured under a light microscope (OLYMPUS, Japan), and the cells were counted using ImageJ software.
Statistical analysis
Data were analyzed using GraphPad Prism 6.0 and are presented as the mean ± SEM with at least three repeats. Comparisons between groups were performed using unpaired Student’s t tests. Two-sided p values < 0.05 were considered statistically significant.
Results
VEGF–GFP–JEG3 and VEGF–GFP–HTR8 cells were established by infecting JEG3 and HTR8 cells with LV–VEGF–GFP
To establish the V-J and V-H cell lines, JEG3 and HTR8 cells were transduced with LV–VEGF–GFP. V-H and V-J cells were obtained after separately sorting for GFP-positive cells by flow cytometry (Fig. 1a, e). The VEGF-A mRNA levels were significantly higher in the V-H and V-J cell lines than in the HTR8 or JEG3 cell lines, as determined by qRT-PCR (Fig. 1b, f). Moreover, the VEGF-A protein levels were also significantly increased in the V-H and V-J supernatants (Fig. 1c, g). Interestingly, the sFlt-1 and sFlt-1 e15a mRNA levels and the sFlt-1 protein levels were also increased in these two cell lines (Fig. 1b, d, f, h).
Establishing the VEGF–GFP–JEG3 (V-J) and VEGF–GFP–HTR8 (V-H) cell lines: Image analysis of V-H cells (green: V-H) (a). Scale bar = 50 µm. QPCR analysis of VEGF-A, sFlt-1, sFlt-1 e15a, Flt-1, and KDR expression in the HTR8 cell line after transfection with LV–VEGF–GPF or in the control (b). ELISA analysis of VEGF-A (c) and sFlt-1 (d) expression in V-H cells or in the control. Image analysis of V-J cells (green: V-J) (e). Scale bar = 50 µm. QPCR analysis of the expression of VEGF-A, sFlt-1, and relative genes in the JEG3 cell line after transfection with LV–VEGF–GPF or in the control (f). ELISA analysis of VEGF-A (g) and sFlt-1 (h) expression in JEG3 cells after transfection with LV–VEGF–GPF or in the control. *p < 0.05, **p < 0.01. (Color figure online)
VEGF-A regulated sFlt-1 production through the VEGF-A/Flt-1 or/and VEGF-A/KDR pathways
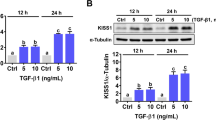
Since we identified VEGF-A as a regulator of sFlt-1, we decided to further explore the pathway through which VEGF-A regulates sFlt-1 expression. Because VEGF-A has two receptors, Flt-1 and KDR, MK-2461, XL-184, and ABT-869 were administered separately to the V-H and V-J cells. Interestingly, qRT-PCR analysis showed that the VEGF-A, sFlt-1, Flt-1, and KDR mRNA levels were significantly increased in the V-H cells after Flt-1 or/and KDR inhibition (Fig. 2a–c). However, the sFlt-1 proteins levels were dramatically decreased in the V-H supernatants (Fig. 2d) and cells (Fig. 2i, j), and the sFlt-1 mRNA levels were markedly decreased in the V-J cells after treatment with the three inhibitors (Fig. 2e–g). In addition, the ELISA (Fig. 2h) and western blot analyses (Fig. 2i, k) showed that the sFlt-1 protein levels were significantly decreased after treatment with all of the VEGF-A receptor inhibitors.
Relative gene expression after treatment with VEGF receptor inhibitors: QPCR analysis of the mRNA levels of VEGF-A, sFlt-1, sFlt-1 e15a, Flt-1, and KDR in VEGF–GPF–HTR8 (V-H) cells after a 24-h incubation with VEGF-A receptor inhibitors or in the control (a–c). V-H cells treated with MK-2461 are shown in (a). V-H cells treated with XL-184 or ABT-869, respectively (b, c). Both ELISA analysis (d) and western blot analysis (i, j) of sFlt-1 expression in V-H cells after incubation with three VEGF-A receptor inhibitors or in the control. QPCR analysis of the mRNA expression levels of VEGF-A, sFlt-1, and related genes in VEGF–GPF–JEG3 (V-J) cells after treatment (24 h) with VEGF-A receptor inhibitors or in the control (e–g). Figure (e) represents V-J cells treated with MK-2461. The XL-184 and ABT-869 treatment results are shown in (f, g). ELISA analysis (h) and western blot analysis (i, k) of sFlt-1 expression in V-J cells after treatment with three VEGF-A receptor inhibitors or in the negative control. Plus: treated; minus: untreated. *p < 0.05, **p < 0.01
The migration and invasive abilities of HTR8 and JEG3 were altered after VEGF overexpression
Previous studies have reported that sFlt-1 could inhibit the invasion of trophoblast cells [20]. Since we confirmed that VEGF-A regulates sFlt-1 production through the VEGF-A/Flt-1 or/and VEGF-A/KDR signaling pathways, we further investigated the migration and invasion abilities of HTR8 and JEG3 cells after the different treatments. Wound healing assay analysis showed that the V-H migration rate was significantly lower than that of HTR8 cells, although it partially recovered after incubation with the inhibitors (MK-2461, XL-184 and ABT-869) for 24 h (Fig. 3a, c). In addition, the changes in the invasion ability of the V-H cells followed the same pattern under the above treatment conditions (Fig. 3b, d). Moreover, we found that the migration ability of V-J cells was not altered compared to that of JEG3 cells, but it did significantly increase after treatment with the inhibitors (except ABT-869) (Fig. 4a, c). However, analysis of the invasion assay showed that the invasion ability of V-J cells was significantly lower than that of JEG3 cells. Additionally, the reduced invasive ability of V-J cells could be ameliorated after treatment with the three VEGF-A receptor inhibitors to levels even higher than those in JEG3 cells when treated with the Flt-1 and KDR inhibitors by themselves (Fig. 4b, d).
Effects on the migration and invasion abilities of VEGF–GFP–HTR8 (V-H) cells after treatment with VEGF-A receptor inhibitors: wound healing assay images (a) and the percentage of wound healing in HTR8 and V-H cells after treatment with three VEGF-A receptor inhibitors compared with that in the negative control (c). Invasion assay images (b) and quantitation of HTR8 and V-H cell migration after treatment with three VEGF-A receptor inhibitors and in the negative control (d). *p < 0.05, **p < 0.01. Scale bar = 20 µm
Effects on the migration and invasion abilities of VEGF–GFP–JEG3 (V-J) cells after treatment with VEGF-A receptor inhibitors: wound healing assay images (a) and the percentage of wound healing in JEG3 and V-J cells after treatment with three VEGF-A receptor inhibitors compared with that in the negative control (c). Invasion assay images (b) and quantitation of JEG3 and V-J cell migration after treatment with three VEGF-A receptor inhibitors and in the negative control (d). *p < 0.05, **p < 0.01. Scale bar = 20 µm
Discussion
In the present study, sFlt-1 up-regulation by VEGF-A was determined to be mediated by the VEGF/Flt-1 and/or VEGF/KDR signaling pathways in the JEG3 and HTR8 cell lines. SFlt-1 expression was dramatically increased in both V-H and V-J cells, as determined by qRT-PCR analysis and ELISA in these VEGF165-overexpressing HTR8 and JEG3 cell lines. In addition, the migration and invasion abilities of the V-H and V-J cells were dramatically lower than those of the HTR8 and JEG3 cell lines, although they could be significantly increased after treatment with VEGF-A receptor inhibitors. Our findings indicate that VEGF-A overexpression weakens the migration and invasion abilities of trophoblast cells and the remodeling of spiral arteries, at least in part by regulating sFlt-1 through the VEGF/Flt-1 and/or VEGF/KDR signaling pathways. This result has potential key implications for the design of PE therapies that involve the VEGF/Flt-1 and/or VEGF/KDR signaling pathways.
Our findings demonstrate that the migration and invasion abilities of trophoblast cells become weakened when VEGF-A expression is significantly elevated. Extravillous trophoblast (EVT) invasion is a critical process during the first trimester of human pregnancy [21]. The relationship between EVTs and spiral arteries has been reported previously [22], but the details underlying their molecular interactions remain unclear. Nevertheless, studies have shown that a failure of spiral artery remodeling could lead to the pathophysiology of PE [23]. Previous research has suggested that the expression and release of VEGF are dramatically elevated in PE placentas [24]. A recent study found that slight increases in local VEGF expression during early pregnancy could result in severe placental vascular damage [16]. Moreover, another recent study reported significantly higher VEFG serum levels in those with severe PE than in those with mild PE and in controls, and the researchers thought that VEGF might be a significant marker for predicting the severity of PE [25]. These results indicate that increased VEGF-A expression may result in inadequate spiral artery remodeling, ultimately leading to PE.
Interestingly, we also found that sFlt-1 expression was significantly increased in trophoblast cells overexpressing VEGF-A. It is widely known that sFlt-1 is involved in the pathogenesis of PE. Studies have found that hypertension, proteinuria, and renal damage, all characteristics of PE, could be easily induced in pregnant mice [26] or rats [27] by overexpressing sFlt-1 in their placentas. Another study showed bleeding placentas and embryo loss in sFlt-1 placenta-specific knockout mice, suggesting that sFlt-1 is important for maintaining placental function [9]. Abundant recent evidence has shown that VEGF can directly stimulate sFlt-1 expression. First, an in situ hybridization study of the placental basal plates of PE patients showed VEGF to be strongly expressed in decidual cells and sFlt-1 expression to be significantly increased in ETV cells [16]. Second, VEGF stimulated both vascular endothelial cells in vitro and human placenta explants releasing sFlt-1 depending on the dose of VEGF [15]. Third, expression of the Flt-1 unique variant sFlt-1-14 was increased in PE patients, and VEGF could stimulate sFlt-1-14 to increase the number of vascular smooth muscle cells [28]. Therefore, our data further validate the hypothesis that VEGF regulates sFlt-1 production in trophoblast cell lines.
The sFlt-1–VEGF balance exists in multiple organisms, and normally functioning tissues and organs within these organisms are very important. For example, sFlt-1 overexpression was shown to inhibit VEGF, which inhibited corneal blood vessel growth and thus guaranteed the maintenance of corneal transparency [29]. Although animal experiments have been conducted in which exogenous VEGF was administered to neutralize excess sFlt-1 [30], the mechanism underlying this phenomenon is unknown. VEGF-A has two cell membrane receptors, Flt-1 and KDR. In addition, a previous study reported that sFlt-1 could inhibit the invasive ability of trophoblast cells in vitro [31]. Thus, according to previous research and the data in the present study, we assume that the up-regulation of sFlt-1 via VEGF-A is mediated through the VEGF-A/Flt-1 and/or VEGF-A/KDR signaling pathways. To support our hypothesis, we administered three VEGF-A receptor inhibitors to V-H and V-J cells. Our data showed that sFlt-1 expression was significantly decreased, and the migration and invasion abilities of V-H and V-J cells were clearly rescued when VEGF-A receptors were inhibited by both inhibitors separately or in combination.
In summary, although VEGF-A is necessary for normal placental development, we have shown that elevated VEGF-A expression could up-regulate sFlt-1 production and weaken the migration and invasion abilities of trophoblast cells. Our results also showed that sFlt-1 expression was significantly decreased and that the migration and invasion abilities of V-H and V-J cells were clearly rescued by VEGF-A receptor inhibition using inhibitors individually or in combination. Therefore, we inferred that sFlt-1 up-regulation by VEGF-A may be mediated by the VEGF/Flt-1 and/or VEGF/KDR signaling pathways. However, elucidating which pathway plays this key role requires further investigation.
References
Sircar M, Thadhani R, Karumanchi SA (2015) Pathogenesis of preeclampsia. Curr Opin Nephrol Hypertens 24:131–138. https://doi.org/10.1097/MNH.0000000000000105
Leañosmiranda A, Camposgalicia I, Berumenlechuga MG, Molinapérez CJ, Garcíapaleta Y, Isordiasalas I, Ramírezvalenzuela KL (2015) Circulating angiogenic factors and the risk of preeclampsia in systemic lupus erythematosus pregnancies. J Rheumatol 42:1141. https://doi.org/10.3899/jrheum.141571
Bergmann A, Ahmad S, Cudmore M, Gruber AD, Wittschen P, Lindenmaier W, Christofori G, Gross V, Gonzalves ACDC, Gröne HJ (2010) Reduction of circulating soluble Flt-1 alleviates preeclampsia-like symptoms in a mouse model. J Cell Mol Med 14:1857–1867. https://doi.org/10.1111/j.1582-4934.2009.00820.x
Palmer KR, Kaitu’Ulino TJ, Hastie R, Hannan NJ, Ye L, Binder N, Cannon P, Tuohey L, Johns TG, Shub A (2015) Placental-specific sFLT-1 e15a protein is increased in preeclampsia, antagonizes vascular endothelial growth factor signaling, and has antiangiogenic activity. Hypertension 66:1251–1259. https://doi.org/10.1161/HYPERTENSIONAHA.115.05883
Kumasawa K, Ikawa M, Kidoya H, Hasuwa H, Saitofujita T, Morioka Y, Takakura N, Kimura T, Okabe M (2011) Pravastatin induces placental growth factor (PGF) and ameliorates preeclampsia in a mouse model. Proc Natl Acad Sci 108:1451–1455. https://doi.org/10.1073/pnas.1011293108
Thadhani R, Kisner T, Hagmann H, Bossung V, Noack S, Schaarschmidt W, Jank A, Kribs A, Cornely OA, Kreyssig C (2011) Pilot study of extracorporeal removal of soluble fms-like tyrosine kinase 1 in preeclampsia. Circulation 124:940–950. https://doi.org/10.1161/CIRCULATIONAHA.111.034793
Ikeda T, Yoshitomi Y, Saito H, Shimasaki T, Yamaya H, Kobata T, Ishigaki Y, Tomosugi N, Yoshitake Y, Yonekura H (2016) Regulation of soluble Flt-1 (VEGFR-1) production by hnRNP D and protein arginine methylation. Mol Cell Biochem 413:1–10. https://doi.org/10.1161/CIRCULATIONAHA.111.034793
Gonçalves-Rizzi VH, Possomato-Vieira JS, Sales Graça TU, Nascimento RA, Dias-Junior CA (2016) Sodium nitrite attenuates hypertension-in-pregnancy and blunts increases in soluble fms-like tyrosine kinase-1 and in vascular endothelial growth factor. Nitric Oxide Biol Chem 57:71. https://doi.org/10.1016/j.niox.2016.05.004
He Y, Smith SK, Day KA, Clark DE, Licence DR, Charnockjones DS (1999) Alternative splicing of vascular endothelial growth factor (VEGF)-R1 (FLT-1) pre-mRNA is important for the regulation of VEGF activity. Mol Endocrinol 13:537–545
Miquerol L, Langille BL, Nagy A (2000) Embryonic development is disrupted by modest increases in vascular endothelial growth factor gene expression. Development 127:3941–3946
Zhou Y, Mcmaster M, Woo K, Janatpour M, Perry J, Karpanen T, Alitalo K, Damsky C, Fisher SJ (2002) Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am J Pathol 160:1405–1423. https://doi.org/10.1016/S0002-9440(10)62567-9
Hunter A, Aitkenhead M, Caldwell C, Mccracken G, Wilson D, Mcclure N (2000) Serum levels of vascular endothelial growth factor in preeclamptic and normotensive pregnancy. Hypertension 36:965–969
Tal R, Shaish A, Barshack I, Polak-Charcon S, Afek A, Volkov A, Feldman B, Avivi C, Harats D (2010) Effects of hypoxia-inducible factor-1alpha overexpression in pregnant mice: possible implications for preeclampsia and intrauterine growth restriction. Am J Pathol 177:2950. https://doi.org/10.2353/ajpath.2010.090800
Zhao H, Wu L, Wang Y, Zhou J, Li R, Zhou J, Wang Z, Xu C (2017) Nicotine promotes vascular endothelial growth factor secretion by human trophoblast cells under hypoxic conditions and improves the proliferation and tube formation capacity of human umbilical endothelial cells. Reprod Biomed Online. https://doi.org/10.1016/j.rbmo.2016.12.014
Ahmad S, Ahmed A (2004) Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ Res 95:884–891 https://doi.org/10.1161/01.RES.0000147365.86159.f5
Fan X, Rai A, Kambham N, Sung JF, Singh N, Petitt M, Dhal S, Agrawal R, Sutton RE, Druzin ML (2014) Endometrial VEGF induces placental sFLT-1 and leads to pregnancy complications. J Clin Investig 124:4941–4952. https://doi.org/10.1172/JCI76864
Yang YL, Ren LR, Sun LF, Huang C, Xiao TX, Wang BB, Chen J, Zabel BA, Ren P, Zhang JV (2016) The role of GPR1 signaling in mice corpus luteum. J Endocrinol 230:55–65. https://doi.org/10.1530/JOE-15-0521
Wang L, Zhang D, Yu Y, Guan H, Qiao C, Shang T (2013) RNA interference-mediated silencing of laminin receptor 1 (LR1) suppresses migration and invasion and down-regulates matrix metalloproteinase (MMP)-2 and MMP-9 in trophoblast cells: implication in the pathogenesis of preeclampsia. J Mol Histol 44:661–668. https://doi.org/10.1007/s10735-013-9515-6
Li X, Wu Y, Liu A, Xin T (2016) MiR-27b is epigenetically downregulated in tamoxifen resistant breast cancer cells due to promoter methylation and regulates tamoxifen sensitivity by targeting HMGB3. Biochem Biophys Res Commun 477:768–773. https://doi.org/10.1016/j.bbrc.2016.06.133
Meekins JW, Pijnenborg R, Hanssens M, Mcfadyen IR, Asshe A (1994) A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol 101:669–674
Huppertz B (2015) Maternal-fetal interactions, predictive markers for preeclampsia, and programming. J Reprod Immunol 108:26–32. https://doi.org/10.1016/j.jri.2014.11.003
Lyall F (2005) Priming and remodelling of human placental bed spiral arteries during pregnancy—a review. Placenta 26(Suppl A):S31. https://doi.org/10.1016/j.placenta.2005.02.010
Labarrere CA, Dicarlo HL, Bammerlin E, Hardin JW, Kim YM, Chaemsaithong P, Haas DM, Kassab GS, Romero R (2017) Failure of physiologic transformation of spiral arteries, endothelial and trophoblast cell activation, and acute atherosis in the basal plate of the placenta. Am J Obstet Gynecol 216:287.e1. https://doi.org/10.1016/j.ajog.2016.12.029
Baker PN, Krasnow J, Roberts JM, Yeo KT (1995) Elevated serum levels of vascular endothelial growth factor in patients with preeclampsia. Obstet Gynecol 86:815–821. https://doi.org/10.1016/0029-7844(95)00259-T
Kurtoglu E, Avci B, Kokcu A, Celik H, Dura MC, Malatyalioglu E, Ozdemir AZ (2015) Serum VEGF and PGF may be significant markers in prediction of severity of preeclampsia. J Maternal-Fetal Neonatal Med. https://doi.org/10.3109/14767058.2015.1072157
Kumasawa K, Ikawa M, Kidoya H, Hasuwa H, Saito-Fujita T, Morioka Y, Takakura N, Kimura T, Okabe M (2011) Pravastatin induces placental growth factor (PGF) and ameliorates preeclampsia in a mouse model. Proc Natl Acad Sci USA 108:1451. https://doi.org/10.1073/pnas.1011293108
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, Libermann TA, Morgan JP, Sellke FW, Stillman IE, Maynard SE, Min JY, Merchan J et al (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt-1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Investig 111:649–658. https://doi.org/10.1172/JCI17189
Sela S, Itin A, Natanson-Yaron S, Greenfield C, Goldman-Wohl D, Yagel S, Keshet E (2008) A novel human-specific soluble vascular endothelial growth factor receptor 1 cell type-specific splicing and implications to vascular endothelial growth factor homeostasis and preeclampsia. Circ Res 102:1566. https://doi.org/10.1161/CIRCRESAHA.108.171504
Ambati BK, Nozaki M, Singh N, Takeda A, Jani PD, Suthar T, Albuquerque RJ, Richter E, Sakurai E, Newcomb MT (2006) Corneal avascularity is due to soluble VEGF receptor-1. Nature 443:993–997. https://doi.org/10.1038/nature05249
Farina A, Sekizawa A, De SP, Purwosunu Y, Okai T, Cha DH, Kang JH, Vicenzi C, Tempesta A, Wibowo N (2008) Gene expression in chorionic villous samples at 11 weeks’ gestation from women destined to develop preeclampsia. Prenat Diagn 28:956. https://doi.org/10.1002/pd.2109
Meekins JW, Pijnenborg R, Hanssens M, Mcfadyen IR, Van AA (1994) A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. BJOG Int J Obstet Gynaecol 101:669–674
Acknowledgements
This work was supported by Grants from the National Key Research and Development Program of China (2016YFC1000402), the National Natural Science Foundation (81571445), the Natural Science Foundation of Guangdong Province (2016A030313178), and the Shenzhen Basic Research Fund (JCYJ2015052109 4519488).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiao, Z., Li, S., Yu, Y. et al. VEGF-A regulates sFlt-1 production in trophoblasts through both Flt-1 and KDR receptors. Mol Cell Biochem 449, 1–8 (2018). https://doi.org/10.1007/s11010-018-3337-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-018-3337-5