Abstract
The present study evaluated the effects of asiatic acid (AA), a pentacyclic triterpenoid from Centella asiatica on lipid metabolism parameters in a rat model of obesity induced using a high fat diet (HFD) for 42 days. AA (20 mg/kg body weight [BW]) was administered orally once daily for 42 days, and an orlistat-treated group of rats (10 mg/kg BW) was included for comparison. Changes in BW, blood glucose levels, insulin resistance and leptin, adiponectin, amylase, and lipase levels in the blood; lipid profiles of plasma; liver antioxidants levels; and acetyl CoA carboxylase(ACC), uncoupling protein-2 (UCP2), and carnitine palmitoyltransferase-1 (CPT1) mRNA expression were observed in the experimental rats. Our results revealed that AA (20 mg/kg BW), similar to orlistat, reduced the increase in BW; increased bone mineral contents and bone mineral densities; reduced blood glucose levels, insulin resistance, leptin, plasma lipid levels; increased adiponectin, amylase, lipase levels in the blood; showed antioxidant activity; and altered mRNA expression of lipid metabolism-related genes, including ACC, UCP 2, and CPT 1, in the HFD-fed rats. From these results, we concluded that AA possesses significant anti-obesity potential through the suppression of BW gain, lipid lowering action, development of insulin and leptin sensitivity, antioxidant activity, and increased mRNA expression of lipid metabolism-related genes.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The obesity epidemic is widespread. The prevalence and incidence of obesity are escalating worldwide in developing and developed countries, adversely affecting both men and women of different ages [1]. Obesity increases the risk of various diseases including type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular diseases [2]. It is characterized by an anomalous or unnecessary fat accumulation attributable to an imbalance between energy intake and energy expenditure [3]. The etiology of obesity is dissimilar. However, the root cause is an energy discrepancy in which more calories are consumed than expended.
Numerous therapeutic interventions are available for the treatment of obesity, including low calorie diets, increased physical activity, behavioral treatments, pharmacological interventions, and bariatric surgery. However, these interventions generally have limited efficacy and safety [4]. Pharmacotherapy for obesity treatment has advanced remarkably in recent times. Along with lifestyle modifications, a reduction in supplement assimilation, and identification of groups of drugs that influence lipid assembly and utilization will be suitable for developing treatments for obesity. The drugs that are presently permitted for obesity by the US Food and Drug Administration (FDA) include orlistat, diethylpropion, and phendimetrazine, of which only orlistat is accepted for long-term use [5]. Currently, the market for anti-obesity drugs is growing rapidly, but the available drugs cannot meet the market demand. Hence, identifying novel anti-obesity drugs to alleviate obesity is necessary [6]. Epidemiological studies have recommended the use of phytoconstituents that can reduce the risk of diabetes, cardiovascular diseases, and obesity [7], thus suggesting that the consumption of asiatic acid may be beneficial for the treatment of metabolic diseases.
Asiatic acid (AA) is a triterpene found abundantly in Centella asiatica (L.), a perennial herbaceous creeper of the Apiaceae family [8]. It possesses an extensive array of biological functions including antioxidant, hepatoprotective, and anti-inflammatory activities [9]. Furthermore, AA exhibits antidiabetic properties by enhancing plasma levels of insulin, reducing blood glucose levels, and adjusting the status of the lipid-metabolizing enzymes [10]. It is also reported to prevent lipid peroxidation and improves the antioxidant status in rats with streptozotocin-induced diabetes [11]. However, no information pertaining to the anti-obesity effects of AA is available. Therefore, the purpose of the present study is to appraise the anti-obesity potential of AA in HFD-fed rat model.
Materials and methods
Chemicals
AA (2α, 3β, 23-trihydroxyurs-12-en-28-oic acid; Fig. 1) and orlistat (04139 Sigma) were purchased from Sigma-Aldrich (St. Louis, Missouri, USA). Fasting blood glucose kits and insulin kits were procured from Stanbio Laboratory USA, Bio-Merieux, RCS, Lyon, France. All the reagents used in the experiments were analytical grade reagents of the highest purity.
Animals
Male Sprague–Dawley rats were obtained from Department of Biochemistry, Muthyammal College of Arts and Science, Rasipuram, Namakkal District, Tamilnadu, India. The experimental rats were maintained under standard laboratory conditions (temperature: 22 ± 2 °C; humidity: 40–60%) and were permitted food and water ad libitum. The rats, initially weighing 180–200 g, were divided into four groups of six each (n = 6). All procedures involving laboratory animals were in accordance with the institutional animal ethical committee of Muthyammal College of Arts and Science (Approval No: IAEC/MCAS/05/2016).
High fat diet formula
A normal diet (ND) and HFD were procured from the National Center for Laboratory Animal Sciences, National Institute of Nutrition, Hyderabad, India (Table 1). The normal control rats were fed with standard rodent chow pellet diet according to AIN-93 guidelines, whereas the other three groups of rats were fed with HFD throughout the experiment.
Experimental design
-
Group 1 ND control group (Control).
-
Group 2 HFD group (HFD control).
-
Group 3 HFD rats orally treated with AA (20 mg/kg BW) in a vehicle solution for 42 days [10].
-
Group 4 HFD rats orally treated with orlistat (10 mg/kg BW) in a vehicle solution for 42 days [12].
Measurement of body weight
The BW and the total amount of food consumption (data not shown) of each rat were measured. Toward the end of the experiment, blood was collected from overnight fasted anesthetized animals by using retro-orbital puncture method. Blood was collected in anticoagulant-coated vials and allowed to stand for 15 min at room temperature. The plasma was separated by centrifugation at 2500 rpm for 15 min. At the end of the experimental period, the rats were fasted overnight, anesthetized, and sacrificed by cervical decapitation.
Blood glucose and insulin levels and insulin resistance
Plasma glucose was estimated using standard kits (Cat No 1060-500, Stanbio laboratory, USA). The plasma level of insulin was determined using kits from Bio-Merieux, RCS, Lyon, France. The insulin resistance index was evaluated by substituting the fasting serum insulin and plasma glucose levels in the following homeostasis model assessment (HOMA) formula: HOMA = fasting serum insulin (mU/L) × fasting plasma glucose (mM)/22.5.
Oral glucose tolerance test (OGTT)
OGTT was performed toward the end of the experiment; after overnight fasting, glucose was administered orogastrically at a dose of 2.0 g/kg BW and blood samples were collected at 0, 30, 60, and 120 min, and the blood glucose levels were evaluated.
Determination of biochemical profiles
Blood samples were centrifuged at 4000 rpm/min for 10 min to separate the plasma for lipid profile analysis and stored at −20 °C until further use. Liver tissues were weighed and rinsed in ice-cold saline. A 10% tissue homogenate was prepared using 0.025 M Tris–HCl buffer, pH 7.5. After centrifugation at 2000 rpm for 10 min, the clear supernatant was used for further biochemical assays. The plasma levels of low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides (TGs), total cholesterol (TC) by enzymatic colorimetric methods using kits (Nicholas Piramal India Ltd., Mumbai, India). Plasma amylase (cat. no. 84, Labtest® Minas Gerais, Brazil) and lipase (BioClin®, Minas Gerais, Brazil) were analyzed using the commercial kits. Plasma leptin and adiponectin (Crystal Chem, Downers Grove, IL, USA) was measured by enzyme-linked immunosorbent assay (ELISA) performed in duplicate and was expressed in ng mL−1.
Liver antioxidant analysis
The liver was excised and rinsed in ice-cold normal saline and then in an ice-cold 10% KCl solution, blotted, dried, and weighed. A 10% w/v homogenate was prepared in the ice-cold KCl solution and centrifuged at 2000 rpm for 10 min at 4 °C. The supernatant thus obtained was used for the estimation of the levels of antioxidants. The level of thiobarbituric acid reactive substances (TBARS) and glutathione (GSH), the activities of superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx) in tissue were quantified using commercially available kits, purchased from Cayman Chemical Company, USA, following the manufacturer’s instructions.
RT- PCR analysis
Total RNA was isolated from the liver tissue of the rats by using a combination of proteinase K, buffer component, RNX-Plus reagent, and high temperature according to the manufacturer’s instructions. For cDNA synthesis, random hexamer (1 μL), Oligo (dT) (1 μL), and dNTP (1 μL) were used. Then, 10 μL RNA was added to each tube for 5 min at 65 °C and immediately placed at 4 °C. The other mixture, containing nuclease-free water (4.5 μL), M-MuLV 10× buffer (2 μL), and M-MuLV 200 U/μl (0.5 μL), was prepared in an Eppendorf tube, and added to the first tube. Final reaction volume was 20 μL and the next run duration was 60 min at 42 °C with the primers. The sequences of the primers were as follows: UCP 2, forward 5TAAAGCAGTTCTACACCAAGGG-3 and reverse 5′CGAAGGCAGAAGTGAAGTGG-3,CPT-1,forward 5′TAGGACAGGCAGAAAATTGC3′ and reverse 5CAGTAGGAGCCGATTCAAAA-3, ACC 1, forward F 5TCTATTCGGGGTGACTTTC3′ and reverse 5′ CTATCAGTCTGTCCAGCCC3. The housekeeping gene β-actin was used for normalization.
Western blot analysis
The liver of the rats were collected and lysed using a bead beater and centrifuged at 7000 rpm for 15 min at 4 °C. The suspension samples were collected, and 20 µL of each sample was loaded on a 6% sodium dodecyl sulfate gel and run for the HFD and treated groups (AA and orlistat). The gels were transferred from bands to polyvinylidene fluoride membrane using trans turbo gel transfer equipment. The primary antibodies anti-ACC (Ser79), anti-UCP 2 (ab67241), and anti CPT 1 (ab53532) were added, and the membrane developed blots which were analyzed using ChemiDoc equipment (ChemiDoc™, Bio-Rad Laboratories, Inc.).
Histopathological studies
Harvested liver tissues from the sacrificed animals were fixed in 10% neutral-buffered formalin solution, dehydrated in ethanol, and embedded in paraffin. Then, 5-µm thick sections were prepared using a rotary microtome and stained with hematoxylin and eosin dye for microscopic observations.
Statistical analysis
One-way ANOVA was used, and the results were expressed as mean ± standard deviation (SD). The least significant difference (LSD) test was also performed. The level of statistical significance was set at p < 0.05.
Results
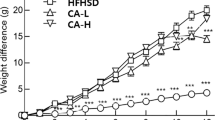
Figure 2 depicts the changes in BW in the control and HFD groups during the experiment. The BW of the HFD group was significantly (p < 0.05) higher than that of the normal control group because of HFD intake for 42 days. The groups treated with orally administered AA (20 mg/kg BW) or orlistat exhibited a significantly (p < 0.05) lower increase in BW than the HFD control group did.
Table 2 depicts the levels of plasma glucose, plasma insulin, and insulin resistance in the control and experimental obese rats. A significant (p < 0.05) increase was observed in the levels of plasma glucose, plasma insulin, and insulin resistance in the HFD-fed rats. Oral supplementation of AA (20 mg/kg BW) or orlistat tended to bring the levels of blood glucose and plasma insulin toward near normal levels.
Figure 3 presents the level of oral glucose tolerance in the control and experimental obese rats. In the control rats, a significant increase was observed in the blood glucose level, and it reached the maximum value at 30 min after glucose load. Then, the levels declined to near basal levels at 120 min. However, in the HFD-induced obese rats, the blood glucose levels were at the maximum value even beyond 60 min after glucose load and remained high over the next 90 min. Oral administration of AA (20 mg/kg BW) or orlistat to obese rats resulted in a significant reduction in the blood glucose levels at 90 min compared with the HFD control rats.
Figure 4 depicts the levels of leptin and adiponectin in the control and experimental obese rats. A significant (p < 0.05) increase in leptin levels and decrease in adiponectin levels were observed in the HFD-induced obese rats compared with the control rats. Oral administration of AA (20 mg/kg BW) or orlistat reduced the levels of leptin and adiponectin to near normal levels.
The activities of amylase and pancreatic lipase of the normal and experimental obese rats are depicted in Fig. 5. The HFD-fed rats exhibited a significant increase (p < 0.05) in the activities of amylase and pancreatic lipases. Oral administration of AA (20 mg/kg BW) or orlistat to obese rats significantly reduced the activity of amylase and pancreatic lipase.
Figure 6 presents the lipid profiles of the control and HFD-induced obese rats. The levels of plasma and liver lipids were significantly higher in the experimental obese rats than in the normal rats. Oral administration of AA (20 mg/kg BW) or orlistat significantly (p < 0.05) reduced the levels of plasma and liver lipids in obese rats to near normal levels.
Table 3 lists the levels of TBARS and activities of GSH, SOD, CAT, and GPx in the livers of the control and HFD-induced experimental obese rats. A considerable decrease in the activities of GSH, SOD, CAT, and GPx and a concomitant increase in the level of TBARS were observed in the HFD-induced experimental obese rats. Treatment with AA or orlistat considerably increased the activities of SOD, CAT, and GPx and reduced the levels of TBARS in livers of treated animals.
Figure 7 and a depicts the mRNA levels of CPT 1, UCP 2 and ACC 1 in the tissues of the control and experimental obese rats. Significantly (p < 0.05) lower levels of CPT 1 and UCP 2 mRNA and a concomitant increase in the levels of ACC 1 mRNA were observed in the tissues of the HFD control rats compared with the normal control rats. AA (20 mg/kg BW) or orlistat administration (oral) significantly (p < 0.05) increased the activity of CPT 1 and UCP 2 and reduced the activity of ACC 1 in the tissues of the treated obese rats. Figure 7b depicts the expression of the proteins CPT 1, UCP 2, and ACC 1 in the tissues of the control and experimental obese rats. Western blot analysis of these proteins revealed that the alterations in protein expression were normalized after treatment with AA or orlistat, and these results were supported by mRNA expression studies.
Effect of AA on the mRNA levels of CPT-1, UCP-2, and ACC-1 in tissues of control and experimental obese rats. a CPT-1, UCP-2, and ACC-1 mRNA expressions. Values are expressed as Mean ± SD for 6 animals in each group. Values are statistically significant at *p < 0.05. aSignificantly different from control. bSignificantly different from HFD control. b Western blot analysis of CPT-1, UCP-2, and ACC-1 protein expressions in control and experimental groups. I: Normal control; II: HFD control; III: HFD + AA; IV: HFD + Orlistat. L1: ACC; L2: UCP 2; L3: CPT 1
The group of ND-fed control rats exhibited normal histological architecture (Fig. 8a). Significant hepatic steatosis was observed along with severe swelling of the hepatic cells. Fat accumulation was observed in the livers of the HFD-fed rats (Fig. 8b). Treatment with AA or orlistat resulted in the prevention of hepatic fat deposition in hepatocytes and, reduced most of the pathological alterations induced by HFD in the rats (Fig. 8c, d).
Effect of AA in Liver of control and experimental obese rats. a (Normal Control) Rats administrated normal diet showed normal histological architecture; H&E, X40. b (HFD Control): Hepatic steatosis was observed along with severe swelling in hepatic cells and also fat accumulation was observed in the livers of HFD-fed rats; H&E, X40. c (HFD + AA), d (HFD + Orlistat) Treatment with AA and Orlistat reduced most of the pathological alterations induced by HFD in rats; H&E, X40
Discussion
Diet-induced obesity (DIO) in animals shares many features with human obesity; hence, it is widely used to identify medicinal foods for alleviating obesity. Prolonged feeding with fat-enriched diets increases in the BW in liable rats in the range of 10–20% compared with standard chow-fed controls. Although HFDs produced from animals and plant fats do not exhibit consistent differences because of fat-type effects, some authors have described obesity resistance and less hypertrophy of visceral fat pads when diets produced from fish oil are used. According to the literature, semi-purified diets with a fat content of 40% produced using animal fats and plant oils that contain ω-6/ω-9 fatty acid cause insulin resistance and obesity, whereas diets with large amounts of ω-3-fatty acids do not. However, given the plethora of dietary regimes described in the literature, characterizing a single all encompassing HF diet composition is difficult. Furthermore, diets theoretically composed of identical fat types might yield diverse results because of inherent differences among the primary fat sources and among various diet preparation methods [13].
The signs of DIO are insulin resistance, changes in body weight composition, impaired glucose tolerance, and abnormal levels of lipids [2]. In the present study, increased BW and fat were observed in HFD-fed rats. Long-term HFD intake results in increased bodyweight and plasma comorbidity factors [14]. These effects might occur because of the consumption of an energy-rich diet in the form of saturated fats (lard) and its accretion in different body fat pads [15], thus leading to an excessive development of the adipose tissue. Furthermore, the ratio of calorie ingestion to energy utilization determines the bodyweight. In this study, HFD provided a total energy content of 17.03 kJg−1. Thus, compared with the ND, the HFD was hypercaloric. The HFD contained less carbohydrate but more lipids than the ND, with a net energy difference of 4.37 kJ g−1. Comparable effects have been reported in previous animal studies in which obesity was induced using high-fat rodent diets having similar sources of fat as the HFD in the current study and a similar experimental length to the current study [2]. The HFD-fed rats treated with AA exhibited a significantly lower BW increase than the HFD control rats did. In the present study, AA apparently did not suppress feeding in the HFD-fed rats (data not shown). Hence, the AA-induced weight loss involves a mechanism that is independent of hypophagia. The relatively low BW gain may be caused by numerous mechanisms including unusual food assimilation, decreased body energy storage, and the reduction in the degree of BW gain [14].
The supplementation of an HFD for a period of 30 days caused hyperglycemia, as shown by the increased levels of plasma glucose, plasma insulin, and insulin resistance [16]. In the current study, the HFD with 58% calories as fat, caused insulin resistance in rats over a short period of time. Therefore, HFD intake for a period of 30 days causes insulin resistance syndrome and increased BW (obesity), hypertriglyceridemia, and mild hyperglycemia [17]. HFD-fed rats may be susceptible to insulin resistance because the receptor cells are blocked by fat deposits; consequently, diabetes becomes evident. In the present study, we found that the HFD-fed rats clearly exhibited hyperglycemia in the presence of similar amounts of plasma insulin concentrations as the normal controls. These rats also exhibited the persistence of insulin resistance. In the present study, a significant increase in the fasting blood levels of glucose and insulin, insulin resistance, and BW gain was observed in the HFD-fed rats compared with the normal control rats. This effect might be due to HFD intake [17]. Moderate hepatic and muscular uptake of glucose caused hyperlipidemia because of increased fat mobilization from the adipose tissue and resistance to the anti-lipolytic action of insulin. Impaired insulin function is related to an excessive intake of lipids. Although HFDs have been reported to induce insulin resistance through different mechanisms, the resistance is mainly considered to involve the Randle or glucose–fatty acid cycle [18].
HFD supplementation is demonstrated by increased TG and TC levels. Accordingly, a variation in lipid profiles can be used as an index of obesity. In the present study, HFD intake increased the lipid profile in the experimental obese rats. In addition, the modifications in the lipid profile induced by HFD might involve lipolysis, intestinal fat absorption, and the activation of gastric lipases. High TC levels increase the risk of coronary heart disease. A high LDL-C level is a risk factor for coronary heart disease, whereas a high HDL-C level facilitates the transport of excess cholesterol to the liver for excretion in the bile [19]. The increase in TG level caused by dietary cholesterol was shown to reduce fatty acid oxidation, which in turn increases the levels of hepatic and plasma triglycerol [20].
Obesity is accountable for the escalating occurrence of metabolic disease. In the body, the adipose tissue is a key site of energy storage and is crucial for energy homeostasis [15]. It is well known that insulin can ultimately stimulate leptin secretion during the metabolism of nutrients, particularly during glucose utilization in adipocytes. Hyperlipidemia, hyperglycemia, insulin resistance, impaired glucose metabolism, distinctive visceral adiposity, hyperinsulinemia, and decreased bone mineral concentration and bone mineral density are the common characteristics of DIO in rodents. In the present study, HFD treatment to the experimental animals confirmed obesity as evidenced by the increased BW, hyperglycemic condition, and increased insulin resistance [21]. Under physiological conditions, insulin enhances lipogenesis and inhibits lipolysis leading to increased circulating levels of glucose and lipids, thus resulting in impaired glucose-stimulated insulin secretion [22]. HFD is intimately associated with the development of obesity by active adipocytes; HFD results when the adipocytes incorporate glucose and free fatty acids (FFAs) to synthesize and accumulate TG to store energy [23]. In the present study, we observed that AA treatment reduced plasma insulin level, suggesting that AA could improve insulin resistance in the experimental animals. AA promotes insulin sensitivity, thus lowering insulin resistance and reducing glucose levels in obese rats, perhaps by controling the cell energy metabolism or reducing the storage of FFAs. Evidence substantiates that AA considerably lowered blood glucose levels in rats with streptozocin-induced diabetes where asiatic acid preserved β-cell death and promoted their proliferation [24]. Furthermore, administration of AA significantly improved glucose homeostasis in a metabolic syndrome such as diabetes [11].
The adipose tissue is the primary site of fat accumulation. Accumulation of excessive fat in the adipocytes is the fundamental observable symptom for obesity. Adipose tissue secretes numerous adipokines including leptin, adiponectin, resistin, visfatin, tumor necrosis factor, and interleukin-6 which participate in energy regulation [25]. Leptin and adiponectin secreted by adipocytes are believed to play prominent roles in controling metabolic homeostasis. Reduced plasma adiponectin levels were observed in obese animals and, the low levels was positively connected to HDL-C levels [1]. Leptin, a circulating fat-derived protein produced by the fat tissue, plays a fundamental role in controlling BW by restraining food intake and improving energy consumption. Leptin resistance is a feature of DIO, in which the blood leptin levels diminish and do not respond to target tissues (example, fat tissue, muscles, liver, and hypothalamus). Adipocytes secrete leptin in direct proportion to adipose tissue mass as well as nutritional status [26], where as adiponectin is inversely correlated with body mass [27]. During the development of obesity, elevated levels of leptin and concomitantly decreased levels of adiponectin are observed [27, 28]. Leptin secretion is positively interrelated with the extent of the TG stores in adipocytes [29]. In the present study, increased leptin and decreased adiponectin levels were observed in the plasma of HFD control group compared with the control group. Treatment with AA lowered leptin and enhanced adiponectin in the plasma of the experimental rats. A few polyphenols have been reported to affect lipid catabolism and diminish insulin resistance which are fundamental to obesity [30]. These observations suggest that the decreased leptin and increased adiponectin levels after AA supplementation may have ameliorated insulin resistance in obese rats, thus resulting in decreased plasma lipid levels and weight loss [31].
Amylase and lipase, the key catalysts in carbohydrate and lipid metabolism, are the focus for developing medication outlines for treatment of some metabolic disorders. Pancreatic lipase, the principal lipolytic enzyme secreted from the pancreas, hydrolyzes dietary fat into fatty acid and 2-monoacylglycerol. Inhibition of this digestive enzyme is accordingly useful in the treatment of overweight patients [1]. α-amylase, one of the key digestive compounds discharged from the pancreas and salivary organs, is included in hydrolytic process of starch [32]. Because dietary lipids and sugars constitute the major source of undesirable calories, the hindrance of fat and carbohydrate digestion is a novel methodology for reducing fat absorption. Activating lipase or inhibiting pancreatic lipase would have an anti-obesity effect. Lowered pancreatic amylase discharge reduces the assimilation of carbohydrates by suppressing their processing, thus resulting in decreased energy intake [33]. Various exploratory reports have reported that α-amylase inhibitors, most of which are extricated from plants, can reduce post-prandial hyperglycemia, thus regulating abnormal glucose metabolism and countering metabolic disorders [34]. In the present study, pancreatic lipase and amylase levels increased in HFD-induced obese rats. Oral supplementation of AA inhibited the activity of pancreatic lipase and α-amylase in the treated rats compared with HFD control rats. The minimized levels of pancreatic amylase and lipase may represent a component that impedes the assimilation and ingestion of starches and lipids, which in turn, can reduce the caloric admission in AA-treated HFD-fed obese rats, to enhance weight reduction.
Obesity, particularly abdominal obesity, is an independent risk factor that increases cardiovascular disease risk and overall mortality and warrants medical attention [35]. The HFD-induced obese rats exhibited anomalies in plasma and tissue biomarkers that mimic the commencement of a group of metabolic risks including abnormalities in lipid profile. HFD-induced obesity is associated with increasing levels of TGs, very low-density lipoproteins (VLDLs), TC, phospholipids (PLs), FFAs, and a decrease in plasma levels of HDL [36]. In the present study, lipid-level abnormalities such as elevated TGs, VLDLs, TC, PL, FFA, and LDL, and reduced plasma levels of HDL were observed. These findings was supported by Park et al. [37] During the fed state, elevation of chylomicrons is a typical element which causes an increase in the levels of TC, TGs, and endogenous VLDL generation. The increased release of FFAs from fat tissue to different tissues increases, primarily to the liver during obesity [38], and it might be because of the increment of leptin resistance. The increase in the level of TGs was because of dietary cholesterol that had appeared to reduce unsaturated fat oxidation, which thus expanded the levels of hepatic and plasma TG and caused the excessive accumulation of TGs in the lipid stores [2]. The elevated level of phospholipids in this present study was probably due to the elevated levels of FFA and TC that can enhance the production of PLs. The elevated PL level in the present study may be because of the elevated levels of FFA [36] and an increase in cholesterol levels that can support the generation of phospholipids. High TC levels intensify the risk of coronary heart disease by increasing LDL-C levels. However, high HDL-C levels facilitate the transport of surplus cholesterol to the liver for excretion in the form of bile [39]. Oral supplementation of AA significantly lowered the levels of TC, TGs, FFAs, and PLs in both serum and liver and the LDL-C levels in the serum of the rats with HFD-induced obesity. Yongqi et al. [40] reported that supplementation of phytoconstituents to fed animals leads to a hypolipidemic state by reducing cholesterol absorption and secretion from the intestine, which leads to the reduced availability of FFAs to the liver. Our finding is consistent with this report.
The liver is considered one of the vital metabolic organs in the body, regulating and maintaining lipid homeostasis. Insulin deficit causes various disturbances in regulatory and metabolic processes [35], which in turn cause accumulation of lipids in the liver. In obesity, the liver stores excess amounts of fatty acids and after esterification with glycerol phosphate, the fatty acids are deposited as TG. This leads to a reduction in insulin-mediated metabolic activity and can cause diabetes, which ensues in metabolic syndrome [41]. The increase in the liver cholesterol levels of obese rats observed in our study could be due to decreased removal of cholesterol from the extra hepatic tissues by HDL cholesterol and also increased cholesterogenesis [19]. Treatment of obese rats with AA and orlistat showed a decrease in the liver cholesterol and TG levels. This may be due to enhanced clearance and also the decreased production of the major transporters of endogenously synthesized cholesterol and triglycerides; thus, AA exhibited hepatoprotective effects.
Oxidative damage in cells is invariably associated with disturbances in multiple non-enzymatic and enzymatic antioxidant protection systems present in the cells [42]. Enzymatic antioxidants such as CAT, GPx, and SOD synergistically prevent lipid peroxidation and scavenge reactive oxygen species. SOD, the natural antioxidant enzyme in cells, plays a crucial role in oxygen defense metabolism by intercepting and reducing the superoxide radical to hydrogen peroxide [43]. CAT, a heme-containing omnipresent enzyme, is well known to be involved in the detoxification of high hydrogen peroxide concentrations and defending the tissues from highly reactive hydroxyl radicals. GPx, a selenium-containing tetrameric glycoprotein, occurs in high concentrations in cells. It detoxifies hydrogen peroxide into molecular oxygen and water through the oxidation of reduced GSH [44]. GPx has been revealed to be a significant adaptive response to a state of prolonged peroxidative stress [45]. Previous studies have demonstrated that through obesity induced by HFD, enzymatic antioxidant levels were noticeably reduced. In the current study, lower hepatic GPx, CAT, and SOD activities were observed in HFD-fed rats than in the control rats. This is consistent with the results of Brahmanaidu et al. [46], who demonstrated relatively low levels of antioxidant enzymes in HFD-fed animals which might result from high production of free radicals. Administration of AA significantly enhanced GPx, SOD, and CAT activities and diminished TBARS [47] levels in HFD-fed rats. This finding indicates the potential of AA as an effectual inhibitor of the oxidative stress induced by HFD.
Obesity is connected with lipid accretion not only in the adipose tissues but also in non-adipose tissues, such as the liver and skeletal muscles [48]. Skeletal muscles are the chief sites of fatty acid catabolism and abnormal fat accumulation in the skeletal muscle causes metabolic disorders including overweight. CPT 1 and UCP 2 act as the rate-limiting enzyme for β-oxidation and main regulator of thermogenesis, respectively [49]. ACC 1 is the first and rate-limiting enzyme in the peroxisomal β-oxidation pathway [50]. Fatty acids are transformed to acetyl CoA through mitochondrial oxidation. Fatty acid oxidation is inhibited by dephosphorylated AMPK. PPARγ is known to be activated by SREBP1c, which leads to reduced FFA oxidation [51, 52]. In the present study, the elevated expression of ACC 1 and concomitantly reduced expression of CPT 1 and UCP 2 were observed in HFD-induced obese rats. Oral administration of AA altered the expression of ACC 1, CPT 1, and UCP 2 to near normal. These results were also supported by the western blot analysis results. Moreover, AA restored the PPAR-γ downstream genes CPT 1 and UCP 2, contributing systematically to energy catabolism. Thus, the findings imply that treatment with AA can reduce DIO by promoting lipid oxidation through activation of PPAR-γ and its downstream genes.
In the present study, the histopathological examinations of the livers of HFD-fed rats revealed microvesicular steatosis in the hepatocytes. Notably, treatment with AA and orlistat reduced most of the pathological alterations induced by HFDs in rats because it reduced hepatic lipid accumulation, which resulted from both decreased lipogenesis and increased fatty acid oxidation. Therefore, AA has potential therapeutic use as a nutraceutical ingredient for the prevention of obesity and hyperlipidemia.
In conclusion, our results suggest that dietary supplementation of asiatic acid extracted from C. asiatica considerably reduces the increase in BW and fat percentage in HFD-induced obese rats by altering lipid metabolic markers. Hence, these results strongly suggest that asiatic acid has therapeutic potential for the management of obesity and hyperlipidemia and for the prevention of cardiovascular diseases.
References
Despres JP (2012) Body fat distribution and risk of cardiovascular disease: an update. Circulation 126:1301–1313
Saravanan G, Ponmurugan P, Deepa MA, Senthilkumar B (2014) Anti-obesity action of gingerol: effect on lipid profile, insulin, leptin, amylase and lipase in male obese rats induced by a high-fat diet. J Sci Food Agric 94:2972–2977
Ferranti S, Mozaffarian D (2008) The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem 54:6945–6955
Jindal A, Brietzke S, Sowers JR (2012) Obesity and the cardiorenal metabolic syndrome: therapeutic modalities and their efficacy in improving cardiovascular and renal risk factors. Car Ren Med 2(4):314–327
George M, Rajaram M, Shanmugam E (2014) New and emerging drug molecules against obesity. J Cardiovasc Pharmacol Ther 19(1):65–76
Colagiuri S (2010) Diabesity: therapeutic options. Diabetes Obes Metab 12:463–473
Kishino E, Ito T, Fujita K, Kiuchi Y (2006) A mixture of the Salacia reticulata (Kotala himbutu) aqueous extract and cyclodextrin reduces the accumulation of visceral fat mass in mice and rats with high-fat diet-induced obesity. J Nutr 136:433–439
Zhao Y, Shu P, Zhang Y, Lin L (2014) Effect of Centella asiatica on oxidative stress and lipid metabolism in hyperlipidemic animal models. Oxid Med Cell Longev 154:1–7
Huang SS, Chiu CS, Chen HJ, Hou WC, Sheu MJ, Lin YC, Shie PH, Huang GJ (2011) Antinociceptive activities and the mechanisms of anti-inflammation of asiatic acid in mice. Evid Based Complement Altern Med. doi:10.1155/2011/895857
Ramachandran V, Saravanan R, Senthilraja P (2014) Antidiabetic and antihyperlipidemic activity of asiatic acid in diabetic rats, role of HMG CoA: in vivo and in silico approaches. Phytomed 212:225–232
Ramachandran V, Saravanan R (2013) Asiatic acid prevents lipid peroxidation and improves antioxidant status in rats with streptozotocin-induced diabetes. J Funct Foods 5:1077–1087
Ji W, Zhao M, Wang M, Yan W, Liu Y, Ren S (2017) Effects of canagliflozin on weight loss in high-fat diet-induced obese mice. PLoS ONE 12(6): e0179960.
Buettner R, Schölmerich J, Bollheimer LC (2007) High-fat diets: modeling the metabolic disorders of human obesity in rodents. Obesity 15:798–808
Naidu PB, Uddandrao VS, Naik RR, Suresh P, Meriga B, Begum MS, Pandiyan R, Saravanan G (2016) Ameliorative potential of gingerol: promising modulation of inflammatory factors and lipid marker enzymes expressions in HFD induced obesity in rats. Mol Cell Endocrinol 419:139–147
Oben J, Kuate D, Agbor G, Momo C, Talla X (2006) The use of a Cissus quadrangularis formulation in the management of weight loss and metabolic syndrome. Lip Heal Dis 5:24
Srinivasan K, Patole PS, Kaul CL, Ramarao P (2004) Reversal of glucose intolerance by pioglitazone in high-fat diet fed rats. Exp Clin Pharmacol 26:327–333
Naidu PB, Ponmurugan P, Begum MS, Mohan K, Meriga B, Naik RR, Saravanan G (2015) Diosgenin reorganises hyperglycaemia and distorted tissue lipid profile in high-fat diet–streptozotocin-induced diabetic rats. J Sci Food Agric 95:3177–3182
Randle PJ, Garland PB, Hales CN, Newsholme EA (1963) The glucose fatty-acid cycle. Its role in insulin sensitivity andmetabolic disturbances in diabetes mellitus. Lancet 1:785–789
Saravanan G, Ponmurugan P (2012) Ameliorative potential of S-allylcysteine: effect on lipid profile and changes in tissue fattyacid composition in experimental diabetes. Exp Toxicol Pathol 64:639–644
Fungwe TV, Cagen LM, Cook GA (1993) Dietary cholesterol stimulated hepatic biosynthesis of triglyceride and reduces oxidation of fatty acids in the rat. J Lipid Res 34:933–941
Kim Y, Park T (2008) Genes are differentially expressed in the epididymal fat of rats rendered obese by a high-fat diet. Nutr Res 28:414–422
Zhou CJ, SongHuang JQ (2013) Sweet tea leaves extract improves leptin resistance in diet-induced obese rats. J Ethnopharm 145:386–392
Manuel TV, Sam JB (2007) Role of dietary so y protein in obesity. Int J Med Sci 4:72–82
Liu J, He T, Lu Q, Shang J, Sun H, Zhang L (2010) Asiatic acid preserves β cell mass and mitigates hyperglycemia in streptozocin-induced diabetic rats. Diabetes Metab Res Rev 26:448–454
Garg A (2006) Adipose tissue dysfunction in obesity and lipodystrophy. Clin Cornerstone 8:7–13
Cnop M, Landchild MJ, Vidal J, Havel PJ, Knowles NG, Carr DR (2002) The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations. Diabetes 51:1005–1015
Arita Y, Kihara S, Ouchi N (1999) Paradoxical decrease of an adipose-specific protein, adiponectin in obesity. Biochem Biophys Res Commun 257:79–83
Kamohara S, Burcelin R, Halaas JL, Friedman JM, Charron MJ (1997) Acute stimulation of glucose metabolism in mice by leptin treatment. Nature 389:374–377
Staiger H, Haring HU (2005) Adipocytokines: fat-derived humoral mediators of metabolic homeostasis. Exp Clin Endocrinol Diabetes 113:67–79
Crozier A, Jaganath IB, Clifford MN (2009) Dietary phenolics: chemistry, bioavailability and effects on health. Nat Prod Rep 26:1001–1043
Ono Y, Hattori E, Fukaya Y, Imai S, Ohizumi Y (2006) Anti-obesity effect of Nelumbo nucifera leaves extract in mice and rats. J Ethnopharm 106:238–244
Nakajima K, Muneyuki T, Munakata H (2011) Revisiting the cardiometabolic relevance of serum amylase. BMC Res Not 4:419
Tundis R, Loizzo MR, Menichini F (2010) Natural products as alpha-amylase and alpha-glucosidase inhibitors and their hypoglycaemic potential in the treatment of diabetes: an update. Mini Rev Med Chem 10:315–331
Layer P, Rizza RA, Zinsmeister AR, Carlson GL, DiMagno EP (1986) Effect of a purified amylase inhibitor on carbohydrate tolerance in normal subjects and patients with diabetes mellitus. Mayo Clin Proce 61:442–447
Naidu PN, Uddandrao VS, Sasikumar V, Naik RR, Pothani S, Begum MS, Varatharaju C, Meriga B, Kalaivani A, Saravanan G (2017) Reversal of endothelial dysfunction in aorta of streptozotocinnicotinamide-induced type-2 diabetic rats by S-Allylcysteine. Mol Cell Biochem. doi:10.1007/s11010-017-2994-0
Jin D, Xua Y, Mei X (2013) Antiobesity and lipid lowering effects of theaflavins on high-fat diet induced obese rats. J Funct Foods 5:1142–1150
Park Y, Storkson JM, Liu W, Albright J, Cook ME, Pariza MW (2004) Structure–activity relationship of conjugated linoleic acid and its cognates in inhibiting heparin-releasable lipoprotein lipase and glycerol release from fully differentiated 3T3-L1 adipocytes. J Nutr Biochem 15:561–569
Torre-Villalvazo I, Tovar AR, Ramos-Barragan VE, Cerbon-Cervantes MA, Torres N (2008) Soy protein ameliorates metabolic abnormalities in liver and adipose tissue of rats fed a high fat diet. J Nutr 138:462–468
Garjani A, Fathiazad F, Zakheri A, Akbari NA, Azarmie Y (2009) The effect of total extract of Securigera securidaca L. seeds on serum lipid profiles, antioxidant status, and vascular function in hypercholesterolemic rats. J Ethnopharm 126:525–532
Yongqi G, Guanzhong W, Xin S, Hongxia Y, Juan Z (2009) Antiobesity action of a daidzein derivative on male obese mice induced by a high-fat diet. Nutr Res 29:656–663
Moller DE (2001) New drug targets for type 2 diabetes and the metabolic syndrome: a review. Nature 414:821–827
Uddandrao VS, Brahmanaidu P, Saravanan G (2016) Therapeutical perspectives of S-allylcysteine: effect on diabetes and other disorders in animal models. Car Hem Age Med Chem. doi:10.2174/1871525714666160418114120
Winterbourn CC (1995) Concerted antioxidant activity of glutathione and superoxide dismutase. In: Packer L, Fuchs J (eds) Biothiols in health and disease. Marcel Dekker Inc, New York, pp 117–134
Saravanan G, Ponmurugan P (2011) Ameliorative potential of S-allylcysteine on oxidative stress in STZ induced diabetic rats. Chem Biol Interact 189:100–106
Uddandrao VS, Brahmanaidu P, Meriga B, Saravanan G (2016) The potential role of S-allylcysteine as antioxidant against various disorders in animal models. Oxid Antioxid Med Sci 5(3):79–86
Naidu PB, Harishankar N, Meriga B, Pothana S, Sajjalaguddam RR (2015) Effects of Piper nigrum extracts: Restorative perspectives of high-fat diet-induced changes on lipid profile, body composition, and hormones in Sprague-Dawley rats. Pharm Biol 53(9):1318–1328
Naidu PB, Uddandrao VS, Pothani S, Naik RR, Begum MS, Varatharaju C, Pandiyan R, Saravanan G (2016) Effects of S-allylcysteine on biomarkers of polyol pathway in experimental type II diabetes in rats. Can J Diabetes 40:442–448
Van Herpen NA, Schrauwen-Hinderling VB (2008) Lipid accumulation in non-adipose tissue and lipotoxicity. Physiol Behav 94:231–241
Harbilas D, Braulta A, Valleranda D (2012) Populus balsamifera L. (Salicaceae) mitigates the development of obesity and improves insulin sensitivity in a diet-induced obese mouse model. J Ethnopharm 141:1012–1020
Wanga LJ, Zhang HW, Zhoua JY (2014) Betaine attenuates hepatic steatosis by reducing methylation of the MTTP promoter and elevating genomic methylation in mice fed a high-fat diet. J Nutr Biochem 25:329–336
Andrews ZB, Erion DM, Beiler R, Choi CS, Shulman GI, Horvath TL (2010) Uncoupling protein-2 decreases the lipogenic actions of ghrelin. Endocrinology 151:2078–2086
Ferre P, Foufelle F (2010) Hepatic steatosis: a role for de novo lipogenesis and the transcription factor SREBP-1c. Diabetes Obes Metab 12:83–92
Acknowledgements
The authors thank Muthyammal College of Arts and Science, Rasipuram, Tamilnadu, India, for providing facilities to do animal studies and also express heartfelt thanks to the management of K. S. Rangasamy College of Arts and Science, Tiruchengode, Tamilnadu, for their support and encouragement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures involving laboratory animals were in accordance with the guidelines of Committee for the purpose of control and supervision of experiments on animals (CPCSEA), Government of India, and institutional animal ethical committee of Muthyammal College of Arts and Science (Approval No: IAEC/MCAS/05/2016).
Rights and permissions
About this article
Cite this article
Rameshreddy, P., Uddandrao, V.V.S., Brahmanaidu, P. et al. Obesity-alleviating potential of asiatic acid and its effects on ACC1, UCP2, and CPT1 mRNA expression in high fat diet-induced obese Sprague–Dawley rats. Mol Cell Biochem 442, 143–154 (2018). https://doi.org/10.1007/s11010-017-3199-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-3199-2