Abstract
Recombinant COMP-Ang1, a chimera of angiopoietin-1 (Ang1), and a short coiled-coil domain of cartilage oligomeric matrix protein (COMP) can stimulate multiple cellular processes. Proliferative capacity of periodontal ligament (PDL) fibroblasts (PLFs) is important for maintaining PDL integrity and homeostasis. In this study, we explored whether exogenous COMP-Ang1 addition enhances proliferation of human PLFs and the cellular mechanisms therein. We initially isolated and characterized PLFs, where the cells showed highly positive staining for surface markers, CD90, CD105, and CD146. COMP-Ang1 treatment increased proliferation of PLFs by stimulating migration of cells into S and G2/M phases. This increase was coupled with decreased p21Cip and p27Kip levels and enhanced cyclin D1, cyclin-dependent kinase (CDK) 2, and CDK4 induction. Transfection with si-Tie2 near completely blocked COMP-Ang1-stimulated cell cycle progression in PLFs. Tie2 knockdown also inhibited COMP-Ang1-induced phosphorylation of mitogen-activated protein kinases (MAPKs). In addition, COMP-Ang1-mediated activation of Akt and c-Jun was suppressed by treating each of pharmacological inhibitors specific to phosphoinositide 3-kinase (PI3K) (LY294002 and Wortmannin) or MAPKs (PD98059, SB203580, and SP600125). Similarly, COMP-Ang1-mediated increases in DNA synthesis and cyclin D1 induction were prevented by treating inhibitor of MAPKs and PI3K or by c-Jun knockdown. These results suggest that COMP-Ang1 enhances survival and proliferation of human PLFs through the activation of Tie2-mediated signaling, where PI3K/Akt and MAPK-c-Jun signaling pathways act as downstream effectors. Collectively, COMP-Ang1 may be a useful as a stimulator of human PLFs and therefore improves PDL integrity and homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal tissues consisted mainly of three parts such as gingival, periodontal ligament (PDL), and alveolar bone. PDL is a highly specialized fibrous connective tissue that attaches the tooth root to the surrounding alveolar bone and maintains tooth stability and function. The PDL consists of a heterogeneous cell population including fibroblasts, osteoblasts, cementoblasts, epithelial and endothelial cells, and stem-like cells known as PDL stem cells (PDLSCs) [1, 2]. It has been considered that PDL functions are affected according to cellular activities of PDL fibroblasts (PLFs) which are the most abundant cells in the PDL [3]. PLFs play important roles in maintaining PDL integrity during alveolar bone remodeling [4]. PLFs are also able to differentiate into osteoblastic cells and collagen-forming cells and produce various types of paracrine and autocrine factors [5, 6]. Thus, it is postulated that PLFs have critical roles in maintaining PDL homeostasis and in protecting PDL against physiological and biological stresses. Furthermore, considerable evidence has proven that controlling the proliferation of stem/progenitor cells is to be a key approach for a successful cell-based therapy [7, 8]. This may suggest that improving the proliferative capacity of PLFs is one of the beneficial strategies to inhibit PDL degradation caused by various mechanical and biological damages.
Much attention has focused on the recombinant chimeric protein of angiopoietin 1 (Ang1) with a short coiled-coil domain from cartilage oligomeric matrix protein (COMP) as a potent stimulator of cellular processes required for proliferation, differentiation, and migration of stem-like cells. In fact, COMP-Ang1 had a more stable angiogenic activity than did native Ang1 in vascular formation [9]. COMP-Ang1 also showed multiple potentials to enhance osteoblast differentiation [10], bone formation [11], and chondrocyte maturation [12]. We recently found that COMP-Ang1 stimulates proliferation, differentiation, and migration of bone marrow mesenchymal stem cells (MSCs) [13] and promotes bone formation in an animal model of calvarial defects [14]. We also demonstrated that the potentials of COMP-Ang1 are correlated with its angiogenic and chemoattractive activities [13]. Our previous findings with other reports suggest that COMP-Ang1 regulates positively cellular processes required for differentiation, survival, and proliferation of PLFs [10–14]. However, the exact modes of action by which COMP-Ang1 improves proliferation of PLFs are not yet investigated.
In this study, we explored whether exogenous COMP-Ang1 addition actually enhances viability and proliferation in human PLFs. In order to understand the related mechanisms, we examined the roles of several signaling molecules including Tie-2, cyclins, cyclin-dependent kinases (CDKs), mitogen-activated protein kinases (MAPKs), phosphoinositide 3-kinase (PI3K)/Akt, and c-Jun in COMP-Ang1-exposed PLFs. We also compared the potential of COMP-Ang1 on PLFs to that of native Ang1.
Materials and methods
Chemicals and laboratory wares
Carrier-free recombinant COMP-Ang1 and fetal bovine serum (FBS) were purchased from Enzo Life Sciences Inc. (Farmingdale, NY, USA) and Gibco-BRL (Gaithersburg, MD, USA), respectively. Pharmacological inhibitors, including PD98059 (for phospho-extracellular signal-regulated kinase; p-ERK), SB203580 (for p-p38 kinase), SP600125 (for p-c-Jun N-terminal kinase; p-JNK), and LY294002 and Wortmannin (for PI3K) were purchased from TOCRIS (Bristol, UK). Monoclonal antibodies specific for cell surface markers such as STRO-1, CD45, CD90, CD105, and CD146 were obtained from Becton–Dickinson (San Jose, CA, USA). Unless otherwise specified, other antibodies and chemicals were supplied from Santa Cruz Biotechnology (Santa Cruz, CA, USA) and Sigma-Aldrich Co. (St. Louis, MO, USA), respectively. All laboratory items were purchased from SPL Life Sciences (Pochun, South Korea).
Isolation and culture of human PLFs
Disease free molars were collected from seven healthy male patients, 20–28 years old (23.7 ± 2.5 age), who required for extraction of teeth in the process of orthodontic treatment, at the Chonbuk National University Hospital (Jeonju, South Korea). All donors gave written informed consent for the use of their tissues, and this study was approved by the Ethical Committee of Chonbuk National University Hospital. The isolation and culture of PLFs were carried out according to the methods described elsewhere with a slight modification [15]. In brief, PDL was scraped from the root of molars eluted from each of patients and then enzymatically digested for 1 h at 37 °C in a buffer containing 3 mg/ml collagenase type I (Worthington Biochem, Freehold, NJ, USA) and 4 mg/ml of dispase (Worthington Biochem). Single cell suspensions were obtained from different individuals using a 70-μm Falcon cell strainer (Franklin Lakes, NJ, USA) and incubated in DMEM supplemented with 10 % FBS and antibiotics (100 IU/ml penicillin G and 100 μg/ml streptomycin) in 100 mm culture dish. The cultures were switched to a fresh batch of medium every 3 days allowing subculture when the cells reached 70–80 % confluence.
Characterization of PLFs
The characterization of PLFs was performed by analyzing the expression of cell surface markers at passage 2. In brief, PLFs were harvested using 0.25 % trypsin/EDTA buffer and fixed with 4 % formaldehyde for 30 min. Cells were washed with phosphate buffered saline (PBS) containing 0.2 % bovine serum albumin and then incubated for 30 min in PBS containing fluorescein isothiocyanate (FITC)—conjugated monoclonal antibodies directed against antigens (STRO-1, CD90, and CD105) or phycoerythrin (PE)-conjugated monoclonal antibodies directed against CD antigens (CD45 and CD146). Flow cytometric analysis was performed using a FACS calibur flow cytometer (Becton–Dickinson) and CellQuest software. After characterization, subcultures of PLFs from seven different individuals were mixed and used for further experiments, where all experiments were carried out at passages 3–5.
Measurement of proliferation rates
We applied three different methods to measure the effects of COMP-Ang1 on viability and proliferation of PLFs. Initially, PLFs were divided onto 96-multiwell plates at the density of 10,000 cells/well and incubated in serum-free DMEM for 24 h. The cells were exposed to various concentrations (0–600 ng/ml) of COMP-Ang1 in DMEM supplemented with 10 % FBS for 72 h and then 10 μl of Cell Counting Kit-8 (CCK-8) solution (Dojindo Lab., Kumamoto, Japan) was added to the cultures. After incubation for additional-2 h, absorbance of the dye specific to CCK-8 was measured at 450 nm using a microplate reader (Molecular Devices, Austin, TX, USA). For BrdU incorporation assay, serum starved-PLFs for 24 h were incubated in DMEM containing 10 % FBS and COMP-Ang1 (0–600 ng/ml). After incubation for 48 h, cells were treated with 10 μM BrdU assay kit solution (Roche, Indianapolis, IN, USA) followed by additional-24 h incubation. Absorbance of the dye was measured at 370 nm using a microplate reader (Molecular Devices).The level of DNA synthesis in COMP-Ang1-exposed PLFs was also measured by adding 10 μCi of 3H-thymidine deoxyribose (TdR; Amersham Pharmacia Biotech, Inc., Piscataway, NJ, USA) to each well of 96-multiwell plates during the last 16 h of 72 h incubation. Cells were collected using a harvester (Inotech Inc., Dietikon, Switzerland), and beta emission from the 3H-TdR-incorporated cells was determined using a liquid scintillation counter (Packard Instrument Co., Downers Grove, IL, USA).
Reverse transcriptase-polymerase chain reaction (RT-PCR)
Total cellular RNA was extracted from PLFs using Trizol reagent following the manufacturer’s instructions (Invitrogen, Carlsbad, CA, USA). Total RNA (1 μg) was subjected to cDNA synthesis with SuperScript Reverse Transcriptase II and oligo12−18 primers (Invitrogen). Power SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA, USA) was used to detect the accumulation of PCR product during cycling with the ABI Step One plus sequence detection system (Applied Biosystems). The thermocycling conditions were as follows: predenaturation at 95 °C for 10 min, amplification using three-step cycles of denaturation at 95 °C for 15 s, annealing at 60 °C for 30 s, and extension at 72 °C for 30 s with 40 cycles. PCR products were run on a 1.5 % agarose gel and visualized with a UV illuminator. Oligonucleotide primers designed using primer express 3.0 (Applied Biosystems) were follows: 5′-CAA CGG ATT TGG TCG TAT TGG-3′ and 5′-GCC TTC TCC ATG GTG GTG AA-3′ for GAPDH (NM_002046.3), 5′-AAG GCG GAG GAG ACC TGC GCG-3′ and 5′-ATC GTG CGG CAT TGC GGC-3′ for cyclin D1 (NM_53056), and 5′-AGG GCC TAG AGC CTG AAA CAG-3′ and 5′-CCC TCC CCA ATC ACA TCT TG-3′ for Tie2 (NM_000459.3). These primers give a PCR product of 300, 381, and 400 bp, respectively.
Western blot analysis
Cell lysates were made in a NP-40 lysis buffer as described elsewhere [16]. Equal amounts (25 μg/sample) of protein extracts were separated by 12–15 % SDS-PAGE and blotted onto polyvinyl difluoride membranes. The blots were probed with primary antibodies overnight at 4 °C prior to incubation with secondary antibody in a blocking buffer for 1 h. The blots were developed with enhanced chemiluminescence (Amersham Pharmacia Biotech Inc.) and exposed on X-ray film (Eastman-Kodak Co., Rochester, NY, USA).
Cell cycle analysis
PLFs were incubated in serum-free DMEM for 24 h, and the cultures were replaced to new media containing 10 % FBS in the presence and absence of COMP-Ang1. After 48 h of incubation, cells were processed for propidium iodide (PI) staining as described elsewhere [17]. PI intensity in the cells (1 × 104 cells/sample) was analyzed using a FACS Calibur system (Becton–Dickinson) and cell cycle progression was determined using WinMDI program (version 2.9).
Small interfering (si) RNA transfection
PLFs were spread onto 60-mm culture dishes (4 × 105 cells per dish). When these cells reached 70–80 % confluence, the cultures were transfected with 50 nM Tie2 siRNA, c-Jun siRNA, or scrambled siRNA oligonucleotides using DharmaFECT 1 siRNA Transfection Reagent (Dharmacon, Lafayette, CO, USA) according to manufacturer’s instructions. After 48 h of transfection, cells were exposed to COMP-Ang1 and processed for further analyses.
Statistical analysis
All data are expressed as the mean ± standard deviation (SD). A one-way analysis of variance (ANOVA) followed by Scheffe’s test was used for multiple comparisons using SPSS program (version 12.0). Student t test was also used to determine significance differences between two sets of data. A value of p < 0.05 was considered statistically significant.
Results
Characteristics of human PLFs
As PLFs are a heterogeneous cell population, we analyzed surface molecules expressed in the cells using flow cytometer. Cultured PLFs showed adherent clonogenic cell clusters of fibroblast-like cells at 10 days post culture (Fig. 1a). The PLFs exhibited mostly positive staining for CD90 (99.7 ± 3.1 %) and CD105 (96.0 ± 3.5 %), while 45.9 ± 6.2 % of PLFs were positive to CD146 (Fig. 1b, c). However, almost of the PLFs showed negative staining for STRO-1 (1.0 ± 0.6 %) and CD45 (0.2 ± 0.3 %). When proliferation rate was determined by BrdU incorporation assay, PLFs had a high uptake rate of BrdU relatively at the early times of incubation (Fig. 1d).
Characterization of human PLFs. a PLFs showing a clonogenic formation at 10 days post culture with fibroblast-like morphology. b Flow cytometric characterization of cell surface markers. Isotype controls of PLFs are presented as filled red histograms, while the specific cell surface markers were as black open histograms. c The percentages of cells positively stained with each of surface marker antibodies were calculated using WinMDI 2.9 programs (n = 5). d Proliferating rate of cultured PLFs was measured at the indicated days after incubation using BrdU assay kit (n = 5)
COMP-Ang1 increases dose-dependently viability and proliferation of PLFs through Tie2-mediated signaling
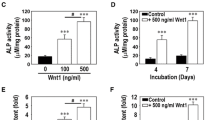
We examined the effects of COMP-Ang1 on viability and proliferation of PLFs. Measuring the optical density specific for CCK-8 (Fig. 2a) or BrdU (Fig. 2b) revealed that COMP-Ang1 increased viability and proliferation of PLFs in a dose-dependent manner. Based on these results, we selected the concentration of COMP-Ang1 at 300 ng/ml as the appreciate dose for subsequent experiments. We next explored the roles of Tie2 signaling pathway in COMP-Ang1-stimulated proliferation of PLFs. Transfecting the cells with si-Tie2 decreased the level of Tie2 protein as compared with the control (Fig. 2c). COMP-Ang1-mediated increase in the optical density specific for CCK-8 was significantly (p < 0.001) inhibited by silencing of Tie2 (Fig. 2d). Transfection itself with si-Tie2 did not reduce viability of PLFs. Knockdown of Tie2 also reduced the absorbance specific for BrdU in COMP-Ang1-exposed PLFs (data not shown). In addition, COMP-Ang1 increased the level of TdR incorporation in PLFs in a dose-dependent manner (Fig. 2e), and this increase was significantly (p < 0.01) diminished by knockdown of Tie2 (Fig. 2f).
COMP-Ang1 increases viability and proliferation of PLFs via Tie2-mediated signaling. PLFs were incubated for 72 h with the indicated concentrations of COMP-Ang1 and the absorbance of the dye specific to CCK-8 (a) or BrdU (b) was measured using a microplate reader. c PLFs were transfected with si-Tie2, and after 48 h of transfection, the cellular Tie2 levels were determined by Western blot analysis. PLFs were exposed to COMP-Ang1 after 48 h of transfection and CCK-8 (d) and TdR incorporation assays (e, f) were performed at 72 h post incubation. *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the untreated control cultures; ## p < 0.01 and ### p < 0.001 compared to COMP-Ang1 treatment alone (n = 7)
COMP-Ang1 stimulates cell cycle progression in PLFs
We examined whether COMP-Ang1-stimulated proliferation in PLFs is coupled with the changes in cell cycle progression. Treatment with COMP-Ang1 decreased proportion of cells in the G 0/G 1 phase but increased the migration of many cells into the S and G2/M phases (Fig. 3a, b). These changes in cell cycle progression were dependent on the concentrations of COMP-Ang1 added. Western blot analysis revealed that COMP-Ang1 affected differently the induction of cell cycle regulatory factors in PLFs; COMP-Ang1 (300 ng/ml) suppressed significantly the induction of p21Cip (p < 0.01) and p27Kip proteins (p < 0.01), while it augmented the protein levels of CDK4 (p < 0.01), CDK2 (p < 0.001), and cyclin D1 (p < 0.001) (Fig. 3c, d). Significant changes in the levels of cell cycle regulatory proteins were also shown when the cells were treated with 100 ng/ml COMP-Ang1. In contrary, there was no significant increase in cyclin E level in COMP-Ang1-exposed PLFs (Fig. 3d). To more understand the effect of Tie2 signaling on cell proliferation, PLFs transfected with si-Tie2 were exposed to 300 ng/ml COMP-Ang1 for 48 h and processed for Western blot and flow cytometric analyses. Tie2 knockdown restored the COMP-Ang1-mediated decreases in p21Cip and p27Kip protein levels similar to that of untreated control and reduced the level of cyclin D1 (Fig. 4a, b). In parallel with these results, knockdown of Tie2 diminished migration of cells into the S and G2/M phases with the subsequent increase in cell population present in the G0/G1 phase (Fig. 4c, d). The knockdown of Tie2 also inhibited COMP-Ang1-mediated increases in cyclin D1 mRNA expression (Fig. 5a) and CCK-8 uptake in PLFs (Fig. 5b). Similarly, treatment with native Ang1 at the same dose increased the cyclin D 1 expression and optical density specific for the CCK-8 in the cells, and these increases were almost completely inhibited by knockdown of Tie2.
COMP-Ang1 increases migration of cells into S and G2/M phases with increased induction of CDKs and cyclin D1 in PLFs. PLFs were exposed to the indicated concentrations of COMP-Ang1, and 48 h later, the cells were analyzed by flow cytometry after PI staining (a, b) and Western blotting (c, d). The cell cycle progression was determined using the WinMDI 2.9 program. Panel d shows the relative fold changes of cell cycle regulatory proteins after normalizing the levels to that of β-actin. *p < 0.05, **p < 0.01, and ***p < 0.001 compared to the untreated control cultures (n = 3)
Knockdown of Tie2 inhibits COMP-Ang1-stimulated cell cycle progression of PLFs with increased induction of p21Cip and p27Kip. At 48 h after transfection, PLFs were exposed to 300 ng/ml COMP-Ang1, and 48 h later, protein levels of p21Cip, p27Kip, and cyclin D1 (a, b) and cell cycle progression (c, d) were determined by Western blot and flow cytometric analyses, respectively. **p < 0.01 and ***p < 0.001 compared to the untreated control cultures; # p < 0.05 and ## p < 0.01 compared to COMP-Ang1 treatment alone (n = 3)
Native Ang1 mimics the effect of COMP-Ang1 on cyclin D1 induction and viability in PLFs, which is downregulated by knockdown of Tie2. PLFs transfected with si-Tie2 were treated with 300 ng/ml of native Ang1 or COMP-Ang1. a The levels of cyclin D1 mRNA were determined by RT-PCR at 24 h post incubation, while b viability of the cells was measured using CCK-8 solution after 72 h of incubation. ***p < 0.001 compared to the untreated control cultures; # p < 0.05 and ### p < 0.001 compared to native Ang1 or COMP-Ang1 treatment alone (n = 5)
COMP-Ang1 phosphorylates PI3K/Akt, MAPKs, and activator protein-1 (AP-1) subfamilies in PLFs
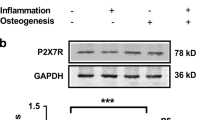
In order to verify the downstream mediators involved in COMP-Ang1-stimulated Tie2 signaling, we determined cellular levels of various protein kinases by Western blot analysis. The phosphorylated levels of Tie-2, Akt, ERK, JNK, c-Fos, and c-Jun were increased in COMP-Ang1-exposed PLFs (Fig. 6a). These increases were fast after treatment with COMP-Ang1 and, at most cases, were dose dependent (Fig. 6b). However, COMP-Ang1 did not increase the expression of Tie2 at a significant level (Fig. 6c, d). We next examined the roles of Tie2 on COMP-Ang1-activated MAPKs by silencing Tie2. Knockdown of Tie2 reduced significantly the levels of p-ERK (p < 0.001), p-JNK (p < 0.001), and p-p38 kinase (p < 0.01) similar to those of untreated controls (Fig. 7a, b). Silencing of Tie2 also suppressed the COMP-Ang1-stimulated phosphorylation of Akt and c-Jun in the cells (data not shown).
COMP-Ang1 treatment increases phosphorylation of Tie-2, Akt, MAPKs, and AP-1 subproteins in PLFs. a PLFs were exposed to COMP-Ang1 (0–300 ng/ml) and at the indicated times (0–60 min) after the exposure, phosphorylated levels of the indicated protein kinases were determined by immunoblotting. b Relative intensity of each of the phosphorylated kinases was calculated using a densitometer after normalizing those with whole proteins or β-actin. c, d PLFs were exposed to 300 ng/ml COMP-Ang1 and 24 h later, mRNA level of Tie2 was measured by RT-PCR. *p < 0.05, **p < 0.01, and ***p < 0.001 compared between the cultures exposed to 100 and 300 ng/ml COMP-Ang1 at the same incubation times; # p < 0.05, ## p < 0.01, and ### p < 0.001 compared with the incubation times at the same concentrations of COMP-Ang1 (n = 4)
Knockdown of Tie2 suppresses COMP-Ang1-stimulated phosphorylation of MAPKs in PLFs. a Control or si-Tie2-transfected PLFs were incubated with and without 300 ng/ml COMP-Ang1, and after 60 min of incubation, the levels of phosphorylated MAPKs were determined by immunoblotting. b Relative intensities of the phosphorylated MAPKs were calculated using a densitometer after normalizing the levels to that of β-actin. **p < 0.01 and ***p < 0.001 compared to the untreated control cultures; # p < 0.05 and ### p < 0.001 compared to the COMP-Ang1 treatment alone (n = 4)
PI3K/Akt and MAPK signaling pathways mediate COMP-Ang1-stimulated viability and proliferation of PLFs
To better understand the roles of PI3K/Akt and MAPKs in COMP-Ang1-exposed PLFs, the protein levels of p-Akt and p-c-Jun were determined after treatment with 300 ng/ml COMP-Ang1 in the presence and absence of each of the pharmacological inhibitors. Treatment with inhibitors specific to PI3K/Akt (LY294002 and Wortmannin) and ERK (PD98059), but not p38 kinase (SB203580) and JNK (SP600125), suppressed COMP-Ang1-mediated Akt phosphorylation (Fig. 8a). On the contrary, p–c-Jun levels were reduced only by treating PLFs with each inhibitor of MAPKs (Fig. 8b). All pharmacological inhibitors examined showed a significant inhibition on COMP-Ang1-stimulated incorporations of CCK-8 (Fig. 8c) and 3H-TdR in PLFs (Fig. 8d). Specifically, inhibitors of PI3K/Akt and ERK diminished COMP-Ang1-mediated increase in CCK-8 uptake more efficiently than did JNK or p38 kinase inhibitor (Fig. 8c). TdR incorporation increased by COMP-Ang1 was attenuated by inhibitors of MAPKs more than by PI3K/Akt inhibitors, where SP600125 inhibited at the most (Fig. 8d).
Effects of PI3K/Akt and MAPK inhibitors on the viability and proliferation in COMP-Ang1-exposed PLFs. PLFs were pretreated with the indicated concentrations of each PI3K/Akt or MAPK inhibitor for 2 h prior to the exposure of COMP-Ang1. Thirty minutes later, the levels of p-Akt and Akt (a) and p-c-Jun and c-Jun (b) in the cells were analyzed by Western blotting. These cells were also processed for the determination of viability (c) and TdR incorporation (d) at 72 h post exposure to each of the inhibitors. ***p < 0.001 compared to the untreated control cultures; # p < 0.05, ## p < 0.01, and ### p < 0.001 compared to the COMP-Ang1 treatment alone or between the indicated groups by a line (n = 5)
Knockdown of c-Jun inhibits COMP-Ang1-mediated increases in cyclin D1 induction and DNA synthesis by PLFs
To verify the roles of c-Jun in COMP-Ang1-stimulated proliferation, PLFs were transfected with si-c-Jun. Western blot analysis showed an apparent decrease in c-Jun and p-c-Jun protein after the transfection (Fig. 9a). Knockdown of c-Jun significantly attenuated the COMP-Ang1-mediated increases in DNA synthesis (Fig. 9b) and cyclin D1 induction to the levels similar to that of untreated controls (Fig. 9c, d). COMP-Ang1-mediated increase in proportion of cells in the G2/M phase was also disappeared by c-Jun knockdown (data not shown).
Knockdown of c-Jun inhibits COMP-Ang1-stimulated proliferation and cyclin D1 induction in PLFs. a At 48 h after transfection with si-c-Jun, PLFs were exposed to 300 ng/ml COMP-Ang1, and 30 min later, protein levels of c-Jun and p-c-Jun were determined by Western blotting. These cells were also processed for the analyses of TdR incorporation at 72 h post incubation (b) or for the determination of cyclin D1 levels by Western blotting at 48 h post incubation (c). Panel d indicates the fold changes of cyclin D1 after normalizing the levels to that of β-actin. ***p < 0.001 compared to the untreated control cultures; ## p < 0.01 compared to COMP-Ang1 treatment alone (n = 5)
Discussion
PLFs are able to regenerate PDL and thereby maintain the integrity and homeostasis of the PDL. This ability may be due to a stem cell-like property of PLFs to proliferate, differentiate, and migrate. Thus, we initially characterized cultured PLFs by determining the expression patterns of cell surface markers including CD45, CD90, CD, 105, CD146, and STRO-1. CD45, a type I transmembrane protein, is expressed mostly in differentiated hematopoietic cells and regulates a variety of cellular processes required for cell growth, differentiation, and mitosis [18]. CD90 has been used as a marker for stem-like cells as well as lymphocytes, mesangial cells, and fibroblasts [19]. CD105 has a crucial role in angiogenesis and thus in growth and survival of tumor cells and in the development and remodeling of the cardiovascular system [20]. CD146 is also used as a marker for MSCs isolated from multiple organs, and its expression is related positively with multipotency of stem cells [21]. Specifically, STRO-1, the best-known MSC marker, is currently used as a marker to isolate and identify PDLSCs [1, 22]. In this study, cultured PLFs exhibited highly positive staining for CD90, CD105, and CD146. The cultured PLFs also showed a clonogenic property at 10 days post incubation and a proliferating potential. Although the percentage of cells expressing STRO-1 was only about 1 %, our data suggest that the PLFs have in part stem cell-like characteristics such as PDLSCs and MSCs. It is important to note that number of PDLSCs present in PDL is quite less than PLFs and PDLSC’s multipotency is reduced timely according to the incubation time. Based on the stem-like property of PLFs and their abundance in the PDL, we consider that PLFs may be a beneficial target to stimulate the regeneration of PDL.
A variety of polypeptide growth factors have been studied for that they can facilitate the regeneration of periodontal tissues [23]. Growth factors are capable of modulating the cellular processes essential for proliferation, differentiation, and survival [24, 25]. We previously found that COMP-Ang1 promoted multiple cellular processes in bone marrow MSCs through the activation of Tie2-mediated signaling [13]. We have also shown that COMP-Ang1 enhances migration of PDLSCs into calvarial defect in an animal model [13] and facilitates proliferation as well as chondrogenic and osteogenic differentiation of MSCs [26]. These findings led us to postulate that COMP-Ang1 treatment improves the proliferative capacity of human PLFs. Our current data strongly support the ability of COMP-Ang1 to enhance survival and proliferation of PLFs.
It is commonly accepted that Ang1 regulates endothelial cell survival [27] and promotes endothelial differentiation from stem/progenitor cells [28]. Ang1 also protects MSCs against serum starvation and hypoxia-induced apoptosis [29]. It is important to consider that the Ang1-induced cell survival and proliferation is regulated tightly by Tie2-mediated signaling. Although native expression of Tie2 and its receptor differs among the origins of cells [10, 12], accumulated evidence has proven that the induction of Tie2 is essential for COMP-Ang1-stimulated proliferation, differentiation, and survival in stem-like cells [12, 13, 26]. The translocalization of Tie2 was also the main event in COMP-Ang1-stimulated angiogenesis and vascular enlargement [9, 30]. As proven by that Tie2 knockdown inhibited COMP-Ang1-mediated increases in the cellular uptake of CCK-8 and 3H-TdR, our results reveal the involvement of Tie2-mediated signaling in COMP-Ang1-enhanced viability and proliferation of PLFs.
The current findings highlight that COMP-Ang1-stimulated DNA synthesis in human PLFs is due to the migration of many cells into the S and G2/M phases. This study also shows that the decreases in p21Cip and p27Kip levels and the increases in cyclin D1, CDK2, and CDK4 may be the cellular events responsible for COMP-Ang1-stimulated cell cycle progression. In general, the transition of cells from G 0/G 1 to S or G 2/M phase depends on CDKs, which form complexes with cyclins [31, 32]. These complexes between CDKs and cyclins promote DNA synthesis by activating other downstream effectors [33, 34]. Upregulation of p21Cip and/or p27Kip negatively controls cell cycle progression by blocking the formation of CDK/cyclin complexes [35, 36]. These reports may suggest that COMP-Ang1-stimulated cell proliferation is more closely associated with downregulated expression of cell cycle inhibitors than other events. However, additional experiments are necessary to clarify the molecular mechanisms by which COMP-Ang1 regulates the expression of cell cycle regulator factors.
MAPKs regulate various cellular processes including survival, proliferation, migration, and differentiation [37–39]. MAPKs also control cell cycle progression by modulating the phosphorylation of cell cycle regulatory factors [38] and activate AP-1-mediated signaling by phosphorylating c-Jun and c-Fos proteins [40]. Akt is a serine/threonine-specific protein kinase and plays crucial roles in cell survival [41, 42]. Our results demonstrate that COMP-Ang1 stimulates phosphorylation of PI3K/Akt and MAPKs through the activation of Tie2-mediated signaling. Based on the current findings, we suggest that PI3K/Akt regulates predominantly survival of PLFs, while MAPKs stimulate cell proliferation through the activation of c-Jun-mediated signaling. The observation that knockdown of c-Jun prevented COMP-Ang1-stimulated DNA synthesis and cyclin D1 induction supports the involvement of c-Jun as the downstream effector of MAPKs. This result was in part consistent with a previous report showing that c-Jun activation is associated with proliferation and angiogenesis [43]. We also postulate that ERK-mediated signaling plays the dual modes of action on survival and proliferation, in that ERK inhibitor attenuated almost completely the cellular uptake of CCK-8 and 3H-TdR as well as the phosphorylation of Akt in COMP-Ang1-exposed PLFs. Taken as a whole, it is suggested that Tie2-mediated activation of PI3K/Akt and MAPK-c-Jun signaling pathways is to be the main mechanism involved in COMP-Ang1-enhanced viability and proliferation in PLFs.
In conclusion, the current study shows that human PLFs have stem cell-like characteristics and COMP-Ang1 treatment enhances viability and proliferation of the PLFs through Tie2-mediated activation of PI3K/Akt and MAPK-AP-1 signal transduction pathways (Fig. 10). As the proliferative capacity in PLFs is an important factor to maintain PDL functions, our results indicate a clinical usefulness of COMP-Ang1 in improving PDL integrity and homeostasis. More detail experiments will be needed to confirm whether COMP-Ang1 regenerates the PDL and protect PDL degradation against physiological and biological damages using animal models.
Proposed signaling pathways involved in COMP-Ang1-mediated increases in viability and proliferation in human PLFs. COMP-Ang1 activates PI3K/Akt and MAPKs through Tie2-mediated signaling in human PLFs. PI3K/Akt pathway may stimulate predominantly a signaling related to cell viability and survival, while MAPKs enhance cell proliferation by phosphorylating c-Jun
References
Nagatomo K, Komaki M, Sekiya I, Sakaguchi Y, Noguchi K, Oda S, Muneta T, Ishikawa I (2006) Stem cell properties of human periodontal ligament cells. J Periodontal Res 41:303–310
McCulloch CA, Bordin S (1991) Role of fibroblast subpopulations in periodontal physiology and pathology. J Periodontal Res 26:144–154
Sodek J, Limeback HF (1979) Comparison of the rates of synthesis, conversion and maturation of type I and type III collagens in rat periodontal tissues. J Biol Chem 254:10496–10502
Lekic P, McCulloch CA (1996) Periodontal ligament cell population: the central role of fibroblasts in creating a unique tissue. Anat Rec 245:327–341
Kim SY, Lee JY, Park YD, Kang KL, Lee JC, Heo JS (2013) Hesperetin alleviates the inhibitory effects of high glucose on the osteoblastic differentiation of periodontal ligament stem cells. PLoS One 8:e67504
Kook SH, Jeon YM, Park SS, Lee JC (2014) Periodontal fibroblasts modulate proliferation and osteogenic differentiation of embryonic stem cells through production of fibroblast growth factors. J Periodontol 85:645–654
Vogel G (2000) Cell biology. Stem cells: new excitement, persistent questions. Science 290:1672–1674
Wagers AJ, Weissman IL (2004) Plasticity of adult stem cells. Cell 116:639–648
Cho CH, Kammerer RA, Lee HJ, Steinmetz MO, Ryu YS, Lee SH, Yasunaga K, Kim KT, Kim I, Choi HH, Kim W, Kim SH, Park SK, Lee GM, Koh GY (2004) COMP-Ang1: a designed angiopoietin-1 variant with nonleaky angiogenic activity. Proc Natl Acad Sci USA 101:5547–5552
Jeong BC, Kim HJ, Bae IH, Lee KN, Lee KY, Oh WM, Kim SH, Kang IC, Lee SE, Koh GY, Kim KK, Koh JT (2010) COMP-Ang1, a chimeric form of angiopoietin 1, enhances BMP2-induced osteoblast differentiation and bone formation. Bone 46:479–486
Park BH, Yoon SJ, Jang KY, Kim MR, Lee HS, Kim KB, Park H, Lee SY, Park HS, Lim ST, Song KJ, Kim JR (2010) COMP-angiopoietin-1 accelerates bone formation during distraction osteogenesis. Bone 46:1442–1448
Kim S, Lee JC, Cho ES, Kwon J (2013) COMP-Ang1 accelerates chondrocyte maturation by decreasing HO-1 expression. J Cell Biochem 114:2513–2521
Kook SH, Lim SS, Cho ES, Lee YH, Han SK, Lee KY, Kwon J, Hwang JW, Bae CH, Seo YK, Lee JC (2014) COMP-angiopoietin 1 increases proliferation, differentiation, and migration of stem-like cells through Tie-2-mediated activation of p38 MAPK and PI3K/Akt signal transduction pathways. Biochem Biophys Res Commun 455:371–377
Lim SS, Kook SH, Bhattarai G, Cho ES, Seo YK, Lee JC (2015) Local delivery of COMP-angiopoietin 1 accelerates new bone formation in rat calvarial defects. J Biomed Mater Res Part A 103A:2942–2951
Kook SH, Son YO, Hwang JM, Kim EM, Lee CB, Jeon YM, Kim JG, Lee JC (2009) Mechanical force inhibits osteoclastogenic potential of human periodontal ligament fibroblasts through OPG production and ERK-mediated signaling. J Cell Biochem 106:1010–1019
Kook SH, Lee JC (2012) Tensile force inhibits the proliferation of human periodontal ligament fibroblasts through Ras-p38 MAPK up-regulation. J Cell Physiol 227:1098–1106
Kook SH, Son YO, Jang YS, Lee KY, Lee SA, Kim BS, Lee HJ, Lee JC (2008) Inhibition of c-Jun N-terminal kinase sensitizes tumor cells to flavonoid-induced apoptosis through downregulation of JunD. Toxicol Appl Pharmacol 227:468–476
Yasui T, Mabuchi Y, Toriumi H, Ebine T, Niibe K, Houlihan DD, Morikawa S, Onizawa K, Kawana H, Akazawa C, Suzuki N, Nakagawa T, Okano H, Matsuzaki Y (2016) Purified human dental pulp stem cells promote osteogenic regeneration. J Dent Res 95:206–214
Barry FP, Boynton RE, Haynesworth S, Murphy JM, Zaia J (1999) The monoclonal antibody SH-2, raised against human mesenchymal stem cells, recognizes an epitope on endoglin (CD105). Biochem Biophys Res Commun 265:134–139
Alvarez R, Lee HL, Wang CY, Hong C (2015) Characterization of the osteogenic potential of mesenchymal stem cells from human periodontal ligament based on cell surface markers. Int J Oral Sci 7:213–219
Melkerson-Watson LJ, Waldmann ME, Gunter AD, Zaroukian MH, Esselman WJ (1994) Elevation of lymphocyte CD45 protein tyrosine phosphatase activity during mitosis. J Immunol 153:2004–2013
Simmons PJ, Torok-Storb B (1991) Identification of stromal cell precursors in human bone marrow by a novel monoclonal antibody, STRO-1. Blood 78:55–62
Nagayasu-Tanaka T, Anzai J, Takaki S, Shiraishi N, Terashima A, Asano T, Nozaki T, Kitamura M, Murakami S (2015) Action mechanism of fibroblast growth factor-2 (FGF-2) in the promotion of periodontal regeneration in beagle dogs. PLoS One 10:e0131870
Yu Y, Bai F, Liu Y, Yang Y, Yuan Q, Zou D, Qu S, Tian G, Song L, Zhang T, Li S, Liu Y, Wang W, Ren G, Li D (2015) Fibroblast growth factor (FGF21) protects mouse liver against D-galactose-induced oxidative stress and apoptosis via activating Nrf2 and PI3K/Akt pathways. Mol Cell Biochem 403:287–299
Kim MS, Lee DY (2015) Insulin-like growth factor binding protein-3 enhances etoposide-induced cell growth inhibition by suppressing the NF-κB activity in gastric cancer cells. Mol Cell Biochem 403:107–113
Kim S, Lee JC, Cho ES, Kwon J (2013) COMP-Ang1 promotes chondrogenic and osteogenic differentiation of multipotent mesenchymal stem cells through the Ang1/Tie2 signaling pathway. J Orthop Res 31:1920–1928
Kim I, Kim HG, So JN, Kim JH, Kwak HJ, Koh GY (2000) Angiopoietin-1 regulates endothelial cell survival through the phosphatidylinositol 3-kinase/Akt signal transduction pathway. Circ Res 86:24–29
Joo HJ, Kim H, Park SW, Cho HJ, Kim HS, Lim DS, Chung HM, Kim I, Han YM, Koh GY (2011) Angiopoietin-1 promotes endothelial differentiation from embryonic stem cells and induced pluripotent stem cells. Blood 118:2094–2104
Liu XB, Jiang J, Gui C, Hu XY, Xiang MX, Wang JA (2008) Angiopoietin-1 protects mesenchymal stem cells against serum deprivation and hypoxia-induced apoptosis through the PI3K/Akt pathway. Acta Pharmacol Sin 29:815–822
Cho CH, Kim KE, Byun J, Jang HS, Kim DK, Baluk P, Baffert F, Lee GM, Mochizuki N, Kim J, Jeon BH, McDonald DM, Koh GY (2005) Long-term and sustained COMP Ang1 induces long-lasting vascular enlargement and enhanced blood flow. Circ Res 97:86–94
Jirawatnotai S, Aziyu A, Osmundson EC, Moons DS, Zou X, Kineman RD, Kiyokawa H (2004) Cdk4 is indispensable for postnatal proliferation of the anterior pituitary. J Biol Chem 279:51100–51106
Martin A, Odajima J, Hunt SL, Dubus P, Ortega S, Malumbres M, Barbacid M (2005) Cdk2 is dispensable for cell cycle inhibition and tumor suppression mediated by p27(Kip1) and p21(Cip1). Cancer Cell 7:591–598
Sherr CJ (1996) Cancer cell cycles. Science 274:1672–1677
Dzau VJ, Braun-Dullaeus RC, Sedding DG (2002) Vascular proliferation and atherosclerosis: new perspectives and therapeutic strategies. Nat Med 8:1249–1256
Sherr CJ, Roberts JM (1999) CDK inhibitors: positive and negative regulators of G1-phase progression. Genes Dev 13:1501–1512
Conqueret O (2003) New roles for p21 and p27 cell-cycle inhibitors: a function of each cell compartment? Trends Cell Biol 13:65–70
Ono K, Han J (2000) The p38 signal transduction pathway: activation and function. Cell Signal 12:1–13
Zhang W, Liu HT (2002) MAPK signal pathways in the regulation of cell proliferation in mammalian cells. Cell Res 12:9–18
Ryu CH, Park SA, Kim SM, Lim JY, Jeong CH, Jun JA, Oh JH, Park SH, Oh WI, Jeun SS (2010) Migration of human umbilical cord blood mesenchymal stem cells mediated by stromal cell-derived factor-1/CXCR4 axis via Akt, ERK, and p38 signal transduction pathways. Biochem Biophys Res Commun 398:105–110
Lee JC, Son YO, Pratheeshkumar P, Shi X (2012) Oxidative stress and metal carcinogenesis. Free Radic Biol Med 53:742–757
Peng SB, Peek V, Zhai Y, Paul DC, Lou Q, Xia X, Eessalu T, Kohn W, Tang S (2005) Akt activation, but not extracellular signal-regulated kinase activation, is required for SDF-1alpha/CXCR4-mediated migration of epithelioid carcinoma cells. Mol Cancer Res 3:227–236
Wang G, Ma N, Meng L, Wei Y, Gui J (2015) Activation of the phosphatidylinositol 3-kinase/Akt pathway is involved in lipocalin-2-promoted human pulmonary artery smooth muscle cell proliferation. Mol Cell Biochem 410:207–213
Vleugel MM, Greijer AE, Bos R, van der Wall E, van diest PJ (2006) c-Jun activation is associated with proliferation and angiogenesis in invasive breast cancer. 37:668–674
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (KRF) funded by the Ministry of Science, ICT and future Planning (NRF-2013R1A2A2A01967207).
Author information
Authors and Affiliations
Corresponding author
Additional information
Shin-Saeng Lim and Sung-Ho Kook have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lim, SS., Kook, SH. & Lee, JC. COMP-Ang1 enhances DNA synthesis and cell cycle progression in human periodontal ligament cells via Tie2-mediated phosphorylation of PI3K/Akt and MAPKs. Mol Cell Biochem 416, 157–168 (2016). https://doi.org/10.1007/s11010-016-2704-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-016-2704-3