Abstract
Introduction
Abortion law reforms have been hypothesized to influence reproductive, maternal, and neonatal health services and health outcomes, as well as social inequalities in health. In 2014, Mozambique legalized abortion in specific circumstances. However, due to challenges implementing the law, there is concern that it may have negatively influenced neonatal outcomes.
Methods
Using a difference-in-differences design, we used birth history data collected via the Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS) between 2004 and 2018 to assemble a panel of 476 939 live births across 17 countries including Mozambique. We estimated the effect of the abortion reform on neonatal mortality by comparing Mozambique to a series of control countries that did not change their abortion policies. We also conducted stratified analyses to examine heterogeneity in effect estimates by household wealth, educational attainment, and rural/urban residence.
Results
The reform was associated with an additional 5.6 (95% CI = 1.3, 9.9) neonatal deaths per 1,000 live birth. There was evidence of a differential effect of the reform, with a negative effect of the reform on neonatal outcomes for socially disadvantaged women, including those with no schooling, in poorer households, and living in rural areas.
Discussion
Given the delay in implementation, our analyses suggest that abortion reform in Mozambique was associated with an initial increase in neonatal mortality particularly among socially disadvantaged women. This may be due to the delay in effective implementation, including the dissemination of clear guidelines and expansion of safe abortion services. Longer-term follow-up is needed to assess the impact of the reform after 2018, when services were expanded. Abortion legal reform without adequate implementation and enforcement is unlikely to be sufficient to improve abortion access and health outcomes.
Significance
While abortion reforms have been hypothesized to affect a host of maternal and neonatal outcomes, few empirical studies have examined the effect of abortion reforms on neonatal outcomes.
AbstractSection What this Study AddsDue to challenges in the implementation of the 2014 abortion legalization in Mozambique, it may have negatively influenced neonatal outcomes, particularly for socially disadvantaged women. Abortion legalization alone without adequate implementation and enforcement is unlikely to be sufficient for substantial change in abortion access and health outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An estimated 25.1 million unsafe abortions occur each year, with 97% of these in low- and middle-income countries (LMICs) (Ganatra et al., 2017; Singh et al., 2018). An important factor regulating access to safe abortion in LMICs is abortion law (Arroyave & Moreno, 2018).
In July 2014, the Mozambique Parliament introduced legislation for the Voluntary Interruption of Pregnancy, which legalized abortion in some specific circumstances as part of a new penal code (Law No. 35/2014) (Assembleia da República, 2014). This law allowed abortion to be performed by a physician or other qualified health professional in approved health facilities in the first 12 weeks of pregnancy, with the consent of the pregnant woman. In cases of rape or incest, abortion was legalized during the first 16 weeks, and in cases of fetal anomaly it was made legal in the first 24 weeks.
Prior to this legislation, the nation’s criminal code, inherited from the Portuguese colonial code, established a punishment of 2–8 years of imprisonment for the provision or procurement of abortion unless the woman’s health or life was at risk (Agadjanian, 1998; Goçalves, 1972). However, a 1981 Ministry of Health (MOH) decree supported a broad interpretation of this risk and abortion was performed in designated public hospitals throughout the country (Gallo et al., 2004). During this period, abortion in Mozambique was regarded as quasi-legal due to the discrepancy between the written law and everyday practice (Agadjanian, 1998; Gallo et al., 2004; Rosário & Gianella, 2019).
When the law was passed in 2014, it cancelled the ministerial decree, but implementation was delayed and there were no clear guidelines for health facilities and providers (Rosário & Gianella, 2019). During the period between passing the law and the provision of implementation guidelines, providers refrained from performing abortion services due to confusion and lack of clarity around the policy guidelines, as well as fear of legal repercussions. Abortion services that had previously been available for specified fees were no longer officially provided (Ministério da Saúde, 2017; Rosário & Gianella, 2019).
Provision of abortion services started to improve in early 2018, following the publication and dissemination of Diploma Ministerial no. 60/2017 along with the clinical guidelines that defined standards for safe abortion for health facilities and providers, in parallel with training of health providers and community outreach work that publicized the registered health facilities offering abortion services (Ministério da Saúde, 2017).
Abortion reforms have been hypothesized to influence maternal and neonatal health services and health outcomes, as well as social inequalities in health (Clarke & Muhlrad, 2021; Mitrut & Wolff, 2011). Abortion access reduces the risk of unsafe abortions and provide women with an alternative to carrying unwanted pregnancies to term (Clarke & Muhlrad, 2021; Dott, 2010; Latt et al., 2019). On average, women who live where abortion is more accessible are also more likely to seek prenatal care, take folic acid or multivitamins, avoid consuming alcohol or illicit drugs, and follow clinical advice for reducing the risk of adverse maternal, fetal, and neonatal outcomes (Bahk, 2015; Delgado-Rodríguez et al., 1997; Dott, 2010).
Similarly, availability of legal and safe abortion services can mitigate the psychosocial stress and anxiety that often accompanies carrying unwanted pregnancy(Barton et al., 2017; Kantorová, 2020). Research suggests that women experiencing psychological stressors such as anxiety and depression during pregnancy have a higher risk of pregnancy complications such as pre-eclampsia and a higher risk of having adverse pregnancy and birth outcomes (Bahk, 2015; Gipson et al., 2008). Supplementary Fig. 1 shows a conceptual framework illustrating how abortion reforms might influence neonatal outcomes.
While abortion reforms have been hypothesized to affect a host of maternal and neonatal outcomes, most of the literature on the impact of abortions reforms has examined maternal outcomes. Few empirical studies have examined the effect of abortion legal reform on neonatal outcomes (Miller et al., 1988; Quick, 1978; Valente, 2017). A systematic review examining the effect of abortion reforms on health services and outcomes in LMICs found mixed evidence of an effect of abortion reform on neonatal outcomes (Ishola et al., 2021).
Abortion law reforms may have heterogeneous effects given that they take place in highly distinct political, economic, and social contexts (Johnson et al., 2018; Lavelanet et al., 2018). Delays in implementation and temporary restriction in access to abortion services following legal reforms designed to expand access may have negatively influenced neonatal outcomes in Mozambique.
In this study, we examined whether the 2014 abortion legal reform in Mozambique was associated with neonatal mortality using a difference-in-differences (DD) design.
Methods
Data Sources
We used data from the Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS) to measure neonatal mortality and other individual and household-level characteristics. The DHS and MICS are nationally representative household surveys that collect standardized health and demographic data, including information on birth histories, sexual and reproductive health, maternal and neonatal health, as well as other key socio-demographic characteristics such as household assets (Corsi et al., 2012; Khan & Hancioglu, 2019). The DHS employs a two-stage cluster sampling design, with the first stage selecting clusters and the second stage selecting households (Corsi et al., 2012). All women aged 15 to 49 who slept in the household the night before the survey were invited to complete a structured questionnaire. To ensure comparability, trained interviewers and standardized tools and methodologies are used. The MICS makes use of similar sampling procedures, methods, and measures to those employed by the DHS (Khan & Hancioglu, 2019). We utilized both the DHS and MICS to increase our sample size and the number of pre and post intervention time points in the intervention and control countries. This provided greater resolution for modeling pre-intervention trends in the outcomes and checks for violations of the parallel trends assumption. It also increases the precision of the estimated treatment effects.
Sample
We used harmonized DHS and MICS collected between 2004 and 2020. We included 17 potential control countries that did not implement changes to their abortion laws during this study period. These control countries were identified based on the following criteria: (i) a similar sub-Saharan classification to that of Mozambique as indicated in the World Bank Data Catalogue, (ii) at least two available DHS/MICS surveys, including at least one conducted prior to the abortion reform in Mozambique, and (iii) no evidence of significant reproductive health reforms during the study period that might have affected our primary outcome of interest.
Because DHS/MICS surveys were not available for Mozambique beyond 2018, our study period extended from 2004 to 2018. Our analytical sample comprised all live births to DHS/MICS respondents in this period, including 476 939 children born between 2004 and 2018 from 51 DHS/MICS surveys across 17 countries, including Mozambique. The DD design allowed us to disentangle the impact of the intervention from other confounding factors. Trends in neonatal mortality in the pre-reform period from 2004 to 2014 were approximately parallel for Mozambique compared to the potential control countries, suggesting that the parallel trends assumption necessary for the DD design to provide a valid estimate of the average treatment effect on the treated (ATT) was not violated (Strumpf E.C, Harper S, & Kaufman J.S, 2017). Supplementary Table 1 provides the survey years, birth years, and sample sizes for each country.
Measures
The exposure of interest was the adoption of a policy legalizing abortion in Mozambique in July 2014. Live births occurring in Mozambique prior to July 2014 were considered unexposed and those occurring in and after July 2014 were defined as exposed.
Our outcome variable was neonatal mortality which was measured by a binary indicator for whether a child who was born alive died within the first 28 days of life. Women interviewed in the DHS/MICS were asked to provide birth histories up to 5 years before the interview and those reporting a deceased child were asked to give the age at death. These data were used to construct a panel of live births by year of birth. We restricted to live births that occurred at least 29 days prior to the interview date to ascertain whether each child survived the neonatal period following birth. We included data on neonatal deaths occurring up to 5 years prior to the date of each survey to ensure uniformity across surveys and to minimize self-reporting errors.
Based on relevant literature, we included covariates associated with neonatal mortality in LMICs at the individual and household levels (Kayode, Ansah, Agyepong, & et al., 2014). We also included country-level characteristics that may be associated with changes to abortion policies and trends in neonatal mortality from the World Bank’s World Development Indicators and Global Development Finance databases. Additionally, we incorporated the polychoric dual-component household wealth index (P2C) as a substitute for the DHS wealth index (Martel et al., 2021). This index is more sensitive to key characteristics of rural wealth and is intended to account for the urban bias of the regular DHS approach.
Statistical Analysis
We used a linear probability model of the general form below:
where \(Y_{{ict}}\) represents the outcome for each observation \(i\) in country \(c\) in birth year \(t\). \(Policyct\)is a time-varying indicator for whether the birth occurred before or after the implementation of the abortion reform in Mozambique. Accordingly, \({\upbeta }1\) represents the effect of the reform on the probability of neonatal death on the risk difference scale. In the first model, we included fixed effects for country, \(\text{d}c\), and year, \(\text{g}t\), to account for, respectively, unobserved time-invariant confounders that vary across countries and shared temporal trends in neonatal mortality (Model 1). In the second model, we additionally adjusted for individual and household characteristics, represented by the vector \(Xict\)(Model 2). In the third model, we further controlled for time-varying country-level potential confounders, specifically per capita GDP, female labor force participation, and per capita total and government health expenditures, represented by the vector \(Zct\) (Model 3). The effects of the abortion law reform were therefore identified by changes in the probability of neonatal mortality in Mozambique (treated country) before and after its abortion law reform compared to corresponding changes in control countries that did not modify their policies during the study period. In addition, we conducted stratified analyses from the fully adjusted models to examine heterogeneity in effect estimates by household wealth, educational attainment and rural/urban residency. We used tests of homogeneity to provide statistical evidence of whether effects varied across strata. All three models incorporated respondent-level sampling weights to account for individual survey sampling designs. Per DHS guidelines, we applied the de-normalization of standard weights approach described in the DHS Sampling and Household Listing Manual (ICF International, 2012) to calculate an appropriate sampling weight for each observation in the analyses, using information on the number of women aged 15–49 years in each survey-year, available from the Population Division of the United Nations (Department for Economic and Social Affairs, 2013). We also estimated robust standard errors to account for clustering at the country level. We performed all analyses using Stata version 15 (StataCorp, 2016). Study data and code are available in the interest of reproducibility.
For sensitivity analyses, we first reported unweighted estimates to examine whether our results were sensitive to the inclusion of sampling weights. Second, we estimated the effect of the policy reform using a logistic regression model, with using post-estimation to estimate comparable marginal effects on the risk difference scale. Third, we examined whether the association between abortion reform and neonatal mortality varied by timing of exposure. We modified the exposure definition to include the estimated time of conception since births occurring after July 2014 may have been unaffected by the reform while in utero. Fourth, we added lead and lagged effect to examine whether there were delayed or persistent effects of the policy reform, as well as whether associations were observed prior to the implementation of the abortion reform.
Results
Table 1 shows the distribution of individual, household, and country level characteristics for treated and control countries prior to the implementation of the abortion law reform in Mozambique in 2014.
In the pre-intervention period, the rate of neonatal mortality was 28.7 per 1,000 live births. Trends in neonatal mortality in treated and control countries were stable in the pre-intervention period, with an increase in neonatal mortality in Mozambique after the abortion legal reform (Fig. 1). Supplementary Fig. 2 shows similar pre-intervention trends in neonatal mortality for treated and control countries.
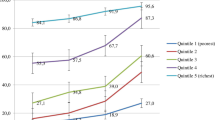
Table 2 provides estimates of the effect of the abortion legal reform on the probability of neonatal death. In the fully adjusted model (Model 3), the reform was associated with an additional 5.6 (95% Confidence Interval (CI) = 1.3, 9.9) neonatal deaths per 1,000 live births. Figure 2 shows the differential association between abortion legal reform and neonatal mortality by household SES, educational attainment and rural/urban residence (Supplementary Table 2).
Results from sensitivity analyses are shown in Supplementary Table 3. The effects of abortion legal reform on neonatal mortality were relatively robust. When logistic models were used, the reform was associated with a comparable increase in neonatal mortality of 6.8 (95% CI = 2.2, 11.4) deaths per 1,000 live births (Model A). The association between the reform and neonatal mortality was similar in unweighted and weighted models, with unweighted estimates showing an additional 5.8 (95% CI = 2.2, 9.3) neonatal deaths per 1,000 live births (Model B). When we varied the timing of exposure to include time of conception, the reform was associated with an increase of 6.4 (95% CI = 3.8, 9.0) neonatal deaths per 1,000 live births (Model C). In the analysis of dynamic effects, the reform was associated with lagged effects on neonatal mortality, however, the lead effects were closer to the null (Model D).
Discussion
We used samples of 467 303 live births in 17 LMICs recorded in DHS/MICS surveys between 2004 and 2018 to evaluate the effect of abortion legal reform in Mozambique on neonatal mortality. Our analyses suggest that abortion legal reform was associated with an additional 5.6 (95% CI = 1.3, 9.9) neonatal deaths per 1,000 live births, and that the reform had an adverse impact specifically among socially disadvantaged groups. These findings were robust to alternative model specifications.
Policies legalizing abortion are expected to increase access to safe abortion, decrease unintended pregnancies and ultimately improve maternal and neonatal outcomes (Kantorová, 2020; Miller et al., 1988). Nonetheless, evidence on the relationship between abortion legalization and neonatal outcomes is mixed. Studies have reported reductions in neonatal mortality and improvements in birth outcomes such as birthweight following abortion legalization in Romania Oregon and New York State (Lanham et al., 1974; Mitrut & Wolff, 2011; Quick, 1978). In contrast, an effect of abortion legalization on neonatal outcomes was not detected in other studies, including evaluations of reforms in Nepal and Uruguay (Antón et al., 2018; Valente, 2017). Our results indicate that due to the delay in implementation, abortion legal reform in Mozambique may be associated with an initial increase in neonatal mortality.
Although reforms to legalize abortion are intended to improve access, ineffective implementation and enforcement may result in unintended consequences (Oberman, 2021). Abortion legislation that fails to reflect and anticipate how liberalized grounds for abortion will be established may deter medical practitioners from promptly delivering care to eligible women (Dickens et al., 2007). Several recent decisions of international human rights courts address governmental duties regarding implementation of abortion laws including prompt access to safe and quality abortion care (Dickens et al., 2007).
The quasi-legal status of abortion in Mozambique prior to the abortion reform made abortion partially accessible through designated public hospitals under the discretion of hospital directors (Agadjanian, 1998; Gallo et al., 2004). However, following the 2014 abortion reform, poor implementation, including a delay in disseminating clear guidelines and expanding safe abortion services may have initially reduced access to safe abortion and led to an increase in neonatal death. Comprehensive abortion care, clinical standards and guidelines for health facilities and providers were disseminated only at the end of 2017. Services only started to be rolled out slowly across the country thereafter in 2018 (Rosário & Gianella, 2019). For example, in Tete province, the third most populous province, services were initiated in 6 of 15 districts in 2019, are currently only provided in approximately half of districts. Services are also generally still only provided in district hospitals and not in rural health facilities (Rosário & Gianella, 2019).
In a study describing abortion procedures and exploring factors influencing the abortion decision-making process among young women who had undergone induced abortion in Mozambique following legal reform, none of the participants had followed a legal procedure to obtain abortion and half had received abortion outside of health facilities (Frederico et al., 2020). Women cited lack of knowledge about the new abortion law and lack of legal abortion services. This research highlights the importance of clarifying and informing women and providers of their legal entitlements and ensuring that abortion services are available in all circumstances described in the law.
It is possible that other contextual changes in Mozambique that coincided with the abortion legal reform, may have contributed to the observed increase in neonatal mortality. For example, in 2016, the discovery of illegal debt incurred by the Mozambican government triggered a period of fiscal and monetary instability and the withdrawal of external aid, including to the health sector, that forced the government to reduce public spending severely and led to huge cuts in public services including health services, and consequently may have contributed to reduced service access and quality and increased adverse health outcomes including NMR (Costs And Consequences of the Hidden Debt Scandal of Mozambique, 2021).
Furthermore, our analyses showed heterogeneity in the effect of abortion legal reform on neonatal mortality in Mozambique. Socially disadvantaged women, including those in households with fewer assets, residing in rural areas and who did not complete secondary school, experienced poorer neonatal outcomes following abortion legal reform, whereas there was no effect of the reform among their less disadvantaged counterparts. Some studies have examined how abortion legalization affected socioeconomic groups differentially (Frederico et al., 2020; Grossman & Jacobowitz, 1981; Joyce, 1987). Following the abortion legal reform in Mozambique, Frederico et al. (Frederico et al., 2020) reported that only people with a certain level of education, income and a sufficiently large social network could access legal and safe abortion procedures. It is possible that the reform further worsened the existing inequities in maternal and newborn health through unequal access to safe abortion services for disadvantaged women and girls.
There may be a differential effect of the reform based on country regions (Northern, Central, and Southern) and religious affiliation. The importance and implication of religion may differ across different segments of the society. Some studies have emphasized the association between women’s autonomy and religious affiliation in Mozambique (V. Agadjanian & Yabiku, 2015; Daca, Sebastian, Arnaldo, & et al., 2020). However, we lacked data by province, and we were unable to compare effect across regions.
There were limitations to our study. First, our study period does not capture the period after clinical guidelines and standards for professionals and health facilities were widely accessible. Longer-term impacts of the abortion reform on sexual and reproductive health outcomes warrants further investigation, as we would expect to see improvements in access to safe abortion services only after the introduction of guidelines and training that began in 2018. Second, there is the potential for unmeasured confounding. While the DD design accounts for “fixed” (non time-varying) differences across countries, as well as shared temporal trends in the outcome, and allows us to disentangle the impact of the intervention from other confounding factors, we also accounted for individual and household characteristics, controlled for potential confounding by country-level covariates. Nonetheless, there may have been other unmeasured changes, including other policy changes, that coincided with the timing of the abortion reform in Mozambique and influenced our outcomes of interest. Third, measurement of neonatal mortality is subject to underreporting or misclassification since it depends on maternal recall. This may bias our estimates if such underreporting or misclassification were different between treated and control countries. Finally, generalisation of our results should be done cautiously, as results may vary for countries with different political, cultural, religious, and sociodemographic contexts vis-à-vis Mozambique.
While acknowledging the limitations in this study, our analyses suggest that abortion reform in Mozambique was associated with an increase in neonatal mortality, particularly for socially disadvantaged women. This may be due to the delay in provision of clear guidelines and implementation of safe abortion services. Abortion legalization alone may be insufficient for substantial change in abortion access and health outcomes without effective implementation and enforcement. A longer follow up is needed to assess if the immediate adverse effect of the reform was later reversed. Further research is also needed to understand how constraints to implementation and enforcement of abortion reforms affect access to abortion services.
Data Availability
We utilized the Demographic and Health Surveys (DHS) and UNICEF Multiple Indicator Cluster Surveys (MICS). Both are publicly available, but users must first register. Registration, which requires a summary of the proposed study and selection of country datasets, can be completed at: https://dhsprogram.com/data/new-user-registration.cfm and https://mics.unicef.org/visitors/sign-up respectively
Code Availability
Code for data analysis is available upon request from the corresponding author
References
Agadjanian, V. (1998). Quasi-legal Abortion Services in a sub-saharan setting: Users’ Profile and motivations. International Family Planning Perspectives, 24(3), 111–116.
Agadjanian, V., & Yabiku, S. T. (2015). Religious belonging, Religious Agency, and women’s autonomy in Mozambique. Journal for the Scientific Study of Religion, 54(3), 461–476.
Antón, J. I., Ferre, Z., & Triunfo, P. (2018). The impact of the legalisation of abortion on birth outcomes in Uruguay. Health Economics, 27, 1103–1119.
Arroyave, F. A. B., & Moreno, P. A. (2018). A systematic Bibliographical Review: Barriers and facilitators for Access to Legal Abortion in Low and Middle Income Countries. Open Journal of Preventive Medicine, 8(5), 147–168.
Assembleia da República (2014). Boletim da República: Lei n°. 35/2014 de 31 de Dezembro, vol. I Série n. Maputo: 14° Suplemento Imprensa; 2014 i>https://www.wlsa.org.mz/wp-content/uploads/2017/11/Diploma_Ministerial_60-2017.pdf Accessed 19 February 2021. Retrieved from
Bahk, J., Yun, S. C., & Kim, Y. (2015). Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the Panel Study on Korean Children (PSKC). BMC pregnancy and childbirth, 15(85), 1–12.
Barton, K., Redshaw, M., Quigley, M. A., & Carson, C. (2017). Unplanned pregnancy and subsequent psychological distress in partnered women: A cross-sectional study of the role of relationship quality and wider social support. Bmc Pregnancy and Childbirth, 17(1), 44. https://doi.org/10.1186/s12884-017-1223-x.
Clarke, D., & Muhlrad, H. (2021). Abortion laws and women’s health. Journal of Health Economics, 76, 102413. https://doi.org/10.1016/j.jhealeco.2020.102413.
Corsi, D. J., Neuman, M., Finlay, J. E., & Subramanian, S. V. (2012). Demographic and health surveys: A profile. International Journal of Epidemiology, 41(6), 1602–1613. https://doi.org/10.1093/ije/dys184.
Costs and consequences of the hidden debt scandal of Mozambique. (2021). Retrieved from Centro De Integridade Pública (CIP), Moçambique, and Chr. Michelsen Institute, Norway.
Daca, C., Sebastian, M. S., & Arnaldo, C. (2020). Socio-economic and demographic factors associated with reproductive and child health preventive care in Mozambique: a cross-sectional study. International Journal for Equity in Health, 19(200), 1–9.
Delgado-Rodríguez, M., Gómez-Olmedo, M., Bueno-Cavanillas, A., & Gálvez-Vargas, R. (1997). Unplanned pregnancy as a major determinant in inadequate use of prenatal care. Preventive Medicine, 26(6), 834–838.
Department for Economic and Social Affairs (2013). World population prospects: the 2012 revision. Retrieved from United Nations Secretariat.
Dickens, B., Cook, R., & Erdman, J. (2007). Achieving transparency in implementing abortion laws. International Journal of Gynecology and Obstetrics, 99, 157.
Dott, M., Rasmussen, S. A., Hogue, C. J., et al. (2010). Association between Pregnancy Intention and Reproductive-health related behaviors before and after pregnancy recognition, National Birth defects Prevention Study, 1997–2002. Maternal and Child Health Journal, 14, 373–381.
Frederico, M., Arnaldo, C., Decat, P., Juga, A., Kemigisha, E., Degomme, O., & Michielsen, K. (2020). Induced abortion: A cross-sectional study on knowledge of and attitudes toward the new abortion law in Maputo and Quelimane cities, Mozambique. Bmc Women’s Health, 20(1), 129. https://doi.org/10.1186/s12905-020-00988-6.
Gallo, M. F., Gebreselassie, H., Victorino, M. T., Dgedge, M., Jamisse, L., & Bique, C. (2004). An assessment of abortion services in public health facilities in Mozambique: Women’s and providers’ perspectives. Reproductive Health Matters, 12(24 Suppl), 218–226. https://doi.org/10.1016/s0968-8080(04)24027-7.
Ganatra, B., Gerdts, C., Rossier, C., Johnson, B. R., Tuncalp, O., Assifi, A., & Alkema, L. (2017). Global, regional, and subregional classification of abortions by safety, 2010-14: Estimates from a bayesian hierarchical model. Lancet, 390(10110), 2372–2381. https://doi.org/10.1016/S0140-6736(17)31794-4.
Gipson, J. D., Koenig, M. A., & Hindin, M. J. (2008). The effects of unintended pregnancy on infant, child, and parental health: A review of the literature. Studies in Family Planning, 39(1), 18–38. https://doi.org/10.1111/j.1728-4465.2008.00148.x.
Goçalves, M. (1972). Portuguese criminal code, with annotation and Commentary. Editora Almedina. (in Portuguese).
Grossman, M., & Jacobowitz, S. (1981). Variations in infant mortality rates among counties of the United States. Demography, 18(4), 695–713.
ICF International. (2012). Demographic and Health Survey sampling and household listing manual. Maryland: ICF International.
Ishola, F., Ukah, U. V., Alli, B. Y., & Nandi, A. (2021). Impact of abortion law reforms on health services and health outcomes in low- and middle-income countries: A systematic review. Health Policy Plan, 36(9), 1483–1498. https://doi.org/10.1093/heapol/czab069.
Johnson, B. R., Lavelanet, A. F., & Schlitt, S. (2018). Global abortion policies database: A new approach to strengthening knowledge on laws, policies, and human rights standards. BMC International Health and Human Rights, 18, ARTN35.
Joyce, T. (1987). The Impact of Induced Abortion on Black and White Birth Outcomes in the United States. Demography, 24(2), 229–244.
Kantorová, V. (2020). Unintended pregnancy and abortion: What does it tell us about reproductive health and autonomy. Lancet Glob Health, 8(9), 1106–1107.
Kayode, G. A., Ansah, E., & Agyepong, I. A. (2014). Individual and community determinants of neonatal mortality in Ghana: a multilevel analysis. Bmc Pregnancy And Childbirth, 14(165), 1–12.
Khan, S., & Hancioglu, A. (2019). Multiple Indicator cluster surveys: Delivering Robust data on children and women across the Globe. Studies in Family Planning, 50(3), 279–286.
Lanham, J. T., Kohl, S. G., & Bedell, J. H. (1974). Changes in pregnancy outcome after liberalization of the New York State abortion law. American Journal of Obstetrics and Gynecology, 118(4), 485–492. https://doi.org/10.1016/s0002-9378(16)33688-2.
Latt, S. M., Milner, A., & Kavanagh, A. (2019). Abortion laws reform may reduce maternal mortality: an ecological study in 162 countries. BMC Women’s Health, 19(1), 1–9.
Lavelanet, A. F., Schlitt, S., Johnson, B. R., & Ganatra, B. (2018). Global abortion policies database: A descriptive analysis of the legal categories of lawful abortion. BMC International Health and Human Rights, 18, ARTN44.
Martel, P., Mbofana, F., & Cousens, S. (2021). The polychoric dual-component wealth index as an alternative to the DHS index: Addressing the urban bias. J Glob Health, 11, 04003.
Miller, M. K., Stokes, C. S., & Warland, R. H. (1988). The effect of legalization and Public Funding of abortion on neonatal mortality: An intervention analysis. Population Research and Policy Review, 7(1), 79–92.
Ministério da Saúde (2017). Boletim da República: Diploma Ministerial n°. 60/2017 de 20, vol. I Série n. Maputo: de Setembro; 2017. p. 147. http://www.wlsa.org.mz/wp-content/../Diploma_ministerial_60-2017.pdf. Accessed 17 Feb 2021.
Mitrut, A., & Wolff, F. C. (2011). The impact of legalized abortion on child health outcomes and Abandonment. Evidence from Romania. Journal of Health Economics, 30, 1219–1231.
Oberman, M. (2021). How Abortion Laws Do and Don’t Work. Law, Gender & Society, 36, 163.
Quick, J. D. (1978). Liberalized abortion in Oregon: Effects on Fertility, Prematurity, fetal death, and infant death. American Journal of Public Health, 68(19), 1003–1008.
Rosário, C., & Gianella, C. (2019). Evolução histórico-legal do processo de despenalização do aborto em Moçambique – períodos-chave na extensão do direito ao aborto. In A. Carlos, B. M. Cau, B. Chilundo, J. J. Picardo, & S. Griffin (Eds.), Planeamento Familiar e Políticas de Saúde Sexual e Reprodutiva em Moçambique (pp. 259–279). Madrid: CEPSA.
Singh, S., Remez, L., Sedgh, G., Kwok, L., & Onda, T. (2018). Abortion Worldwide 2017: Uneven Progress and Unequal Access. Washington, DC: Guttmacher Institute.
StataCorp. (2016). Stata Statistical Software: Release 15. College Station. Texas: StataCorp LP.
Strumpf, E. C., Harper, S., & Kaufman, J. S. (2017). In Methods in, & Social Epidemiology (Eds.), Fixed effects and difference in differences. Jossey-Bass.
Valente, C. (2017). Improved access to abortion, neonatal mortality, and gender bias: Evidence from Nepal. Economic and Social Research Council.
Funding
Funds for this project were provided by the Fonds de recherche du Québec—Santé (FRQS) PhD scholarship (FI) and a Canadian Institute of Health Research (CIHR) Foundation grant (FRN 148467) (AN).
Author information
Authors and Affiliations
Contributions
FI and AN contributed to the study conception and design, FI performed data collection and analysis and wrote the first draft of the manuscript. AN, CR, SG, and CK contributed to the writing of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Ethical Approval
This study used de-identified, publicly available secondary data. The DHS data collection procedures were reviewed and approved by the ICF Institutional Review Board (IRB). The MICS survey responds to local regulations and protocols regarding data collection and fieldwork. Each survey is approved by the relevant country-specific ethical review board that oversees research studies on human subjects in each of the participating countries.
Consent to Participate
Not Applicable.
Consent for Publication
Not Applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishola, F., Rosario, C., Griffin, S. et al. Abortion Legal Reform and Neonatal Mortality in Mozambique. Matern Child Health J 28, 587–595 (2024). https://doi.org/10.1007/s10995-023-03876-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03876-1