Abstract
Background
Neonatal deaths remain a serious public health concern in Ethiopia; being one of the top five countries contributing to half of the neonatal deaths worldwide. Although antenatal care (ANC) is assumed as one of the viable options that contribute to neonatal survival, findings from original studies indicated disparities in the effect of ANC on neonatal mortality. Thus, this review aimed to determine the pooled effect of ANC on neonatal mortality in Ethiopia.
Methods
Databases such as PubMed, EMBASE, CINAHL, HINARI, and Cochrane Central Library were searched for articles using keywords. Selection of eligible articles and data extraction were conducted by an independent author. The risk of a bias assessment tool for non-randomized studies was used to assess the quality of the articles. Comprehensive meta-analysis version 2 software was used for meta-analysis. Heterogeneity and publication bias of included studies were assessed using I2 test statistic and Egger test, respectively. The random-effect model was employed; an outcome is reported using a risk ratio with a 95% confidence interval.
Results
Of 28 included studies, 20 showed receiving at least one ANC visit had a significant association with neonatal mortality. Accordingly, the estimated pooled risk ratio for neonatal mortality was 0.59 (95% CI 0.45, 0.77) among infants born to women who had at least one ANC visit compared to infants born to women who had no ANC visits.
Conclusion
This finding indicated that neonatal mortality was decreased among infants born to women who had at least one ANC visit compared to infants born to women who had no ANC visit. Therefore, promoting and strengthening ANC service utilization during pregnancy would accelerate the reduction of neonatal mortality in Ethiopia.
Significance
In some studies, providing ANC services reduces the risk of neonatal mortality, in others, the ANC visits did not significantly decrease neonatal mortality in Ethiopia, which represents a dismal picture of neonatal mortality (NM) in sub-Saharan Africa (SSA) region. Therefore, evidence emanated from comprehensive searches of review performed with several studies represented from various regions of the country which determine the effect of ANC on NM is essential to reinforce strategies that could help for newborn survival and wellbeing of neonates in Ethiopia. Hence, this study aimed to systematically examine the effect of ANC on NM by combining a wide range of reviews, to provide concrete evidence for policymakers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The universally accepted neonatal period is birth to the first 28 days of life and is the time in which the child is most vulnerable to death (United Nations Children’s Fund, 2019). The neonatal mortality (NM) rate is calculated using the number of deaths per 1000 live births in a given period (WHO, 2005). Globally, an estimated 5.4 million under-five deaths were reported in 2017 and of which around 2.5 million of them died in the first month of life; contributing to 47% of under-five deaths (United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2017; World Health Organisation, 2019). Neonatal mortality is an urgent public health concern with about 6,500 neonatal deaths every day around the globe. Surprisingly, more than 80% of neonates are suffering from preventable causes of death (United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2018; WHO, 2016a). Although the world has made significant improvements in reducing childhood mortality (United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2018), remarkable disparities have been observed in reduction among high, and low-middle-income countries (LMICs) (United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2017; World Health Organization, 2019). And, the trend for NM contribution to under-five mortality is persistently high since the inception of the millennium development goals; 31% in 1990, and 41% in 2018 (Lopez, 2014; Mejía-Guevara et al., 2019; Tekelab et al., 2019a, 2019b).
The highest number of NM occurred in Sub-Saharan Africa (SSA) and South Asia countries each accounting for 39% and 38%, respectively (United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2019). The SSA countries have the highest rate (27 per 1000 live births) of NM worldwide and from the top 10 countries contributing to NM rates in the world, eight countries are located in this region (Jena et al., 2020; United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2017). Despite significant progress in maternal and child mortality, neonatal health problems remained part of the unfinished agenda in many East African countries, including Ethiopia (Abate et al., 2020; Gebremedhin et al., 2016). In Ethiopia, there are high proportions of neonatal deaths; being one of the top ten countries prominently affected by NM, and is one of the top five countries contributing to half of NM in the globe (Jena et al., 2020; Wright, 2014).
In an attempt to reduce the high toll of NM (Berhan & Berhan, 2014; Jena et al., 2020), the government of Ethiopia developed a National Newborn and Child Survival Strategy which also help to accelerate the achievement of the sustainable development goal (SDG) target 3.2 for ending preventable neonatal deaths or stillbirths to as few as 12 per 1000 live or total births (UN-DESA, 2017). Addressing this goal would save the lives of 5 million newborns from 2018 to 2030 (Hug et al., 2019; United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2018; WHO Press Release, 2017). However, current trends showed more than 60 countries, including Ethiopia will miss this target (United Nations Inter-agency Group for Child Mortality Estimation (UNIGME), 2018). Therefore, attaining ambitious survival goals needs ensuring universal access to safe, effective, high-quality, and affordable care for women and children (WHO, 2015a). More importantly, in Ethiopia, the decline of NM remained stagnant; according to the mini Ethiopian demographic health survey (EDHS) 2019 report, the NM rate was 30 per 1000 live births; NM is the highest in the world and the country continues to suffer from the steepest reduction of odds of neonatal survival in the world (Ethiopian Public Health Institute ICF, 2019).
Effective and timely maternal health care services before conception, during pregnancy, and childbirth could save nearly 3 million newborns in high-burden countries (Tekelab et al., 2019a, 2019b). Antenatal care is recognized as one of the fundamental strategies to reduce stillbirth and NM irrespective of the socio-demographic background (Arunda et al., 2017; Gregory et al., 2016; Lambon-Quayefio & Owoo, 2014; Mohamed et al., 2016; Singh et al., 2014; WHO, 2015b). It is an ideal entry point for maternal and neonatal health care to ensure access to several health care interventions (Ibrahim et al., 2012; Raatikainen et al., 2007; WHO, 2016c). An estimated 10–20% of NM is averted by the provision of ANC services (Darmstadt et al., 2005; WHO, 2009); although the focused ANC model which was developed in the 1990s is associated with more perinatal deaths than the 2016 world health organization (WHO) positive pregnancy experience ANC model (WHO, 2016b, 2016c).
A systematic review and meta-analysis performed in SSA reported that ANC utilization contributed to the reduction of NM (Tekelab et al., 2019a, 2019b). However, the study does not include adequate primary studies from Ethiopia and its effect was not evaluated in the context of Ethiopia; indeed, there is variation in the practice of maternal health services. In Ethiopia, some studies found that the risk of NM is reduced in births of women with at least one ANC visit compared to no ANC visit (Alebel et al., 2020; Debelew et al., 2014; Kidus et al., 2019; Orsido et al., 2019; Worku et al., 2012) whereas others found no relationship between having an ANC visit and NM (Demisse et al., 2017; Elmi Farah et al., 2018; Wakgari & Wencheko, 2013; Worku et al., 2014). Hence the reported disparities in the effect of ANC on neonatal outcomes in these fragmented studies call for the importance of having robust evidence emanated from several primary studies, representing the various geographical area of the country. Therefore, in Ethiopia where there is a high proportion of NM, the availability of strong abridged evidence on the effect of ANC on NM would offer reliable evidence for policymakers to critically reinforce the ANC program and design optimal ANC service.
Methods
The present systematic review and meta-analysis methodology was prepared following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist (Moher et al., 2015).
Eligibility Criteria
The eligibility criteria for this systematic review and meta-analysis include observational (cross-sectional, case–control, and cohort) studies with the following criteria: (i) the studies that included women who gave birth without any specific risk factors; (ii) the studies were conducted in the perinatal period provided that if the studies differentiate early neonatal death as the death of neonate with in the first seven days and neonatal mortality was defined a death during the first 28 days of life; (iii) studies that reported the risk of perinatal or neonatal mortality; (iv) the ANC utilization was considered as possible factors/exposure for neonatal mortality; and (v) the article is published in the English language. However, articles that focus on the number of ANC visits to determine NM (i.e., without yes/no response for ANC visit) were excluded from the meta-analysis. Further, studies emanated from review, commentary, editorials, fact sheets, and policy briefs were not included in the analysis.
PICO
- Population::
-
live birth neonates.
- Intervention::
-
neonates born to women who utilized at least one ANC visit.
- Comparison::
-
neonates born to women who did not utilize at least one ANC visit.
- Outcome::
-
neonatal mortality.
Information Sources and Search Strategy
Searching of PubMed, EMBASE, CINAHL, and HINARI databases were carried out from January 1990 to June 2020. We reasonably selected the year of publication (1990) as focused antenatal care has been implemented since 1990. We also retrieved records through the Cochrane Central library and Google Scholar. Searching was performed using the following key/Medical Subject Heading (Mesh) terms: “Antenatal care”, “prenatal care”, “obstetrics”, “pregnancy care”, “maternity care” “maternal health services”, “perinatal mortality”, “neonatal mortality”, “neonatal death”, “newborn death”, “Ethiopia” (Table S1).
Study Selection
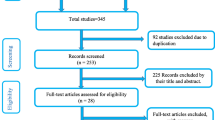
The selection of the studies involved three steps. First, duplicates were removed and eligible articles were screened based on their title and abstract by two authors (GT and KS) independently. Second, full-text studies were evaluated based on the predetermined inclusion criteria. Third, the methodological quality appraisal was performed for studies that met the inclusion criteria. Any disparity between the two reviewers was resolved through discussion and common consensus. Overall, preferred reporting items for systematic reviews and meta-analysis flow chart was used to record the selection process of the studies (Fig. 1).
Data Extraction
The data extraction template was prepared using an excel sheet. The authors read all included studies in detail to extract pertinent data for the review based on first author, year of publication, study setting, study design, sample size, number of dead neonates and survivors among ANC attendants, and number of dead neonates and survivors among non-ANC attendants (Table1).
Measurement
An outcome variable (NM) was defined as the death of the neonate within the first four weeks (28 days) of life (Lander, 2006). The presence or absence of an ANC visit was used as an exposure variable. Antenatal care visit refers to a woman's pregnancy checkup once or more from a health facility that is given by a skilled attendant during pregnancy (WHO, 2006).
Individual Study’s Quality Assessment
The review authors rigorously assessed the quality of included studies using the Risk of Bias Assessment Tool for Non-Randomized Studies (RoBANS) (Kim et al., 2013). Accordingly, six parameters (selection bias, confounding bias, performance bias, attrition bias, and reporting bias) were used to evaluate the quality of the studies. Each article was allocated to one of three possible groups; ‘low risk’, ‘high risk’, and ‘unclear’ based on these parameters (Table S2).
Data Synthesis and Analysis
A Microsoft excel spreadsheet was used to extract data from potentially eligible articles; then exported to Comprehensive Meta-analysis (CMA) version 2. software for analysis. The overall impact of maternal ANC utilization on NM was carried out by using a DerSimonian and Laird random-effects model (DerSimonian & Laird, 1986) and the risk ratio with a 95% confidence interval (CI) was determined. The existence of heterogeneity among included studies was checked using the I2 test statistic, which defines the percentage of total variation among studies due to heterogeneity rather than chance (Hardy & Thompson, 1998). Hence, subgroup analysis was conducted to explore the presence of possible sources of heterogeneity among studies. The pooled effect size was reported in the form of a risk ratio with 95% CI. A p-value of less than 0.05 was considered statistically significant. Furthermore, the presence of publication bias was investigated by using a visual inspection of funnel plot and Egger’s regression intercept (Egger et al., 1997).
Results
Study Characteristics
We identified 6117 studies during initial searching, of which, 44 full-text articles were assessed against eligibility criteria. Thus, 16 studies were excluded due to lack of exposure variable (6 articles) (Desalew et al., 2020; Gizaw et al., 2014; Mediratta et al., 2020; Mekonnen et al., 2013; Mengesha et al., 2016; Seid et al., 2019), absence of outcome variable (5 articles) (Andargie et al., 2013; Goba et al., 2018; Roro et al., 2018; Tadesse & Fantahun, 2017; Wolde et al., 2019), an outcome variable was compared with the number of ANC visits (3 articles) (Mersha et al., 2019; Tewabe et al., 2018; Haile et al., 2020) and insufficient data (2 articles) (Hadgu et al., 2020; Tura et al., 2020). Finally, 28 original studies were retained for this systematic review and meta-analysis (Fig. 1).
Study Description
The majority of the included studies were published in the last five years. We included thirteen cohort (Alebel et al., 2020; Asmare, 2018; Debelew et al., 2014; Dessu et al., 2020; Elmi Farah et al., 2018; Mekasha et al., 2020; Mengistu, 2020; Orsido et al., 2019; Roro et al., 2019; Sahle-Mariam & Berhane, 1997; Tessema & Tesema, 2020; Worku et al., 2014; Worku et al., 2012), seven case–control (Alemu et al., 2020; Araya et al., 2015; Kolobo et al., 2019; Kolola et al., 2016; Mohamed et al. 2016; Tesfaye et al., 2019) and eight cross-sectional (Aragaw, 2016; Basha et al., 2020; Demisse et al., 2017; Kebede et al., 2012; Wakgari & Wencheko, 2013; Wesenu et al., 2017; Woday et al., 2019; Yehuala & Teka, 2015) design studies. The sample size of participants in the original studies ranged from 228 to 11,023 neonates. Eight studies were from Amhara regional state (Alebel et al., 2020; Alemu et al., 2020; Demisse et al., 2017; Kebede et al., 2012; Kolola et al., 2016; Mengistu et al., 2020; Worku et al., 2014; Yehuala & Teka, 2015), five studies were from Oromia regional state (Aragaw, 2016; Debelew et al., 2014; Kolobo et al., 2019; Roro et al., 2019; Wesenu et al., 2017), three studies were from South Nation Nationalities People (SNNP) (Dessu et al., 2020; Orsido et al., 2019; Tesfaye et al., 2019) and Addis Ababa city administration (Asmare, 2018; Sahle-Mariam & Berhane, 1997; Worku et al., 2012). There were also two studies from the Somali regional state (Elmi Farah et al., 2018; Mohamed et al., 2016); one national study (Mekasha et al., 2020), one study from Benishangul Gumz region (Kidus et al., 2019), Afar region (Woday et al., 2019), and Tigray region (Araya et al., 2015). Further, we also included studies from the 2011 and 2016 Ethiopian Demographic Health Survey reports (Basha et al., 2020; Tessema & Tesema, 2020; Wakgari & Wencheko, 2013). Table 1 reveals a total of 59,104 neonates were involved in the review to determine the pooled effect of at least one ANC visit on NM in Ethiopia.
Individual Study’s Risk of Bias
The risk of bias in the selection of participants in the study was low for all studies. The bias due to incomplete outcome data reporting or missing data as a result of attrition was low in most of the included studies. Measurement bias due to the inadequate measurement of risk factors was low among twenty-two studies. However, the risk of confounding bias was high in twelve studies, but low in eighteen studies that adjusted for major confounding variables during the final analysis (Table 2).
A Pooled Effect Size of Antenatal Care on Neonatal Mortality
From the 28 studies included in this review, 20 studies showed ANC services utilization was significantly associated with NM. The random pooled effect of ANC on NM was 0.59 (95% CI: 0.45, 0.77) for infants born to women who had at least one ANC visit compared to infants born to women who had no ANC visit (Fig. 2).
Studies’ Heterogeneity and Publication Bias
Overall, there was considerable heterogeneity across the included studies, with I2 statistics = 95.3% and p-value < 0.001. Therefore, to explore the possible sources of heterogeneity, a subgroup analysis was carried out using study design, setting, and sample size. The heterogeneity that was present in the overall meta-analysis disappeared when the included studies were stratified by study region. For instance, in a subgroup analysis of Ethiopian Somalia region (RR = 0.64 [95% CI 0.46, 0.90]; p = 0.75 for the heterogeneity test, I2 = 0.0%) were not statistically heterogeneous. However, heterogeneity remained high within subgroups for sample size, study design, and setting. Stratification of the included studies by region also indicated a strong association between ANC and neonatal mortality; its association was found among studies conducted in the SNNP region compared to other regions and the overall pooled estimate. Accordingly, the risk ratio of neonatal mortality among infants born to women who had at least one ANC visit was 73% lower compared to infants born to women who had no ANC visit in a study conducted in the SNNP region (OR 0.27, 95% CI 0.17–0.42) (Table 3).
The visual inspection of the funnel plot illustrated that studies assessing the effect of ANC on neonatal mortality were symmetrically distributed (Fig. 3). The Egger regression test also indicated no evidence of publication bias (p-value = 0.90). Hence, our meta-analysis is unlikely to suffer from publication bias.
Discussion
Despite there is promising progress in reducing infant mortality and under-five mortality in Ethiopia, the decline for NM remained stagnant in recent years, which contributes to the highest rate of neonatal death in the SSA region. To reduce the high burden of neonatal mortality, the Ethiopian ministry of health designed and implanted maternal health services, most notably ANC services as one of the essential strategies. The current systematic review and meta-analysis, therefore, aimed to determine the effect of ANC on NM in Ethiopia, after including a large number of primary studies that characterize the wider geographical areas of the country.
This review showed that women who had at least one ANC visit were less likely to lose their neonates compared to neonates born to women who had no ANC visit. Accordingly, there is a 41% reduction in the risk of NM among infants born to women who had at least one ANC visit compared to infants born to women who had no ANC visit. This is in line with a review reported from SSA which indicated a 39% reduction in the risk of NM among infants born to women who initiated at least one ANC visit (Tekelab et al., 2019a, 2019b). Similarly, the finding of this systematic review and meta-analysis is in line with the study conducted in Zimbabwe, where utilization of ANC substantially reduces the likelihood of NM (Makate & Makate, 2017). A demographic and health survey done in SSA also reported a 48% reduction in the risk of NM among infants born to women who received at least one ANC visit compared to their counterparts (Doku & Neupane, 2017).
This notable effect of ANC against NM is because, ANC is one of the essential approaches to tackle NM (Canavan et al., 2017) through ensuring WHO recommendations for pregnant women such as disease prevention, early identification, and treatment of pregnancy complications which in turn help to reduce the risk of neonatal infection and death. The provision of folic acid supplementation, the distribution of insecticide-treated bed-net (ITN) for malaria prevention, and early detection and treatment of syphilis, including urinary tract infections during ANC visits (WHO, 2016c) are also widely important to avert the leading contributors of NM such as preterm birth and low birth weight (Cogswell et al., 2003; Siega-Riz et al., 2006; Zeng et al., 2008).
Antenatal care is an entry point for women to adhere to the continuum of care (institutional delivery, postnatal care, and infant immunization) (Ejigu et al., 2018; Fekadu et al., 2019; Haile et al., 2020). Hence, the use of these services would reduce neonatal mortality through the provision of quality essential newborn care (Alamneh et al., 2020), neonatal resuscitation (Lee et al., 2011; Patel et al., 2017), newborn immunization (Babirye et al., 2012; Boulton et al., 2019; Kassahun et al., 2015), promotion of breastfeeding, and advice on maternal nutrition (Alebel et al., 2018; Arage & Gedamu, 2016). The finding of this study implies that reinforcing ANC service utilization by skilled health care providers is a cost-effective intervention approach for the survival of newborns and the well-being of neonates, especially in Ethiopia, where the country is disproportionately affected by NM. This highlights ANC visit plays a crucial role to reduce NM; policy designers and program implementers should strengthen the ANC services utilization.
Strength and Limitations of the Study
The inclusion of several studies in the pooled analysis through the use of a comprehensive search strategy that fairly represents the wider geographical area of the country could closely determine the effect of ANC on the neonatal outcome, hence, this would offer strong implications to reinforce the existing maternal health policy. In this review, almost all the original studies that fitted to the review topic were published in the last five years which indicates, that the study raised NM reduction through ANC service provision is a relatively current issue. However, the interpretation of this study should bear in mind the following limitations. First, the inclusion of participants from the NICU population in some of the primary studies possibly affects the result. Second, the use of retrospective data and community-based study settings in some of the primary studies could be subjected to recall bias. Last, we do not investigate the quality of ANC visits based on service contents as the focus was mainly on the association between ANC visits and NM.
Conclusion
According to this finding NM markedly declined among infants born to women who had as few as one ANC visit compared to infants born to women who had no ANC visit. Therefore, to accelerate the progress in the reduction of newborn death in Ethiopia, promoting the utilization of ANC services by skilled providers is mandatory. Further, to reduce the unacceptably high NM, the review implies health care providers should strive to retain pregnant women within the continuum of care which in turn prevents the death of the neonates from sepsis and complications of preterm birth.
Data Availability
The review authors will share the data when requested with reasonable justification.
Code Availability
Not applicable.
References
Abate, B. B., Kasie, A. M., Reta, M. A., & Kassaw, M. W. (2020). Neonatal sepsis and its associated factors in East Africa: A systematic review and meta-analysis. International Journal of Public Health, 65(9), 1623–1633. https://doi.org/10.1007/s00038-020-01489-x
Alamneh, Y., Adane, F., Yirga, T., & Desta, M. (2020). Essential newborn care utilization and associated factors in Ethiopia: A systematic review and meta-analysis. BMC Pregnancy and Childbirth, 20(1), 124. https://doi.org/10.1186/s12884-020-2804-7
Alebel, A., Tesma, C., Temesgen, B., Ferede, A., & Kibret, G. D. (2018). Exclusive breastfeeding practice in Ethiopia and its association with antenatal care and institutional delivery: A systematic review and meta-analysis. International Breastfeeding Journal, 13(1), 31. https://doi.org/10.1186/s13006-018-0173-x
Alebel, A., Wagnew, F., Petrucka, P., Tesema, C., Moges, N. A., Ketema, D. B., Yismaw, I., Melkamu, M. W., Hibstie, Y. T., Temesgen, B., Bitew, Z. W., Tadesse, A. A., & Kibret, G. D. (2020). Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: a prospective cohort study. BMC Pediatrics, 20(1), 72–72. https://doi.org/10.1186/s12887-020-1963-z
Alemu, A. Y., Belay, G. M., Berhanu, M., & Minuye, B. (2020). Determinants of neonatal mortality at neonatal intensive care unit in Northeast Ethiopia: Unmatched case-control study. Tropical Medicine and Health, 48, 40–40. https://doi.org/10.1186/s41182-020-00232-9
Andargie, G., Berhane, Y., Worku, A., & Kebede, Y. (2013). Predictors of perinatal mortality in rural population of Northwest Ethiopia: A prospective longitudinal study. BMC Public Health, 13(1), 168.
Aragaw, Y. (2016). Perinatal mortality and associated factor in Jimma university specialized hospital. South West Ethiopia. Gynecol Obstet (sunnyvale), 6(409), 2161–2932. https://doi.org/10.4172/2161-0932.1000409
Arage, G., & Gedamu, H. (2016). Exclusive Breastfeeding Practice and Its Associated Factors among Mothers of Infants Less Than Six Months of Age in Debre Tabor Town, Northwest Ethiopia: A Cross-Sectional Study. Advances in Public Health, 2016, 3426249. https://doi.org/10.1155/2016/3426249
Araya, T., Ghiwot, H., Gidey, G., Tilahun, W., & Mola, M. (2015). risk factors of neonatal deaths among asphyxiated neonates in Ayder Referral Hospital, Mekelle, Ethiopia: A case control study.
Arunda, M., Emmelin, A., & Asamoah, B. O. (2017). Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: Analysis of national survey data. Global Health Action, 10(1), 1328796.
Asmare, Y. (2018). Survival status and predictor of mortality among premature neonate admitted to neonatal intensive care unit from 2013–2017 in Tikur Anbesa specialized hospital, Addis Ababa, Ethiopia, 2018. Nursing Addis Ababa: Addis Ababa University, 70, 4172.
Babirye, J. N., Engebretsen, I. M., Makumbi, F., Fadnes, L. T., Wamani, H., Tylleskar, T., & Nuwaha, F. (2012). Timeliness of childhood vaccinations in Kampala Uganda: A community-based cross-sectional study. PLoS ONE, 7(4), e35432.
Basha, G. W., Woya, A. A., & Tekile, A. K. (2020). Determinants of neonatal mortality in Ethiopia: An analysis of the 2016 Ethiopia demographic and health survey. African Health Sciences, 20(2), 715–723. https://doi.org/10.4314/ahs.v20i2.23
Berhan, Y., & Berhan, A. (2014). Perinatal mortality trends in Ethiopia. Ethiopian Journal of Health Sciences, 24(Suppl), 29–40. https://doi.org/10.4314/ejhs.v24i0.4s
Boulton, M. L., Carlson, B. F., Wagner, A. L., Porth, J. M., Gebremeskel, B., & Abeje, Y. (2019). Vaccination timeliness among newborns and infants in Ethiopia. PLoS ONE, 14(2), e0212408.
Canavan, M. E., Brault, M. A., Tatek, D., Burssa, D., Teshome, A., Linnander, E., & Bradley, E. H. (2017). Maternal and neonatal services in Ethiopia: Measuring and improving quality. Bulletin of the World Health Organization, 95(6), 473.
Cogswell, M. E., Parvanta, I., Ickes, L., Yip, R., & Brittenham, G. M. (2003). Iron supplementation during pregnancy, anemia, and birth weight: A randomized controlled trial. The American Journal of Clinical Nutrition, 78(4), 773–781.
Darmstadt, G. L., Bhutta, Z. A., Cousens, S., Adam, T., Walker, N., De Bernis, L., Team, L. N. S. S. (2005). Evidence-based, cost-effective interventions: how many newborn babies can we save? The Lancet, 365(9463), 977–988.
Debelew, G. T., Afework, M. F., & Yalew, A. W. (2014). Determinants and causes of neonatal mortality in Jimma Zone, Southwest Ethiopia: A multilevel analysis of prospective follow up study. PLoS ONE, 9(9), e107184–e107184. https://doi.org/10.1371/journal.pone.0107184
Demisse, A. G., Alemu, F., Gizaw, M. A., & Tigabu, Z. (2017). Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of University of Gondar Hospital. Northwest Ethiopia. Pediatric Health Med Ther, 8, 57.
DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188.
Desalew, A., Sintayehu, Y., Teferi, N., Amare, F., Geda, B., Worku, T., Abera, K., & Asefaw, A. (2020). Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in eastern Ethiopia: A facility-based prospective follow-up study. BMC Pediatrics, 20, 1–11.
Dessu, S., Habte, A., Melis, T., & Gebremedhin, M. (2020). Survival status and predictors of mortality among newborns admitted with neonatal sepsis at public hospitals in Ethiopia. International Journal of Pediatrics, 2020, 8327028. https://doi.org/10.1155/2020/8327028
Doku, D. T., & Neupane, S. (2017). Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. International Journal of Epidemiology, 46(5), 1668–1677. https://doi.org/10.1093/ije/dyx125
Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634.
Ejigu Tafere, T., Afework, M. F., & Yalew, A. W. (2018). Antenatal care service quality increases the odds of utilizing institutional delivery in Bahir Dar city administration, North Western Ethiopia: A prospective follow up study. PLoS ONE, 13(2), e0192428–e0192428. https://doi.org/10.1371/journal.pone.0192428
Elmi Farah, A., Abbas, A. H., & Tahir Ahmed, A. (2018). Trends of admission and predictors of neonatal mortality: A hospital based retrospective cohort study in Somali region of Ethiopia. PLoS ONE, 13(9), e0203314. https://doi.org/10.1371/journal.pone.0203314
Ethiopian Public Health Institute ICF. (2019). Ethiopia mini demographic and health survey 2019: Key indicators. Journal of Chemical Information and Modeling, 53, 1689–1699.
Fekadu, G. A., Ambaw, F., & Kidanie, S. A. (2019). Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: Further analysis of the 2016 demographic and health survey. BMC Pregnancy and Childbirth, 19(1), 64–64. https://doi.org/10.1186/s12884-019-2216-8
Gebremedhin, D., Berhe, H., & Gebrekirstos, K. (2016). Risk factors for neonatal sepsis in public hospitals of Mekelle City, North Ethiopia, 2015: Unmatched case control study. PLoS ONE, 11(5), e0154798–e0154798. https://doi.org/10.1371/journal.pone.0154798
Gizaw, M., Molla, M., & Mekonnen, W. (2014). Trends and risk factors for neonatal mortality in Butajira District, South Central Ethiopia, (1987–2008): A prospective cohort study. BMC Pregnancy and Childbirth, 14, 64–64. https://doi.org/10.1186/1471-2393-14-64
Goba, G. K., Tsegay, H., Gebregergs, G. B., Mitiku, M., Kim, K. A., & Alemayehu, M. (2018). A facility-based study of factors associated with perinatal mortality in Tigray, northern Ethiopia. International Journal of Gynecology & Obstetrics, 141(1), 113–119.
Gregory, K. D., Niebyl, J. R., & Johnson, T. R. (2016). Preconception and prenatal care: Part of the continuum. GABBE SG Et Al. Obstetrics: Normal and Problem Pregnancies, 7, 101–124.
Hadgu, F. B., Gebretsadik, L. G., Mihretu, H. G., & Berhe, A. H. (2020). Prevalence and factors associated with neonatal mortality at Ayder comprehensive specialized hospital, Northern Ethiopia. A cross-sectional study. Pediatric Health Med Ther, 11, 29–37. https://doi.org/10.2147/PHMT.S235591
Haile, D., Kondale, M., Andarge, E., Tunje, A., Fikadu, T., & Boti, N. (2020). Level of completion along continuum of care for maternal and newborn health services and factors associated with it among women in Arba Minch Zuria woreda, Gamo zone, Southern Ethiopia: A community based cross-sectional study. PLoS ONE, 15(6), e0221670.
Hardy, R. J., & Thompson, S. G. (1998). Detecting and describing heterogeneity in meta-analysis. Statistics in Medicine, 17(8), 841–856.
Hug, L., Alexander, M., You, D., & Alkema, L. (2019). National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: A systematic analysis. The Lancet Global Health, 7(6), e710–e720.
Ibrahim, J., Yorifuji, T., Tsuda, T., Kashima, S., & Doi, H. (2012). Frequency of antenatal care visits and neonatal mortality in Indonesia. Journal of Tropical Pediatrics, 58(3), 184–188.
Jena, B. H., Biks, G. A., Gelaye, K. A., & Gete, Y. K. (2020). Magnitude and trend of perinatal mortality and its relationship with inter-pregnancy interval in Ethiopia: A systematic review and meta-analysis. BMC Pregnancy and Childbirth, 20(1), 1–13.
Kassahun, M. B., Biks, G. A., & Teferra, A. S. (2015). Level of immunization coverage and associated factors among children aged 12–23 months in Lay Armachiho District, North Gondar Zone, Northwest Ethiopia: A community based cross sectional study. BMC Research Notes, 8(1), 1–10.
Kebede, B., Gebeyehu, A., Sharma, H. R., & Yifru, S. (2012). Prevalence and associated factors of neonatal mortality in North Gondar Zone, Northwest Ethiopia. Ethiopian Journal of Health Development, 26(2), 66–71.
Kidus, F., Woldemichael, K., & Hiko, D. (2019). Predictors of neonatal mortality in Assosa zone, Western Ethiopia: A matched case control study. BMC Pregnancy and Childbirth, 19(1), 108–108. https://doi.org/10.1186/s12884-019-2243-5
Kim, S. Y., Park, J. E., Lee, Y. J., Seo, H.-J., Sheen, S.-S., Hahn, S., Jang, B.-H., & Son, H.-J. (2013). Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. Journal of Clinical Epidemiology, 66(4), 408–414. https://doi.org/10.1016/j.jclinepi.2012.09.016
Kolobo, H., Chaka, T., & Kassa, R. (2019). Determinants of neonatal mortality among newborns admitted to neonatal intensive care unit Adama, Ethiopia: A case–control study. Journal of Clinical Neonatology, 8(4), 232–237. https://doi.org/10.4103/jcn.JCN_23_19
Kolola, T., Ekubay, M., Tesfa, E., & Morka, W. (2016). Determinants of neonatal mortality in North Shoa Zone, Amhara Regional State. Ethiopia. Plos One, 11(10), e0164472–e0164472. https://doi.org/10.1371/journal.pone.0164472
Lambon-Quayefio, M. P., & Owoo, N. S. (2014). Examining the influence of antenatal care visits and skilled delivery on neonatal deaths in Ghana. Applied Health Economics and Health Policy, 12(5), 511–522.
Lander, T. (2006). Neonatal and perinatal mortality: country, regional and global estimates. World Health Organization.
Lee, A. C., Cousens, S., Wall, S. N., Niermeyer, S., Darmstadt, G. L., Carlo, W. A., Keenan, W. J., Bhutta, Z. A., Gill, C., & Lawn, J. E. (2011). Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: A systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health, 11(3), 1–19.
Lopez, A. D. (2014). Levels & Trends in Child Mortality: Report 2014, Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation: United Nations Inter-agency Group for Child Mortality Estimation (UN IGME).
Makate, M., & Makate, C. (2017). The impact of prenatal care quality on neonatal, infant and child mortality in Zimbabwe: Evidence from the demographic and health surveys. Health Policy and Planning, 32(3), 395–404.
Mediratta, R. P., Amare, A. T., Behl, R., Efron, B., Narasimhan, B., Teklu, A., Shehibo, A., Ayalew, M., & Kache, S. (2020). Derivation and validation of a prognostic score for neonatal mortality in Ethiopia: A case-control study. BMC Pediatrics, 20(1), 238–238. https://doi.org/10.1186/s12887-020-02107-8
Mejía-Guevara, I., Zuo, W., Bendavid, E., Li, N., & Tuljapurkar, S. (2019). Age distribution, trends, and forecasts of under-5 mortality in 31 sub-Saharan African countries: A modeling study. PLoS Medicine. https://doi.org/10.1371/journal.pmed.1002757
Mekasha, A., Tazu, Z., Muhe, L., Abayneh, M., Gebreyesus, G., Girma, A., McClure, E. M., Goldenberg, R. L., & Nigussie, A. K. (2020). Factors associated with the death of preterm babies admitted to neonatal intensive care units in Ethiopia: A Prospective, Cross-sectional, and observational study. Glob Pediatr Health. https://doi.org/10.1177/2333794X20970005
Mekonnen, Y., Tensou, B., Telake, D. S., Degefie, T., & Bekele, A. (2013). Neonatal mortality in Ethiopia: Trends and determinants. BMC Public Health, 13(1), 483.
Mengesha, H. G., Wuneh, A. D., Lerebo, W. T., & Tekle, T. H. (2016). Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: Prospective cohort study. BMC Pregnancy and Childbirth, 16(1), 202.
Mengistu, B. A., Yismaw, A. E., Azene, Z. N., & Mihret, M. S. (2020). Incidence and predictors of neonatal mortality among neonates admitted in Amhara regional state referral hospitals, Ethiopia: Prospective follow up study. BMC Pediatrics, 20(1), 142. https://doi.org/10.1186/s12887-020-02031-x
Mersha, A., Bante, A., & Shibiru, S. (2019). Neonatal mortality and its determinates in public hospitals of Gamo and Gofa zones, southern Ethiopia: Prospective follow up study. BMC Pediatrics, 19(1), 499–499. https://doi.org/10.1186/s12887-019-1881-0
Mohamed Shaker EL-Slayed Azzaz, A., Martínez-Maestre, M. A., & Torrejón-Cardoso, R. (2016). Antenatal care visits during pregnancy and their effect on maternal and fetal outcomes in pre-eclamptic patients. Journal of Obstetrics and Gynaecology Research, 42(9), 1102–1110.
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Paul, S., & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1–9.
Orsido, T. T., Asseffa, N. A., & Berheto, T. M. (2019). Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: A retrospective cohort study. BMC Pregnancy and Childbirth, 19(1), 83. https://doi.org/10.1186/s12884-019-2227-5
Osman, M. O., Nur, A. M., Abdilahi, A. O., & Ibrahim, A. M. (2020). Risk Factors of neonatal death in neonatal intensive care unit at Sheik Hassan Yabare Referral Hospital, East Ethiopia, 2019: Unmatched case control study. American Journal of Pediatrics., 6(2), 162–167.
Patel, A., Khatib, M. N., Kurhe, K., Bhargava, S., & Bang, A. (2017). Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: A systematic review and meta-analysis. BMJ Paediatr Open. https://doi.org/10.1136/bmjpo-2017-000183
WHO Press Release, W. I., World Bank Press Release, . (2017). Levels and Trends in Child Mortality Retrieved from https://sdg.iisd.org/news/un-report-finds-newborn-child-mortality-rates-on-the-rise/
Raatikainen, K., Heiskanen, N., & Heinonen, S. (2007). Under-attending free antenatal care is associated with adverse pregnancy outcomes. BMC Public Health, 7(1), 268.
Roro, E. M., Sisay, M. M., & Sibley, L. M. (2018). Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia Region, Ethiopia: Community based nested case control study. BMC Public Health, 18(1), 888–888. https://doi.org/10.1186/s12889-018-5757-2
Roro, E. M., Tumtu, M. I., & Gebre, D. S. (2019). Predictors, causes, and trends of neonatal mortality at Nekemte Referral Hospital, east Wollega Zone, western Ethiopia (2010–2014). Retrospective Cohort Study. Plos One, 14(10), e0221513–e0221513. https://doi.org/10.1371/journal.pone.0221513
Sahle-Mariam, Y., & Berhane, Y. (1997). Neonatal mortality among hospital delivered babies in Addis Ababa, Ethiopia. The Ethiopian Journal of Health Development (EJHD), 11(3), 1997.
Seid, S. S., Ibro, S. A., Ahmed, A. A., Olani Akuma, A., Reta, E. Y., Haso, T. K., & Fata, G. A. (2019). Causes and factors associated with neonatal mortality in Neonatal Intensive Care Unit (NICU) of Jimma University Medical Center, Jimma, South West Ethiopia. Pediatric Health, Medicine and Therapeutics, 10, 39–48. https://doi.org/10.2147/phmt.s197280
Siega-Riz, A. M., Hartzema, A. G., Turnbull, C., Thorp, J., McDonald, T., & Cogswell, M. E. (2006). The effects of prophylactic iron given in prenatal supplements on iron status and birth outcomes: A randomized controlled trial. American Journal of Obstetrics and Gynecology, 194(2), 512–519.
Singh, A., Pallikadavath, S., Ram, F., & Alagarajan, M. (2014). Do antenatal care interventions improve neonatal survival in India? Health Policy and Planning, 29(7), 842–848. https://doi.org/10.1093/heapol/czt066
Tadesse, Y., & Fantahun, M. (2017). Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an unmatched case control study. BMC Pregnancy and Childbirth. https://doi.org/10.1186/s12884-017-1420-7
Tekelab, T., Akibu, M., Tagesse, N., Tilhaun, T., Yohanes, Y., & Nepal, S. (2019a). Neonatal mortality in Ethiopia: A protocol for systematic review and meta-analysis. Systematic Reviews, 8(1), 103.
Tekelab, T., Chojenta, C., Smith, R., & Loxton, D. (2019b). The impact of antenatal care on neonatal mortality in sub-Saharan Africa: A systematic review and meta-analysis. PLoS ONE, 14(9), e0222566.
Tesfaye, S., Gebru, Z., Mamo, M., Getahun, F., & Boti, N. (2019). Determinants of perinatal mortality in Arba Minch general hospital, Gamo Zone, Southern Ethiopia. Ethiopian Journal of Reproductive Health, 11(4), 7–7.
Tessema, Z. T., & Tesema, G. A. (2020). Incidence of neonatal mortality and its predictors among live births in Ethiopia: Gompertz gamma shared frailty model. Italian Journal of Pediatrics, 46(1), 138. https://doi.org/10.1186/s13052-020-00893-6
Tewabe, T., Mehariw, Y., Negatie, E., & Yibeltal, B. (2018). Neonatal mortality in the case of Felege Hiwot referral hospital, Bahir Dar, Amhara Regional State, North West Ethiopia 2016: A one year retrospective chart review. Italian Journal of Pediatrics, 44(1), 57–57. https://doi.org/10.1186/s13052-018-0498-5
Tura, A. K., Scherjon, S., van Roosmalen, J., Zwart, J., Stekelenburg, J., & van den Akker, T. (2020). Surviving mothers and lost babies - burden of stillbirths and neonatal deaths among women with maternal near miss in eastern Ethiopia: A prospective cohort study. Journal of Global Health, 10(1), 01041310–01041310. https://doi.org/10.7189/jogh.10.010413
UN-DESA. (2017). “Sustainable Development Goal 3: Ensure healthy lives and promote well-being for all at all ages,” Sustainable Development Knowledge Platform, 2017. . Retrieved from https://sustainabledevelopment.un.org/sdg3
United Nations Inter-agency Group for Child Mortality Estimation (UNIGME). (2017). ‘Levels & Trends in Child Mortality: Report 2017, Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation’ Retrieved from New York:
United Nations Inter-agency Group for Child Mortality Estimation (UNIGME). (2018). ‘Levels & Trends in Child Mortality: Report 2018, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’, . Retrieved from New York:
United Nations Inter-agency Group for Child Mortality Estimation (UNIGME). (2019). ‘Levels & Trends in Child Mortality: Report 2019, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’. Retrieved from New York:
United Nations Children’s Fund. (2019). Monitoring the Situation of Children and Women, Neonatal and Child Mortality Estimation. UNICEF; 2019. Retrieved from https://www.unicef.org/reports/ending-preventable-newborn-deaths-stillbirths-quality-health-coverage-2020-2025
Wakgari, N., & Wencheko, E. (2013). Risk factors of neonatal mortality in Ethiopia. Ethiopian Journal of Health Development, 27(3), 192–199.
Wesenu, M., Kulkarni, S., & Tilahun, T. (2017). Modeling determinants of time-to-death in premature infants admitted to neonatal intensive care unit in Jimma University Specialized Hospital. Annals of Data Science, 4(3), 361–381.
WHO. (2005). make every mother and child count. Geneva, Swizerland Retrieved from http://www.who.int/whr/2005/en/index.html.
WHO. (2006). Neonatal and perinatal mortality: Country, regional and global estimates. World Health Organization.
WHO. (2009). Women and health: Today’s evidence tomorrow’s agenda. Swizerland World Health Organization.
WHO. (2015a). Global Strategy for Women’s, Children’s and Adolescent’s Health 2016–2030. Swizerland.
WHO. (2015b). World health statistics 2015. World Health Organization.
WHO. (2016a). MCEE-WHO methods and data sources for child causes of death 2000–2015. Swierland.
WHO. (2016b). New guidelines on antenatal care for a positive pregnancy experience. Retrieved from https://www.who.int/reproductivehealth/news/antenatal-care/en/
WHO. (2016c). WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience: Summary Retrieved from https://apps.who.int/iris/bitstream/handle/10665/259947/WHO-RHR-18.02-eng.pdf;jsessionid=A4700DA7000A5EEBF454BC915AEC1DB0?sequence=1
Woday, A., Mekuria, Y., & Denis, C. (2019). Newborn Mortality And Its Associated Factors Among Neonates Admitted At Public Hospitals In Afar Region; A Health Facility Based Study.
Wolde, H. F., Gonete, K. A., Akalu, T. Y., Baraki, A. G., & Lakew, A. M. (2019). Factors affecting neonatal mortality in the general population: Evidence from the 2016 Ethiopian Demographic and Health Survey (EDHS)-multilevel analysis. BMC Research Notes, 12(1), 610. https://doi.org/10.1186/s13104-019-4668-3
Worku, A. G., Yalew, A. W., & Afework, M. F. (2014). The contributions of maternity care to reducing adverse pregnancy outcomes: A cohort study in Dabat District, Northwest Ethiopia. Maternal and Child Health Journal, 18(6), 1336–1344.
Worku, B., Kassie, A., Mekasha, A., Tilahun, B., & Worku, A. (2012). Predictors of early neonatal mortality at a neonatal intensive care unit of a specialized referral teaching hospital in Ethiopia. Ethiopian Journal of Health Development, 26(3), 200–207.
World Health Organisation. (2019). Newborns: reducing mortality. Geneva, Swizerland Retrieved from https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
World Health Organization. (2019). Newborns: Reducing mortality. World Health Organization.
Wright, S. (2014). Ending newborn deaths: Ensuring every baby survives: Save the Children.
Yehuala, S., & Teka, Z. (2015). Survival analysis of premature infants admitted to Neonatal Int ensive care unit (NICU) in Northwest Ethiopia using Semi-Parametric Fr ailty Model. Journal of Biometrics & Biostatistics, 6(1), 1.
Zeng, L., Cheng, Y., Dang, S., Yan, H., Dibley, M. J., Chang, S., & Kong, L. (2008). Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation, and perinatal mortality in rural western China: Double blind cluster randomised controlled trial. BMJ. https://doi.org/10.1136/bmj.a2001
Acknowledgements
We would like to acknowledge Haramaya University and all authors of the primary studies. We would also like to thank Addisu Shunu and Yitagesu Sintayehu for their contribution (i.e., searching databases and reviewing manuscript) to this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The review authors contributed to the review. The review authors made a significant contribution like drafting or writing, or critically reviewing the manuscript, selecting journal, and reviewing the documents before submission. The review authors also will take responsibility and accountability for the contents of the article.
Corresponding author
Ethics declarations
Competing interests
There is no competing interest.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tiruye, G., Shiferaw, K. Antenatal Care Reduces Neonatal Mortality in Ethiopia: A Systematic Review and Meta-Analysis of Observational Studies. Matern Child Health J 27, 2064–2076 (2023). https://doi.org/10.1007/s10995-023-03765-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03765-7