Abstract
Purpose
Perinatal mood and anxiety disorders can have far reaching negative impact on both maternal mental health and child growth and development. Multimodal group parenting programs have been shown to improve maternal mental health symptoms however, they are often costly to provide and not accessible to many mothers, especially those mothers suffering from mental health symptoms. Therefore, the authors sought to answer the following question by undertaking a systematic review of the literature: are parenting interventions aimed at improving maternal-child interaction also a way to address mental health symptoms (i.e. depression, anxiety, stress) in mothers?
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. An online platform that supports the systematic review process and quality assessment according to Cochrane guidelines, Covidence, was used in conjunction with an adapted extraction tool to identify relevant studies and extract data for analysis.
Results
11 articles were included in the qualitative synthesis. There was great heterogeneity between study interventions and measurement of outcomes for maternal mental health symptoms which precluded meta-analysis.
Conclusion
Studies reviewed did not demonstrate consistent evidence to recommend that parenting interventions leads to improvement in maternal mental health symptoms for depression, anxiety or stress. However, there was evidence that participating in parenting programs does not worsen these symptoms and some encouraging evidence that alternative delivery methods, beyond face to face, could, with more research, lead to more financially feasible and sustainable models of delivery of these types of interventions in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance Statement
What is already known
There is evidence that group-based parenting interventions that focus on behavioral, cognitive-behavioral and multimodal parenting interventions improve psycho-social health in mothers. However behavioral and multi-modal programs are often resource intensive for both providers and mothers.
What this study adds
This review reports that there is currently inconsistent evidence to recommend parent interventions alone to improve maternal mental health symptoms. But there is some encouraging evidence that alternative delivery methods beyond face to face could lead to more financially feasible and sustainable models of delivery in the future.
Introduction
Maternal mental health has gained increasing attention in both the Academic and lay literatures due to its implications for both mother and child. In pregnancy, major depression affects up to 12.7% of women (Gaynes et al., 2005). In the post-partum period, depressive symptoms are estimated to range from 8 to 27% in the U.S. (Ko et al., 2017; Long et al., 2018). In that same period, anxiety occurs in about 8.5% (Goodman et al., 2016). Perinatal stress is also commonly reported by mothers (Ross and McLean, 2006).
Maternal mental health not only impacts the mother but also her developing children. Perinatal mood and anxiety disorders in mothers have been associated with negative effects on infants and young children, especially during the critical early years of development beginning with inadequate mother-child bonding (Righetti-Veltema et al., 2002; Hoffman et al., 2017). Depressive symptoms reduce mothers’ ability to respond to infant cues in an appropriate and sensitive manner (Lovejoy et al., 2000; Wheeler et al., 2007). Postpartum depression is associated with developmental delays in cognition, language and motor skills (Smith-Nielsen et al., 2016) and poorer behavioral outcomes (Hay et al., 2003; Grace et al., 2003; Fihrer et al., 2009).
When mothers are provided with concrete attainable skills for improving interactions with their child, the impact of depression on both mother and child can be mitigated (Beeber et al., 2010). But mothers with poor mental health often report low energy, and they use the limited energy they do have to meet their children’s needs (McKechnie et al., 2018). Thus, mothers are less likely to prioritize their own needs, including seeking needed healthcare treatment for themselves (O’Hara 2009; McKechnie et al., 2018). However, if the intervention is promoted as a way to support the child’s needs, mothers are more likely to engage in the program (Beeber et al., 2004, 2010). Our experience in practice and research with mothers who have mental health symptom and young children led to the development of our research question for this systematic review: are indirect interventions aimed at improving maternal-child interaction a way to also address mental health symptoms (i.e. depression, anxiety, stress) in mothers?
This review differs from the Cochrane review (Barlow et al., 2014) which reported that group-based parenting programs of three types (behavioral, cognitive-behavioral and multimodal) are associated with improved psychosocial health in the short-term. First, our question is not limited to group-based interventions, which mothers may find difficult to access due to needs for childcare and travel to the meeting point. Secondly, we excluded multi-modal programs that included psychotherapies, as we were interested in interventions that were focused on parenting the child (the child’s needs) rather than on the mother herself. Finally, we narrowed the focus from general psychosocial health to the more specific mental health symptoms of depression, anxiety, and stress.
Methods
The authors followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Studies were eligible for review if they included a parenting focused intervention for mothers with children between the ages of 0 and 5 years old, measured maternal mental health symptoms (e.g. depression, anxiety, stress) as a secondary outcome, and were conducted in a community setting (i.e. not residential treatment or hospitalization). Interventions that were not parenting focused (e.g. general psychotherapy, support groups, sleep or massage focused) were excluded.
The search was performed in PubMed, EMBASE (Elsevier), CINAHL Plus with Full Text (EBSCO), and PsycInfo (EBSCO) and included articles from January 1, 1989 to February 20, 2019 (the last date of searching). Authors selected 1989 as the first year of interest due to a state of the science paper published that year on the implications of maternal depression for young children (Gross, 1989). The search included subject headings and keywords for depression, psychosocial health, maternal health, and maternal welfare, and keywords relating to parent education or training. Results were restricted to English language articles. The full search strategy for each database can be found in Online Appendix A.
Results of each search were uploaded into Covidence (www.covidence.org), an online platform for screening and data extraction. Duplicates across searches were flagged and removed by Covidence. Following the previously described eligibility criteria, each title and abstract were screened by two reviewers; any differences in inclusion/exclusion determinations were discussed before moving forward with the review. Every full text screening was also conducted by at least two reviewers, with any differences discussed and resolved.
The following data was extracted for each study by 2 reviewers and entered into a table: article information (authors, institution, year of publication, sponsorship sources, country, setting), methods (study design, inclusion/exclusion criteria, intervention groups, sample size, recruitment, retention, measures used [depression, anxiety, stress]), population (inclusion criteria, exclusion criteria, group differences, baseline characteristics: child’s age, mother’s age, etc.), interventions (characteristics: intensity, topics, method), outcomes (depressive symptoms, anxiety, and/or stress). This extraction table was then coded for relevant findings. Quality assessment was completed following the Cochrane guidelines (Higgins et al., 2011); each study was assessed by at least two reviewers and consensus was reached following discussion.
Selection Process
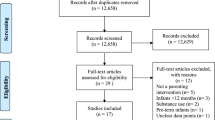
The database searches identified 889 unique articles, with reviewers excluding 830 articles through title/abstract screening. The remaining 59 abstracts were reviewed and screened again by at least two reviewers. Upon full text review, 48 articles were excluded; reasons for exclusion are listed in Fig. 1. After screening and exclusions, 11 articles were included in the synthesis. Findings are reported as follows: (1) study and sample characteristics; (2) parenting interventions characteristics; (3) secondary outcomes of maternal mental health.
Study and Sample Characteristics
Study characteristics are summarized on Tables 1 and 2. All eleven studies reviewed were conducted as randomized control trials, with two using randomized cluster design (Bayer et al., 2010; Chang et al., 2015). Nine studies used intervention group vs. control or usual care group (Gross et al. 1995; Connell et al., 1997; Niccols 2009; Bayer et al., 2010; Letourneau et al., 2011; Berkule et al., 2014; Homem et al., 2015; Chang et al., 2015; Doyle et al., 2017; Boyd et al., 2019). Recruitment methods included consecutive invitation to potentially qualifying participants at hospitals and clinics or health centers (Bayer et al., 2010; Berkule et al., 2014; Chang et al., 2015), distribution of information via the usual media channels (Boyd et al., 2019; Connell et al., 1997; Doyle et al., 2017; Farris et al., 2013; Gross et al., 1995; Letourneau et al., 2011; Niccols, 2009) and from a larger parent study (Homem, et al., 2015). The duration of follow up ranged from 2 months (Boyd et al., 2019) to 5 years (Doyle et al., 2017). After removing the outlier of 5 years, the mean duration of follow up was 7.5 months with a mode of 3 months. Total retention rates ranged from a low of 53% at 60 months follow up (Doyle et al., 2017) to 90% at 1 month (Niccols, 2009).
Of the 11 studies included, nine were conducted in English-speaking high-income countries. One study was conducted in Portugal, another high-income country (Homem et al., 2015). The remaining study was conducted in Jamaica and St. Lucia, both upper middle-income countries, and Antigua, a high-income country (Chang et al., 2015).
Sample sizes ranged from 20 (Boyd et al., 2019) to 539 (Bayer et al., 2010). Most studies reported maternal mean age between 25 and 36 years old. Four studies targeted mothers with low socioeconomic status (Berkule et al., 2014; Chang et al., 2015; Doyle et al., 2017; Boyd et al., 2019) and two additional studies included a large proportion of mothers with other high-risk factors such as rural living (Connell et al., 1997) or substance misuse, social isolation, etc. (Bayer et al., 2010). Two studies specifically reported the use of a homogenous and lower-risk sample (Gross et al., 1995; Farris et al., 2013).
Parenting Intervention Characteristics
Parenting intervention characteristics are summarized in Table 3. Parenting interventions were diverse, but all studies used evidence-based parenting programs (Online Appendix B). Each intervention focused on identifying ineffective parenting techniques and promoted positive and effective parenting behaviors with infants/toddlers. In addition, appropriate play and child development were common themes in the education delivered.
Multiple methods for intervention delivery were used in the studies, and some studies included different types of delivery for different participant groups. Five studies included face to face group sessions for at least one group, which was the most common format for parenting interventions (Gross et al., 1995; Connell et al., 1997; Niccols, 2009; Bayer et al., 2010; Homem et al., 2015; Chang et al., 2015). Three other studies included interventions delivered face to face but in a home setting (Letourneau et al., 2011; Berkule et al., 2014; Doyle et al., 2017). Two additional studies were delivered face to face individually in a non-home setting (Farris et al., 2013; Boyd et al., 2019). Three studies also included samples that received the intervention remotely, over the phone (Connell et al., 1997) or via the internet (Farris et al., 2013; Boyd et al., 2019).
The interventions were also offered in a variety of settings. Five took place in a researcher-chosen setting (Gross et al., 1995; Niccols, 2009; Farris et al., 2013; Homem et al., 2015; Boyd et al., 2019), three in a primary care setting (Bayer et al., 2010; Berkule et al., 2014; Chang et al., 2015), two in the mother’s home (Letourneau et al., 2011; Doyle et al., 2017), and three remotely via phone or internet (Connell et al., 1997; Farris et al., 2013; Boyd et al., 2019).
Studies also varied widely in who provided the intervention. Interventionists included trained peer mentors (Letourneau et al., 2011), community health workers (Chang et al., 2015), trained facilitators (Niccols, 2009; Berkule et al., 2014; Boyd et al., 2019), experts or persons with advanced educational credentials (i.e., child psychologists, psychiatrists or social workers) (Connell et al., 1997; Bayer et al., 2010; Farris et al., 2013; Homem et al., 2015), and nurses (Bayer et al., 2010; Farris et al., 2013; Chang et al., 2015).
The intervention dose (duration and frequency) also varied widely across studies. The duration ranged from being unmeasurable (delivered through mailed written materials) (Berkule et al., 2014) or described as a “session” without a specific duration each time (Gross et al., 1995) to 2 h per session (Bayer et al., 2010). Studies that included online asynchronous interventions also had no reported measure for time of intervention (Farris et al., 2013; Boyd et al., 2019). The rest of the study’s intervention sessions lasted from 20 to 60 min at a time. The most common frequency for intervention delivery was weekly (Gross et al., 1995; Connell et al., 1997; Niccols, 2009; Letourneau et al., 2011; Farris et al., 2013; Homem et al., 2015; Boyd et al., 2019).
Interventions also had a range of intensities across study. For the purpose of this review, interventions were considered more intense based on the expectations for the mother. For example, if an intervention required physical resources such as a computer, that would be a higher intensity. Intensity was also judged based on ease of access; if a mother needed to travel to an additional site (rather than a home visit or having the intervention wrapped into a pre-existing appointment) or needed to secure childcare to complete the intervention, then that intervention was also considered higher intensity. Six of the eleven studies included interventions that were deemed higher intensity (Gross et al., 1995; Niccols, 2009; Bayer et al., 2010; Farris et al., 2013; Homem et al., 2015; Boyd et al., 2019).
Secondary Outcomes of Maternal Mental Health
Depression
Ten of the studies included in this review reported on maternal depression as an outcome (Table 1). However, there was still variation across studies, as depressive symptoms were assessed with six different scales: Center for Epidemiological Studies Depression Scale (CES-D) (Gross et al., 1995; Niccols 2009; Chang et al., 2015), Depression Anxiety Stress Scales-21 (DASS-21; depression subscale) (Connell et al., 1997; Bayer et al., 2010), Beck Depression Inventory(Homem et al., 2015; Boyd et al., 2019), Symptoms Checklist-90 Revised (SCL-90-R, depression subscale) (Farris et al., 2013), Edinburgh Postnatal Depression Scale (EPDS) (Letourneau et al., 2011), and Patient Health Questionnaire-9 (PHQ-9) (Berkule et al., 2014).
Studies reported a range of findings related to improvement in depressive symptoms (Table 4). Three of the eleven studies reported that parenting interventions were associated with a statistically significant decrease in maternal depressive symptoms from baseline at the p < 0.05 level (Niccols, 2009; Farris et al., 2013; Boyd et al., 2019), and one additional study reported improved symptoms in the intervention group at p = 0.08 (Connell et al., 1997). Another study did not collect depressive symptom scores prior to intervention, but did report that the two intervention groups had lower scores compared to the control group at program completion (Berkule et al., 2014). Four studies reported no significant effect on depressive symptoms (Gross et al., 1995; Bayer et al., 2010; Homem et al., 2015; Chang et al., 2015). One study reported that the opposite occurred, with the control group having a significant decrease in depressive symptoms compared with the intervention group (p = 0.04) (Letourneau et al., 2011).
Anxiety
Three studies addressed maternal anxiety as shown on Tables 1 and 4. The DASS-21 (anxiety subscale) (Connell et al., 1997; Bayer et al., 2010) was used in two studies. The SCL-90-R was used by Farris et al. (2013). Only one study reported an improvement in anxiety symptoms (p = 0.02) (Connell et al., 1997).
Stress
Stress was measured in four studies, with results summarized on Table 4. Two used the DASS-21 (stress subscale) (Connell et al., 1997; Bayer et al., 2010) and two used the Parenting Stress Index short form (PSI-SF) (Gross et al., 1995; Doyle et al., 2017). A significant improvement on parental stress scores was reported in half of the studies (N = 2) (Gross et al., 1995; Connell et al., 1997).
Quality Assessment
Risk of bias was assessed for all studies using the Cochrane Collaboration risk of bias tool as applicable (Table 5) (Higgins et al., 2011). Sequence generation reporting bias was low in all but two studies where reporting was unclear (Gross et al., 1995; Homem et al., 2015). Allocation concealment was reported clearly in seven studies (Bayer et al., 2010; Letourneau et al., 2011; Berkule et al., 2014; Homem et al., 2015; Chang et al., 2015; Doyle et al., 2017; Boyd et al., 2019). By virtue of the fact that these are studies where the participants and interventionist personnel were aware of the parenting intervention, blinding was virtually impossible and led to a high risk of bias in all but two studies (Niccols 2009; Doyle et al., 2017). Blinding of outcomes assessors for all outcomes occurred in only three studies (Niccols, 2009; Letourneau et al., 2011; Berkule et al., 2014) with the rest either not reported or at high risk for bias. Risk of bias in complete outcomes reporting was low with two studies assessed as high risk because of high drop-out rates (Connell et al., 1997; Boyd et al., 2019). All outcomes of interest that were included in the purpose or methods were also included in the results for a low risk of selective reporting.
Discussion
In this manuscript, we reviewed studies exploring maternal mental health symptoms (depression, anxiety, stress) as secondary outcomes following parenting interventions. Eleven relevant studies were included in the final review. Ten studies analyzed depressive symptoms, three included anxiety, and four included stress. The findings from the review demonstrate that there is mixed evidence for the potential of parenting interventions to improve maternal mental health symptoms. Studies that compared depressive symptoms before and after the parenting interventions which resulted in an improvement in depression scores were small, including less than 50 total participants (Boyd et al., 2019; Farris et al., 2013; Letourneau et al., 2011; Niccols, 2009) and the one study that reported improvement in anxiety and stress only had 21 participants (Connell et al., 1997). The final study that measured an improvement in stress was also small with a total of 23 families (Gross et al., 1995). The fact that none of the studies with larger sample sizes demonstrated improvements in maternal mental health measures leads to the conclusion that the current evidence does not support parenting interventions as a mechanism to improve maternal mental health. Overall, the studies included had low risk of bias, with the most significant concern being the challenge of blinding participation in a parenting intervention versus being in a control group. While the studies tested a variety of interventions, there were many similarities across them. The most common delivery method was face to face, but it is notable that the two studies using web-based interventions and one using a phone delivery intervention all reported significant improvement in maternal depressive symptoms compared to controls (Farris et al., 2013; Boyd et al., 2019). In addition, there was no consistent evidence of improvement in mental health symptoms with increased intensity or overall length of time of the delivery of the interventions.
Nor was there consistent evidence that efforts to overcome barriers to participation were effective. As an example, Boyd et al. (2019) went to great efforts, offering childcare, meals and transportation to participants enrolled in the face to face group and still had low participation compared to the web delivered services group. The multimodal parenting programs included in the Barlow et al. (2014) review also often included psychotherapies and additional types of support for mothers and families, all requiring significant resources in time and money from the provider perspective.
Although our review did not provide evidence that participating in parenting education programs also led to improved mental health symptoms, there was only 1 study that demonstrated an improvement in the control group. With a small sample size, it is also the only study that used peers who had a prior history of depression as interventionists (Letourneau et al., 2011). Therefore, we can confidently conclude that mothers’ mental health is not worsened by participation in these programs and given the limited energy for engagement when depressive symptoms are present, there is more potential for good than harm in doing so.
Limitations
While a comprehensive and reproducible search was conducted in all relevant databases, a search of gray literature was not included, therefore some studies not reported in mainstream peer-reviewed scientific publications may have been overlooked. Also, only studies in English were included which may have also led to overlooking relevant studies. The heterogeneity of the interventions and the outcome measures precluded a meta-analysis of the results, limiting the strength of the review to a qualitative assessment.
Implications for Practice
Although it has been shown that multi-modal group parenting interventions can improve maternal mental health symptoms (Barlow et al., 2014), we need to continue to identify, implement and evaluate interventions that can actually be maintained in the long term. We need low cost interventions that require few resources and can be delivered in a sustainable way. Providers have a limited amount of time; organizations, particularly public ones, often have limited resources to provide these services. Additionally, mothers have numerous demands on their time and must prioritize engagement based on personal circumstances, including their child’s needs, family and work needs and often lastly their own mental health needs. Therefore, providers and researchers may wish to try and engage mothers, particularly those mothers with depressive symptoms in whatever means they can. If that means through a parenting intervention focused on the child’s needs, then encourage that, because it may be the first step towards improving maternal mental health.
Not surprisingly, some of the studies included in this review reported challenges with recruitment and retention of mothers with symptoms of depression. Others have also reported on similar difficulties (Hughes-Morley et al., 2015; Tryphonopoulos and Letourneau, 2015). Consideration must be given to the expectations of engagement and energy expense or resource utilization from the mother’s point of view if research and practice are to build off what is already known. Another consideration is to include qualitative assessments of the intervention itself, the delivery method and the mother’s perception of helpfulness given the time and resources she spent on it. Qualitative assessment of perceived impact of maternal mental health symptoms on the mother within the context of her life is also needed to help determine the clinical significance of symptoms and symptom improvement not just the statistically significant ones.
More research is needed to continue to explore technology-based options for intervention. For example, in addition to noting improvement in mental health symptoms, the studies that provided interventions that were not face to face, but web-based, also had better or equal attendance/retention in the intervention groups compared to the face to face groups (Farris et al., 2013; Boyd et al., 2019). Given the high resource utilization from both the provider and participant perspectives for face to face programs, web-based delivery offers a potentially sustainable and more cost-effective opportunity and indicates a promising area for further exploration.
Conclusion
Based on the included studies there is not consistent evidence to recommend parenting programs as an intervention to improve maternal mental health symptoms. However, there is a preponderance of evidence that participation in parenting programs does not worsen maternal mental health symptoms and some encouraging evidence that alternative delivery methods, beyond face to face, could lead to more financially feasible and sustainable models of delivery of these types of interventions in the future.
References
Barlow, J., Smailagic, N., Huband, N., et al. (2014). Group-based parent training programmes for improving parental psychosocial health. Cochrane Database Systematic Review. https://doi.org/10.1002/14651858.CD002020.pub4
Bayer, J. K., Hiscock, H., Ukoumunne, O. C., et al. (2010). Three-year-old outcomes of a brief universal parenting intervention to prevent behaviour problems: Randomised controlled trial. Archives of Disease in Childhood, 95, 187–192. https://doi.org/10.1136/adc.2009.168302
Beeber, L., Holditch-Davis, D., Belyea, M., et al. (2004). In-home intervention for depressive symptoms with low-income mothers of infants and toddlers in the United States. Health Care for Women International, 25, 561–580. https://doi.org/10.1080/07399330490444830
Beeber, L. S., Holditch-Davis, D., Perreira, K., et al. (2010). Short-term in-home intervention reduces depressive symptoms in early head start Latina mothers of infants and toddlers. Research in Nursing & Health, 33, 60–76. https://doi.org/10.1002/nur.20363
Berkule, S. B., Cates, C. B., Dreyer, B. P., et al. (2014). Reducing maternal depressive symptoms through promotion of parenting in pediatric primary care. Clinical Pediatrics (Phila), 53, 460–469. https://doi.org/10.1177/0009922814528033
Boyd, R. C., Price, J., Mogul, M., et al. (2019). Pilot RCT of a social media parenting intervention for postpartum mothers with depression symptoms. Journal of Reproductive and Infant Psychology, 37, 290–301. https://doi.org/10.1080/02646838.2018.1556788
Chang, S. M., Grantham-McGregor, S. M., Powell, C. A., et al. (2015). integrating a parenting intervention with routine primary health care: A cluster randomized trial. Pediatrics, 136, 272–280. https://doi.org/10.1542/peds.2015-0119
Connell, S., Sanders, M. R., & Markie-Dadds, C. (1997). Self-directed behavioral family intervention for parents of oppositional children in rural and remote areas. Behavior Modification, 21, 379–408. https://doi.org/10.1177/01454455970214001
Doyle, O., Delaney, L., O’Farrelly, C., et al. (2017). Can early intervention improve maternal well-being? Evidence from a randomized controlled trial. PLoS ONE, 12, e0169829. https://doi.org/10.1371/journal.pone.0169829
Farris, J. R., Bert, S. S. C., Nicholson, J. S., et al. (2013). Effective intervention programming: Improving maternal adjustment through parent education. Administration and Policy and Mental Health Services Research, 40, 211–223. https://doi.org/10.1007/s10488-011-0397-1
Fihrer, I., McMahon, C. A., & Taylor, A. J. (2009). The impact of postnatal and concurrent maternal depression on child behaviour during the early school years. Journal of Affective Disorders, 119, 116–123. https://doi.org/10.1016/j.jad.2009.03.001
Gaynes, B. N., Gavin, N., Meltzer-Brody, S., et al. (2005). Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evidence Report/Technology Assessment (Summary) 1–8.
Goodman, J. H., Watson, G. R., & Stubbs, B. (2016). Anxiety disorders in postpartum women: A systematic review and meta-analysis. Journal of Affective Disorders, 203, 292–331. https://doi.org/10.1016/j.jad.2016.05.033
Grace, S. L., Evindar, A., & Stewart, D. E. (2003). The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Archives of Women’s Mental Health, 6, 263–274. https://doi.org/10.1007/s00737-003-0024-6
Gross, D. (1989). Implications of maternal depression for the development of young children. Image: The Journal of Nursing Scholarship, 21, 103–107. https://doi.org/10.1111/j.1547-5069.1989.tb00108.x
Gross, D., Fogg, L., & Tucker, S. (1995). The efficacy of parent training for promoting positive parent–toddler relationships. Research in Nursing & Health, 18, 489–499. https://doi.org/10.1002/nur.4770180605
Hay, D. F., Pawlby, S., Angold, A., et al. (2003). Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology, 39, 1083–1094. https://doi.org/10.1037/0012-1649.39.6.1083
Higgins, J. P. T., Altman, D. G., Gotzsche, P. C., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928–d5928. https://doi.org/10.1136/bmj.d5928
Hoffman, C., Dunn, D. M., & Njoroge, W. F. M. (2017). Impact of postpartum mental illness upon infant development. Current Psychiatry Reports, 19, 100. https://doi.org/10.1007/s11920-017-0857-8
Homem, T. C., Gaspar, M. F., Santos, M. J. S., et al. (2015). Incredible years parent training: does it improve positive relationships in portuguese families of preschoolers with oppositional/defiant symptoms? Journal of Child and Family Studies, 24, 1861–1875. https://doi.org/10.1007/s10826-014-9988-2
Hughes-Morley, A., Young, B., Waheed, W., et al. (2015). Factors affecting recruitment into depression trials: Systematic review, meta-synthesis and conceptual framework. Journal of Affectice Disorders, 172, 274–290
Ko, J. Y., Rockhill, K. M., Tong, V. T., et al. (2017). Trends in postpartum depressive symptoms—27 states, 2004, 2008, and 2012. MMWR. Morbidity and Mortality Weekly Report, 66, 153–158. https://doi.org/10.15585/mmwr.mm6606a1
Letourneau, N., Stewart, M., Dennis, C.-L., et al. (2011). Effect of home-based peer support on maternal-infant interactions among women with postpartum depression: A randomized, controlled trial. International Journal of Mental Health and Nursing, 20, 345–357. https://doi.org/10.1111/j.1447-0349.2010.00736.x
Long, M. M., Morgan, F. G., Wilkes, C. A., et al. (2018). Screening rates, elevated risk, and correlates of postpartum depression in an obstetric population [28O]. Obstetrics and Gynecology, 131, 170S. https://doi.org/10.1097/01.AOG.0000533163.70256.b2
Lovejoy, M. C., Graczyk, P. A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20, 561–592. https://doi.org/10.1016/S0272-7358(98)00100-7
McKechnie, A. C., Waldrop, J., Matsuda, Y., et al. (2018). Mothers’ perspectives on managing the developmental delay of a child with considerations for contextual influences and maternal functioning. Journal of Family Nursing, 24, 405–442. https://doi.org/10.1177/1074840718780474
Niccols, A. (2009). Immediate and short-term outcomes of the ‘COPEing with Toddler Behaviour’ parent group. Journal of Child Psychology and Psychiatry, 50, 617–626. https://doi.org/10.1111/j.1469-7610.2008.02007.x
O’Hara, M. W. (2009). Postpartum depression: What we know. Journal of Clinical Psychology, 65, 1258–1269. https://doi.org/10.1002/jclp.20644
Righetti-Veltema, M., Conne-Perréard, E., Bousquet, A., & Manzano, J. (2002). Postpartum depression and mother–infant relationship at 3 months old. Journal of Affective Disorders, 70, 291–306. https://doi.org/10.1016/S0165-0327(01)00367-6
Ross, L. E., & McLean, L. M. (2006). Anxiety disorders during pregnancy and the postpartum period. Journal of Clinical Psychiatry, 67, 1285–1298. https://doi.org/10.4088/JCP.v67n0818
Smith-Nielsen, J., Tharner, A., Krogh, M. T., & Vaever, M. S. (2016). Effects of maternal postpartum depression in a well-resourced sample: Early concurrent and long-term effects on infant cognitive, language, and motor development. Scandinavian Journal of Psychology, 57, 571–583. https://doi.org/10.1111/sjop.12321
Tryphonopoulos, P. D., & Letourneau, N. (2015). Challenges and opportunities in recruitment of depressed mothers: lessons learned from three exemplar studies. Annals of Psychiatry and Mental Health, 3, 1022
Wheeler, A., Hatton, D., Reichardt, A., & Bailey, D. (2007). Correlates of maternal behaviours in mothers of children with fragile X syndrome. Journal of Intellectual Disability Research, 51, 447–462. https://doi.org/10.1111/j.1365-2788.2006.00896.x
Acknowledgement
Dr. Salomon was supported by the University of California San Francisco, School of Nursing’s Institutional Training Grant (T32) #T32NR016920.
Author information
Authors and Affiliations
Contributions
JW developed the idea for the review, EM performed the literature search and JW, MB and RS performed the data analysis. All authors participated in the drafting and critical revision of the work and approved the final submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Waldrop, J., Baker, M., Salomon, R. et al. Parenting Interventions and Secondary Outcomes Related to Maternal Mental Health: A Systematic Review. Matern Child Health J 25, 870–880 (2021). https://doi.org/10.1007/s10995-021-03130-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-021-03130-6