Abstract
Objective
The purpose of this health system’s study is to assess the availability of Emergency Obstetric Care (EmOC) services in birthing centres in Taplejung District of eastern Nepal.
Methods
A cross-sectional survey was conducted in 2018 in all 16 public health facilities providing delivery services in the district. Data collection comprised: (1) quantitative data collected from health workers; (2) observation of key items; and (3) record data extracted from the health facility register. Descriptive statistics were used to calculate readiness scores using unweighted averages.
Results
Although key health personnel were available, EmOC services at the health facilities assessed were below the minimum coverage level recommended by the World Health Organisation. Only the district hospital provided the nine signal functions of Comprehensive EmOC. The other fifteen had only partially functioning Basic EmOC facilities, as they did not provide all of the seven signal functions. The essential equipment for performing certain EmOC functions was either missing or not functional in these health facilities.
Conclusions for Practice
The Ministry of Health and Population and the federal government need to ensure that the full range of signal functions are available for safe deliveries in partially functioning EmOC health facilities by addressing the issues related to training, equipment, medicine, commodities and policy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Very few studies have described the infrastructure, human resources, drugs, equipment of birthing centres, BEmOC and CEmOC sites in Nepal. However, these studies have focused on district-level hospitals that provide CEmOC services only, or limited to community-based birthing centres (without BEmOC or CEmOC).
What this study adds? This study provides detailed information on the availability of equipment, medicines and commodities along with a readiness to provide BEmOC and CEmOC services in all birthing centres of Taplejung District. Besides, this study gives additional information on the reasons for not performing particular EmOC signal functions.
Introduction
Maternal and neonatal mortality are major public health problems worldwide and in Nepal. Despite substantial progress in reducing the Maternal Mortality Ratio (MMR) in Nepal from 539 to 239 maternal deaths per 100,000 between 1996 and 2016 (Ministry of Health et al. 2017a; Pradhan et al. 1997), the MMR was the second-highest in South-East Asia after Myanmar (WHO 2019). The neonatal mortality rate which was stagnant at 33 deaths per 1000 live births for almost a decade (2001–2010) (Ministry of Health and Population et al. 2007, 2012) had declined to 21 deaths per 1000 live births in 2016 (Ministry of Health et al. 2017a).
The availability of Emergency Obstetric Care (EmOC) service is essential for increasing access to quality obstetric and neonatal care (Mkoka et al. 2014), increasing utilisation of maternal care services and institutional delivery (Rana et al. 2007), and ultimately reducing maternal and neonatal deaths (WHO et al. 2009). The availability of EmOC also indicates health system readiness to manage pregnancy and childbirth complications (Paxton et al. 2006). Studies have shown that with EmOC in place, up to 60% of maternal deaths and 85% of intrapartum-related neonatal deaths could be averted per year (Lawn et al. 2009).
The Government of Nepal is continuing to expand the availability and access to EmOC through public and private health facilities as mandated strongly by policies and strategies (Ministry of Health 2017, 2016b; Family Health Division 2006, 2002). The availability of EmOC demands a skilled birth attendant (SBA) and a provision of seven ‘signal functions' for Basic EmOC (BEmOC): (1) administration of parenteral antibiotics; (2) administration of uterotonic drugs; (3) administration of parenteral anticonvulsants for pre-eclampsia and eclampsia; (4) manual removal of the placenta; (5) removal of retained products; (6) performing assisted vaginal delivery; and (7) basic neonatal resuscitation while Comprehensive EmOC (CEmOC) cover all seven BEmOC services plus (8) the ability to do a caesarean section; and (9) blood transfusion (WHO et al. 2009).
As such, health posts (HPs) and primary health care centres (PHCCs) are strengthened to provide 24/7 delivery services and hospitals to deliver CEmOC services in all 77 districts of Nepal. As a result, 2101 (43%) HPs and 188 (90%) PHCCs were providing services regularly, and a CEmOC site was established in 72 districts (but only 60 were functional) in 2018 (Ministry of Health and Population 2019). Nevertheless, nationally, the percentage of EmOC met need was only 38% in 2018 (Ministry of Health and Population 2019). The government’s safe motherhood and neonatal health long-term plan (2006–2017) was to have delivery services in 70% of HPs, BEmOC services in 80% of PHCCs, and CEmOC service in 60 districts by 2017 (Family Health Division 2006).
Very few studies have described the availability of human resources, medicines, and equipment to provide EmOC services in Nepal (Ministry of Health et al. 2017a, b; Pradhan et al. 2010). Studies that have reported on the readiness of health facilities have focused on district-level hospitals that provide CEmOC services only (Devkota et al. 2011) or limited to community-based birthing centres (without BEmOC and CEmOC) (Family Health Division 2014).
Currently, expansion and quality improvement of maternal and neonatal health service delivery at remote areas are being tested in Taplejung district (Ministry of Health 2016a). However, relatively little is known regarding the situation and readiness of health facilities to provide EmOC locally. Efforts to scale up maternal health services in this remote district and achieve the related sustainable development goals (SDGs) have drawn attention to the need for evidence about service availability and readiness of birthing centres. Hence, our study aims to assess what birthing centres exist and how ready these health facilities are to provide EmOC services in Taplejung District.
Methods
Study Area and Context
The study was conducted in Taplejung; one of the remote mountainous districts in eastern Nepal. In 2016, the total number of women of reproductive age (15–49 years) was 37,965, the expected pregnancies and live births were 3478 and 2950, respectively (Ministry of Health 2016a). Sixty-two health facilities (excluding private pharmacies and clinics) were providing maternal and newborn care services at the time of the survey. Of these health facilities, 61 were public (one District Hospital, two PHCCs, 50 HPs and eight community health units) and one was a private hospital.
According to the district health system, seven auxiliary nurse midwives (ANMs) (four non-SBA, three SBA), two operation theatre trained nurses, one anaesthesia doctor/assistant, two obstetrics/gynaecologists, two medical officers, and nine paramedics in a district hospital provide CEmOC services. Paramedics in Nepal includes health assistant (HA), auxiliary health worker (AHW), senior auxiliary health worker (Sr. AHW), laboratory technologist/officer/technician/assistant, radiographer, and darkroom assistant. Similarly, in PHCCs four paramedics (one HA, two AHWs/Sr.AHW, one laboratory technician/assistant), four ANMs (two non-SBAs, two SBAs) and one medical officer provide maternal and newborn care services. In HP, which is a lower level of a healthcare facility in the Nepalese health system, two ANMs (at least one SBA in a health facility providing a delivery service) and three paramedics (one HA, two AHWs/Sr.AHW) provide health services.
Selection of the Health Facilities
The survey involved all 16 public health facilities providing delivery services in the district viz., one District Hospital (15 bedded) designated to provide CEmOC, two PHCCs designated to provide BEmOC and 13 HPs designated to provide normal delivery services (Supplementary Fig. S1).
Study Design and Data Collection
A cross-sectional health facility survey was conducted in 2018 using three data collection methods. First, data enumerators visited 16 birthing centres and collected data using a structured survey tool. We used the core service availability and readiness assessment (SARA) questionnaire; the validated tool that has been designed to assess and monitor the service availability and readiness of health facilities (WHO 2015).
Pre-testing of the survey questionnaire was done in two birthing centres of a neighbouring district. Following the pre-testing (van Teijlingen and Hundley 2005), adjustments were made to the questionnaire to account for the information gained, resulting in the standard core questionnaire adapted for the district. Two enumerators and one field supervisor were mobilised to collect the data. The data collectors and field supervisor received one-day training before data collection. Data collectors obtained written informed consent in the local language before collecting the data from each concerned facility in-charge or nurse.
Secondly, data collectors observed the essential items that allowed us to determine the availability and the condition of equipment, medicines and commodities for EmOC. Finally, we extracted data from the health management information systems (HMIS) register of the included health facilities to determine the utilisation of EmOC signal functions and other maternal and newborn care services.
The ethical review board of the Nepal Health Research Council approved this study (Reg. No. 435/2017) in December 2017.
Data Management and Analysis
The data collected on the paper questionnaire were checked for accuracy, completeness and consistency before entering electronically into Census and Survey Processing System (CSPro) Version 6.3 (WHO 2015). The complete data set was later analysed using SPSS version 24.
Descriptive statistics were used to assess the availability of EmOC services measured across domains (staff and guidelines, equipment, diagnostics (only in District Hospital), and medicines and commodities). The availability of EmOC services was also measured by determining the number of health facilities that performed the complete set of required signal functions (seven for BEmOC and nine for CEmOC) in three months before the assessment. Any facility providing at least one of the seven signal functions was considered as partially functioning BEmOC. Readiness scores were equal to the sum of the means that were obtained for each tracer item in a domain, divided by the total number of items in the domain, and then multiplied by 100. Readiness scores were calculated using unweighted averages.
Results
Availability of Key Health Workers
Figure 1 shows the number of health workers at the time of assessment against the minimum staffing requirements for EmOC services. At the time of the survey, 117 health workers in 16 health facilities were providing health services. Paramedics represented the largest category of staff 43 (36.8%). SBA trained nursing staff, including ANMs 33 (28.2%) were the second-largest cadre of health workers in the birthing centres. Six medical officers (5.1%) were available in the District Hospital and PHCCs only. Obstetricians (2.6%) and anaesthesia doctor/assistant (1.7%) were available only in the District Hospital (Fig. 1). Noticeably, the number of health workers in each group surpassed the number of sanctioned posts except for paramedics.
Availability of EmOC Signal Functions
Only the District Hospital offered CEmOC services (Table 1). None of the PHCCs could provide all seven signal functions. All 13 HPs had carried out at least one of the seven signal functions in three months before assessment (partially functioning BEmOC). While the most commonly performed EmOC signal functions in three months before assessment by the surveyed health facilities was an administration of uterotonic drugs (oxytocin) (87.5%), the least performed BEmOC signal function was an administration of parenteral anticonvulsants (12.5%). None of the HPs studied ever used parenteral anticonvulsants. Similarly, none of the PHCCs expected to provide seven signal functions of BEmOC performed manual removal of placenta or assisted vaginal delivery during three months preceding the assessment.
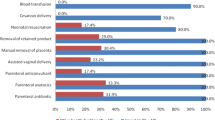
Reasons for not Performing EmOC Signal Functions
Except for the District Hospital, other surveyed health facilities did not perform a caesarean section and blood transfusion solely because of a policy that only district hospitals and higher-level health facilities with a recommended infrastructure and trained providers to manage complicated deliveries can offer this service (Fig. 2). Although the reasons for not performing other seven signal functions were mixed, lack of case/patient requiring signal functions was predominant.
Percentage of Services Utilisation in EmOC Facilities
Overall, 62.7% (662) of all institutional births occurred in CEmOC facility in the fiscal year 2016/17 (Table 2). The percentage of SBA delivery was also higher in CEmOC facility 59.4% (538) compared to partially functioning BEmOC facilities 40.6% (368). However, partially functioning BEmOC facility had the highest percentage of first ANC visits 60.5% (617), fourth ANC visits 71.7%% (457) as per protocol (National Medical Standard for Reproductive Health Vol. II), pregnant women receiving tetanus and diphtheria vaccine 58.7% (535), iron and folic acid 58.1% (735) including women receiving de-worming tablets 56.8% (698).
A total of 94 obstetric complications were recorded at all surveyed health facilities; HP (20.2%), PHCCs (2.1%) and district hospital (77.7%). Postpartum haemorrhage (39.4%), pre-eclampsia/eclampsia (14.9%), puerperal sepsis (12.8%) and prolonged labour (12.8%) were the main obstetric complications (Table 2).
Availability of Selected Essential Equipment
Essential equipment for performing some EmOC functions was not available in all facilities (Table 3). Complete delivery packs, manual vacuum aspiration (MVA) kits, and blank partographs were equally available at 87.5% (14/16). Oxygen supply (18.8%) was the least common equipment in the surveyed health facilities. Overall, the availability of equipment varied depending on the type of health facility. Equipment was more frequently available in the District Hospital and PHCCs than in HPs.
Availability of Selected Essential Medicines and Commodities
Chlorhexidine gel, oxytocin, magnesium sulphate and intravenous solution with infusion set (without dextrose) were equally available at 87.5% (14/16) of health facilities on the day of the survey (Table 4). Gentamicin injection 31.3% (5/16) was least available in all health facilities offering EmOC included. While PHCCs lacked ampicillin injections, the District Hospital was deficient in xylocaine (lidocaine), blood supply and other essential medicines (e.g., halothane, thiopental).
Obstetric Service Readiness in Health Facilities
The overall readiness score was 76.8% for providing BEmOC, and the highest was for equipment (87.1%) and the lowest for staff and guidelines (51.3%) as shown in Fig. 3. A higher-level health facility (District Hospital) had a higher readiness score than a lower-level health facility (HP), 95.8% versus 74.0%. Figure 4 shows the overall readiness score to provide CEmOC was 70.0% and highest for staff and guidelines (100.0%) and diagnostics (100.0%), and the lowest for medicines and commodities (44.4%).
Overall facility readiness scores for BEmOC. Staff and guidelines included five tracer items: (1) Guidelines for essential childbirth care; (2) checklists and/or job-aids for essential childbirth care; (3) guidelines for essential newborn care; (4) staff trained in essential childbirth care; (5) staff trained in newborn resuscitation. Equipment included 14 tracer items: (1) emergency transport; (2) sterilization equipment; (3) examination light; (4) delivery pack; (5) suction apparatus (mucus extractor); (6) manual vacuum extractor; (7) vacuum aspirator or D&C kit (with speculum); (8) neonatal bag and mask; (9) delivery bed; (10) partograph; (11) gloves; (12) infant weighing scale; (13) blood pressure apparatus; (14) soap and running water OR alcohol-based hand rub. Medicines and commodities included six tracer items: (1) injectable uterotonic (oxytocin); (2) injectable ampicillin; (3) injectable gentamicin; (4) magnesium sulphate (injectable); (5) skin disinfectant (chlorhexidine); (6) intravenous solution with an infusion set
Overall facility readiness scores for CEmOC. Staff and guidelines included four tracer items: (1) guidelines for CEmOC; (2) staff trained in CEmOC; (3) staff trained in surgery; (4) staff trained in anaesthesia. Equipment included five tracer items: (1) anaesthesia equipment; (2) resuscitation table; (3) incubator; (4) oxygen; (5) spinal needle. Diagnostics included two tracer items: (1) blood typing; and (2) crossmatch testing. Medicines and commodities included nine tracer items: (1) blood supply sufficiency; (2) blood supply safety; (3) inj xylocaine; (4) epinephrine (injectable); (5) halothane (inhalation); (6) atropine (injectable); (7) thiopental (powder); (8) suxamethonium bromide (powder); and (9) ketamine (injectable)
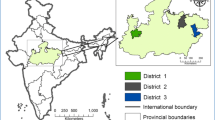
Geographic Distribution of EmOC Facilities
Access to EmOC services varied across the district. Only one available CEmOC facility was in Phungling Municipality (district headquarter). Partially functioning BEmOC facilities were mainly available in rural municipalities of South-East and South-West regions, as shown in Supplementary Fig. S1. All these health facilities were located in hilly areas with an elevation ranging between 1295 to 2484 m.
Discussion
This study provides detailed information on the availability of staff, equipment, medicines and commodities along with the readiness of birthing centres to provide EmOC services in Taplejung District. The District Hospital provided nine signal functions of CEmOC for 129,767 people at the time of the study. Other fifteen were found to be partially functioning BEmOC facilities, as they did not provide all the seven signal functions. The WHO handbook on monitoring EmOC recommends the minimum of five EmOC facilities with at least one CEmOC per 500,000 population (WHO et al. 2009). According to the standard set by the guideline, our study has shown that overall the minimum acceptable level of EmOC services in Taplejung has not been met, although, District Hospital offers CEmOC.
The District Hospital, as a consequence, was overcrowded with deliveries. The study found that in the fiscal year 2016/17, 62.7% of total institutional deliveries in the district took place in the District Hospital. The relatively higher percentage of women delivering in the District Hospital irrespective of a lower percentage of fourth ANC visits as per protocol (28.3%) than in partially functioning BEmOC (71.7%) has several explanations. First, the District Hospital handles most of the complicated cases referred from other health facilities within the district. In addition, as other partially functioning EmOC services were located mainly in the remote hilly areas, the pregnant women and their families due to remoteness and lack of comprehensive services including caesarean section may less prefer them (Anastasi et al. 2015; Bohren et al. 2014).
Most of the EmOC services in PHCCs are underutilised, which could be linked to the lack of necessary facilities such as operating theatre to handle complicated cases despite the availability of a trained SBA. The lower readiness of EmOC services in HPs may encourage women to deliver at home without SBA assistance (Roro et al. 2014). There may also be an increased risk of bypassing local birth centres and delivering at higher-level health facilities (Karkee et al. 2015).
Unlike the studies conducted in Nepal and other low- and middle-income countries (LMICs), our study found that Taplejung District has good availability of key health personnel for providing EmOC services. At the time of assessment, the number of SBAs, non-SBAs, ANMs and doctors surpassed the sanctioned post except for paramedics. The main reason behind the fulfilment of the sanctioned post was because the Government of Nepal had recruited short-term contracted health workers through the Public Service Commission during the time of the survey.
The overall readiness score to provide BEmOC in Taplejung (76.8%) was much higher than figures shown in other LMICs (Bintabara et al. 2019; Kanyangarara et al. 2018; Andriantsimietry et al. 2016). In Madagascar, district hospitals had a mean score of 60.4%, and basic health centres had 44.5% for BEmOC services in 2014 (Andriantsimietry et al. 2016). In Tanzania, the overall readiness score for BEmOC was 40.3% (Bintabara et al. 2019). A study that assessed the obstetric service readiness in 17 LMICs showed that the median percentage of facilities readiness to provide EmOC was 10% (Kanyangarara et al. 2018). However, the tracer items used by these studies were different from our study. We have included all tracer items across three domains for BEmOC and four domains for CEmOC as recommended by the SARA reference manual (WHO 2015).
A few HPs were performing assisted vaginal deliveries and manual removal of placenta, but PHCCs were not because of a lack of cases to perform these signal functions in the last three months in the PHCCs. The possible rationale for no cases in PHCCS might be due to shorter travel time or distance to the nearest referral/higher-level health facility (Khatri and Karkee 2018). The other reasons for unavailability of a case to perform signal functions may be the non-risk taking attitude of health workers. SBA trained nurses who are certified to perform the signal functions independently can do so only after evaluating that a patient meets the criteria and patients with serious complications would eventually be referred to higher-level health facilities. Consequently, health workers from HPs and PHCCs tend to refer pregnant women to a higher-level health facility than handling the deliveries themselves for fear of maternal and neonatal complications is justifiable. Availability of suitably trained cadre of health workers and equipment in the birthing centres but their fear of maternal and newborn complications and case referring attitude could be the subject of future study. In the future study, it would be useful to know what kind of case the HPs, and PHCCs refer to the higher-level health facilities.
In addition to the lack of cases as the main reason for not performing EmOC services, unavailability of essential equipment and medicine also remained vital. The study found that necessary equipment and medicines for performing some EmOC functions were either missing or not functional. For example, xylocaine was stocked out on the day of the survey and therefore not available in a caesarean section room of the District Hospital. The health personnel interviewed explained that they periodically experienced stock-out of medicine and equipment needed for removal of retained products and performing assisted vaginal delivery, including administration of parenteral antibiotics. The findings are consistent with evidence from studies conducted in India (Sabde et al. 2016), and Ethiopia (Ethiopian Public Health Institute et al. 2017).
Parenteral administration of anticonvulsant was the least performed signal function which is consistent with the findings from Nepal (Ministry of Health et al. 2017b), and other 17 LMICs (Kanyangarara et al. 2018). Similarly, the other signal functions least performed, i.e., removal of retained products by manual vacuum aspirations and assisted vaginal delivery (vacuum extraction) are similar to the findings of the study conducted in LMICs (MEASURE Evaluation PIMA 2016; Worku et al. 2013; Ameh et al. 2012) including Nepal (Ministry of Health et al. 2017b).
Limitations
This study, which involved a survey of health facilities, observation of key items and extraction of data from health facility register, has some limitations. Health workers might have been biased in providing information on the availability of the equipment, supplies and commodities to seek support and influence donor agencies working on the district. To limit this response bias, we chose to observe the essential items and further categorised as observed, reported not seen and not available. To avoid information bias, the respondent of the survey was either facility in-charge or maternal and newborn care service providers.
The data on service utilisation was extracted from the health facility register, i.e., HMIS, held by the health facilities, which is often criticised as being incomplete or poorly recorded. Nevertheless, we attempted to reduce this uncertainty by liaising with the maternity ward in-charge so that she could confirm the validity of the records.
As a cross-sectional study, the mere availability or unavailability of equipment, medicine and commodities at the time of survey may disguise situations when these items were generally available and were only missing at the time of the study and vice versa. In addition, we cannot report any cause and effect as the study provides only a snapshot of the availability and readiness of birthing centres in surveyed health facilities. The study does not include user behaviour as it falls outside the remit of the study objective. Another limitation was that this study does not measure service quality.
Conclusions
In Taplejung, EmOC services were below the minimum coverage level recommended by WHO, and the essential items for performing some EmOC functions were either missing or not functional. The Ministry of Health and Population need to upgrade the partially functioning BEmOC facilities to fully functioning BEmOC services by improving the supply chain of essential medicines and commodities (ampicillin, gentamicin, xylocaine, epinephrine), and emergency transport in all facilities providing delivery services. The National Health Training Centre needs to provide delivery and newborn care service guidelines (Nepal Medical Standard Volume III or Reproductive Health Clinical Protocol) to ensure that EmOC services are provided as per these national guidelines. Besides, the local level government needs to conduct subsequent periodic assessments to examine service standards and progress. The future study needs to focus on the understanding of EmOC service utilisation barriers (potentially geographic or financial).
References
Ameh, C., Msuya, S., Hofman, J., Raven, J., Mathai, M., & van den Broek, N. (2012). Status of emergency obstetric care in six developing countries five years before the MDG targets for maternal and newborn health. PLoS ONE,7(12), e49938.
Anastasi, E., Borchert, M., Campbell, O. M., Sondorp, E., Kaducu, F., Hill, O., et al. (2015). Losing women along the path to safe motherhood: Why is there such a gap between women’s use of antenatal care and skilled birth attendance? A mixed methods study in northern Uganda. BMC Pregnancy & Childbirth,15(1), 287.
Andriantsimietry, S. H., Rakotomanga, R., Rakotovao, J. P., Ramiandrison, E., Razakariasy, M. E. R., Favero, R., et al. (2016). Service availability and readiness assessment of maternal, newborn and child health services at public health facilities in Madagascar. African Journal of Reproductive Health,20(3), 149–158.
Bintabara, D., Ernest, A., & Mpondo, B. (2019). Health facility service availability and readiness to provide basic emergency obstetric and newborn care in a low-resource setting: Evidence from a Tanzania National Survey. British Medical Journal Open,9(2), e020608.
Bohren, M. A., Hunter, E. C., Munthe-Kaas, H. M., Souza, J. P., Vogel, J. P., & Gülmezoglu, A. M. (2014). Facilitators and barriers to facility-based delivery in low- and middle-income countries: A qualitative evidence synthesis. Reproductive Health,11(1), 71.
Devkota, M. G., Shakya, N., Pratap K. C., Dariang, M., Upadhyay, M. T., Karn, S., et al. (2011). Readiness of comprehensive obstetric and neonatal emergency care in Nepal. Kathmandu: National Health Sector Support Programme and Ministry of Health and Population.
Ethiopian Public Health Institute, Federal Ministry of Health, & Averting Maternal Death and Disability. (2017). Ethiopian emergency obstetric and newborn care (EmONC) assessment 2016. Ethiopia: Addis Ababa.
Family Health Division. (2002). National safe motherhood plan (2002–2017). Kathmandu: Family Health Division, Government of Nepal.
Family Health Division. (2006). National safe motherhood and newborn health-long term plan (2006–2017). Kathmandu: Family Health Division, Ministry of Health and Population, Government of Nepal.
Family Health Division. (2014). Results from assessing birthing centers in Nepal. Kathmandu: Family Health Division, Ministry of Health and Population, Government of Nepal.
Kanyangarara, M., Chou, V. B., Creanga, A. A., & Walker, N. (2018). Linking household and health facility surveys to assess obstetric service availability, readiness and coverage: Evidence from 17 low- and middle-income countries. Journal of Global Health,8(1), 010603.
Karkee, R., Lee, A. H., & Binns, C. W. (2015). Bypassing birth centres for childbirth: An analysis of data from a community-based prospective cohort study in Nepal. Health Policy and Planning,30(1), 1–7.
Khatri, R. B., & Karkee, R. (2018). Social determinants of health affecting utilisation of routine maternity services in Nepal: A narrative review of the evidence. Reproductive Health Matters,26(54), 32–46.
Lawn, J. E., Kinney, M., Lee, A. C., Chopra, M., Donnay, F., Paul, V. K., et al. (2009). Reducing intrapartum-related deaths and disability: Can the health system deliver? International Journal of Gynecology & Obstetrics,107(Suppl 1), S123–142.
MEASURE Evaluation PIMA. (2016). Health facility readiness to provide emergency obstetric and newborn care in Kenya: Results of a 2014 assessment of 13 Kenyan counties with high maternal mortality. Nairobi: MEASURE Evaluation PIMA, University of North Carolina at Chapel Hill.
Ministry of Health. (2016a). Annual Report, Department of Health Services 2071/2072 (2014/2015). Kathmandu: Ministry of Health, Government of Nepal.
Ministry of Health. (2016b). Nepal’s every newborn action plan. Kathmandu: Ministry of Health, Government of Nepal.
Ministry of Health. (2017). Nepal health sector strategy implementation plan 2016–2021. Kathmandu: Ministry of Health, Government of Nepal.
Ministry of Health, New ERA, & ICF. (2017a). Nepal demographic and health survey 2016. Kathmandu: Ministry of Health, Nepal.
Ministry of Health, New ERA, Nepal Health Sector Support Program (NHSSP), & ICF. (2017b). Nepal health facility survey 2015. Kathmandu: Ministry of Health, Government of Nepal.
Ministry of Health and Population. (2019). Annual report, department of health services 2074/2075 (2017/2018). Kathmandu: Ministry of Health and Population, Government of Nepal.
Ministry of Health and Population, New ERA, & ICF International Inc. (2012). Nepal demographic and health survey 2011. Kathmandu: Ministry of Health and Population, Nepal.
Ministry of Health and Population, New ERA, & Macro International Inc. (2007). Nepal demographic health survey 2006. Kathmandu: Ministry of Health and Population, Nepal.
Mkoka, D. A., Goicolea, I., Kiwara, A., Mwangu, M., & Hurtig, A. K. (2014). Availability of drugs and medical supplies for emergency obstetric care: Experience of health facility managers in a rural District of Tanzania. BMC Pregnancy & Childbirth,14(1), 108.
Paxton, A., Bailey, P., & Lobis, S. (2006). The United Nations process indicators for emergency obstetric care: Reflections based on a decade of experience. International Journal of Gynecology & Obstetrics,95(2), 192–208.
Pradhan, A., Aryal, R. H., Regmi, G., Ban, B., & Govindasamy, P. (1997). Nepal family health survey 1996. Kathmandu: Ministry of Health, New ERA, and Macro International Inc.
Pradhan, A., Suvedi, B. K., Barnett, S., Sharma, S. K., Puri, M., Poudel, P., et al. (2010). Nepal maternal mortality and morbidity study 2008/2009. Kathmandu: Family Health Division, Ministry of Health and Population, Government of Nepal.
Rana, T. G., Chataut, B. D., Shakya, G., Nanda, G., Pratt, A., & Sakai, S. (2007). Strengthening emergency obstetric care in Nepal: The women’s right to life and health project (WRLHP). International Journal of Gynecology & Obstetrics,98(3), 271–277.
Roro, M. A., Hassen, E. M., Lemma, A. M., Gebreyesus, S. H., & Afework, M. F. (2014). Why do women not deliver in health facilities: A qualitative study of the community perspectives in south central Ethiopia? BMC Research Notes,7(1), 556.
Sabde, Y., Diwan, V., Randive, B., Chaturvedi, S., Sidney, K., Salazar, M., et al. (2016). The availability of emergency obstetric care in the context of the JSY cash transfer programme in Madhya Pradesh, India. BMC Pregnancy & Childbirth,16(1), 116.
van Teijlingen, E., & Hundley, V. (2005). Pilot studies in family planning and reproductive health care. Journal of Family Planning and Reproductive Health Care,31(3), 219–221.
WHO. (2015). Service Availability and Readiness Assessment (SARA): An annual monitoring system for service delivery. Reference Manual. Version 2.2. Geneva: World Health Organization.
WHO. (2019). Maternal mortality estimates by country. Geneva: World Health Organization. Retrieved from https://apps.who.int/gho/data/view.main.1390?lang=en.
WHO, UNFPA, UNICEF, & AMDD. (2009). Monitoring emergency obstetric care: a handbook. Geneva: World Health Organization.
Worku, A. G., Yalew, A. W., & Afework, M. F. (2013). Availability and components of maternity services according to providers and users perspectives in North Gondar, northwest Ethiopia. Reproductive Health,10, 43–43.
Acknowledgements
The authors are grateful to Taplejung District Health Office authority for granting permission to conduct this study. The authors would also like to acknowledge the health workers who gave their valuable time to the study. The authors received no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Banstola, A., Simkhada, P., van Teijlingen, E. et al. The Availability of Emergency Obstetric Care in Birthing Centres in Rural Nepal: A Cross-sectional Survey. Matern Child Health J 24, 806–816 (2020). https://doi.org/10.1007/s10995-019-02832-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-019-02832-2