Abstract
Objective To assess LARC use trends among college women (18–24 years) and identify groups that have increased LARC use. Methods Data were extracted from the National College Health Assessment-II (NCHA-II) fall 2008–2013 surveys. Logistic regression statistics were used to assess LARC use. Results Although LARC use increased from 2008 to 2013 (aOR = 2.62; 95% CI 2.23–3.07), less than half of the sample (44%) reported using contraception at last vaginal sex. Only 2.5% of college women in this study reported using a LARC method; of LARC users, 90% reported using an intrauterine device. Nearly all sociodemographic factors were significantly associated with increases in LARC use including: age, sexual orientation, and insurance status. Conclusions LARC use significantly increased among college women. However, less effective methods such as condoms and short-acting reversible contraceptives are used more frequently. Promoting LARC use for women who desire to effectively prevent pregnancy can reduce unintended pregnancy and improve health outcomes for women while in college. Future work should examine the importance of individual and lifestyle factors that influence college women’s decision to choose a LARC method and seek to eliminate barriers to college women choosing a contraceptive method they believe works best for them.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
This study adds to the current literature regarding long-acting reversible contraceptive (LARC) use among college women. Findings suggest that college women are increasing their use of LARC, which is recommended by professional organizations such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists as the most effective reversible contraception available. Promoting LARC use for women who desire to effectively prevent pregnancy can reduce unintended pregnancy and improve health outcomes for women while in college.
Introduction
Unintended pregnancy in the U.S. has recently declined to 45% of all pregnancies (Finer and Zolna 2016). Yet, younger women (18–24 years) continue to have higher rates of unintended pregnancy overall (Finer and Zolna 2016; Martin et al. 2015) and have higher rates of unintended pregnancy resulting in childbirth compared to other age groups (Finer 2010). College women are at risk of unintended pregnancy due to unprotected and unplanned sex and multiple sexual partners (Fielder and Carey 2011; Turrisi et al. 2006). Among this population, unintended pregnancy can have serious and long-lasting consequences, such as decreased likelihood of college completion (Finer and Zolna 2011), reduced potential lifetime earnings, and lower overall health and wellness (Dehlendorf et al. 2010; Eisenberg et al. 2013). College attendance is also a significant period in the life course because it poses potential biopsychosocial benefits and risks that can alter women’s future health (Braveman 2014). Given the point in their educational careers, college women may desire to delay childbirth. Nonetheless, only 56% of college women used contraception during last vaginal sex (American College Health Association 2015). Furthermore, when college women used a form of contraception, they were more likely to use oral contraceptive pills or male condoms, compared to more effective methods, such as long-acting reversible contraception (LARC) (ACHA 2015).
LARC, which includes intrauterine devices (IUD) and the subdermal hormonal implant, can provide effective pregnancy prevention for 3–10 years (Cheng and Van Leuven 2015). Low rates of LARC use among young women exist even though LARC serves as one of the most effective forms of pregnancy prevention (Daniels et al. 2014; Kavanaugh et al. 2015a, b). Health promotion campaigns have long focused on oral contraceptive pills and condom use as the best options for young women (Jones et al. 2015); yet, these methods are inferior in effectiveness due to the necessity of consistent and correct use. Therefore, young women feel a false sense of protection against unintended pregnancy (Cheng and Van Leuven 2015) and overestimate the effectiveness of OCPs (Sundstrom et al. 2015). College women may face access and psychosocial barriers to choosing LARC, such as low knowledge and negative attitudes and beliefs about LARC (Hall et al. 2016). Additionally, clinicians may possess limited knowledge about LARC and report not knowing enough about methods to encourage young patients to use them, thus reducing patient’s access to contraception-related information and services (American College of Obstetricians and Gynecologists 2012; Cheng and Van Leuven 2015; Fleming et al. 2010; Harper et al. 2008). Current guidance from the American Academy of Pediatrics (AAP 2014) and the American College of Obstetricians and Gynecologists (ACOG 2012) addresses consumers’ and clinicians’ reluctance to use LARC by formally recommending young women use LARC to prevent unintended pregnancies.
LARC use among U.S. women ages 15–44 has significantly increased from 8.6 to 11.6% over a 5 year span (Daniels et al. 2014). More specifically, across age, race, ethnicity and relationship status, LARC use increased while overall contraceptive use rates remained stable (Daniels et al. 2014). In general, LARC use appears to have increased among U.S. women, but little is known if similar trends are occurring among college women. Thus, the purpose of this study was to describe: (1) trends in LARC use among college women ages 18–24 years from 2008 to 2013 and (2) specific sub-groups of college women that have increased LARC use and those that may benefit from additional public health efforts.
Methods
Sample
This study explored LARC use trends among a sample of sexually active college women that completed the National College Health Assessment Survey-II (NCHA-II) (2008–2013). The NCHA-II survey is administered twice each year and is limited to institutions that opt-in by paying to participate. Institutions decide survey administration methods, which may explain variation in response rates by institution (19–36%) (ACHA n.d.). For fall 2013, the mean response rate was 20% (ACHA 2014). This study received an exempt status from the university’s Institutional Review Board.
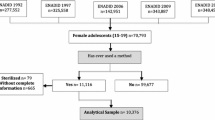
Data were from fall survey periods (2008–2013, N = 179,961) and restricted to females (N = 116,627) and those 18–24 years (N = 97,376). List-wise deletion was used for missing data, which accounted for < 4% of the sample. The final dataset included 92,578 women.
Measures
LARC use was defined as IUD or a subdermal hormonal implant use at last vaginal sex encounter. Additional categories of contraception use at last vaginal sex were operationalized as: any contraception (yes to any contraceptive method use), short-acting reversible contraception (SARC: pill, shot, patch, or ring), condom (male or female condom), and other contraception (diaphragm/cervical cap, contraceptive sponge, spermicide, fertility awareness, withdrawal, sterilization, or other method). Covariates that have been used in previous studies (Daniels et al. 2014; Ernst et al. 2015) were included in this analysis: age (18–20 and 21–24 years), race/ethnicity (white non-Hispanic, black non-Hispanic, Asian, multi-racial, other, Hispanic), sexual orientation (heterosexual, sexual minority), relationship status (not in relationship; in a relationship, not living together; in a relationship, living together; married/partnered; other), and insurance status (insured or not insured). NCHA modified race/ethnicity variables in 2011; therefore, these demographic variables are segmented into two time periods, 2008–2010 and 2011–2013.
Statistical Methods
Frequencies of contraceptive use were calculated by study year and bivariate regression analyses were used to assess contraceptive use trends. To evaluate trends of each contraceptive method, adjusted logistic regression models were estimated controlling for known factors around contraceptive use, such as effects of age, race/ethnicity, sexual orientation, relationship status and insurance status (Abraham et al. 2015; Finer et al. 2012; Peipert et al. 2011). To examine sociodemographic sub-group trends in LARC use, logistic regression models were utilized to assess the effect of year on LARC use in each stratum. Data were analyzed using SAS 9.4.
Results
Sample Characteristics
The majority of participants identified as non-Hispanic white (67%) and were between ages 18 and 20 years (67%). Women mostly identified as heterosexual (93%) and had health insurance (94%). More than half of women reported not being in a relationship (52%). In 2013, less than half of women reported using any contraception at last vaginal sex, 35% of women reported using SARC and 33% of women used a condom (Fig. 1). Overall, among contraception users, only 2.5% of college women reported using a LARC method (Table 1) and IUDs were used more than implants (90 vs. 10%, data not shown).
Contraception use among U.S. college women by year, NCHA-II 2008–2013. In 2013, less than half of women reported using any contraception at last vaginal sex, 35% of women reported using short-acting reversible contraception (SARC), 33% of women used a condom, 20% an “other” form of contraception such as barrier or other natural method, and 4% of women reported using a form of long-acting reversible contraception
Trends in Contraceptive Use
Condoms and any contraception did not significantly change in use from 2008 to 2013; however, SARC decreased, while other contraception and LARC increased. Specifically, LARC use significantly increased each year and doubled from 2008 to 2013. Data from fall 2013 showed that more college women reported LARC use compared to 2008 (aOR = 2.62 95% CI 2.23–3.07). In 2013, other contraceptive method use showed small, yet significant increases and LARC use significantly increased. There were no statistically significant changes in SARC and condom use over time after adjusting for the effects of covariates (Table 1).
LARC Use by Sociodemographic Sub-groups
Given the significant increase in LARC use between 2008 and 2013, a sub-group analysis was conducted to identify LARC trends among demographic sub-groups. This revealed LARC use significantly increased across sociodemographic factors (Table 2).
Race/Ethnicity
Among race categories, only women who identified as Asian or other race did not experience increases in LARC use. However, in 2011 women who identified as white, bi/multiracial or Hispanic had significant increases in LARC use compared to their counterparts in 2008. Those who identified as black were 2.5 times more likely to use LARC in 2013 compared to 2011.
Age
Overall, LARC use significantly increased among age categories; women ages 21–24 years were more likely to use LARC in 2013 than 2008 (OR = 3.23 95% CI 2.50–4.19) as were those ages 18–20 years (OR = 2.24 95% CI 1.83–2.75).
Sexual Orientation
Compared to 2008, heterosexual college women and sexual minority college women reported LARC use more in 2013. College women that identified as heterosexual were nearly two times more likely to report LARC use in 2013 compared to 2008; and college women who identified as a sexual minority were more than three times as likely to report using a LARC method.
Relationship Status
LARC use significantly increased among women in all relationship types from 2008 to 2013 except for those who were included in the other relationship category. Women who were not in a relationship were twice as likely to report LARC use in 2013 than 2008. Notably, those who were in a relationship and cohabiting were almost four times more likely to report LARC use in 2013 than 2008.
Insurance Status
Over time, women who were insured and those who were not insured showed higher levels of LARC use, and those who reported having no insurance were more than three times as likely to report using LARC in 2013 than 2008.
Discussion
We identified trends in LARC use among college women from years 2008 to 2013. Findings from this study demonstrated that LARC use has consistently increased among college women from 2008 to 2013. In 2013, college women were 2.6 times more likely to report using a LARC method at last vaginal sex compared to 2008. Additionally, less common contraceptive methods (e.g., diaphragm, cervical cap) had a slightly significant increase between 2008 and 2013; thus, suggesting college women are using non-hormonal methods to prevent pregnancy. SARC, condoms and any contraception either decreased or remained stable, which could indicate satisfaction among current contraception users or that users are switching to different methods.
Although LARC are recommended for young women (AAP 2014; ACOG 2012), results from this study show that oral contraceptive pills and male condoms are more commonly used. Data from NCHA fall 2013 showed that 54% of female respondents reported using a form of contraception at last vaginal sex (ACHA 2014), which is higher than the number using contraception in this sample. In general, LARC use lags behind these more easily accessible methods as college women may be less familiar with them (Hall et al. 2015). LARC use for this study was measured as use of an IUD or implant; however, when women choose a LARC method, more often it is an IUD (Kavanaugh et al. 2015a, b), which is consistent with these findings. Conversely, some women, including younger women, may perceive IUDs as intrusive and a method previously restricted to women who had given birth, which may cause implants to seem like a more suitable alternative (Fleming et al. 2010).
Furthermore, this study revealed that LARC use has increased among specific sub-groups. Although black women in this current sample used LARC more in 2013 than 2010, use among black women was lower than other racial/ethnic groups. In fact, the proportion of LARC users in this sample is still below national averages for all racial and ethnic groups women in this study. LARC methods were only used by 4% of the sample and the overwhelmingly majority of LARC users identified as white. The current literature highlights differences in LARC use, which are typically negligible rates, among black women (Daniels et al. 2014; Kavanaugh et al. 2015a, b). Researchers have attributed potential differences by race and ethnicity to limited knowledge of LARC among black women, including those in college (Hall et al. 2016), cultural beliefs, and potential medial mistrust (Rocca and Harper 2012). Future research exploring the psycho- and socio-cultural barriers to LARC use is needed.
Current rates of LARC use among young women are still low as compared to older women in the general population (Daniels et al. 2014). This study found that < 5% of college women in 2013 were using a LARC method at last intercourse, which is fairly consistent with 5% of women ages 15–24 years who were using a LARC method 2011–2013 (Daniels et al. 2014). Older women 25–34 years had nearly double (11.1%) the LARC use rates of younger women included in the same sample (Daniels et al. 2014). The age range of women in this sample is less robust than in studies of the general population, yet we see a difference in LARC use by age. We might assume that older college women may have longer term and more stable relationships than younger women for which LARC may be more suitable to them. Previous research on pregnancy ambivalence has shown that although young women may want to prevent pregnancy they may think LARC is “too permanent” or too effective a method (Higgins 2017). Furthermore, women believed that LARC was too much of a commitment for a person who was not in a serious relationship (Higgins 2017). Other researchers have described that younger women may also prefer using coitus-dependent methods or that they may favor methods that they can discontinue independent of a provider (Sundstrom 2012). These preferences for contraception may vary by relationship status and other romantic and personal factors (i.e. woman’s perceived life stage or pregnancy ambivalence) that were not assessed in this study given the limitations of the dataset.
Age may also influence women’s knowledge and sexual and reproductive health literacy. Like women, in the general population, those in college may have low health literacy related to contraception. Women may overestimate the efficacy of less effective methods such as SARC methods and have misconceptions about less familiar methods, such as LARC. In a sample of college women, the majority of women incorrectly believed that IUDs can cause abortion if a woman became pregnant and that IUDs can lead to infertility (Hall et al. 2016). Findings from other studies substantiate claims related to young women’s misconceptions about LARC methods (Brown et al. 2013; Sundstrom et al. 2015). Regarding relationship status, women not in a relationship, women in relationships and not cohabiting with partners, women cohabiting with partners, and married women reported increased rates of LARC use. Studies on LARC use have consistently shown that cohabitation with sex partners is significantly associated with LARC use (Finer and Zolna 2016; Jones et al. 2015; Kavanaugh et al. 2015a, b). While cohabiting women are more likely to use LARC than their counterparts in other types of relationships (Kavanaugh et al. 2015a, b), they are also more likely to experience unintended pregnancy than women in different relationships (Finer and Zolna 2016). In a study that assessed effective contraception use and continuation, women who were in longer term relationships were more likely to use effective methods than women in casual relationships (Upadhyay et al. 2016). Additionally, college women in relationships are also less likely to use LARC methods with condoms (dual use) (Thompson et al. 2017). Monogamy is a protective factor against the risk of sexually transmitted infections, however, multiple sex partners and serial monogamy could increase a woman’s risk (Fielder and Carey 2011; Kelley et al. 2003). In the current study, partnered women of all relationship types experienced increased rates of LARC use, including women not in relationships who may engage in casual sex and hook-ups (Fielder and Carey 2011). Therefore, providers should assess women’s risk of unintended pregnancy and STIs regardless of relationship status.
Lastly, much of the literature cites lack of insurance as a barrier to LARC use, which may be mitigated by the increasing number of public and private funding mechanisms available to make LARC methods more accessible and affordable to at-risk and disadvantaged women (Peipert et al. 2011; Ricketts et al. 2014). Pilot projects and feasibility studies, which aimed to increased access to contraception, particularly LARC, diminished or reduced cost barriers for reproductive-age women thus increasing the number of women choosing LARC (Dehlendorf et al. 2010; Eisenberg et al. 2013; Ricketts et al. 2014). College women may face financial constraints, which may make LARC use less likely. Furthermore, having insurance does not ensure access to LARC on campus as some on-campus health clinics may not accept students’ insurance. However, among this sample of college women, LARC use rates increased regardless of insurance status.
This study has its limitations including self-report data, which may present issues related to social desirability and accuracy of students’ recall. Only colleges and universities that paid to participate in the surveillance system were included in this study, which introduced sampling bias and limited the generalizability of study findings to all higher education institutions (Rahn et al. 2016). Additionally, these data did not provide information as to when women had a LARC method inserted, which could have occurred prior to college attendance.
Notwithstanding the above limitations, this study fills a gap in the research and describes trends in LARC use among a population at risk for unintended pregnancy. With a large majority of young adult women attending college, colleges and student health service departments have an opportunity to promote positive sexual and reproductive health outcomes for college women (Cheng and Van Leuven 2015) but may first need to address barriers to LARC information and access. Healthy Campus 2020’s student objectives aim to improve family planning for college women by reducing unintended pregnancy and increasing number of students who use contraception (ACHA 2012). Currently, limited data exists around structural and institutional barriers to contraception for college women and their partners. One study showed that 70% of colleges surveyed reported having a student health center on site and nearly 20% reported offering LARC to its students (Habel et al. 2018). Regional differences in contraceptive access for college women could diminish if colleges and universities are equipped to provide comprehensive and timely contraceptive services. When institutions are unable to provide the full range of necessary services, collaborations between community-based providers or local health departments could augment service delivery. Additionally, barriers to LARC use persist and future interventions should consider how to appropriately educate college women about contraceptive options, increase affordability and access to LARC methods, and incorporate patient-centered strategies into contraceptive counseling (Cheng and Van Leuven 2015).
This study adds to the current literature regarding LARC use among college women. College attendance presents opportunities to provide targeted services to young women and improve health and wellness outcomes across the life course. Information is needed to assess additional factors that influence college women’s decision to use LARC and strategies to address misinformation and misconceptions that may persist throughout this population. Findings from this study could also have policy implications for colleges to offer and expand women’s access to contraceptive information and services on campus. Ultimately, future work should seek to examine and eliminate barriers to college women choosing a contraceptive method they believe works best for them.
References
Abraham, M., Zhao, Q., & Peipert, J. F. (2015). Young age, nulliparity, and continuation of long-acting reversible contraceptive methods. Obstetrics & Gynecology, 126(4), 823–829. https://doi.org/10.1097/AOG.0000000000001036.
American Academy of Pediatrics. (2014). Contraception for adolescents. Pediatrics, 134(4), e1244–e1256. https://doi.org/10.1542/peds.2014-2299.
American College Health Association. (2012). Student objectives. Retrieved January 3, 2017, from https://www.acha.org/HealthyCampus/HealthyCampus/Student_Objectives.aspx.
American College Health Association. (2014). American College Health Association—National College Health Assessment II: Reference group data report, fall 2013. Hanover, MD: American College Health Association.
American College Health Association. (2015). Spring 2015 reference group executive summary. Retrieved December 11, 2016, from http://www.acha-ncha.org/docs/NCHA-II_WEB_SPRING_2015_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf.
American College Health Association. (n.d.). American College Health Association National College Health Assessment. Retrieved December 21, 2016, from http://www.acha-ncha.org/.
American College of Obstetricians and Gynecologists. (2012). Adolescents and long-acting reversible contraception: Implants and intrauterine devices. ACOG Committee Opinion, 120(539), No. 539. https://doi.org/10.1097/AOG.0b013e3182723b7d.
Braveman, P. (2014). What is health equity: And how does a life-course approach take us further toward it? Maternal and Child Health Journal, 18(2), 366–372. https://doi.org/10.1007/s10995-013-1226-9.
Brown, M. K., Auerswald, C., Eyre, S. L., Deardorff, J., & Dehlendorf, C. (2013). Identifying counseling needs of nulliparous adolescent intrauterine contraceptive users: A qualitative approach. Journal of Adolescent Health, 52(3), 293–300. https://doi.org/10.1016/j.jadohealth.2012.07.004.
Cheng, S.-C. J., & Van Leuven, K. A. (2015). Intrauterine contraception and the facts for college health. The Journal for Nurse Practitioners, 11(4), 417–423. https://doi.org/10.1016/j.nurpra.2014.10.029.
Daniels, K., Daugherty, J., & Jones, J. (2014). Current contraceptive status among women aged 15–44: United States, 2011–2013. NCHS Data Brief, (173), 1–8. https://www.ncbi.nlm.nih.gov/pubmed/25500343.
Dehlendorf, C., Rodriguez, M. I., Levy, K., Borrero, S., & Steinauer, J. (2010). Disparities in family planning. American Journal of Obstetrics & Gynecology, 202(3), 214–220. https://doi.org/10.1016/j.ajog.2009.08.022.
Eisenberg, D., McNicholas, C., & Peipert, J. F. (2013). Cost as a barrier to long-acting reversible contraceptive (LARC) use in adolescents. The Journal of Adolescent Health, 52(4 Suppl), S59–S63. https://doi.org/10.1016/j.jadohealth.2013.01.012.
Ernst, S., Ela, E., McAndrew, L., Steele, M., Challa, S., Zowchowski, M. K., … Hall, K. S. (2015). Awareness and knowledge of long acting reversible contraception among young women on college campus. Journal of Pediatric and Adolescent Gynecology, 28(2), e62. https://doi.org/10.1016/j.jpag.2015.02.076.
Fielder, R., & Carey, M. P. (2011). Prevalence and characteristics of sexual hookups among first-semester female college students. Journal of Sex & Marital Therapy, 36(4), 1–10. https://doi.org/10.1080/0092623X.2010.488118.
Finer, L. B. (2010). Unintended pregnancy among U.S. adolescents: Accounting for sexual activity. The Journal of Adolescent Health, 47(3), 312–314. https://doi.org/10.1016/j.jadohealth.2010.02.002.
Finer, L. B., Jerman, J., & Kavanaugh, M. L. (2012). Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertility and Sterility, 98(4), 893–897. https://doi.org/10.1016/j.fertnstert.2012.06.027.
Finer, L. B., & Zolna, M. R. (2011). Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception, 84(5), 478–485. https://doi.org/10.1016/j.contraception.2011.07.013.
Finer, L. B., & Zolna, M. R. (2016). Declines in unintended pregnancy in the United States, 2008–2011. The New England Journal of Medicine, 374(9), 843–852. https://doi.org/10.1056/NEJMsa1506575.
Fleming, K. L., Sokoloff, A., & Raine, T. R. (2010). Attitudes and beliefs about the intrauterine device among teenagers and young women. Contraception, 82(2), 178–182. https://doi.org/10.1016/j.contraception.2010.02.020.
Habel, M. A., Coor, A., Beltran, O., Becasen, J., Pearson, W. S., & Dittus, P. (2018). The state of sexual health services at US colleges and universities. Journal of American College Health, 1–10.
Hall, K., Ela, E., Zochowski, M., Challa, S., McAndrew, L., Steel, M., … Ernst, S. (2015). College women’s knowledge of and perceived barriers to long-acting reversible contraceptive methods. Contraception, 92(4), 404–405. https://doi.org/10.1016/j.contraception.2015.06.198.
Hall, K. S., Ela, E., Zochowski, M. K., Caldwell, A., Moniz, M., McAndrew, L., … Ernst, S. (2016). “I don’t know enough to feel comfortable using them:” Women’s knowledge of and perceived barriers to long-acting reversible contraceptives on a college campus. Contraception, 93(6), 556–564. https://doi.org/10.1016/j.contraception.2016.02.007.
Harper, C. C., Blum, M., de Bocanegra, H. T., Darney, P. D., Speidel, J. J., Policar, M., & Drey, E. A. (2008). Challenges in translating evidence to practice: The provision of intrauterine contraception. Obstetrics & Gynecology, 111(6), 1359–1369. https://doi.org/10.1097/AOG.0b013e318173fd83.
Higgins, J. A. (2017). Pregnancy ambivalence and long-acting reversible contraceptive (LARC) use among young adult women: A qualitative study. Perspectives on Sexual and Reproductive Health. https://doi.org/10.1363/psrh.12025.
Jones, R. K., Tapales, A., Lindberg, L. D., & Frost, J. (2015). Using longitudinal data to understand changes in consistent contraceptive use. Perspectives on Sexual and Reproductive Health, 47(3), 131–139. https://doi.org/10.1363/47e4615.
Kavanaugh, M., Jerman, J., & Finer, L. (2015a). Changes in use of long-acting reversible contraceptive methods among U.S. women, 2009–2012. Obstetrics & Gynecology, 126(5), 917–927. https://doi.org/10.1097/AOG.0000000000001094.
Kavanaugh, M., Jerman, J., & Finer, L. (2015b). Who uses long-acting reversible contraceptive methods in the United States, which methods do they use and who stops using them? Contraception, 92(4), 381. https://doi.org/10.1016/j.contraception.2015.06.110.
Kelley, S. S., Borawski, E. A., Flocke, S. A., & Keen, K. J. (2003). The role of sequential and concurrent sexual relationships in the risk of sexually transmitted diseases among adolescents. Journal of Adolescent Health, 32(4), 296–305.
Martin, J. A., Hamilton, B. E., Osterman, M. J., Curtin, S. C., & Matthews, T. J. (2015). Births: Final data for 2013. National Vital Statistics Reports, 64(1). http://www.ncbi.nlm.nih.gov/pubmed/25603115.
Peipert, J. F., Zhao, Q., Allsworth, J. E., Petrosky, E., Madden, T., Eisenberg, D., & Secura, G. (2011). Continuation and satisfaction of reversible contraception. Obstetrics & Gynecology, 117(5), 1105–1113. https://doi.org/10.1097/AOG.0b013e31821188ad.
Rahn, R. N., Pruitt, B., & Goodson, P. (2016). Utilization and limitations of the American College Health Association’s National College Health Assessment instrument: A systematic review. Journal of American College Health, 64(3), 214–237. https://doi.org/10.1080/07448481.2015.1117463.
Ricketts, S., Klingler, G., & Schwalberg, R. (2014). Game change in Colorado: Widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspectives on Sexual and Reproductive Health, 46(3), 125–132. https://doi.org/10.1363/46e1714.
Rocca, C. H., & Harper, C. C. (2012). Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use? Perspectives on Sexual and Reproductive Health, 44(3), 150–158. https://doi.org/10.1363/4415012.
Sundstrom, B. (2012). Fifty years on “the pill”: A qualitative analysis of nondaily contraceptive options. Contraception, 86(1), 4–11. https://doi.org/10.1016/j.contraception.2011.10.016.
Sundstrom, B., Baker-Whitcomb, A., & DeMaria, A. L. (2015). A qualitative analysis of long-acting reversible contraception. Maternal and Child Health Journal, 19(7), 1507–1514. https://doi.org/10.1007/s10995-014-1655-0.
Thompson, E. L., Vamos, C. A., Griner, S. B., Logan, R., Vázquez-Otero, C., & Daley, E. M. (2017). Sexually transmitted infection prevention with long-acting reversible contraception: Factors associated with dual use. Sexually Transmitted Diseases. https://doi.org/10.1097/OLQ.0000000000000620.
Turrisi, R., Mallett, K. A., Mastroleo, N. R., & Larimer, M. E. (2006). Heavy drinking in college students: Who is at risk and what is being done about it? The Journal of General Psychology, 133(4), 401–420. https://doi.org/10.3200/GENP.133.4.401-420.
Upadhyay, U. D., Raifman, S., & Raine-Bennett, T. (2016). Effects of relationship context on contraceptive use among young women. Contraception, 94(1), 68–73. https://doi.org/10.1016/j.contraception.2016.02.025.
Acknowledgements
The opinions, findings, and conclusions presented/reported in this article are those of the authors and are in no way meant to represent the corporate opinions, views, or policies of the American College Health Association (ACHA). ACHA does not warrant nor assume any liabilities or responsibility for the accuracy, completeness, or usefulness of any information presented in this article. This work was presented at American Academy of Health Behavior 2016 Annual Meeting.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Logan, R.G., Thompson, E.L., Vamos, C.A. et al. Is Long-Acting Reversible Contraceptive Use Increasing? Assessing Trends Among U.S. College Women, 2008–2013. Matern Child Health J 22, 1639–1646 (2018). https://doi.org/10.1007/s10995-018-2560-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2560-8