Abstract
Objectives Studies examining risk factors for preterm birth (PTB) such as psychosocial stress are often focused on women with a history of PTB; however, most preterm babies are born to women with no history of preterm birth. Our objective was to determine if the relationship between psychosocial stress and PTB is altered by parity. Non-Hispanic black (NHB) women have increased psychosocial stress and PTB; therefore, we further aimed to determine if race alters the relationship between psychosocial stress, parity, and PTB. Methods We performed a secondary analysis of the Healthy Pregnancy, Healthy Baby Study comparing pregnant women who were primiparous (first pregnancy), multiparous with history of preterm birth, or multiparous with history of term birth. Perceived stress, perceived racism, interpersonal support, John Henryism and self-efficacy were measured using validated instruments. Logistic regression was used to model the effect of psychosocial stress on PTB stratified by parity and race. Results The analysis entire cohort included 1606 subjects, 426 were primiparous, 268 had a history of presterm birth, and 912 had a history of term birth. In women with a history of term birth, higher self-efficacy was associated with lower odds of spontaneous PTB, and this association was amplified in NHB women. In women with a history of spontaneous PTB, John Henryism Active Coping was associated with lower odds of spontaneous PTB in the index pregnancy. Conclusions for Practice The relationship between psychosocial stress and PTB may be mediated by parity and race.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known on the subject? Women with a history of preterm birth are at risk for recurrence; however, most preterm babies are born to women with no history of preterm birth. Preterm birth is multifactorial and some studies suggest psychosocial stress may be a risk factor. What this study adds? Our findings suggest instruments for measuring psychosocial stress may be important tools for identifying multiparous women with a history of term birth who are at increased risk for preterm birth in their current pregnancy. These instruments may be especially relevant for NHB women who are high risk for preterm birth and psychosocial stress.
Introduction
Preterm birth is the leading cause of neonatal morbidity and mortality (Mathews and MacDorman 2013). Parity is one of the most powerful predictors of preterm birth. Women with history of preterm birth are at greatest risk, with a 30% chance of recurrence (Laughon et al. 2014; Mercer et al. 1999). Comparatively, the incidence of preterm birth in primiparous women (first pregnancy) is 10%, and women with a history of term birth have the lowest incidence at 4% (Dekker et al. 2012; Kazemier et al. 2014). Given the easily identifiable increased risk, many preterm birth prevention studies have focused solely on women with a history of preterm birth. However, these studies ignore the remaining majority of the pregnant population, namely primiparous women and women with a history of term birth. Although the risk of preterm birth is lower in these populations, when preterm birth occurs in these women, it is equally problematic. It is therefore imperative to include women with varying parities when examining PTB risk factors.
Multiple risk factors are associated with spontaneous preterm birth including maternal anatomic anomalies (e.g. short cervix, uterine anomalies), uterine distension from multi-fetal gestation, infection, behavioral factors (e.g. smoking, substance use), and psychosocial stress (Borg et al. 2013). Psychosocial stress encompasses anxiety derived from perceived (e.g. gender or racial discrimination) and tangible pressures (e.g. food scarcity or homelessness) across the life-course. Stress induces physiologic changes including elevations in cortisol releasing hormone (CRH), which leads to increases in prostaglandins and inflammatory cytokines, both of which are associated with uterine contractions and spontaneous preterm birth (Guendelman et al. 2008; Levine et al. 2016; Ruiz et al. 2016). Despite biologic plausibility, studies examining the impact of psychosocial stress on preterm birth have shown inconsistent results (Arbour et al. 2012; Khashan et al. 2009; Kramer et al. 2011, 2009), possibly due to the poorly characterized interaction between psychosocial stress, parity, and other risk factors.
Race may also alter the relationship between psychosocial stress, parity, and preterm birth. Non-Hispanic black (NHB) race is strongly associated with preterm birth, with 13.3% of NHB births occurring preterm compared to 9% in non-Hispanic white (NHW) women(“March of Dimes 2017 Premature Birth Report Card.”). Although there are likely multiple factors leading to the race disparity in preterm birth, NHB pregnant women, on average, have higher psychosocial stress and unique stressors compared with other racial and ethnic groups (Dole et al. 2004; Grobman et al. 2016; Kramer et al. 2011; Lu and Chen 2004). Therefore the relationship between psychosocial stress and parity may be amplified in NHBs.
Our primary objective is to determine if the relationship between psychosocial stress and spontaneous preterm birth is altered based on obstetrical history (i.e. nulliparity, history of term birth or history of prior preterm birth). Our secondary objective is to determine if race alters the relationship between psychosocial stress, parity, and preterm birth.
Methods
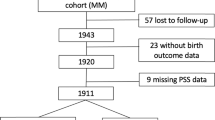
We performed a secondary analysis of data from the IRB-approved Healthy Pregnancy, Healthy Baby Study (HPHB), which was a prospective cohort study of ~ 1800 pregnant women enrolled from 2005 to 2010 in Durham, NC. The HPHB study was part of the US Environmental Protection Agency funded Southern Center on Environmentally-Driven Disparities in Birth Outcomes. Eligible participants were English-speaking adult women who lived in Durham County, had a singleton, non-anomalous fetus at 18–28 weeks gestation and received their care at the Duke Obstetrics Clinic or the Durham County Health Department Prenatal Care. Socio-demographic data, medical comorbidities and parity were obtained through enrollment interview and medical record review. Parity was categorized into three groups: primiparous (first pregnancy), multiparous with history of preterm birth (one or more prior pregnancies delivered before 37 weeks gestation) and multiparous with history of term birth (all prior pregnancies delivered at or beyond 37 weeks gestation).
Psychosocial stress was measured at a single time-point upon enrolment to the study using a battery of validated instruments each aimed to measure a different element of psychosocial health. The Perceived Stress Scale (PSS) is designed to measure the degree to which potentially stressful situations are perceived as unpredictable and/or stressful by an individual (Cohen and Williamson 1988).The Perceived Racism Scale (PRS) measures the respondents experience with racism during their current pregnancy and throughout their life (Dole et al. 2004). The Interpersonal Support Evaluation List (ISEL) is a list of 40 statements with Likert scale responses aimed at tangible support and self-esteem supports (Cohen et al. 1985). The John Henryism Active Coping Scale (JHAC) measures the degree to which respondents display a coping style common among African Americans that incorporates extreme goal-directed behaviors as a response to psychosocial and environmental stressors (James 1996). The Jerusalem and Schwarzer General Self-Efficacy Scale (SE score) is designed to measure perceived self-efficacy (i.e. belief in one’s ability to cope and adapt to stressors in daily activities and stressful events) (Jerusalem et al. 1992).
We limited our analysis to NHB and NHW women due to small numbers of women from other racial groups in the HPHB study. Baseline socio-demographic characteristics and medical comorbidities were compared by parity using Kruskal–Wallis test or ANOVA for continuous variables and Chi square or Fisher’s exact test for categorical variables. With a primary outcome of spontaneous preterm birth, logistic regression was used to model the effect of psychosocial stress on spontaneous preterm birth while controlling for parity, maternal age, race, chronic medical illness (chronic hypertension, pregestational diabetes), chronic psychiatric history (depression, anxiety), and tobacco use during pregnancy. To further understand the effect of psychosocial stress in women with different obstetrical histories, we performed stratified analyses using the same logistic regression described above within each parity subgroup (i.e. primiparous, history of preterm birth, and history of term birth). Finally, given the high rate of psychosocial stress and unique stressors within the NHB community, we also performed a stratified analysis of parity subgroups among NHB participants only. The proportions of missingness observed in psychosocial stress scales and spontaneous preterm birth ranged between 3 and 7%. Therefore, complete case analysis was carried out with the assumption that data were missing completely at random. p value was considered significant at α = 0.05. Analysis was performed in R (version 3.4.2).
Results
Among the entire HPHB cohort, 1606 subjects (1256 NHBs and 350 NHWs) had complete data available for analysis. Within this cohort, 426 women were primiparous, 268 had a history of preterm birth, and 912 had a history of term birth. Socio-demographic features varied across these three groups (Table 1). As expected, primiparous women were younger than multiparous women (i.e. those with a history of term or preterm birth). The median parity was higher in women with a history of preterm birth compared to women with a history of term birth. Body mass index was highest in women with a history of preterm birth and lowest in primiparous women. With respect to medical comorbidities, women with a history of preterm birth had higher rates of chronic hypertension, diabetes, depression, anxiety, tobacco use and illicit drug use. In all three subgroups, the majority of women had a high school diploma, were born in the USA or Canada, over 70% were not married and over 70% of the pregnancies in each group were unplanned. There was no difference in psychosocial stress across the three groups with the exception of ISEL, which was higher in primiparous women (Table 3).
Among the entire cohort, 237 (15.3%) of the pregnancies resulted in preterm birth, of which 125 (52.7%) were spontaneous. As expected, women with a history of preterm birth had the highest spontaneous preterm birth rate (Table 2). Specifically, 18.1% (48/265) of women with a history of preterm birth had spontaneous preterm birth in the index pregnancy, compared to 6.7% (27/403) of primiparous women and 5.7% (50/881) of women with a history of term birth. There was no difference in psychosocial stress across the three groups with the exception of ISEL, which was higher in primiparous women (Table 3). In an analysis including all participants irrespective of parity, there was no significant association between psychosocial stress measures and spontaneous preterm birth after controlling for confounders (Table 4). The findings were different when evaluating spontaneous preterm birth in the index pregnancy and psychosocial stress within parity subgroups, as described below.
In the sub-analysis by parity (Table 4), higher SE was associated with 52% lower odds of spontaneous preterm birth in the index pregnancy (aOR 0.48; 95% CI [0.24, 0.88], p = 0.02) and higher ISEL was associated with 4% lower odds of spontaneous preterm bith in the index pregnancy (aOR 0.96; 95% CI [0.92, 1.00], p = 0.03) among multiparous women with a history term birth. Higher JHAC was associated with a 6% lower odds of PTB in multiparous women with a history of preterm birth (aOR 0.94; 95% CI [0.90, 0.996], p = 0.04). There was no significant association between spontaneous preterm birth and any other stress measures in primiparous women.
Within the subset of NHB participants (Table 5), the association between spontaneous preterm birth in the index pregnancy, SE (aOR 0.41; 95% CI [0.21, 0.81], p = 0.01) and ISEL (aOR 0.96; 95% CI [0.92, 0.996], p = 0.03) was also observed in NHB women with a history of term birth. There were no other significant associations between preterm birth and any other stress measures examining the subset of primparous and multiparous NHB women with a history of term birth.
Discussion
The key finding in our study is that self-efficacy and interpersonal support are protective against spontaneous preterm birth in multiparous women with history of term birth while John Henryism Active Coping (JHAC) is protective against spontaneous preterm birth in multiparous women with history of preterm birth. We did not find an association between measures of psychosocial stress and preterm birth in primiparous women. This may be due to an overall low event rate and limited power. It is also plausible that preterm birth during first pregnancies are more likely to result from a discrete medical etiology, e.g. cervical insufficiency or a genetic predisposition. These conditions may dominate the causal pathway of preterm birth such that psychosocial stress is less impactful during a woman’s first pregnancy. Our data suggests that the ability to cope with and adapt to psychosocial stressors which is measured by self-efficacy, may influence preterm birth risk in multiparous women with a history of term birth, a group that would routinely be considered at low risk for preterm birth. This finding is consistent with the data linking psychosocial stress and elevations in cortisol releasing hormone (CRH), which leads to increases in prostaglandins and inflammatory cytokines. (Guendelman et al. 2008; Levine et al. 2016; Ruiz et al. 2016). In addition, the protective effect of self-efficacy, was even more significant among NHB multiparous women with a prior term birth, demonstrating the need for individualized patient-level strategies. The link between JHAC and preterm birth is logical given that JHAC is designed to measure, “prolonged, high-effort coping with difficult psychosocial environmental stressors(James 1994).” Although the psychosocial environmental stressors are typically associated with racism and poverty, one can image that facing a pregnancy after a prior preterm birth can cause extreme stress and highly motivated behavioral patterns to avoid a similar outcome.
We have identified measurable dimensions of psychosocial stress that are associated with preterm birth in women with a history of term birth, a group in whom preterm birth is often very challenging to predict. Additionally, we have identified JHAC as a potentially risk-reducing coping mechanism for recurrent preterm birth. Despite their potential impact, our findings must be viewed in the light of important limitations. First, the current study is a secondary analysis and is therefore limited to the data that was collected during the primary study. The psychosocial stress questionnaires were only administered at a single time-point during enrolment between 18 and 28 weeks therefore based on the current analysis it is unclear how changes in psychosocial stress before and during pregnancy alter outcomes. Additionally, given inclusion criteria of the primary study, the current analysis may exclude women with mid-trimester preterm birth. Preterm births were coded as spontaneous or medically indicated, however there is limited data beyond these crude classifications therefore our knowledge of the precise etiology of the preterm births is limited. Despite these limitations, our findings suggest measuring self-efficacy and interpersonal support during early pregnancy may identify women with a history of term birth who are at higher risk for a preterm birth in their current pregnancy. Although JHAC has been associated with some deleterious efforts in NHBs such as hypertension and peptic ulcer disease, elements of JHAC may be incorporated as part of a preterm birth prevention program.
Given the lack of effective population-level strategies to prevent preterm birth, it is imperative that we identify therapeutic targets and effective interventions across the population of pregnant women. Currently, the most effective preterm birth prevention strategies focus on multiparous women with a previous preterm birth due to the risk of recurrence and clear opportunity for identification and intervention. Yet such interventions are ineffective for nulliparous women and multiparous women with a history of term births. These groups include the majority of the pregnant population. Without strategies to target these groups, the rate of preterm birth will remain unacceptably high. Given the multifactorial etiology of preterm birth, it is likely that effective preventive strategies will vary by risk factor, such as psychosocial stress. Future studies to determine if self-efficacy and interpersonal support reliably identifies women with a history of term birth who are at increased risk for preterm birth are warranted. If current study’s findings are reproducible, further studies to determine factors that influence self-efficacy and interpersonal support as well as interventions to increase resiliency measures have the potential to reduce preterm birth in this population. Approaches to identify and improve upon social support and coping skills could lead to low intensity, safe strategies to reduce preterm birth and overall maternal psychosocial health.
References
Arbour, M. W., Corwin, E. J., Salsberry, P. J., & Atkins, M. (2012). Racial differences in the health of childbearing-aged women. MCN: The American Journal of Maternal/Child Nursing, 37(4), 262–268. https://doi.org/10.1097/NMC.0b013e31824b544e.
Borg, F., Gravino, G., Schembri-Wismayer, P., & Calleja-Agius, J. (2013). Prediction of preterm birth. Minerva Ginecologica, 65(3), 345–360.
Cohen, S., et al. (1985) Measuring the functional components of social support. In I. G. Sarason & B. R. Sarason (Eds.) Social support: Theory, research, and applications (pp. 73–94). Dordrecht: Martinus Nijhoff.
Cohen, S., & Williamson, G. (1988). Perceived stress in a probability sample of the United States. In S. Spacapan, S. Oskamp (Eds.) The social psychology of health. Newbury Park, CA: Sage.
Dekker, G. A., Lee, S. Y., North, R. A., McCowan, L. M., Simpson, N. A., & Roberts, C. T. (2012). Risk factors for preterm birth in an international prospective cohort of nulliparous women. PLoS ONE, 7(7), e39154. https://doi.org/10.1371/journal.pone.0039154.
Dole, N., Savitz, D. A., Siega-Riz, A. M., Hertz-Picciotto, I., McMahon, M. J., & Buekens, P. (2004). Psychosocial factors and preterm birth among African American and White women in central North Carolina. American Journal of Public Health, 94(8), 1358–1365.
Grobman, W. A., Parker, C., Wadhwa, P. D., Willinger, M., Simhan, H., & Silver, B., … Eunice Kennedy Shriver National Institute of Child Health Human Development nuMoM2b Network, B. M. D. (2016). Racial/ethnic disparities in measures of self-reported psychosocial states and traits during pregnancy. American Journal of Perinatology. https://doi.org/10.1055/s-0036-1586510.
Guendelman, S., Kosa, J. L., Pearl, M., Graham, S., & Kharrazi, M. (2008). Exploring the relationship of second-trimester corticotropin releasing hormone, chronic stress and preterm delivery. The Journal of Maternal-Fetal & Neonatal Medicine, 21(11), 788–795. https://doi.org/10.1080/14767050802379031.
James, S. (1996). The John Henryism Scale for active coping. In: R. Jones (Ed.) Handbook of tests and measurements for Black populations. Hampton, VA: Cobb & Henry Publishers
James, S. A. (1994). John Henryism and the health of African-Americans. Culture, Medicine and Psychiatry, 18(2), 163–182.
Jerusalem, M., Schwarzer, R. (1992). Self-efficacy as a resource factor in stress appraisal processes. In R. Schwarzer (Eds.) Self-efficacy: Thought control of action (pp. 195–213). Washington, DC: Hemisphere
Kazemier, B. M., Buijs, P. E., Mignini, L., Limpens, J., de Groot, C. J., Mol, B. W., & Ebm, C. (2014). Impact of obstetric history on the risk of spontaneous preterm birth in singleton and multiple pregnancies: A systematic review. BJOG, 121(10), 1197–1208. https://doi.org/10.1111/1471-0528.12896 (discussion 1209).
Khashan, A. S., McNamee, R., Abel, K. M., Mortensen, P. B., Kenny, L. C., Pedersen, M. G., … Baker, P. N. (2009). Rates of preterm birth following antenatal maternal exposure to severe life events: A population-based cohort study. Human Reproduction, 24(2), 429–437. https://doi.org/10.1093/humrep/den418.
Kramer, M. R., Hogue, C. J., Dunlop, A. L., & Menon, R. (2011). Preconceptional stress and racial disparities in preterm birth: An overview. Acta Obstetricia et Gynecologica Scandinavica, 90(12), 1307–1316. https://doi.org/10.1111/j.1600-0412.2011.01136.x.
Kramer, M. S., Lydon, J., Seguin, L., Goulet, L., Kahn, S. R., McNamara, H., … Platt, R. W. (2009). Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. American Journal of Epidemiology, 169(11), 1319–1326. https://doi.org/10.1093/aje/kwp061.
Laughon, S. K., Albert, P. S., Leishear, K., & Mendola, P. (2014). The NICHD Consecutive Pregnancies Study: Recurrent preterm delivery by subtype. American Journal of Obstetrics & Gynecology. https://doi.org/10.1016/j.ajog.2013.09.014.
Levine, T. A., Alderdice, F. A., Grunau, R. E., & McAuliffe, F. M. (2016). Prenatal stress and hemodynamics in pregnancy: A systematic review. Archives of Women’s Mental Health, 19(5), 721–739. https://doi.org/10.1007/s00737-016-0645-1.
Lu, M. C., & Chen, B. (2004). Racial and ethnic disparities in preterm birth: The role of stressful life events. American Journal of Obstetrics & Gynecology, 191(3), 691–699. https://doi.org/10.1016/j.ajog.2004.04.018.
March of Dimes 2017 Premature Birth Report Card. Retrieved from https://www.marchofdimes.org/mission/prematurity-reportcard.aspx.
Mathews, T. J., & MacDorman, M. F. (2013). Infant mortality statistics from the 2009 period linked birth/infant death data set. National Vital Statistics Reports, 61(8), 1–27.
Mercer, B. M., Goldenberg, R. L., Moawad, A. H., Meis, P. J., Iams, J. D., Das, A. F., … McNellis, D. (1999). The preterm prediction study: Effect of gestational age and cause of preterm birth on subsequent obstetric outcome. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. American Journal of Obstetrics & Gynecology, 181(5 Pt 1), 1216–1221.
Ruiz, R. J., Gennaro, S., O’Connor, C., Dwivedi, A., Gibeau, A., Keshinover, T., & Welsh, T. (2016). CRH as a predictor of preterm birth in minority women. Biological Research for Nursing, 18(3), 316–321. https://doi.org/10.1177/1099800415611248.
Acknowledgements
This research was supported by funding from the U.S. Environmental Protection Agency (RD-83329301-0).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wheeler, S., Maxson, P., Truong, T. et al. Psychosocial Stress and Preterm Birth: The Impact of Parity and Race. Matern Child Health J 22, 1430–1435 (2018). https://doi.org/10.1007/s10995-018-2523-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2523-0