Abstract
Objective We examined the association between parent and child fruit and vegetable (F&V) intake, physical activity (PA), and body mass index in an ethnic minority and low-income sample. Methods The study sample consisted of 86 children ages 5–7 years (80% Hispanic) and their parents. Three parent health variables (healthy weight, recommended F&V servings per day, and recommended weekly PA) were used to create a healthy role model index. Associations between the parent index and corresponding child health behaviors and weight were examined. Results Most parents (53.5%) were not healthy role models, 30.2% were limited healthy role models, 16.3% were good role models, and none were excellent role models; most parents and children did not meet guidelines for healthy weight, F&V intake, and PA. Parents who scored higher on the index were more likely to have children with higher levels of F&V. Furthermore, parents who had a healthy weight were 3.7 times more likely to have a child who had a healthy weight. Additionally, parents who were consuming the recommended servings of F&V per day were 10 times more likely to have children who were also consuming the recommended servings of F&V per day compared to parents who were not consuming the recommended servings of F&V per day. Conclusions for Practice These findings suggest the important role of parental modeling of healthy behaviors to their young children among minority/low-income families. Parents may serve as an important mechanism of change for children’s health status by increasing their own healthy lifestyle behaviors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Pediatric obesity is a significant public health concern. Parental obesity increases the risk of pediatric obesity into adulthood. What this study adds? Findings highlight the important role of parental modeling of healthy behaviors to their young children among minority/low income families. Parents can serve as an important mechanism of change on their children’s health by increasing their own healthy lifestyle behaviors.
Association of Parental Role Modeling with Child Weight and Health Behaviors
Public Health Concern of Pediatric Obesity
Pediatric obesity represents a significant public health concern, with epidemiological research indicating that 31.8% of children between the ages of 2 and 19 years are overweight or obese (Ogden et al. 2014). Rates of pediatric overweight and obesity are especially high among children from racial and ethnic minority backgrounds with recent estimates as high as 38.9% (Ogden et al. 2014). Demographic variables associated with racial and ethnic minority status, such as poverty level, access to fresh foods, and high saturation of fast-food restaurants in low socioeconomic (SES) communities, are also associated with increased rates of pediatric obesity (Morland et al. 2006; Powell et al. 2007). For example, children living in high poverty neighborhoods have a 50% higher chance of being overweight than those not living in poverty (Delva et al. 2006). Furthermore, parental obesity increases the risk of pediatric obesity into adulthood with overweight children who have an obese parent having twice the risk of becoming an obese adult (Whitaker et al. 1997). However, few studies have examined the influence of parents on obesity and related health behaviors among young children from ethnic minority and low-income backgrounds (Kumanyika and Grier 2006).
Recommended Healthy Practices
To help reduce rates of obesity, the U.S. Department of Health and Human Services (USDHHS 2008) and the Department of Agriculture (USDA; McGuire 2011) developed research-based guidelines for healthy weight, nutrition, and physical activity, as indicated below:
Weight
Children with a body mass index (BMI) between the 85th and 95th percentile are considered overweight, and ≥ the 95th percentile are considered obese (Barlow and Dietz 1998). For adults, a BMI score between 25 and 29.9 kg/m2 is considered overweight, and ≥ 30 kg/m2 is considered obese (NHLBI 1998).
Nutrition
The USDHHS and USDA recommended that children and adults eat five or more servings of fruits and/or vegetables (F&V) per day (McGuire 2011). The U.S. national average for consuming the recommended F&V is 1% for adults and 2% for children (USDHHS 2010) indicating that the vast majority of children and adults do not meet the recommended amounts of F&V.
Physical Activity (PA)
The U.S. Department of Health and Human Services (2008) states that children and adolescents should engage in at least 60 min of daily PA. Furthermore, the 60 min of PA should be either moderate (e.g., brisk walking, bicycling at less than 10 miles per hour) or vigorous (e.g., running, swimming laps) in intensity and should include vigorous PA at least 3 days per week (USDHHS 2008). For adults, recommendations are for at least 150 min of moderate or vigorous PA per week (USDHHS 2008). In the United States, < 20% of adults meet the recommended PA guidelines, and < 20% of adolescents meet the youth guidelines (State of the Plate 2010). Additionally, only 42% of children ages 6–11 years have at least 1 h per day of moderate to PA (Troiano et al. 2008).
Parents as Role Models
Previous research has shown an association between parental modeling of F&V intake and their child’s F&V intake. For example, research has demonstrated in a sample of middle-class non-Hispanic white 5-year-old females that higher levels of reported F&V intake in their mothers was associated with higher levels of girls’ F&V intake (Fisher et al. 2002). Vereecken et al. (2010) focused on non-Hispanic white families and found a positive association between children and parents F&V intake; however, weight was not examined.
Similar to the effect of parent modeling of F&V intake, parent modeling of PA (i.e., engaging in more PA) has been shown to be positively associated with children’s PA levels. For example, in a sample of middle-class non-Hispanic white 4–7-year-old children, those with physically active mothers were two times as likely to be active compared to children of inactive mothers (Moore et al. 1991). Furthermore, research has demonstrated that middle-class 5-year-old non-Hispanic white girls living with parents who reported low PA levels and high-caloric dietary intake had significantly higher BMI and skinfold thickness than girls living with parents with high PA levels and lower-caloric dietary intake (Davison and Birch 2002).
A few studies have shown Hispanic youth engage in less PA overall, are sedentary when their parents are sedentary, and receive less parental support to be active (Ruiz et al. 2011; Hoefer et al. 2001). Despite the documented relation between parent and child PA, relatively few studies have included children and families from low-income, ethnic minority backgrounds, and none examined the combination of parental BMI, PA, and F&V intake as a single index of healthy role model status.
Purpose of Study
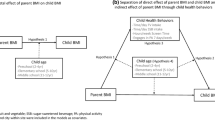
Given the association between healthy lifestyle habits (i.e., healthy eating and PA) and lifelong wellbeing (Matheson et al. 2012), the purpose of this study was to address significant gaps in the pediatric obesity literature by examining the relationship between child and parent BMI, F&V consumption, and PA levels in a sample of families primarily from minority and low-income backgrounds. We hypothesized that the majority of children and their parents would not meet recommended guidelines. We also predicted that parents who were “healthy role models” would be more likely to have children who ate more F&V, had greater levels of PA, and had lower BMI z-scores compared to parents who were less healthy role models.
Methods
Procedures
Participants were recruited from two elementary schools as part of a larger school-based intervention study to prevent obesity in which students at one school received an active intervention. The current study combines baseline data from all participants at both schools. Following institutional review board approval, letters introducing the study were distributed to all parents of children in Kindergarten and 1st grade classrooms (N = approximately 600). Forms indicating that parents were interested in the study were returned by 234 parents. A research associate then contacted interested families to schedule a study visit. One parent and one child from each family were consented during the study visit (N = 86). The schools were located in predominately low-income (56% on free/reduced lunch) neighborhoods in a southeastern metropolitan city. A majority (98%) of parents identified themselves and their child as being from an ethnic minority background (see Table 1).
The study sample (N = 86) was representative of the community and school population in terms of income and ethnic minority background. Since this was a pilot study and feasibility study, our aim was not to recruit a very large sample of children at the two schools.
Measures
Child and Parent Anthropometrics
Parent and child height and weight were measured by calibrated stadiometer (Seca 214; Seca North America East, Hanover, MD) and portable digital scale (Tanita Model BC551; Tanita Corp of America, Arlington Heights, IL) in triplicate by trained research staff and then used the mean height and weight to calcualte BMI (weight in kg/height in meters squared) for both parents and children; child BMI scores were transformed into z-scores based on national norms (Kuczmarski 2000).
Child and Parent Dietary Intake
Assessment of parent and child dietary intake was obtained by a 24-h dietary recall which has been shown to be a valid measure of dietary intake (Block 1982; Johnson et al. 1996). Research associates trained by a nutritionist administered two 24-h dietary recalls to the parent and child, respectively. Parents were asked to recall and describe foods and drinks consumed at each meal during the previous day including portion sizes. Pictures of portion sizes were provided to aid in estimation. Children also completed 24-h dietary intake recalls for intake over the previous day with the help of their parent who confirmed accuracy of their child’s report or provided information about the child’s intake if the child could not recall (Block 1982). In the case that the child’s report was discrepant with the parent’s report, the parent’s report was used. Consistent with previous research (Mink et al. 2010), a research associate entered the collected meal information for the 24-h period into Nutritionist Pro-V (Axxya Systems 2006), a nutrition analysis software. Child and parent F&V intake (servings per day) was used as a key measure of dietary behavior given the USDHHS and USDA daily serving recommendations (McGuire 2011) at the time this data was collected.
Child and Parent PA
Child PA was assessed via accelerometetry. Each child wore a uniaxial accelerometer (Lifecorder, Suzuken Co. Ltd, Japan) on their waist belt for 7 days. Participants were instructed to wear the accelerometer device from the time of awakening until just before bedtime, and to remove the device while bathing or swimming. The device provided activity data in 4 s epochs over 2-min periods as levels of intensity. Intensity levels range from zero to nine with zero being no activity. The intensity of a 2-min period is measured as the most frequent intensity recorded during the 30 four-second epochs in that 2 min. Accelerometry data was analyzed to exclude non-active/sleep time and mild levels of exertion, thereby including only moderate to vigorous PA. To increase the validity of PA data, it is recommended that days with maximum hours of wear time be included (Migueles et al. 2017). Non-wear/sleep time is defined as 40 consecutive minutes of zero activity recording. Donaldson et al. (2016) showed that 4 valid days of measurement are comparable to 1 week. Therefore, the 4 best days (i.e., days with the most data recorded) of the 7 days worn were used in the analyses.
Parent PA levels were assessed via the modifiable activity questionnaire, which assesses previous 12-month PA during leisure and work and has been shown to be reliable and valid (Kriska et al. 1990; Pereira et al. 1997). Participants were asked to provide information on the number of months, times per week, and duration in a day that they participated in a list of common activities and any other activities that may not have been listed. Total time participating in the activity and time spent participating in moderate to vigorous PA was calculated.
Data Analysis Plan
All analyses were conducted using SPSS 22. Descriptive analyses were conducted for child zBMI, parent BMI, child and parent F&V intake (servings per day), child daily minutes of moderate to vigorous PA, and parent weekly minutes of moderate to vigorous PA. A healthy parental role model index score was calculated by the sum of the three dichotomous (0 = No, 1 = Yes) health status indicators: (1) healthy BMI; (2) recommended servings of F&V per day; and (3) recommended minutes of moderate to vigorous PA. Parents were classified as “unhealthy” role models (score of 0), “limited healthy” role models (score of 1), “good healthy” role models (score of 2), or “excellent healthy” role models (score of 3). Regression analyses between the parental role model index and child zBMI scores, F&V intake, and PA, respectively, were examined. Odds ratios examined the relationships between each health status indicator for both parent and child.
Results
Preliminary Analyses
Nine families had missing data on at least one variable. According to Little’s MCAR test, data were missing completely at random (χ2 = 31.75, p > .05). Outlier analyses were conducted and no outliers were found. No significant associations between outcome variables and demographic variables were found and therefore no covariates were included in the analyses.
Parental Role Modeling and Child Health Outcomes
A majority of parents (54%) were classified as unhealthy role models and did not meet the recommendations for BMI, F&V or PA; 30% of parents were classified as limited healthy role models; 16% of parents were classified as good healthy role models; and none of the parents in the sample were classified as excellent healthy role models (see Table 2).
Descriptives for individual parent and child health status indicators are included in Table 2. Most parents and children did not meet the guidelines for healthy weight (87% and 43%, respectively), F&V consumption (89% and 91%, respectively), or PA (68% and 83%, respectively). A significant association was found between the healthy parent role model index score and child-reported F&V intake, F(1,77) = 4.96, p = .029, indicating that parents who were healthier role models had children with higher F&V intake. No associations were found between the healthy parent role model index score and child zBMI F(1,84) = .16, p = .69, or child PA F(1,70) = .05, p = .82, respectively (see Table 3).
Several significant associations were found between individual parent health status indicators (i.e., healthy weight, meets recommended F&V and PA guidelines) and corresponding child health status indicators (see Table 4).
Parents who were a healthy weight were 3.7 times more likely to have a child who had a healthy weight compared to parents who did not have a healthy weight. Similarly, parents who were consuming the recommended servings of F&V per day were 10 times more likely to have children who were also consuming the recommended servings of F&V per day compared to parents who were not consuming the recommended servings of F&V per day. However, no significant association between parents and children meeting the recommended amount of PA per day were found.
Discussion
We found most of the parents and nearly half of the children were in the overweight or obese ranges. These high rates illustrate the need for obesity interventions among young, ethnic minority children and their families. Consistent with prior work in Caucasian samples, we also found that most parents and children did not meet the F&V and PA recommendations (Kim et al. 2014; Troiano et al. 2008; USDHHS 2010; State of the Plate 2010). Our findings replicate and extend such findings by including a young mostly Hispanic sample. Additionally, we found that child weight was not related to meeting F&V and PA recommendations. Given the documented relationship between meeting recommended guidelines and health problems (Huang et al. 2011; Janssen and Leblanc 2010), it is important to find ways to improve adherence to F&V and PA recommendations in America’s largest growing minority sample.
Parents considered healthy role models were more likely to have a child with higher F&V intake. These results are consistent with previous research on the relation between parental and child consumption of F&V in primarily white, non-Hispanic populations (Fisher et al. 2002; Wardle et al. 2005). Moreover, parents who met the criteria for positive health status indicators (i.e., healthy weight and meeting daily F&V recommendations) were more likely to have children who also had these respective positive health status indicators. Thus, the combination of healthy role modeling behaviors is associated with child healthy habits (i.e., increased child F&V consumption) but also parents who meet criteria for individual recommendations impact their child’s healthy habits in that domain. It could be the case that children who have a healthy weight are meeting the recommendations for F&V consumption and PA. However, no significant association was found between BMI and F&V consumption, and PA, respectively, in this sample. This highlights an important association between childhood obesity and parental role modeling and is a potential target for intervention. Given the low rates of adherence to recommendations in this sample, these findings suggest that targeting parents of young children to improve their own dietary intake and PA may be a useful strategy to help improve their children’s health behaviors and BMI.
The parent healthy role model index was not significantly related to child zBMI or PA. Given the young age of the children in the current sample, parents’ unhealthy behaviors may not yet be reflected in their child’s weight or amount of PA. However, the parent healthy role model index was associated with child F&V intake, which has been found to be related to child weight (Epstein et al. 2001). A longitudinal study to assess the impact of parental healthy role modeling in early childhood on later child health factors would help explore this possible relation further.
Results have important clinical implications, such as promoting increases in parent F&V consumption and PA in interventions as a means of increasing F&V intake in children to reduce the risk of child obesity. Other research also suggests parents serve as role models and reinforce healthy eating and PA in their children (Epstein et al. 2001; Foster et al. 2005; Wyse et al. 2011; Bere et al. 2005). Interventions that aim to improve child health outcomes via parental factors have been shown to be effective but have not focused solely on parent F&V intake or parent PA (Wyse et al. 2011; Bere et al. 2005). A telephone intervention used by Wyse et al. (2011) focused on parental modeling, but parent F&V consumption was not measured. Findings from Wrotniak et al. (2004) showed that parents who lost weight had children who did better in family-based behavioral weight control programs for overweight children than parents who did not lose weight. Therefore, future research should examine in the context of a randomized controlled trial the extent to which increases in parental F&V consumption and PA results in positive child health outcomes.
Furthermore, current obesity interventions focus on many different components (e.g., limiting fats, reducing calories, increasing PA, and limiting sedentary activity) for both parents and children that may require drastic changes to daily lifestyle. Previous research has found that when treatments are simplified, adherence is improved (Haynes et al. 2002). Having too many goals to work on at once for both parents and children and goals that require drastic changes may be overwhelming and difficult for families to achieve (Foster et al. 2005). Given the relation between parent healthy behaviors and child F&V consumption, an intervention for parents of young children that solely focuses on increasing parent F&V consumption and PA may be more feasible for families and cost efficient.
Study Strengths and Limitations
Strengths of the study include the focus on young ethnic minority children, the examination of parental and child BMI and health behaviors, the use of validated self-report procedures for assessment of dietary intake and PA, and the use of accelerometry for objective assessment of PA in the children. However, several limitations should be considered when interpreting the findings. First, this study used a cross-sectional design and therefore causal inferences cannot be made. Second, the parental dietary and PA data were self-report measures and are subject to rater bias. While these methods have been previously validated, inclusion of more objective measures (e.g., accelerometery) would help corroborate self-report data. Third, although the healthy parental role model index used in the analysis has clear face validity, more data is needed to confirm the criterion-related validity of the index. Additionally, future research that aims to focus on nutrition in particular, would benefit from including a more thorough indicator of nutrition, such as the Healthy Eating Index (Guenther et al. 2014). Fourth, the sample was 90% Hispanic and therefore the findings may only generalize to this subgroup of minorities. However, Hispanics are America’s largest growing minority sample. Lastly, although interest forms were sent home to 600 families, and 234 of these families expressed interest, only 86 families were consented and participated in the study. Although, these 86 families were representative of the school and community demographics. Additionally, given that this was part of a pilot study, the sample size was relatively small, and some findings may not have been significant due to limited power. Furthermore, this small sample size may have led to overestimated OR’s. The literature would benefit from additional studies with a larger sample of similarly high-risk families.
Conclusions
Despite these limitations, this study illustrates the association of parent and child BMI and F&V intake, indicating the potential effect of parental modeling on their young children’s weight and F&V intake. Studies of family behavioral lifestyle interventions for child obesity focus on measuring children’s weight outcomes and places less emphasis on parental health and lifestyle behaviors. Thus, interventions for pediatric obesity may benefit by targeting parental weight, diet, and PA in future randomized controlled trials.
Implications for Research and Practice
Future research should examine in the context of a randomized controlled trial the extent to which increases in parental F&V consumption and improved BMI results in positive child health outcomes. Clinically, interventions should focus on promoting increases in parent F&V consumption and PA as a means of increasing F&V intake in children to reduce the risk of child obesity. Focusing on parents may be more practical for families to implement and cost efficient.
References
Barlow, S. E., & Dietz, W. H. (1998). Obesity evaluation and treatment: Expert committee recommendations. Pediatrics, 102(3), e29–e29.
Bere, E., Veierød, M. B., & Klepp, K. I. (2005). The Norwegian school fruit programme: Evaluating paid vs. no-cost subscriptions. Preventive Medicine, 41(2), 463–470.
Block, G. (1982). A review of validations of dietary assessment methods. American Journal of Epidemiology, 115(4), 492–505.
Davison, K. K., & Birch, L. L. (2002). Obesigenic families: Parents’ physical activity and dietary intake patterns predict girls’ risk of overweight. International Journal of Obesity, 26(9), 1186.
Delva, J., O’Malley, P. M., & Johnston, L. D. (2006). Racial/ethnic and socioeconomic status differences in overweight and health-related behaviors among American students: National trends 1986–2003. Journal of Adolescent Health, 39(4), 536–545.
Donaldson, S. C., Montoye, A., Tuttle, M. S., & Kaminsky, L. A. (2016). Variability of objectively measured sedentary behavior. Medicine and Science in Sports and Exercise, 48(4), 755–761.
Epstein, L. H., Gordy, C. C., Raynor, H. A., Beddome, M., Kilanowski, C. K., & Paluch, R. (2001). Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obesity, 9(3), 171–178.
Fisher, J. O., Mitchell, D. C., Smiciklas-Wright, H., & Birch, L. L. (2002). Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. Journal of the Academy of Nutrition and Dietetics, 102(1), 58–64.
Foster, G. D., Makris, A. P., & Bailer, B. A. (2005). Behavioral treatment of obesity–. The American Journal of Clinical Nutrition, 82(1), 230S–235S.
Guenther, P. M., Kirkpatrick, S. I., Reedy, J., Krebs-Smith, S. M., Buckman, D. W., Dodd, K. W., Casavale, K. O., & Carroll, R. J. (2014). The healthy eating index-2010 is a valid and reliable measure of diet quality according to the 2010 dietary guidelines for Americans. The Journal of Nutrition, 144(3), 399–407.
Haynes, R. B., McDonald, H. P., & Garg, A. X. (2002). Helping patients follow prescribed treatment: Clinical applications. Journal of the American Medical Association, 288(22), 2880–2883.
Hoefer, W. R., McKenzie, T. L., Sallis, J. F., Marshall, S. J., & Conway, T. L. (2001). Parental provision of transportation for adolescent physical activity. American Journal of Preventive Medicine, 21(1), 48–51.
Huang, J. S., Gottschalk, M., Norman, G. J., Calfas, K. J., Sallis, J. F., & Patrick, K. (2011). Compliance with behavioral guidelines for diet, physical activity and sedentary behaviors is related to insulin resistance among overweight and obese youth. BMC Research Notes, 4(1), 29.
Janssen, I., & LeBlanc, A. G. (2010). Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. International Journal of Behavioral Nutrition and Physical Activity, 7(1), 40.
Johnson, R. K., Driscoll, P., & Goran, M. I. (1996). Comparison of multiple-pass 24-hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in young children. Journal of the American Dietetic Association, 96, 1140–1144.
Kim, S. A., Moore, L. V., Galuska, D., Wright, A. P., Harris, D., Grummer-Strawn, L. M., et al. (2014). Vital signs: Fruit and vegetable intake among children-United States, 2003–2010. MMWR. Morbidity and Mortality Weekly Report, 63(31), 671–676.
Kriska, A. M., Knowler, W. C., LaPorte, R. E., Drash, A. L., Wing, R. R., Blair, S. N., et al. (1990). Development of questionnaire to examine relationship of physical activity and diabetes in pima Indians. Diabetes Care, 13(4), 401–411.
Kuczmarski, R. J. (2000). CDC growth charts. Hyattsville: National Center for Health Statistics
Kumanyika, S., & Grier, S. (2006). Targeting interventions for ethnic minority and low-income populations. The Future of Children, 16, 187–207.
Matheson, E. M., King, D. E., & Everett, C. J. (2012). Healthy lifestyle habits and mortality in overweight and obese individuals. The Journal of the American Board of Family Medicine, 25(1), 9–15.
McGuire, S. (2011). US department of agriculture and US department of health and human services, dietary guidelines for americans, 2010. Washington, DC: US government printing office
Migueles, J. H., Cadenas-Sanchez, C., Ekelund, U., Nyström, C. D., Mora-Gonzalez, J., Löf, M., et al. (2017). Accelerometer data collection and processing criteria to assess physical activity and other outcomes: A systematic review and practical considerations. Sports Medicine, 47(9), 1821–1845.
Mink, M., Evans, A., Moore, C. G., Calderon, K. S., & Deger, S. (2010). Nutritional imbalance endorsed by televised food advertisements. Journal of the American Dietetic Association, 110(6), 904–910.
Moore, L. L., Lombardi, D. A., White, M. J., Campbell, J. L., Oliveria, S. A., & Ellison, R. C. (1991). Influence of parents’ physical activity levels on activity levels of young children. The Journal of Pediatrics, 118(2), 215–219.
Morland, K., Roux, A. V. D., & Wing, S. (2006). Supermarkets, other food stores, and obesity: The atherosclerosis risk in communities study. American Journal of Preventive Medicine, 30(4), 333–339.
National Heart, Lung, Blood Institute, National Institute of Diabetes, Digestive, & Kidney Diseases (US). (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report (No. 98). National Heart, Lung, and Blood Institute.
Ogden, C. L., Carroll, M. D., Kit, B. K., & Flegal, K. M. (2014). Prevalence of childhood and adult obesity in the United States, 2011–2012. The Journal of the American Medical Assoication, 311(8), 806–814.
Pereira, M. A., FitzerGerald, S. J., Gregg, E. W., Joswiak, M. L., Ryan, W. J., Suminski, R. R., et al. (1997). A collection of physical activity questionnaires for health-related research. Medicine and Science in Sports and Exercise, 29(6 Suppl), S1–205.
Powell, L. M., Auld, M. C., Chaloupka, F. J., O’Malley, P. M., & Johnston, L. D. (2007). Associations between access to food stores and adolescent body mass index. American Journal of Preventive Medicine, 33(4), S301–S307.
Ruiz, R., Gesell, S. B., Buchowski, M. S., Lambert, W., & Barkin, S. L. (2011). The relationship between Hispanic parents and their preschool-aged children’s physical activity. Pediatrics, 127(5), 888–895.
State of the Plate: 2010 Study on America’s Consumption of Fruits and Vegetables, 2010. Produce for Better Health Foundation. Web. http://www.pbhfoundation.org.
Troiano, R. P., Berrigan, D., Dodd, K. W., Masse, L. C., Tilert, T., & McDowell, M. (2008). Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise, 40(1), 181.
US Department of Health and Human Services. (2008). 2008 physical activity guidelines for Americans: Be active, healthy, and happy!. Washington, DC: US Department of Health and Human Services. http://www.health.gov/paguidelines.
US Department of Health and Human Services. (2010). Healthy people 2020. Washington, DC: US Department of Health and Human Services. http://www.cdc.gov/nchs/healthy_people.
Vereecken, C., Rovner, A., & Maes, L. (2010). Associations of parenting styles, parental feeding practices and child characteristics with young children’s fruit and vegetable consumption. Appetite, 55(3), 589–596.
Wardle, J., Carnell, S., & Cooke, L. (2005). Parental control over feeding and children’s fruit and vegetable intake: How are they related? Journal of the Academy of Nutrition and Dietetics, 105(2), 227–232.
Whitaker, R., Wright, J., Pepe, M., Seidel, K., & Dietz, W. (1997). Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine, 337, 869–873. https://doi.org/10.1056/NEJM199709253371301.
Wrotniak, B. H., Epstein, L. H., Paluch, R. A., & Roemmich, J. N. (2004). Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Archives of Pediatrics & Adolescent Medicine, 158(4), 342–347.
Wyse, R., Wolfenden, L., Campbell, E., Campbell, K., Brennan, L., Fletcher, A., et al. (2011). A pilot study of a telephone-based parental intervention to increase fruit and vegetable consumption in 3–5-year-old children. Public Health Nutrition, 14(12), 2245–2253.
Acknowledgements
This research was supported by grants from the National Institutes of Health (Grant Nos. 1R34 DK074552 and T32 HD07510). Contribution of JM in the preparation of this manuscript was supported by a grant (no. 21-6/HEC/R&D/PPCR/2017) from the Higher Education Commission of Pakistan.
Author information
Authors and Affiliations
Contributions
AD, JC, & EP, conceived and carried out the study and analyzed data. MV assisted with study procedures. JM, PG, & DB analyzed data. All authors were involved in writing the paper and had final approval of the submitted and published versions.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Coto, J., Pulgaron, E.R., Graziano, P.A. et al. Parents as Role Models: Associations Between Parent and Young Children’s Weight, Dietary Intake, and Physical Activity in a Minority Sample. Matern Child Health J 23, 943–950 (2019). https://doi.org/10.1007/s10995-018-02722-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-02722-z