Abstract
Introduction The importance of patient satisfaction in US healthcare is increasing, in tandem with the advent of new patient care modalities, including virtual care. The purpose of this study was to compare the satisfaction of obstetric patients who received one-third of their antenatal visits in videoconference (“Virtual-care”) compared to those who received 12–14 face-to-face visits in-clinic with their physician/midwife (“Traditional-care”). Methods We developed a four-domain satisfaction questionnaire; Virtual-care patients were asked additional questions about technology. Using a modified Dillman method, satisfaction surveys were sent to Virtual-care (N = 378) and Traditional-care (N = 795) patients who received obstetric services at our institution between January 2013 and June 2015. Chi-squared tests of association, t-tests, logistic regression, and ANOVA models were used to evaluate differences in satisfaction and self-reported demographics between respondents. Results Overall satisfaction was significantly higher in the Virtual-care cohort (4.76 ± 0.44 vs. 4.47 ± 0.59; p < .001). Parity ≥ 1 was the sole significant demographic variable impacting Virtual-care selection (OR = 2.4, 95% CI: 1.5–3.8; p < .001). Satisfaction of Virtual-care respondents was not significantly impacted by the incorporation of videoconferencing, Doppler, and blood pressure monitoring technology into their care. The questionnaire demonstrated high internal consistency as measured by domain-based correlations and Cronbach’s alpha. Discussion Respondents from both models were highly satisfied with care, but those who had selected the Virtual-care model reported significantly higher mean satisfaction scores. The Virtual-care model was selected by significantly more women who already have children than those experiencing pregnancy for the first time. This model of care may be a reasonable alternative to traditional care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Little is known about patient satisfaction with virtual provision of routine prenatal care for low-risk patients; to date, in the United States, only two such programs have been discussed in the literature. Patient satisfaction is becoming influential in health care, and low-risk pregnant patients represent a large subpopulation of basically healthy patients who can be successfully monitored with a mix of in-person and virtual encounters. This study demonstrates high levels of satisfaction for Virtual-care and Traditional-care patients, with significantly higher overall and domain (scheduling, provider, personal, care assessment) scores for patients monitored with a mix of videoconference and in-clinic visits.
Introduction
In the United States, low-risk obstetric patients typically follow a care schedule recommended by the American College of Obstetricians and Gynecologists (ACOG). Consisting of 12–14 visits, patients are seen monthly from weeks 8–28, every 2 weeks from weeks 28–36, and weekly from week 36 until delivery (American Academy of Pediatrics and American College of Obstetricians and Gynecologists 2012). We will refer to this ACOG endorsed paradigm as Traditional-care. Although the specific benefits of Traditional-care have not been demonstrated through randomized clinical trials, and despite a lack of clarity surrounding evidence of its effectiveness (Alexander and Kotelchuck 2001), it is widely adhered to (Baldwin et al. 1994), making it the standard-of-care for obstetric patients in the United States. Studies have demonstrated that reduced visit schedules do not result in adverse medical outcomes (McDuffie et al. 1996; Villar et al. 2001; Walker et al. 2001) or increased use of medical services during pregnancy (McDuffie et al. 1997). Notably, despite acceptable pregnancy outcomes with fewer visits, patients have reported lower satisfaction with care delivery methods that reduce interaction with providers (Carroli et al. 2001; Dowswell et al. 2010; Jewell et al. 2000; Sikorski et al. 1996).
Although telemedicine has been used in the delivery of obstetric care for many years, its use has focused largely on providing specialty care to rural patients whose access to specialists is inadequate (Lowery et al. 2007; Odibo et al. 2013; Wood 2011), management of gestational diabetes (Nudell et al. 2011), and targeted enhancement of care for high-risk pregnancies (Long et al. 2014). A review of 60 articles (Magann et al. 2011) describes the use of telemedicine in obstetrics for patient counseling, specialist interpretation of ultrasounds and non-stress tests, and management of diabetes and postpartum depression. In this growing and important body of literature, however, there is a dearth of reporting on the use of telemedicine for routine prenatal care delivery in low-risk patients.
We reported favorable outcomes for patients engaging in the OBCareConnect™ (OBCC) Virtual Visit program at our institution (Pflugeisen et al. 2016). In this model, which we will refer to as Virtual-care, routine prenatal care is provided to low-risk patients with a mix of five visits conducted in teleconference with an obstetric Advanced Registered Nurse Practitioner (ARNP) and 7–9 face-to-face physician/midwife visits [for further details of the program and its implementation, please see (Pflugeisen et al. 2016)]. Ridgeway et al. (Ridgeway et al. 2015) describe the OB Nest program at Mayo Clinic Rochester in which low-risk obstetric patients have eight physician/midwife face-to-face encounters and six telephone/online nurse visits during their pregnancy. Marko et al. (Marko et al. 2016) report results of a study that randomized 100 low-risk prenatal patients to traditional or mixed in-clinic/virtual care. To our knowledge, no other such programs or studies have been reported in the literature. OBCC and OB Nest uphold the high-level of patient-provider interaction outlined by the ACOG-endorsed traditional care model, but reduce the number of in-clinic, physician/midwife encounters. OB Nest patients reported improved satisfaction with this model of care compared to patients served per ACOG guidelines (Butler Tobah et al. 2016). In this paper we describe patient satisfaction of OBCareConnect™ patients who elected the Virtual Visit track during their pregnancy compared to that reported by women who received traditional prenatal care.
Methods
Virtual-care patients were identified using modifier codes in the electronic medical record (EMR) indicating enrollment in the Virtual Visit program; all Virtual-care patients were assessed and stratified as low-risk by their physician at the time of enrollment. All Virtual-care patients who completed at least one Virtual Visit between March 2013 and January 2016 were invited to participate in the study. A comparison group comprised of patients who enrolled in the Traditional-care program during the same time frame. Electronic records of the potential Traditional-care patients were scanned for encounters that included any “supervision of high-risk pregnancy” diagnosis to rule out patients with a known high-risk pregnancy at the time of enrollment. This resulted in removal of twelve patients from the eligible pool of Traditional-care patients. Pooled pair-matching based on enrollment year was used to create a 2:1 matched sample of Traditional-care patients. In our program, both the women themselves and the physicians have the option to terminate Virtual-care enrollment based on preference and/or pregnancy progression. As such, sample selection was made on intent-to-treat with regard to track enrollment; women who changed tracks or moved care delivery location during the course of their pregnancy were invited to participate according to initial track enrollment.
Surveys were designed for the two care pathways with minimal discrepancies between them. Both surveys were comprised of two sections: a set of Likert scale (Very Poor, Poor, Fair, Good, Very Good) questions regarding the prenatal care experience followed by a set of multiple choice background questions related to demographics and pregnancy. The Traditional-care survey had 17 Likert question compared to 21 on the Virtual-care survey, which included a four-question section on technology that was not applicable to the Traditional-care patients. Sixteen of the Likert scale questions were identical between surveys. The Virtual-care patients were asked about explanations related to using the Doppler and blood pressure cuff, while the Traditional-care patients were asked about explanations related to procedures occurring during their visits. Virtual-care patients were also asked about ease of accessing the Virtual-care provider. See Table 1 for the full set of questions. On the surveys, “prenatal visits” was used interchangeably with “Virtual visits” and “prenatal care provider” was used interchangeably with “Virtual Visit provider.” The Likert questions were divided into domains, including: Scheduling (S), Technology (T), Provider (MD), Personal (P), and General (G); from these, an overall satisfaction score (O) was generated, both including and excluding the technology domain.
The multiple choice demographic questions included: as age, distance from OB clinic, household income, marital status, prior pregnancy loss, employment status, and parity at the time of pregnancy as well as ethnicity. In addition, Traditional-care patients were asked why they chose not to participate in the Virtual Visit program; Virtual-care patients were asked where they completed their Virtual visits and the number of visit completed. The study protocol and instruments were reviewed and approved by the MultiCare Institutional Review Board (MHS IRB Protocol 15.25).
A modified Dillman Method (Dillman 1978) was used to contact patients. Surveys, accompanied by a brief cover letter that explained the purpose of the study and voluntary participation, were mailed to all patients in both cohorts in March, 2016. Exactly 1 week later a thank-you/reminder postcard was mailed to all patients in both cohorts. Four weeks after the initial mailing duplicate surveys were mailed to known non-respondents. To protect patient privacy, the surveys were deidentified, but included an option for the patient provide to her name to avoid receiving a second survey at 4 weeks. Mailings that were returned with a forwarding address were updated and re-mailed to the patient at the forwarding address. Mailings that were returned with no forwarding address were documented as undeliverable and the final denominators for each cohort were recalculated to account for these undeliverable surveys. Completed surveys were received between March and August 2016.
All data were recorded in an Excel database by the Principal Investigator of the study [BMP] and Likert Scale questions were converted to numerical values (1 = Very Poor to 5 = Very Good). Using this integer scaling, we generated domain scores and an overall score for each respondent’s survey. Descriptive statistics were generated for each question, domain, and for overall survey scores. Chi-squared tests of association were used to understand the relationship between care pathway enrollment and categorical background variables. ANOVA models were used to compare both domain and overall satisfaction scores between the two groups; when examining overall satisfaction, we both included and excluded questions from the technology domain, as indicated. Correlations were used to confirm the construct validity and internal consistency of the instruments and to gain insight into priorities of the two groups. Stepwise logistic regression using the Akaike Information Criterion for covariate selection was used to identify variables significantly associated with selection of Virtual-care and the relationship between background and overall satisfaction. All data transformations and analyses were conducted in the R statistical computing environment (R Core Team (2013)) and significance was assessed at the 0.05 level.
Results
Mailing, Response and Demographics
In early March, 2016, patient satisfaction surveys were mailed to 430 Virtual-care and 860 Traditional-care patients. These patients were 69% Caucasian and 32% had subsidized insurance. Surveys were determined to be undeliverable to 7.6% Traditional-care (N = 65) and 12.1% Virtual-care (N = 52) patients; denominators were adjusted on the assumption that a total of 378 Virtual-care and 795 Traditional-care patients received the survey. A total of 96 (12.1%) Traditional-care and 75 (19.8%) Virtual-care patients responded, yielding a significantly higher response rate among Virtual-care patients (estimated difference = 7.7%; 95% CI 3.2, 12.4%; p < .001). Virtual-care and Traditional-care respondent backgrounds were comparable, including employment status during pregnancy (p = .09), partner status during pregnancy (p = .16), self-reported Caucasian race (p = .57), home < 5 miles from prenatal care provider’s office (p = .68), household income > 100k, and prior pregnancy loss (p = .80; Table 2). Average age at the time of pregnancy was 31 years for both groups (p = .72). The sole background characteristic that differed significantly between the two groups was parity: 44.8% of the Traditional-care respondents had enrolled in the program during their first pregnancy, compared to 22.4% of the Virtual-care respondents (estimated difference = 22.1%, 95% CI 8.4, 35.9%; p = .003).
Satisfaction Scores
We evaluated domain and overall satisfaction using analysis of variance (ANOVA). Excluding questions from the technology domain, overall satisfaction was significantly correlated with cohort (F(1,169) = 12.4, p < .001). This finding persisted in a model considering overall satisfaction to be inclusive of questions from the technology domain (F(1,169) = 7.6, p = .006). Excluding the technology domain, overall satisfaction was 4.75 ± 0.44 for Virtual-care respondents. Including the technology domain, overall satisfaction for Virtual-care respondents was 4.69 ± 0.44. Overall satisfaction for Traditional-care patients was 4.46 ± 0.59.
Satisfaction scores of Virtual-care respondents were also significantly higher for each domain (all p < .05). The largest discrepancy between scores was observed in the Scheduling domain with Virtual-care respondents reporting a mean score of 4.81 ± 0.41 compared to 4.32 ± 0.57 for Traditional-care patients (p < .001). The smallest discrepancy was in the Personal domain with a Virtual-care respondent mean of 4.70 ± 0.55 compared to 4.44 ± 0.64 for Traditional-care respondents (p = .01). Figure 1 provides graphical distributions of each domain and the overall satisfaction score for the cohorts, illustrating the significantly smaller variance present among the Virtual-care respondents.
Distributions of satisfaction scores by domain (Scheduling, Provider, Personal, General) and overall satisfaction (Overall). Numeric means ± SD and p-values associated with ANOVA models comparing scores by group provided below each domain. Dots represent outlying values. T traditional-care; V virtual-care
Questionnaire Validity and Reliability
Internal consistency was validated with all Pearson correlations ≥0.4 for domains and their respective questionnaire items and Cronbach’s alpha ≥0.7 for each domain. Among Traditional-care respondents, the provider domain was most highly correlated with total satisfaction (r = .94, 95% CI 0.91, 0.96). as were the general (r = .93, 95% CI 0.90, 0.95) and personal (r = .90, 95% CI 0.86, 0.93) domains. The scheduling domain, however, was moderately associated with total satisfaction (r = .60, 95% CI 0.45, 0.71). Among Virtual-care respondents, the personal domain was most highly correlated with overall satisfaction (r = .93, 95% CI 0.88, 0.95), followed by the general (r = .89, 95% CI 0.83, 0.93), provider (r = .86, 95% CI 0.78, 0.91) and scheduling domains (r = .81, 95% CI 0.71, 0.87).
In both groups of respondents, the questionnaire items that correlated most strongly with overall satisfaction were: overall rating of care received, provider taking the time to listen, provider’s concern for questions, and response to needs and concerns (all r > .8, all p > .001). For Virtual-care respondents, ease of accessing the OB was also strongly correlated with overall satisfaction (4.52 ± 0.82, r = .81, 95% CI 0.71, 0.88; p < .001) as was convenience of visit times and dates (4.88 ± 0.37, r = .80, 95% CI: 0.70, 0.87; p < .001). Questions with strong correlations to overall satisfaction for Traditional-care respondents included explanations about procedures occurring during the visits (4.50 ± 0.76, r = .82, 95% CI 0.75, 0.88; p < .001) and friendliness of the provider (4.64 ± 0.71, r = .82, 95% CI 0.74, 0.88; p < .001). All other questions demonstrated a low to moderate correlation with overall satisfaction (r between 0.35 and 0.79; Table 3).
Track Specific Questions
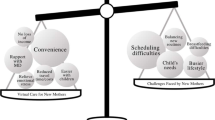
The Virtual-care patients were asked questions in the domain of technology. The mean satisfaction score for the technology domain was 4.43 ± 0.64, which correlated significantly with overall satisfaction (r = .77, 95% CI 0.66, 0.85; p < .001). 85% of the Virtual-care respondents completed 3–5 videoconference encounters; 93% of respondents reported visits occurring at home and 17% reported visits occurring at work. Three respondents did indicate having conducted Virtual Visits while on vacation. Traditional-care respondents were asked to select from a set of nine reasons for not choosing the Virtual Visit program. 71.9% of the Traditional-care respondents indicated a desire to see her provider at each prenatal encounter as a primary reason for opting out of Virtual Visits. Nine Traditional-care respondents (9.4%) indicated discomfort with using the blood pressure cuff and Doppler as a reason for declining participation in the Virtual Visits and two (2.1%) indicated concern with the security of connecting wirelessly for the visits as a motivation for declination.
Factors Influencing Track Selection
Using a stepwise logistic regression with the Akaike Information Criterion for variable selection, we evaluated the impact of background characteristics factors on odds of track selection among respondents. We entered the following variables into the model: parity (1, 2, or ≥3), age (as a continuous variable); partnered, prior pregnancy loss, Caucasian race, drive to obstetrician’s office <5 miles, and household income ≥$100,000 were passed to the model as binary variables. The ordinal variable parity and the binary variable partnered were retained for full analysis and increasing parity, alone, was associated with elevated odds of patient enrollment in the Virtual Visit program (OR 2.3; 95% CI 1.5, 3.5; p < .001). The percentage of respondents enrolled during their first pregnancy was 44.8% Traditional-care compared to 22.7% Virtual-care. 13.5% of Traditional respondents enrolled during their third or higher pregnancy compared to 34.7% of Virtual respondents. However, the percentage of respondents enrolled during a second pregnancy was nearly identical – 39.6% Traditional compared to 40.0% Virtual.
Question Level Analyses
Sixteen of the Likert response questions were identical between the two surveys. Mean values were >4 for all of these questions in both cohorts, but mean response values of Virtual-care respondents were higher for every question than for Traditional-care respondents (Table 1). These differences were statistically significant with the exception of ratings for provider skill and knowledge, concern for privacy, overall satisfaction with care, and likelihood of seeking care at our institution in the future. The largest discrepancies existed in the scheduling domain, with over a half-point difference for frequency of visits starting on time (4.20 vs. 4.76; p < .001) and convenience of visit dates and times (4.31 vs. 4.88; p < .001).
Discussion
The Virtual Visit structure was designed to provide an alternative to standard of care obstetric services for low-risk patients that would increase convenience for pregnant women while upholding the high level of provider interaction that has been reported as desirable to patients. The program affords patients increased engagement in their care through the use of the Doppler and the blood pressure cuff. Our data demonstrate that a mixed-model of care, interspersing videoconference encounters with face-to-face physician visits, can be pleasing to patients. Satisfaction with both prenatal care delivery modalities was high in our population, and satisfaction among Virtual-care respondents was significantly higher than that of Traditional-care respondents in all domains and overall.
We consider patient satisfaction from five domains, of which four are comparable between Traditional-care and Virtual-care groups, using tools that demonstrated acceptable reliability and validity. The Traditional-care respondent cohort reported comparatively lower domain and overall average scores as compared with members of the Virtual-care respondent group. This suggests directions for future quality improvement efforts for Traditional-care patients, with special attention to the scheduling domain, which showed the most drastic difference between groups, and questionnaire-item directed efforts, such as ease of accessing obstetrician, which was one of the lowest scoring items for the Traditional-care respondents.
The requirement that Virtual-care patients connect via videoconference and use a handheld Doppler and blood pressure cuff did not significantly impact overall satisfaction of the Virtual-care respondents. However, questions in this domain scored considerably lower for Virtual-care patients than other domains. While ease of using the blood pressure monitor and Doppler were only slightly lower than the majority of questionnaire item averages, scores for ease of connecting for the visits and quality of connection during the visits were markedly lower. This warrants further exploration, as videoconference platforms varied across the study time period and by patient preference. The cause of lowered satisfaction may have root causes linked to a variety of unmeasured sources, such as patient familiarity and comfort with different videoconference applications, variation in quality of wireless connectivity on the patient or provider end, or technology platform.
The non-significant associations between demographic characteristics and care delivery method (Virtual vs. Traditional) suggest that women who are pregnant for the first time may be significantly less likely to opt for Virtual Visits than women who are already mothers. This finding is consistent with our previous analysis, though in the prior work we also saw significant associations between track selection and partner status and enrollment in the governmental supplemental nutrition program WIC (Pflugeisen et al. 2016). The current work further suggests that women who select Traditional care over a mixture of videoconference and in-clinic visits are highly motivated by a desire to interact face-to-face with the provider at every opportunity. Such findings are highly supportive of upholding a choice-based model for patients. Further work is needed to better understand motivating factors for selection of the Virtual and Traditional care paradigms.
A critical area of future work for this model of care is a randomized controlled trial designed to assess maternal outcomes, both medical and psychosocial, fetal outcomes, and patient satisfaction associated with the program. Excessive weight gain and elevated blood pressure are significant risk factors for adverse pregnancy outcomes including gestational diabetes, premature birth, miscarriage, and preeclampsia (Xiong et al. 2006). Perinatal fetal surveillance has long been used to evaluate the risk of fetal death in high-risk pregnancies. The technology that is now available allows these three critical risk measurements (weight, blood pressure, and fetal heart tones) to be performed by low-risk pregnant women in the home setting and require full evaluation from clinical outcomes to patient reported satisfaction.
A cost analysis of this program is also an important area of future work. The primary limitations of this study are the implicit bias present in retrospective, voluntary response survey studies and the relatively low response rates despite the structured survey distribution and follow up methodology. Additionally, because we allowed for anonymous responses, we were unable to compare characteristics of respondents and non-respondents. However, as the importance of patient satisfaction continues to increase in the provision of health care, this work is an important first step in seeking the antenatal patient’s voice and understanding her perspective.
References
Alexander, G. R., & Kotelchuck, M. (2001). Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public health reports (Washington, D. C.: 1974), 116(4), 306–316.
American Academy of Pediatrics and American College of Obstetricians and Gynecologists. (2012). Guidelines for perinatal care (7th edition). Elk Grove Village, IL: American Academy of Pediatrics.
Baldwin, L. M., Raine, T., Jenkins, L. D., Hart, L. G., & Rosenblatt, R. (1994). Do providers adhere to ACOG standards? The case of prenatal care. Obstetrics and Gynecology, 84(4), 549–556.
Butler Tobah, Y. S., LeBlanc, A., Branda, M., Inselman, J., Gostout, B., & Famuyide, A. (2016). OB nest-a novel approach to prenatal care [21]. Obstetrics & Gynecology, 127(Suppl 1), 7S-8S. doi:10.1097/01.aog.0000483637.05137.18.
Carroli, G., Villar, J., Piaggio, G., Khan-Neelofur, D., Gulmezoglu, M., Mugford, M., & Bersgjo, P. (2001). WHO systematic review of randomised controlled trials of routine antenatal care. Lancet, 357(9268), 1565–1570. doi:10.1016/s0140-6736(00)04723-1.
Dillman, D. A. (1978). Mail and telephone surveys: The total design method. New York: Wiley.
Dowswell, T., Carroli, G., Duley, L., Gates, S., Gulmezoglu, A. M., Khan-Neelofur, D., & Piaggio, G. G. (2010). Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev, 10, CD000934. doi:10.1002/14651858.CD000934.pub2.
Jewell, D., Sharp, D., Sanders, J., & Peters, T. J. (2000). A randomised controlled trial of flexibility in routine antenatal care. BJOG, 107(10), 1241–1247.
Long, M. C., Angtuaco, T., & Lowery, C. (2014). Ultrasound in telemedicine: Its impact in high-risk obstetric health care delivery. Ultrasound Quarterly, 30(3), 167–172. doi:10.1097/ruq.0000000000000073.
Lowery, C., Bronstein, J., McGhee, J., Ott, R., Reece, E. A., & Mays, G. P. (2007). ANGELS and University of Arkansas for Medical Sciences paradigm for distant obstetrical care delivery. American Journal of Obstetrics and Gynecology, 196(6), 534.e1–534.e9. doi:10.1016/j.ajog.2007.01.027.
Magann, E. F., McKelvey, S. S., Hitt, W. C., Smith, M. V., Azam, G. A., & Lowery, C. L. (2011). The use of telemedicine in obstetrics: a review of the literature. Obstetrical & Gynecological Survey, 66(3), 170–178.
Marko, K. I., Ganju, N., Brown, J., Benham, J., & Gaba, N. D. (2016). Remote Prenatal Care Monitoring With Digital Health Tools Can Reduce Visit Frequency While Improving Satisfaction [3]. Obstetrics & Gynecology, 127(Suppl 1), 1S. doi:10.1097/01.AOG.0000483620.40988.df.
McDuffie, R. S. Jr., Beck, A., Bischoff, K., Cross, J., & Orleans, M. (1996). Effect of frequency of prenatal care visits on perinatal outcome among low-risk women. A randomized controlled trial. JAMA, 275(11), 847–851.
McDuffie, R. S. Jr., Bischoff, K. J., Beck, A., & Orleans, M. (1997). Does reducing the number of prenatal office visits for low-risk women result in increased use of other medical services? Obstetrics and Gynecology, 90(1), 68–70. doi:10.1016/s0029-7844(97)00136-1.
Nudell, J., Slade, A., Jovanovic, L., & Hod, M. (2011). Technology and pregnancy. International Journal of Clinical Practice, (170), 55–60. doi:10.1111/j.1742-1241.2010.02579.x.
Odibo, I. N., Wendel, P. J., & Magann, E. F. (2013). Telemedicine in obstetrics. Clinical Obstetrics and Gynecology, 56(3), 422–433. doi:10.1097/GRF.0b013e318290fef0.
Pflugeisen, B., McCarren, C., Poore, S., Carlile, M., & Schroeder, R. (2016). Virtual Visits: Managing antepartum care with modern technology. MCN Am J Matern Child Nurs, 41(1), 24–30.
R Core Team (2013). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. URL http://www.R-project.org/. Retrieved from http://www.R-project.org/.
Ridgeway, J. L., LeBlanc, A., Branda, M., Harms, R. W., Morris, M. A., Nesbitt, K., & Famuyide, A. (2015). Implementation of a new prenatal care model to reduce office visits and increase connectivity and continuity of care: protocol for a mixed-methods study. BMC Pregnancy and Childbirth, 15, 323. doi:10.1186/s12884-015-0762-2.
Sikorski, J., Wilson, J., Clement, S., Das, S., & Smeeton, N. (1996). A randomised controlled trial comparing two schedules of antenatal visits: the antenatal care project. BMJ, 312(7030), 546–553.
Villar, J., Carroli, G., Khan-Neelofur, D., Piaggio, G., & Gulmezoglu, M. (2001). Patterns of routine antenatal care for low-risk pregnancy. Cochrane Database of Systematic Reviews, 4, CD000934. doi:10.1002/14651858.cd000934.
Walker, D. S., McCully, L., & Vest, V. (2001). Evidence-based prenatal care visits: When less is more. Journal of Midwifery & Women’s Health, 46(3), 146–151.
Wood, D. (2011). STORC helps deliver healthy babies: The telemedicine program that serves rural women with high-risk pregnancies. Telemedicine Journal and e-Health, 17(1), 2–4. doi:10.1089/tmj.2011.9996.
Xiong, X., Buekens, P., Fraser, W. D., Beck, J., & Offenbacher, S. (2006). Periodontal disease and adverse pregnancy outcomes: A systematic review. BJOG, 113(2), 135–143. doi:10.1111/j.1471-0528.2005.00827.x.
Acknowledgements
The authors wish to acknowledge the innovators of the Virtual Visit Program—Christi McCarren, Dr. Richard Schroeder, and Dr. Steven Poore—and the ARNP who conducts the Virtual Visits—Malinda Carlile. This work was funded by the MultiCare Institute for Research & Innovation Philanthropic Funds.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pflugeisen, B.M., Mou, J. Patient Satisfaction with Virtual Obstetric Care. Matern Child Health J 21, 1544–1551 (2017). https://doi.org/10.1007/s10995-017-2284-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-017-2284-1