Abstract
Objectives Despite widely-known negative effects of substance use disorders (SUD) on women, children, and society, knowledge about population-based prevalence and impact of SUD and SUD treatment during the perinatal period is limited. Methods Population-based data from 375,851 singleton deliveries in Massachusetts 2003–2007 were drawn from a maternal-infant longitudinally-linked statewide dataset of vital statistics, hospital discharges (including emergency department (ED) visits), and SUD treatment records. Maternal SUD and SUD treatment were identified from 1-year pre-conception through delivery. We determined (1) the prevalence of SUD and SUD treatment; (2) the association of SUD with women’s perinatal health service utilization, obstetric experiences, and birth outcomes; and (3) the association of SUD treatment with birth outcomes, using both bivariate and adjusted analyses. Results 5.5% of Massachusetts’s deliveries between 2003 and 2007 occurred in mothers with SUD, but only 66% of them received SUD treatment pre-delivery. Women with SUD were poorer, less educated and had more health problems; utilized less prenatal care but more antenatal ED visits and hospitalizations, and had worse obstetric and birth outcomes. In adjusted analyses, SUD was associated with higher risk of prematurity (AOR 1.35, 95% CI 1.28–1.41) and low birth weight (LBW) (AOR 1.73, 95% CI 1.64–1.82). Women receiving SUD treatment had lower odds of prematurity (AOR 0.61, 95% CI 0.55–0.68) and LBW (AOR 0.54, 95% CI 0.49–0.61). Conclusions for Practice SUD treatment may improve perinatal outcomes among pregnant women with SUD, but many who need treatment don’t receive it. Longitudinally-linked existing public health and programmatic records provide opportunities for states to monitor SUD identification and treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
What is known State-specific data regarding prevalence of substance abuse disorder (SUD) in the perinatal period are limited, as is research on effects of SUD treatment on delivery outcomes. States need these analyses to inform programming and policy decisions. This study adds The novel linked dataset utilized here provides population-level, state-specific information about SUD prevalence, perinatal health services utilization, birth complications, and SUD treatment prior to delivery. This study provides new information on negative maternal reproductive health outcomes associated with SUD, unmet SUD treatment need, and reduction in risk for prematurity and LBW after SUD treatment on a population-level.
Introduction
Substance use disorder (SUD) is a national public health problem among women of reproductive age, with potential consequences across generations. Substance use and abuse during the prenatal period is associated with increased risks for obstetric and medical complications (Behnke and Smith 2013; McDonald et al. 2007; Lester et al. 2002; Wright and Walker 2001; Huestis and Choo 2002; Tuthill 2000; Ness et al. 1999), less prenatal care (Parlier et al. 2014; Behnke and Smith 2013; Funkhouser et al. 1993), poor birth outcomes (Conradt et al. 2014; Shankaran et al. 2004; Huestis and Choo 2002; Lester et al. 2002), and long-term health and behavioral problems in offspring (Behnke and Smith 2013; Lester and Lagasse 2010; Boucher et al. 2008; Miller-Loncar et al. 2005; Bada et al. 2002; Ornoy et al. 2001). Data from U.S. surveys indicate that approximately 11.9% of women aged 15–44 report illicit drug use in the past month, and 23.7% report heavy or binge alcohol use, with fewer pregnant women using illicit drugs (5.3%) or heavy or binge drinking (2.8%) (Center for Behavioral Health Statistics and Quality 2015; Pan and Yi 2013). The prevention of SUD is thus a public health priority with major implications for maternal and child health.
Despite the widely-known negative effects of SUD on women, children, and society, knowledge about the population-based prevalence and the impact of SUD during the perinatal period is limited and even less is known about the impact of SUD treatment on birth outcomes. Current substance abuse surveillance efforts depend on either: (1) medical record review for those who elect to enroll in studies, which does not provide generalizable or gender-specific data (Harrison and Sidebottom 2008; Fabris et al. 1998; Funkhouser et al. 1993); (2) biologic specimen testing (Behnke 2013), which is neither systematically administered during pregnancy nor universally at the time of delivery and depends on the timing of drug usage; or (3) national surveys, which only capture self-reported medical/SUD conditions (Bada et al. 2002). Epidemiologic analyses often separate the mother–child dyad into unrelated individuals, thus limiting investigation of the impact of maternal SUD and SUD treatment on subsequent birth outcomes. Moreover, most state agencies can record frequencies of SUD treatment episodes, but can not examine patterns of treatment over time for individuals or assess the impact of treatment on women’s or infants’ health outcomes.
The current study derives from a larger investigation of SUD among all Massachusetts women of childbearing age (15–49) in 2002–2008 (Bernstein et al. 2015). In that study, 8.5% of women aged 15–49 were positive for SUD, and only 48% of those women received specialty SUD treatment. Women who received SUD services were less likely to relapse or utilize an emergency department in the year following treatment.
Our aims were to determine: (1) the prevalence of SUD and SUD treatment (overall and by maternal socio-demographic and substance use characteristics); (2) the association between SUD and women’s perinatal health service utilization, obstetric experiences, and birth outcomes [prematurity, low birth weight (LBW), fetal death, neonatal mortality, and post neonatal mortality]; and (3) the association between SUD treatment and birth outcomes among deliveries to women with SUD, among Massachusetts women delivering singleton infants during the study period To our knowledge, this is the first study to directly investigate SUD identification and treatment among a population-based sample of reproductive-aged delivering women living in the U.S.
Methods
Data Base
Institutional Review Boards of Boston University Medical Campus, Massachusetts General Hospital, and the Massachusetts Department of Public Health approved this study. We used three data sources to capture documentation of SUD among women of reproductive age in Massachusetts: (1) the Massachusetts Center for Health Information and Analysis (CHIA) case mix data, which provided SUD-related diagnostic codes from statewide hospital discharge records for all inpatient, observational stay, and emergency department discharges for women aged 15–49 years, including hospital-based inpatient substance abuse treatment services; (2) the Massachusetts Pregnancy to Early Life Longitudinal (PELL) data system, which links birth records to corresponding hospital delivery discharge records, and allows for extraction of evidence of SUDs from both maternal and infant records; and (3) the Massachusetts Bureau of Substance Abuse Services (BSAS) treatment dataset, which provides information about SUD treatment need and utilization in all publicly-funded free-standing SUD specialty treatment programs in the state.
The linkage of these three datasets into singular limited data set, described elsewhere in detail (Bernstein et al. 2015), involved four broad steps: (1) aggregation of individual hospital utilization episodes (~6,000,000 records) into individual women-level records (~1,750,000); (2) linkage of these records to BSAS program records; (3) linkage to the PELL database of deliveries within the state; and (4) identification of women with recent pregnancies in the BSAS dataset.
Study Population
We restricted our study sample initially to women aged 15–49 years who received any inpatient (including deliveries), observational stay, emergency department, or SUD specialty treatment services in MA hospitals, or who participated in any BSAS SUD treatment programs between January 1, 2002 and December 31, 2008. We then further limited the study population to those women (N = 316,839) who had a least one singleton delivery (live or stillborn) between January 1, 2003 and December 31, 2007. We then accounted for their sequential singleton deliveries during the study time period, resulting in a total N = 375,851 of singleton deliveries, the unit of analysis for the current study. We further allowed for an additional year of data (2008) to ascertain infant mortality.
Measures
Substance Use Disorder
We classified women as having SUD based on: (1) birth certificate mention of a positive neonatal toxicology screen or fetal alcohol syndrome; (2) a BSAS treatment system admission record; or (3) specific International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) codes identified by the Explicit Mention of Substance Abuse Need for Treatment in Women (EMSANT-W) algorithm, developed to identify women of reproductive age with SUD through their own diagnosed substance-related health conditions and those of their neonates. EMSANT-W is more fully described elsewhere (Derrington et al. 2015). Women who appeared in the dataset with no evidence of SUD from any source were classified as “non-SUD”.
Data on specific type of drug usage were obtained from hospital and emergency department records, and reports of “drug of choice” on admission to the Massachusetts BSAS treatment system dataset. We differentiated single substance use (alcohol only or drugs only) from “poly-use” (alcohol and drugs together), then by specific substances of interest: alcohol, crack/cocaine, heroin/opiates, cannabis, stimulants, and a grouped category consisting of sedatives, barbiturates, hypnotics, and anesthetics.
We used the PELL birth date to anchor all temporal measures (i.e., likely date of conception, timing of SUD identification and treatment) within the study period of 1 year pre-conception to date of delivery.
Treatment System Utilization
We characterized formal treatment of SUD treatment as (1) professional services received in a specialty treatment facility or hospital-based program; or (2) hospital-based services for detoxification. Specific evidence of treatment for SUD was based either on an admission to a SUD specialty treatment program monitored by BSAS (approximately 90% of all MA substance use treatment programs) or on an ICD-9-CM coding for an inpatient hospital-based detoxification admission. SUD treatment status was established independently for each delivery and defined based on the presence (yes/no) of any SUD treatment received during the time period between 1 year pre conception through delivery. Pre-conception date was established based on birth certificate information.
BSAS data available for this study included dates of admission and discharge (treatment duration), reason for discharge, drug of choice, and treatment modality (i.e., detoxification, outpatient, residential or medication-assisted treatment such as methadone/buprenorphine, and transitional and other recovery support services).
Because multiple treatment strategies are often utilized concurrently, we grouped types of treatment into two categories of services: ‘acute only’ (e.g., admission for inpatient detoxification and stabilization, generally for five or fewer days), and ‘extensive treatment’ (all other modalities). For example, an admission for transitional services might precede a residential admission or outpatient counseling, but all of these modalities together were defined as one extensive continuum of care and categorized together as ‘extensive treatment’ program services. (The impact of specific patterns of treatments and timing of treatment are beyond the scope of this initial paper).
Perinatal Outcomes
Perinatal outcomes derived from the MA PELL data system included: (1) LBW (<2500 g); (2) prematurity (<37 weeks gestation); (3) fetal death (>20 weeks gestation or >350 g); (4) neonatal mortality (0–28 days); and (5) post-neonatal mortality (29–365 days).
Maternal Obstetric Experiences (Outcomes)
Maternal obstetric experiences derived from PELL birth certificate and hospital discharge data included: (1) utilization of antenatal health services (prenatal care usage measured by the APNCU Index (Kotelchuck 1994), ED visits and hospital admissions); and (2) pregnancy-related morbidity (e.g., gestational diabetes, pregnancy induced hypertension) and delivery complications (e.g., premature rupture of membranes, fever, C-section).
Covariates
Socio-demographic covariates derived from PELL included maternal age, race/ethnicity, primary language, education level, marital status, parity, MA state region of residence, and health insurance coverage at birth. Specific chronic and acute medical conditions known to co-occur with SUD were identified through hospital ICD-9-CM diagnosis codes and birth certificate check-off boxes, including anemia, cardiac disease, diabetes, hepatitis B or C, hypertension, lupus erythematosis, pneumonia, renal disease, and seizure disorder.
Finally, we created summary variables for any residual chronic, non-SUD-related maternal health condition and for a psychiatric comorbidity history, which included ICD-9 codes for any mood disorders, psychoses, paranoid and anxiety states, personality disorders, adjustment disorders, PTSD, and stress reactions.
Analytic Approach
SAS v. 9.3 (Cary, NC) was used for all data linkage and analyses. We determined prevalence of SUD and SUD treatment, and then used Chi square analysis to evaluate associations of maternal and infant socio-demographic, birth, and health characteristics with SUD and SUD treatment. Because of the large study sample, virtually all the bivariate Chi square and all multivariate Wald Chi square relationships are statistically significant at p < .001 and p values are not reported further in the text. We then used multivariate logistic regression analyses to estimate the association of SUD with infant outcomes including LBW, prematurity, fetal death, neonatal mortality, and post-neonatal infant mortality. The first model estimated unadjusted associations and the second model controlled for maternal age, race/ethnicity, primary language, education, marital status, parity, health insurance coverage, region of residence, chronic health conditions, psychiatric co-morbidity, adequacy of prenatal care, pregnancy-related conditions, delivery complications, and method of delivery. Finally, among women with identified SUD, we estimated the impact of SUD treatment on infant outcomes, using multivariable analyses controlling for the aforementioned covariates. In all multivariable models, we used generalized estimating equations (GEE) to account for the non-independence of data from women who had more than one delivery during the time period.
Results
SUD Prevalence
Among 375,851 MA singleton deliveries during 2003–2007, 5.5% or 20,707 occurred to women with SUD identified within 1 year of conception, during pregnancy, or at the time of delivery. Just over one-third (35.5%) were identified from BSAS records only; 49.9% from the EMSANT-W algorithm only; and 14.6% from both (data not shown).
Among the women with SUD, 15.9% used alcohol only; 34.2% used drugs only; and 49.9% used both alcohol and drugs. The primary types of substance used were alcohol (57.3%); crack/cocaine (38.9%); heroin, opiates, and/or methadone (39.5%); sedatives, barbiturates, hypnotics, and/or anesthetics (5.4%); and cannabis (37.2%). (Percentages add up to more than 100% due to multiple types of substances used) (data not shown in tables).
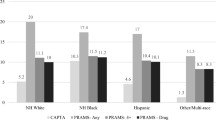
Characteristics of Women with SUD vs. Women without SUD
Women with SUD had more socio-demographic and health disadvantages than women without SUD (Table 1): they were younger (44.7 vs. 27.6% under 25), less educated (55.0 vs. 35.4% high school or less), and less likely to be married (55.8 vs. 70.6%) or have private health insurance (62.1 vs. 36.0%). They also had more pre-existing health conditions (65.1 vs. 44.1%) and co-morbid psychiatric diagnoses (53.1 vs. 13.1%).
Maternal Perinatal Experiences
Compared to women without SUD, women with SUD diagnoses were more likely to have experienced ED visits (38.3 vs. 21.9%) and hospitalizations (24.4 vs. 16.4%) during the antenatal period, but less preventive prenatal care (Table 2). Women with SUD had slightly more pregnancy-related morbidity and delivery complications (detailed maternal morbidity and complications data available from the authors).
SUD and Birth Outcomes
Deliveries to women with SUD had higher rates of LBW (11.1 vs. 5.5%), prematurity (13.1 vs. 8.7%), fetal death (0.6 vs. 0.4%), and neonatal mortality (0.66 vs. 0.36%) than deliveries to women without SUD (Table 3). After adjusting for covariates, deliveries to women with SUD were significantly more likely to be LBW (AOR = 1.73, 95% CI: 1.64–1.82) and premature (AOR = 1.35, 95% CI: 1.28–1.41) than deliveries to women without SUD.
SUD Treatment Prevalence
Among the 20,707 deliveries to women with indicators of SUD, 66% (13,723) had evidence of receiving some mode of SUD treatment during the study period (Table 1). Of those receiving treatment, 7% had acute detox treatment only and 93% had more ‘extensive’ treatment. The vast majority 84% (11,495) of women who received treatment services obtained them through free-standing specialty programs that report to BSAS.
SUD Treatment Access
Among all women with identified SUD need, those receiving SUD treatment compared to those without SUD treatment were more likely to be aged 30 or older (38.0 vs. 23.0%), have at least some college education (53.4 vs. 28.3%), be married (56.2 vs. 20.6%), have private insurance (49.8 vs. 14.6%), live in non-Boston metro regions of MA, and have fewer health (59.2 vs. 76.7%) or psychiatric (38.1 vs. 82.7%) conditions.
Treatment utilization also varied by the three broad substance groupings (data not shown). Cannabis use was associated with the lowest prevalence of treatment (29.9%) and barbiturate use was associated with the highest prevalence of treatment (49.4%), closely followed by heroin, opiates, and methadone (47.9%), alcohol (45.6%), and crack cocaine (42.0%).
SUD Treatment and Birth Outcomes
Among deliveries to women with identified SUD need (Table 4), we observed better birth outcomes for treated compared to untreated women. Treated women with SUD had lower rates of preterm (10.1 vs. 19.0%) and LBW (7.8 vs. 18.0%) births, as well as fetal, neonatal and post-neonatal mortality.
In multivariate analyses, SUD treatment was associated with reduced odds of LBW (AOR = 0.54, 95% CI: 0.49–0.61), preterm birth (AOR = 0.61, 95% CI: 0.55–0.68), and neonatal mortality (AOR = 0.49, 95% CI: 0.31–0.74). Fetal deaths and post-neonatal mortality could not be analyzed in the fully adjusted model due to the small number of cases.
We conducted additional post-hoc comparisons by type of SUD treatment, but found no significant differences between acute only treatment and extensive treatment (“Appendix” section). We further stratified by broad maternal drug of choice groups: SUD treatment was associated with lower odds of LBW and prematurity for all drug groups, though the strength of the association for the alcohol only group was less than the others. Any treatment was associated with lower odds of LBW and prematurity among drug and poly-drug/alcohol-using women, but not for the alcohol-only group.
Discussion
We identified markers for substance use disorder during the period from 1 year prior to conception through the time of delivery among 5.5% of women with singleton deliveries (live births and fetal losses) in Massachusetts between 2003 and 2007. This prevalence and the differences we observed in socio-demographic characteristics, perinatal health and health services, and birth outcomes between deliveries to women with and without markers for SUD confirm prior reports from survey data and small sample trials within the current large population-based data set. What is especially new and noteworthy here is the association of treatment for SUD and lower risk of adverse birth outcomes on a population basis.
SUD Prevalence Estimation
Our population-based prevalence of 5.5% deliveries to SUD-positive women in Massachusetts is consistent with national surveys from the same time period (SAMHSA 2007a, b, 2008). This estimate is lower than the 8.5% SUD prevalence for all MA women aged 15–49 years (Bernstein et al. 2015), and consistent with other studies reporting less substance use by women during pregnancy (Pan and Yi 2013). Our findings may be more precise due to several strategies we used to identify women with SUD during the perinatal period. First, unlike previous analyses that have relied on a single data source, we identified women through birth records, BSAS participation records, and ED and hospitalization records. This linkage resulted in identification of women who may have opted not to disclose substance use in the medical setting—an important issue when substance use disclosure has legal (child protective/abuse) implications. Second, using the birth certificate data, with their gestational age markers, allowed us to assess the timing of when SUD identification and SUD treatment occurred in relation to the infant’s birth. Third, the inclusion of ED data, a frequent locus for treatment of SUD-associated health consequences, likely increased identification of women with SUD. Finally, the EMSANT-W identification algorithm provided us with a more comprehensive, gender-tailored identification of SUD using more precise criteria than previous reports (Derrington et al. 2015). We believe our population-based methodology identifies actual women with SUD rather than simply creating population estimates; and therefore allows for examination of the women’s subsequent health and health care, SUD treatment experiences, and their offspring’s health, which in turn can provide points of entry for public health program interventions.
SUD and Utilization of Perinatal Health Services
Our data show that SUD has a strong negative association with health care utilization during pregnancy. Roberts and Pies (2011) noted that women with SUD were inhibited by fear of being reported to Child Protective Services and by the burden of multiple socio-demographic/health risk factors that are associated with SUD. SUD increases pregnant women’s health status burden, and increases their usage of episodic and emergent health services, and makes for more complex deliveries.
SUD and Birth Outcomes
SUD is a multigenerational, life course chronic disease. This study, like other epidemiologic studies (Burns and Mattick 2007; Crome and Kumar 2007; McDonald 2007; Escobar et al. 2002), shows broad negative impacts of SUD on multiple birth outcomes, even after controlling for associated factors.
The current analysis did not reveal significant differences in maternal health, health services usage, or birth outcomes by drug type or by specific primary drug of choice. This finding may reflect the limitations of administrative data to identify principal substance use. Moreover, many substance users are poly-drug users and/or switch among substances, and thus could appear in many of the drug groupings in an administrative data system.
SUD Treatment
The most important new findings from this study concern utilization of SUD treatment. In this study population, a third of women with SUD did not have evidence of any treatment during the period of 1 year pre-conception through delivery. Among those treated, 7% received no further SUD services beyond detox services, which also reflects an insufficient response to their treatment needs. The gap between women with unmet SUD treatment needs and receipt of services represents too many missed opportunities for active engagement into effective treatment, especially given that MA is one of seven states that prioritize pregnant women for access to SUD treatment. These treatment figures are, however, higher than the 48% of all MA women (15–49) with SUD who received treatment within 1 year prior to or 1 year following SUD identification (Bernstein et al. 2015). We also found important disparities in receipt of treatment; women who were younger, Black or Hispanic, less educated, lacking private insurance, unmarried and with health or psychiatric morbidities were all less likely to get SUD treatment. This suggests a need to increase access to services for the most vulnerable segments of women with SUD.
SUD Treatment and Birth Outcomes
In MA, SUD treatment was associated with substantially better birth outcomes, particularly for LBW and prematurity. Prior research has been limited to small samples and specific treatments; this finding is the first demonstration, to our knowledge, of a positive association with treatment on a population basis. In other prior related studies, Bernstein et al. (2014, 2015) showed that among all MA SUD women aged 15–49 years, SUD treatment was associated with decreased subsequent ED visits, injuries, and hospitalizations within 1 year of treatment.
Limitations
Our prevalence estimate of 5.5% of infants delivered to women with SUD is likely an underestimation. SUD diagnostic codes may have been warranted but not recorded, because substance use was not the focus of a medical encounter, or providers were reluctant to enter this information into a legal record, or women were reluctant to disclose use.
Our population-based analysis did not have the benefit of triangulation with clinical data that might have revealed more cases of SUD. We employed strong epidemiologic measures of SUD prevalence and treatment; but recognize the limitations in the use of any secondary databased SUD measurement algorithm, detecting false positives or false negatives is problematic. Birth outcomes, such as gestational age, may also be incorrectly recorded. And methodologic limits to linkage of multiple data sets may also contribute to inaccurate estimates.
Differences in reproductive outcomes by SUD status or by SUD treatment exposure could be influenced by unidentified confounding risk factors that are differentially distributed across the SUD and SUD treatment groups. In particular, our data did not permit us to analyze birth outcomes by the quantity or severity of drug use either prior to treatment or post-treatment. Nor was the quantity and duration of tobacco use available for examination of their associations with pregnancy outcomes. And while the GEE outcome analyses statistically account for the non-independence of data associated with women who had multiple deliveries, sequential deliveries itself was not examined as a separate independent risk factor.
The definition of treatment was limited to services provided in professional medical or addiction treatment settings; and thus, Alcoholics Anonymous, Narcotics Anonymous or Driving While Intoxicated program participation was not included in this study. We also lacked treatment records from Veterans’ Administration or private facilities that did not contract with BSAS; nonetheless the sources we did have covered the vast majority of treatment options available for MA women with SUD.
Last, generalizability is limited by the age of the study data (2003–2007) and restriction to one state, since treatment access varies considerably over time and across regions of the country. However, our secondary data-based findings add to the existing prevalence estimates derived from surveys and samples restricted to women who received treatment, and allow, for the first time, a population-based analysis of the prevalence and possible impact of treatment.
Policy and Program Implications
Services for women with SUD who are or will become pregnant are inadequate even in Massachusetts, which provides a wide range of treatment modality options and venues. This study’s findings reinforce the need for women’s services, given the intergenerational importance of untreated SUD and the consequences for the health of both women and children. Creating linked, longitudinal data systems, with robust substance use measures, may help states improve their estimates of gender-specific SUD prevalence, treatment utilization, and health and health services consequences.
The life course effects of SUD can be modified, and pregnancy is often a very receptive period for behavioral change and intergenerational concerns. Infant outcomes may be improved among women with SUD who receive treatment. The study findings should give hope to women with SUD, their families, and clinicians, Clinicians have an important role to play in providing the study’s encouraging message to their clients. The study findings should also reinforce policy makers’ efforts to invest in treatment programs for women with SUD, which could lead to lower short- and long-term public expenditures and better population health outcomes.
References
Bada, H. S., Das, A., Bauer, C. R., Shanrakan, S., Lester, B., et al. (2002). Gestational cocaine exposure and intrauterine growth: Maternal lifestyle study. Obstetrics and Gynecology, 100, 916–924.
Behnke, M., Smith, V. C., Committee on Substance Abuse, Committee on Fetus and Newborn. (2013). Prenatal substance abuse: Short- and long-term effects on the exposed fetus. Pediatrics, 131, e1009–1024.
Bernstein, J., Belanoff, C., Cabral, H. J., Babakhanlou-Chase, H., Derrington, T., et al. (2015). Treatment outcomes for substance use disorder among women of reproductive age in Massachusetts. Drug and Alcohol Dependence, 147, 151–159.
Bernstein, J., Bernstein, E., Belanoff, C., Cabral, H. J., Babakhanlou-Chase, H., et al. (2014). The association of injury with substance abuse disorder among women of reproductive age: An opportunity to address a major contributor to recurrent preventable ED visits? Academic Emergency Medicine, 21, 1459–1468.
Boucher, N., Bairam, A., & Beaulac-Baillargeon, L. (2008). A new look at the neonate's clinical presentation after in utero exposure to antidepressants in late pregnancy. Journal of Clinical Psychopharmacology, 28(3), 334–339.
Burns, L., & Mattick, R. P. (2007). Using population data to examine the prevalence and correlates of neonatal abstinence syndrome. Drug and Alcohol Review, 26(5), 487–492.
CDC Number and age-adjusted rates of drug-poisoning deaths involving opioid analgesics and heroin: United States 2000–2014. Accessed 12/22/15 at http://www.cdc.gov/nchs/data/health_policy/AADR_drug_poisoning_involving_OA_Heroin_US_2000-2014.pdf.
Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States. Results from the 2014 National Survey on Drug Use and Health. (HHS Publication No. SMA 15-4927).
Conradt, E., Abar, B., Sheinkopf, S., Lester, B., et al. (2014). The role of prenatal substance exposure and early adversity on parasympathetic functioning from 3 to 6 years of age. Developmental Psychobiology, 56, 821–835.
Crome, I. B., & Kumar, M. T. (2007). Epidemiology of drug and alcohol use in young women. Seminars in Fetal and Neonatal. Medicine, 12(2), 98–105.
Derrington, T., Bernstein, J., Belanoff, C., Cabral, H. J., Babakhanlou-Chase, H., Diop, H., et al. (2015). Development of a grouping tool to identify women of child-bearing age with probable substance use disorders: the explicit-mention substance abuse need for treatment in women (EMSANT-W) algorithm. Maternal and Child Health Journal, 19(10), 2168–2178.
Escobar, G. J., Li, D. K., Armstrong, M. A., Gardner, M. N., Folck, B. F., et al. (2002). Neonatal sepsis workup in infants ≥2000 grams at birth: A population-based study. Pediatrics, 106, 256–263.
Fabris, C., Prandi, G., Perathoner, C., & Soldi, A. (1998). Neonatal drug addiction. Panminerva Medica, 40(3), 239–243.
Funkhouser, A. W., Butz, A. M., Feng, T. I., McCaul, M. E., & Rosenstein, B. J. (1993). Prenatal care and drug use in pregnant women. Drug and Alcohol Dependence, 33(1), 1–9.
Harrison, P. A., & Sidebottom, A. C. (2008). Systematic prenatal screening for psychosocial risks. Journal of Health Care for the Poor and Underserved, 19(1), 258–276.
Huestis, M. A., & Choo, R. E. (2002). Drug abuse’s smallest victims: In utero drug exposure. Forensic Science International, 128(1–2), 20–30.
Kotelchuck, M. (1994). An evaluation of the kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. American Journal of Public Health, 84(9), 1414–1420.
Lester, B. M., & Lagasse, L. L. (2010). Children of addicted women. Journal of Addictive Disease, 29(2), 259–276.
Lester, B. M., Tronick, E. Z., LaGasse, L., Seifer, R., Bauer, C. R., et al. (2002). The maternal lifestyle study: Effects of substance exposure during pregnancy on neurodevelopmental outcome in 1-month-old infants. Pediatrics, 110(6), 1182–1192.
McDonald, S. D., Vermeulen, M. J., & Ray, J. G. (2007). Risk of fetal death associated with maternal drug dependence and placental abruption: A population-based study. Journal of Obstetrics and Gynaecology of Canada, 29(7), 556–559.
Miller-Loncar, C., Lester, B. M., Seifer, R., Lagasse, L. L., Bauer, C. R., et al. (2005). Predictors of motor development in children prenatally exposed to cocaine. Neurotoxicology and Teratology, 27(2), 213–220.
Ness, R. B., Grisso, J. A., Hirschinger, N., et al. (1999). Cocaine and tobacco use and the risk of spontaneous abortion. New England Journal of Medicine, 340(5), 333–339.
Office of Applied Studies. (2007a). Substance abuse and mental health services administration. The NSDUH report: Substance use treatment among women of childbearing age. Rockville: National Clearinghouse for Alcohol and Drug Information.
Office of Applied Studies. (2007b) Substance abuse and mental health services administration (SAMHSA). Results from the 2006 national survey on drug use and health: National findings. Rockville: National Clearinghouse for Alcohol and Drug Information.
Office of Applied Studies. (2008) Substance abuse and mental health services administration (SAMHSA). Results from the 2007 national survey on drug use and health: National findings. Rockville: National Clearinghouse for Alcohol and Drug Information.
Ornoy, A., Segal, J., Bar-Hamburger, R., Greenbaum C. (2001). Developmental outcome of school-age children born to mothers with heroin dependency: Importance of environmental factors. Developmental Medicine and Child Neurolology, 43(10), 668–675.
Pan, I. J., & Yi, H. Y. (2013). Prevalence of hospitalized births affected by alcohol and drug and parturient women diagnosed with substance abuse at live birth delivery: United States, 1999–2008. Maternal and Child Health Journal 17, 667–676.
Parlier, A. B., Fagan, B., Ramage, M., Galvin, S. (2014). Prenatal care, pregnancy outcomes, and postpartum birth control plans among pregnant women with opiate addictions. Southern Medical Journal, 107, 676–683.
Roberts, S. C. M., & Pies, C. (2011). Complex calculations: How drug use during pregnancy becomes a barrier to prenatal care. Maternal and Child Health Journal, 15, 333–341.
Shankaran, S., Das, A., Bauer, C. R., Bada, H. S., Lester, B., et al. (2004). Association between patterns of maternal substance use and infant birth weight, length, and head circumference. Pediatrics, 114(2), e226–e234.
Tuthill, D. P. (2000). Tobacco and cocaine use were independent risk factors for spontaneous abortion in inner-city women. Evidence-based Obstetrics and Gynecology, 2(1), 14.
Wright, A., Walker, J. (2001). Drugs of abuse in pregnancy. Best Practice and Research in Clinical Obstetrics and Gynaecology, 15(6), 987–998.
Funding
Supported in part by NIH NIAAA R21AA018395, NIH NIDA R21DA027181, and supplemental funding from the Massachusetts Department of Public Health Bureau of Substance Abuse Services.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 5.
Rights and permissions
About this article
Cite this article
Kotelchuck, M., Cheng, E.R., Belanoff, C. et al. The Prevalence and Impact of Substance Use Disorder and Treatment on Maternal Obstetric Experiences and Birth Outcomes Among Singleton Deliveries in Massachusetts. Matern Child Health J 21, 893–902 (2017). https://doi.org/10.1007/s10995-016-2190-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-2190-y