Abstract
Objectives To ensure proper nutrition and optimal health outcomes, it is critical that infants are exclusively breastfed (0–6 months) and then receive adequate feeding from 6–23 months (breastfeeding and frequent feedings of complementary foods). Despite policies and guidelines on adequate feeding in Myanmar, past research has found low rates of adequately fed infants 0–11 months and little is known about the adequacy of feeding practices for children 12–23 months. The aim of this study is to understand the feeding practices of children aged 0–24 months in Myanmar and maternal characteristics associated with adequate feeding practices. Methods This study examines the rates of adequately fed infants and young children (0–23 months) in hard-to-reach townships in Myanmar from a cross-sectional, multistage cluster survey. Survey data on nutritional practices were collected from 489 mothers. Data were analyzed using multivariate regressions. Results We found that 41.8 % of infants under 6 months were exclusively breastfed, 63.2 % of those aged 6–11 months were adequately fed, and 10.3 % of 12–23 month-olds were adequately fed. In multivariate regressions we found that antenatal care visits [1–4 visits, AOR = 6.59 (p < 0.01) and >4 visits, AOR = 6.63 (p < 0.05)] was associated with exclusive breastfeeding for under 6 month old infants. Having >4 antenatal care visits [AOR = 9.97 (p < 0.05)] was associated with adequate feeding for 6–11 months old infants. Conclusions Future nutritional interventions and policies should focus on improving messaging about adequate feeding practices, especially for 12–23 months olds.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
This study highlights the lack of adequate child feeding practices, most especially for children 12–23 months, in Myanmar.
Introduction
Under-nutrition continues to be of concern in many developing countries given the strong relationship between inadequate infant and young child feeding and poor health outcomes of children. Poor childhood nutritional status is associated with long-term cognitive and developmental problems, which can impact a child’s future potential [1, 2]. Of the five sub-regions in Asia, Southeast Asia has the second highest prevalence and total number of children who are stunted (29.4 %, 15.6 million), wasted (9.4 %, 5.0 million) and underweight (18.3 %, 9.7 million) [3]. Myanmar has the fourth highest prevalence of underweight children (22.6 %) in the region [3]. The last national survey of women and children in Myanmar indicated that nearly one in four children under age five (22.6 %) are moderately underweight and 5.6 % are classified as severely underweight [4].
The international recommendation for adequate child nutrition is that children be breastfed exclusively for 6 months followed by continued breastfeeding along with the introduction of complementary (semi-solid and solid) food that is safe, appropriate and adequate for up to 2 years of age and beyond [5]. Exclusive breastfeeding among infants under 6 months along with adequate complementary feeding for children 6–23 months are the recommended gold standards for achieving optimal nutrition among children. When a child is 6 months of age, parents are advised to slowly introduce semi-solid and then solid foods, and other liquids such as water. However, there has been varying levels of adherence to this recommendation, particularly in Asia [3]. One recent study in South Asia indicated that there are several elements within the weaning period that can lead to inadequate feeding, including when complementary food is introduced, how often the child is fed relative to their age, the diversity of foods they eat, and the manner in which the food is cooked [3].
Several studies have explored infant and young child feeding but few have examined specifically the predictors, behaviours, and feeding practices among children 12–23 months of age. Past studies have found that only 23.6 % of children in Myanmar are exclusively breastfed up to the age of 6 months [4]. Analysis of large national survey data from nine East and Southeast Asian countries, including Myanmar, found that Myanmar had the lowest rate of timely introduction of complementary foods (5 %) but the highest rate of continued breastfeeding at 2 years of age (67 %) [6]. Past studies, such as those cited above, have not explored socio-demographic characteristics associated with adequate feeding practices. This information is important for future programs.
This study seeks to understand the feeding practices and adherence to adequate feeding goals for children under 24 months of age in Myanmar and explore socio-demographic factors associated with adequate feeding practices.
Methods
A cross-sectional household survey using multistage cluster sampling design was conducted to assess the use of reproductive, maternal, and child health products (including family planning, nutrition supplements, etc.) and services by currently married women of reproductive age among hard-to-reach townships in Myanmar. Hard-to-reach townships were determined based on the indicators of health needs, service coverage and poverty levels. In these townships, the combined population contributed approximately 7 % of Myanmar’s estimated population [7]. Ten townships were selected from 42 hard-to-reach townships using probability proportional to size (PPS) method. A total of 1800 currently married women aged 18–49 were recruited for the survey, including 348 from urban and 1452 from rural areas. To complete 1800 interviews, 2331 eligible women were approached of which 513 were not available for interviews, 16 refused and 2 women cancelled their participation. In selected wards and villages, the interviewer went from household to household to identify eligible participants using a screening questionnaire. Screening included questions to assess if (1) a respondent is a currently married women (2) aged between 18–49 years (3) usual resident of the household. Women who refused to participate or who were not able to be reached after two household visits were not included in the study. A total of 489 of the 1800 women from the sample had at least one child under 2 year-old and were included in this analysis. As this is a part of larger household survey with 1800 participants, 1311 women were not meeting the criteria of having a child under 2 years to answer the infant and young child feeding section. These women were interviewed for other relevant sections such as the utilization of reproductive health, maternal and child health products and services in the survey questionnaire.
Face-to-face interviews were conducted with a team of trained interviewers from September–October, 2014. All the interviews were conducted in the main Myanmar language. A modified form of questionnaire used in Multiple Indicator Cluster Survey Myanmar 2009–2010 was used for the study. The questionnaire was also pretested prior to the roll out of the full survey and revised for ease of understanding and administration.
The three main outcomes explored were: exclusive breastfeeding for 0–5 months old infants and adequate feeding practice for 6–23 months old infants and young children. The proportion of adequate feeding for different age groups were calculated by using the formulas described in Multiple Indicator Cluster Survey 2009–2010 Myanmar (UNICEF) and Indicators for assessing infant and young child feeding practices (WHO & UNICEF) [4, 5]. Adequate feeding practices for 6–23 months was determined based on 2 criteria: [1] infants must be currently breastfed; and [2] infants must receive minimum frequency of solid, semi-solid and soft complementary food within last 24-h. Guidelines suggest that, at a minimum, infants 6–8 months old be fed 2 or more times a day, infants 9–11 months old be fed 3 or more times a day and infants 12–23 months old be fed 4 or more times a day. Questions such as “Is the baby still breastfed? since this time yesterday, how many times did the baby eat solid, semi-solid, or soft foods other than liquids?” were used to assess the adequacy of feeding.
We included predictor variables related to women’s demographics, socio-economic characteristics, household characteristics, and maternal health service utilization. The residential area was defined as urban or rural. The median age of mothers was 30; therefore, a binary variable of under 30 years and above 30 years was created. Education was broken into three categories: illiterate/no schooling; primary or middle schooling; high school or higher education. Occupational status was coded as: housewife; skilled, unskilled and other family businesses; and white-collar professionals. Professionals, management staff, officers and clerical related workers were coded as white-collar professionals while skilled workers, those working in farm, fishery, forest related works, shop owners, small business owners were coded as skilled, unskilled and other family businesses. A binary variable of the number of children under 5 in the household was also created (1 vs. 2–4 children). Wealth quintiles were created using principal component analysis method which included a number of questions about house materials, access to electricity, etc. [8]. Health care utilization was measured using a variable about use of antenatal care (ANC): none; 1–4 visits; and more than 4 visits. A binary variable of whether the woman delivered the child with a skilled or unskilled health provider was also included. Binary variables were also created for the child’s age in each sub-group (under 6 months, 6–11 months and 12–23 months). For the 0–5 months group, the younger group refers to those 0–3 months and older group those 4–5 month; for the 6–11 month old group, the younger group was those 6–8 months and the older 9–11; and for the 12–23 months old group, the younger group was 12–17 and the older 18–23 months.
Bivariate analyses were conducted in order to assess the associations between the outcomes of interest and predictors. Next, we conducted multiple logistic regressions. Sampling weights were incorporated in the analyses to account for multistage cluster design. Stratified analyses were conducted in order to assess differences across age groups. All statistical analyses were performed using the Stata Statistical Software, version 11.0 [9].
The study was reviewed and approved by the Population Services International Research Ethics Board. Verbal informed consent was obtained from participants before taking part in the study.
Results
Proportion of Adequate Feeding
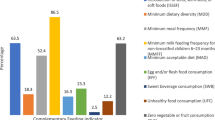
Adequate feeding indicators are age-specific for infants and young children. In this study, 41.8 % of infants under 6 months were exclusively breastfed (Table 1). For infants 6–11 months, 96.5 % were breastfed and 65.5 % received the required number of complementary feedings (solid foods at least 2 times a day for children 6–8 months and at least 3 times a day for those 9–11 months). This resulted in a total of 63.2 % of infants 6–11 months in the study meeting the adequate feeding threshold. In the study, 71.5 % of children 12–23 months were breastfed but only 14.1 % received the required number of complementary feedings (solids food at least 4 times a day). This resulted in a reduction in the percentage of children who were adequately fed (10.3 %) compared with the other age groups in the study.
Demographic Characteristics
Table 2 stratifies demographic characteristics by children’s age group and feeding practices. Across all child age groups, more women in the sample lived in rural compared to urban areas. There are more young mothers (≤30 years) across all child age groups. The majority of women in all groups had primary or middle education, ranging from 54.5 to 60.6 %, followed by illiterate/no formal education and then high school or higher education. More of the women with older children (12–23 months) had only 1 child in total, compared to women with children under 12 months. Women had, on average, 1.5 children under the age of 5. Most women delivered with an unskilled provider in all groups, and more women in all child age groups had children at the lower distribution of each child age group. There were no significant differences between the adequate and non-adequate feeding groups in any of the above categories.
The majority of women were housewives, ranging from 51.1–61.9 %, and in the 12–23 month old age group, a greater proportion of the group adequately feeding was housewives. In the 12–23 month old group, there were significant differences in terms of wealth status between the adequate and non-adequate feeders. In all child age groups, the mean number of ANC visits was about 3.5 and women who were exclusively breastfeeding versus not and women adequately feeding their 12–23 months old versus not had more ANC visits.
Multivariable Models: Associations Between Demographic Characteristics and Adequate Feeding, by Children’s Age Group
In multivariable regressions, rural women with infants under 6 months of age were 2.42 (95 % CI 0.79–7.42, p < 0.1) times more likely to practice exclusive breastfeeding, compared to urban women (Table 3). Women who worked in skilled, unskilled and other family businesses had 0.33 (0.10–1.10, p < 0.1) the odds of exclusive breastfeeding compared to housewives. Women who reported receiving antenatal care 1–4 times during pregnancy and women who reported receiving antenatal care more than 4 times had 6.59 (1.72–25.25, p < 0.01) and 6.63 (1.48–29.60, p < 0.05) the odds of exclusive breastfeeding, respectively, compared to women with no ANC. None of the other variables explored were significantly associated with exclusive breastfeeding.
Women with infants 6–11 months of age who were over 30 years-old were 3.78 (1.33–10.78, p < 0.05) times more likely to be practicing adequate feeding, compared to women under 30. Women who worked in skilled, unskilled or other family businesses had 2.59 (0.95–7.05, p < 0.1) the odds of practicing adequate feeding, compared to housewives. Women who received antenatal care more than 4 times were 9.97 (1.26–79.08, p < 0.01) more likely to be practicing adequate feeding, compared to women with no ANC. Having delivered with a skilled provider, compared to an unskilled provider, was associated with decreased odds of practicing adequate feeding (OR 0.18, 95 % CI 0.06–0.42, p < 0.01). None of the other variables explored were significantly associated with adequate feeding practices among women with 6–11 month old infants.
Women with children 12–23 months of age who were over 30 years old had increased odds of practicing adequate feeding, with an odds ratio of 3.56 (1.25–10.15, p < 0.05), compared to women under 30. Women with primary or middle school education and women with a high school or higher education had increased odds of practicing adequate feeding, by 3.25 (1.31–8.04, p < 0.05) and 7.06 (1.71–29.14, p < 0.05) respectively, compared to women with no education. None of the other variables explored were significantly associated with adequate feeding practices among women with infants 12–23 months of age.
Discussion
Our study found that children 12–23 months of age are faring much worse than children under 6 months and 6–11 months in terms of adequate feeding practices in Myanmar. Results find that there was a dramatic decline in adequate feeding practices for children in the 12–23 month age group. Nine in 10 of these children were being inadequately fed largely due to a large drop in the frequency of complementary feedings per day. Children in this age group should receive at least four feedings with complementary food in addition to breast milk, however, only 14 % of these children were. Very few studies, including the national MICS survey, have analyzed the frequency of complementary feeding among children 12–23 months in Myanmar. This age period is particularly critical in the overall health and development of the child. One study in Tanzania indicated that infants are particularly vulnerable to under-nutrition during the transition from breast milk (as the only source of nourishment) to solid foods [10]. If the transition away from breast milk is not complemented with sufficient and highly nutritious complementary foods, this can negatively affect the short and long term health and developmental outcomes of children.
A large proportion of infants less than 6 months were not meeting the gold standard of being exclusively breastfed; however, rates of exclusive breastfeeding in this study (41.8 %) were higher than what has been reported in the national MICS survey (2009–2010) (23.6 %) [4]. At the start of the recommended weaning age (6 months) and before their first birthday, a very large proportion of the children in this study were still being breastfed but a more moderate proportion was receiving the recommended number of complementary feedings. Hence, overall, adequate feeding practices of infants 6–11 months in this study (63.2 %) was higher than the last national survey (56.5 %), which shows some promise that the frequency of complementary feedings is more in line with international recommendations [4].
We also explored socio-demographic factors associated with exclusive breastfeeding among women with infants <6 months, and adequate feeding practices among women with 6–11 and 12–23 month old infants. Rural women were more likely to exclusively breastfeed, compared to urban women in this sample, perhaps because rural women are less likely to work outside the home, or social norms and support systems in rural areas are more supportive of breastfeeding. Women in skilled, unskilled or other family businesses, compared to being a housewife, were less likely to exclusively breastfeed. Past qualitative research in Myanmar found that working outside the home was one of the main barriers that women faced to exclusive breastfeeding [11]. Receiving antenatal care 1–4 times and more than 4 times was associated with increased women’s odds of exclusively breastfeeding, suggesting that antenatal care represents a good source of information to women about the benefits of exclusive breastfeeding, or that women who receive antenatal care are also the type of women who are more likely to breastfeed (highly motivated women). The receipt of antenatal care is highly correlated with many positive health behaviors, such as facility delivery; however, disentangling whether antenatal care promotes or is correlated with healthy behaviors, such as delivery in facilities or practice adequate feeding practices, is challenging [12].
Being older (over age 30) was associated with increased odds of adequate child feeding in both the 6–11 and 12–23 age groups. Past research in Asia and Africa has found a relationship between maternal age and breastfeeding, child feeding, or child stunting [13, 14]. Older women might be more empowered in their households and therefore have more access to resources to feed their children or be more able to gain information about appropriate feeding practices. Older women might also have more experience with raising other children—either their own or those of the extended family of community. In contrast to the findings on exclusive breastfeeding, participation in skilled, unskilled or other family businesses, compared to being a housewife, was positively associated with adequate feeding among the 6–11 month old infants, but this was not significant for the older age groups. Working mothers might be able to purchase more foods and therefore feed their children more than non-working mothers. Similar to exclusive breastfeeding, receiving antenatal care 4 or more times was associated with increased odds of practicing adequate feeding, although again this was not significant for the 12–23 month old infants. Perhaps information provided in antenatal care sessions is only retained for a few months post-partum, after which, message retention wanes. It is also possible that the messages received in antenatal care sessions are more focused on exclusive breastfeeding and when to introduce complementary food, and less focused on the frequency of complementary feedings needed to meet the adequacy threshold after their infants are 1 year of age.
For the women with infants aged 12–23 months, educational status was associated with adequate feeding practices. This suggests that more educated women are either better able to gain information about what to feed their children and how often to do so or better able to access adequate foods. If this information is not available in antenatal care sessions or during other contacts with health professionals, this could explain why these more educated women are able to gain information from other sources.
Surprisingly, delivery with a trained provider was associated with decreased odds of adequate feeding in the 6–11 month infants. Ideally, women who delivered with a skilled birth attendant should receive information about adequate feeding practices. It is also possible that women misreported the skill level of providers in the survey, since it is often difficult for women to identify who is a skilled or not-skilled provider, especially in rural areas where providers who are often seen in the community might not wear uniforms.
There are several limitations to this study. First, this is self-reported data from mothers, rather than directly observing feeding or reports of other family members about what they fed infants. Past research has found that other household members, such as husbands, grandmothers, older children etc. also provide food to children [11]. Hence, our measure of the number of times a child was fed might be an underestimate of the daily meals that a child received. It is also possible that women might be including her perception of all feedings that the children are receiving, including from other family members, and potentially over reporting. Furthermore, we only collected data on number of times the child was fed, and not the quality and quantity of those meals. WHO and UNICEF recommend that children are introduced to solid foods and liquids starting at 6 months, and that these foods meet certain nutritional standards and are prepared in a safe manner [15]. Past qualitative work in Myanmar found that mashed rice is the most common food introduced first, and that small children are fed few vegetables or meats [16]. Qualitative research found that women in Myanmar believe that rice is nutritious for babies and can help the baby resist the bite of poisonous insects, even though rice alone does not have adequate nutrition for children of this age group [17]. Since, in this context, families often first introduce foods of poor nutritional quality (rice, etc.), adequate feeding practices may even be lower than estimated in this study (had we been able to incorporate nutritional quality information). More information about the types of foods fed to children at the start of the weaning period is needed in this setting.
Finally, the sample population was drawn from townships identified as being hard-to-reach populations. Thus, these findings may not be generalizable to the entire population of Myanmar, and we would hypothesize that the rates of inadequate feeding practices would be higher in these townships than the country as a whole. The cross-sectional nature of this study restricts the interpretation of our analysis to associations, and some measures, such as times received antenatal care or types of providers seen in pregnancy and at delivery, might suffer from recall biases. Finally, due to the overall small sample size, some of the sub-groups became very small, resulting in large confidence intervals for some variables of interest. Future larger nationally representative samples should be collected that can confirm the findings of this analysis.
Despite these limitations, these findings highlight a neglected period for young children between 12–23 months of age in Myanmar, when adequate feeding practices drop precipitously. This is primarily due to children not being fed complementary foods enough times a day, rather than a lack of continued breastfeeding. There has been a concerted effort at promoting exclusive breastfeeding in Myanmar, which remains low; however, the findings of this study suggest that it is in fact the 12–23 month old children that are most at risk. This is an important period for health and development (including cognitive development) [18]. While other literature has highlighted the importance of improvements in feeding frequency and diet quality among children 6–24 months, the focus on the 12–23 months period has not been emphasized [19]. Current guidelines in Myanmar (and globally) highlight exclusive breastfeeding but do not provide detailed information to families about how much and what types of food children should be eating once they begin the weaning period. Our findings suggest that improving messaging through antenatal care sessions on the adequate feeding required to meet the proper nutrition requirements of 12–23 month olds could be successful. Increased and improved education about adequate child feeding practices at the beginning and during the weaning period, such as during interactions with health care providers for vaccinations throughout infancy and early child hood could also be a way of increase knowledge. Focusing on young women and women of low socio-economic status could also improve feeding for these especially high risk infants. It is essential to improve child-feeding practices for this vulnerable and neglected age group, to ensure the health and potential of the Myanmar population in years to come.
References
Shekar, M. (2006). Repositioning nutrition as central to development: A strategy for large scale action. Washingotn, DC: The World Bank.
Walker, S. P., Wachs, T. D., Gardner, J. M., et al. (2007). Child development: risk factors for adverse outcomes in developing countries. The Lancet, 369(9556), 145–157.
Chaparro, C., Oot, L., & Sethuraman, K. (2014). Overview of the nutrition situation in seven countries in Southeast Asia. Washington, DC: FHI 360/FANTA2014.
UNICEF (2011). Myanmar multiple indicator cluster survey 2009–2010.
World Health Organization. (2008). Indicators for assessing infant and young child feeding practices. France: WHO Library Cataloguing-in-Publication Data.
Dibley, M. J., Senarath, U., & Agho, K. E. (2010). Infant and young child feeding indicators across nine East and Southeast Asian countries: An analysis of National Survey Data 2000–2005. Public Health Nutrition, 13(9), 1296–1303. doi:10.1017/S1368980010000844.
Taw, P. N. (2009). Country report on the 2007 fertility and reproductive health survey. Myanmar: Ministry of Immigration and Population, Department of Population and UNFPA.
Filmer, D., & Pritchett, L. H. (2001). Estimating wealth effects without expenditure data-or tears: An application to educational enrollments in states of India. Demography, 38(1), 115–132.
StataCorp. (2011). Stata Statistical Software: Release 12. College Station, TX: StataCorp LP.
Mamiro, P. S., Kolsteren, P., Roberfroid, D., et al. (2005). Feeding practices and factors contributing to wasting, stunting, and iron-deficiency anaemia among 3–23-month old children in Kilosa district, rural Tanzania. Journal of Health, Population and Nutrition, 23(3), 222–230.
Thet, M. M., Khaing, E. E., Diamond-Smith, N., Sudhinaraset, M., Oo, S., & Aung, T. (2016). Barriers to exclusive breastfeeding in the Ayeyarwaddy region in Myanmar: Qualitative findings from mothers, grandmothers, and husbands. Appetite, 1(96), 62–69.
Diamond-Smith, N., & Sudhinaraset, M. (2015). Drivers of facility deliveries in Africa and Asia: regional analyses using the demographic and health surveys. Reproductive Health, 12(6), 1–14.
Kimani-Murage, E. W., Madise, N. J., Fotso, J.-C., et al. (2011). Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health, 11(396), 1.
Shroff, M., Griffiths, P., Adair, L., et al. (2009). Maternal autonomy is inversely related to child stunting in Andhra Pradesh, India. Maternal and Child Nutrition, 5(1), 64–74.
World Health Organization. (2003). Global stategy for infant and young child feeding. New York: UNICEF.
Chit, T. M., Kyi, H., & Thwin, A. (2003). Mothers’ beliefs and attitudes towards child weight, child feeding and related practices in Myanmar. Nutrition and Health, 17(3), 231–254. doi:10.1177/026010600301700306.
Thin Thin, D. (2003). Beliefs attitudes and practices of mother regarding exclusive breast feeding in Myanmar. Melbourne: La Trobe University.
Dewey, K. G., Cohen, R. J., & Rollins, N. C. (2004). Feeding of nonbreastfed children 6–24 months of age in developing countries. Food and Nutrition Bulletin, 25(4), 377–402.
Black, R. E., Allen, L. H., Bhutta, Z. A., et al. (2008). Maternal and child undernutrition: global and regional exposures and health consequences. The Lancet, 371(9608), 243–260.
Acknowledgments
The authors would like to thank Dr. Tin Aung (Director, Strategic Information Department), Dr. Nang Mo Hom (Research Unit/Strategic Information Department), U Zaw Win (Research Unit/Strategic Information Department) and staff from PSI Myanmar for providing the required support for the study. Our thanks will also go to the 3 Millennium Development Goal Fund (3MDG) for financial support to conduct the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that we have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Thet, M.M., Richards, LM., Sudhinaraset, M. et al. Assessing Rates of Inadequate Feeding Practices Among Children 12–24 months: Results from a Cross-Sectional Survey in Myanmar. Matern Child Health J 20, 1688–1695 (2016). https://doi.org/10.1007/s10995-016-1968-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-1968-2