Abstract
Objectives We assessed the impact of varying levels of smokefree regulations on birth outcomes and prenatal smoking. Methods We exploited variations in timing and regulation restrictiveness of West Virginia’s county smokefree regulations to assess their impact on birthweight, gestational age, low birthweight, very low birthweight, preterm birth, and prenatal smoking. We conducted regression analysis using state Vital Statistics individual-level data for singletons born to West Virginia residents between 1995–2010 (N = 293,715). Results Only more comprehensive smokefree regulations were associated with statistically significant favorable effects on birth outcomes in the full sample: Comprehensive (workplace/restaurant/bar ban) demonstrated increased birthweight (29 grams, p < 0.05) and gestational age (1.64 days, p < 0.01), as well as reductions in very low birthweight (−0.4 %, p < 0.05) and preterm birth (−1.5 %, p < 0.01); Restrictive (workplace/restaurant ban) demonstrated a small decrease in very low birthweight (−0.2 %, p < 0.05). Among less restrictive regulations: Moderate (workplace ban) was associated with a 23 g (p < 0.01) decrease in birthweight; Limited (partial ban) had no effect. Comprehensive’s improvements extended to most maternal groups, and were broadest among mothers 21+ years, non-smokers, and unmarried mothers. Prenatal smoking declined slightly (−1.7 %, p < 0.01) only among married women with Comprehensive. Conclusions Regulation restrictiveness is a determining factor in the impact of smokefree regulations on birth outcomes, with comprehensive smokefree regulations showing promise in improving birth outcomes. Favorable effects on birth outcomes appear to stem from reduced secondhand smoke exposure rather than reduced prenatal smoking prevalence. This study is limited by an inability to measure secondhand smoke exposure and the paucity of data on policy implementation and enforcement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
What is known on this subject? Smokefree regulations have the potential to improve birth outcomes by decreasing smoking prevalence among pregnant women and/or reducing secondhand smoke exposure during pregnancy. Research is limited, though, and does not yet provide a consensus statement.
What does this study add? To our knowledge, this is the first direct evaluation of varying degrees of regulation restrictiveness (comprehensive versus partial ban) on and the only long-term evaluation of birth outcomes and prenatal smoking. Also, most previous studies have utilized aggregate data; our study uses individual-level data allowing us to capture individual-level variations. Finally, this is the first study to incorporate pregnancy-related variables (parity, prenatal care, weight gain).
Introduction
Over the past 20 years, smokefree regulations in the workplace and public places have been enacted across the United States at the state, county, and municipal levels. These population-based smoking restrictions have been effective public health interventions in reducing hospital admissions for acute myocardial infarction, stroke, and asthma [6, 23, 27,30, 38], as well as decreasing cigarette consumption and smoking prevalence with variations by sex, age, and socioeconomic status [12, 17, 34, 44]. In addition to these improvements, smokefree regulations have the potential to improve birth outcomes by decreasing smoking prevalence among pregnant women and/or reducing exposure to secondhand smoke (SHS) during pregnancy.
Smokefree Regulations and Birth Outcomes
Smoking during pregnancy is a known risk factor for adverse birth outcomes, including low birthweight (LBW) (<2500 g), preterm birth (PTB) (<37 weeks gestation), neonatal death, sudden infant death syndrome, and spontaneous abortion [7, 20, 24, 28, 41]. Growing evidence indicates that exposure to SHS during pregnancy is also associated with increased risks of adverse birth outcomes, including LBW and possibly PTB and spontaneous abortion [14, 15, 24, 33, 42]. Though smokefree regulations can reduce smoking and SHS exposure, research on the effect of these policies is limited for the prenatal setting and does not yet provide a consensus statement. Additionally, there has been no direct evaluation of the degree of regulation restrictiveness (comprehensive versus partial ban)Footnote 1 on birth outcomes or prenatal smoking.
Studies evaluating the impact of comprehensive smoking bans (ban in workplaces/restaurants/bars) have been conducted at the national and local levels. Evaluations of comprehensive bans in Ireland [25, 26] and Scotland [31] and in the city of Pueblo, Colorado [35] levels have found statistically significant declines in PTB, small for gestational-age (SGA), and prenatal smoking prevalence, though the impact on risk of LBW was mixed. Additionally, Belgium’s national comprehensive smoking ban was implemented in three phases over several years with statistically significant reductions in PTB following each of the three phases, but no change in average birthweight (ABW), LBW, or SGA [13]. Finally, Norway’s ban in public places “where food or drink is served” was evaluated among hospitality workers, for whom it represented a comprehensive smoking ban (workplace/restaurant/bar); findings included statistically significant reductions in very low birthweight (VLBW) and PTB, stemming primarily from changes in prenatal smoking [8].
Smokefree regulations in the workplace have demonstrated less consistent results. A multi-state analysis using the CDC’s Pregnancy Risk Assessment Monitoring System (PRAMS) data found a slight decrease in PTB and small increase in gestational period only among mothers aged 25–34, but no impact on birthweight or prenatal smoking; existing local smokefree regulations were not accounted for [32]. In contrast, two unpublished state-level analyses using Vital Statistics data first for a single state [3] and then for all states [9], both accounting for local smokefree regulations, found small but significant decreases in birthweight, but no effect on gestational age, PTB, or prenatal smoking. While seemingly counterintuitive, these findings may support the limited body of research outside the prenatal context that suggests paradoxical effects can result from tobacco control measures due to compensatory smoking behaviors such as displacement of smoking from public places to private spaces or increased smoking intensity (extracting more nicotine per cigarette) [1, 2, 8]. These paradoxical findings have not, however, been universally supported by the research [10].
The Context of West Virginia
West Virginia (WV) has among the highest smoking prevalence in the United States both in the general population (WV = 28.6 %, US = 21.2 % in 2011) [11] and in the prenatal population (WV = 30.5 %, US = 10.7 % during third trimester in 2010) [40]. Importantly, WV is one of seven U.S. states without a statewide smoking regulation [4].Footnote 2 Unlike some states, however, WV has no state preemption law that would otherwise prohibit local jurisdictions from enacting smokefree regulations more stringent than state law. As such, local Boards of HealthFootnote 3 have enacted county-level “Clean Indoor Air (CIA)” regulations across WV’s 55 counties under their authority to promote public health.Footnote 4 The first CIA regulation was passed in 1992, with 31 additional county CIA regulations following in the mid-1990s and all counties by 2007. Most early CIA regulations were limited in scope, providing smokefree areas in the workplace and/or restaurants. Over time, however, many of these limited regulations have been amended to provide greater smokefree coverage, with CIA regulations of varying degrees of restrictiveness scattered across the state. This patchwork effect and variation in timing of county regulations provides a unique context in which to assess the differential impacts of varying degrees of “restrictiveness” of county-level smokefree regulations.
This study addresses a significant gap in the literature. While there exists an important body of literature on the overall impact of state and national tobacco and smokefree policies, research on the effect of local smokefree policies is quite limited [29]. Additionally, research assessing the effect of local smokefree policy on birth outcomes is even more limited (see, e.g., Page et al. [35]). Finally, to our knowledge, there has been no direct evaluation of varying degrees of regulation restrictiveness (comprehensive versus partial ban) on birth outcomes and prenatal smoking.
Methods
Dataset
We selected the time period of 1995–2010 to capture a pre- and post-CIA timeframe for the majority of WV counties and to encompass the variation in restrictiveness of smokefree regulations provided by CIA changes across counties and over time. Our dataset was drawn from the WV Vital Statistics data representing all births to WV residents by county, providing data on birth outcomes with linked maternal characteristics. Our sample comprised singletons born to WV residents,Footnote 5 representing 293,715 births during the study period. Because our analysis involved only existing county-level datasets from public-use sources with no unique identifiers, this research was exempt from Institutional Review Board approval; all research activities were conducted in accordance with the ethical standards articulated in the 1964 Declaration of Helsinki.
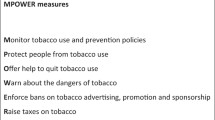
Four categories of smokefree regulations were established based upon three venues for smoking regulation: workplace, restaurant, and bar. Our categories were defined to reflect the greater time (with accompanying exposures) most adults spend in the workplace as compared to other venues, and restaurants more than bars: Comprehensive (ban in workplaces/restaurants/bars), Restrictive (ban in workplaces/restaurants, no restriction in bars), Moderate (ban in workplaces, partial restriction in restaurants, no restriction in bars), and Limited (partial restriction in workplaces, any restriction in restaurants, no restriction in bars). We categorized the 55 counties by smokefree regulation by month of policy implementation or modification (Table 1).Footnote 6 This table demonstrates the wide variation in smokefree regulations across time and restrictiveness, as well as the progression toward more restrictive regulations across time in most counties. Finally, we defined maternal groups for sub-group analysis by maternal age, marital status, and smoking status. Maternal age groups were based upon the minimum legal age for tobacco purchase and marriage without parental consent (18 years), as well as estimated age-related exposures in the three regulated venues (workplace,Footnote 7 restaurants, barsFootnote 8): <18 years, 18–20 years, 21+ years. Marital status and smoking status were categorized as binary variables (Yes/No).
Analysis
We analyzed the impact of the four categories of county smokefree regulations on six outcome variables: Birthweight–BW (log of birthweight, in grams); Gestational Age–GA (in number of days); Low Birthweight–LBW (birthweight <2500 g); Very Low Birthweight–VLBW (birthweight <1500 g); Preterm Birth–PTB (<37 weeks gestation); and, Prenatal Smoking–PS (self-reported smoking status at time of delivery). We introduced covariates drawn from the literature: maternal age, race, educational attainment, and marital status, as well as parity, month prenatal care began, and gestational weight gain (GWG). Also, because air pollution has been shown to impact birth outcomes, we included average annual county level of sulfur dioxide (log of parts per billion).Footnote 9 County fixed effects were introduced (to control for county-specific time-invariant characteristics) as were month fixed effects (to account for the seasonality of outcome variables). Finally, to avoid overestimating the effect of bans, we controlled for non-ban linear county-specific time trends (to account for county-specific trends in the outcome variables).Footnote 10
Several models were tested to avoid potential omitted-variable bias: we introduced secular trends by including the U.S. monthly mean birthweight and mean gestational age as covariates (to control for U.S. factors that might affect birth outcomes) as well as introduced state and federal tobacco tax rates as covariates (to account for any potential impact on tobacco use). The inclusion of these covariates did not change the findings, suggesting the findings are independent of these variables.
We used individual-level weighted least squares regression; however, using binary response models (Probit or Logit) for binary outcomes (LBW, VLBW, PTB, PS) yielded very similar estimates to the linear models. All statistical analyses were conducted using Stata statistical analysis software.
Results
Description of Sample
The sample (Table 2) had similar patterns to the U.S. prenatal population (during the same time period)Footnote 11 for maternal age, marital status, parity, and prenatal care initiation (though the sample had fewer with “No Prenatal Care”). The sample had relatively similar patterns of maternal education to the U.S. population, though the sample had a higher rate of High School only (40 vs. 32 %) and fewer with a College Degree (19 vs. 24 %). There were, however, stark differences in maternal race and smoking status. The sample was more racially homogenous (95 % White, 3 % Black) than the U.S. population (80 % White, 15 % Black). Finally, the sample had markedly higher prenatal smoking rates (26 %) than did the U.S. population (10 %).
Birth outcomes in the sample confirmed the known benefits conferred by specific maternal characteristics, with better outcomes for: 21+ years, married, non-smokers, higher education, adequate prenatal care, and/or GWG over 25 pounds. Mothers <21 years (particularly < 18), those with <HS, inadequate prenatal care (particularly No Prenatal Care), gained < 16 pounds GWG, high parity (5+), and/or smokers had among the worst birth outcomes—unsurprisingly, the same maternal groups with the highest smoking prevalenceFootnote 12 (as high as 50 % among mothers with <HS and those with No Prenatal Care).
Full Sample Analysis
Only Comprehensive and Restrictive smokefree regulations were associated with statistically significant favorable effects on birth outcomes in the full sample (Table 3). Comprehensive was associated with increased birthweight and gestational age, as well as reductions in VLBW and PTB. The only other favorable effect in the full sample was a very small decreased VLBW with Restrictive regulation. Neither less restrictive regulation had any statistically significant favorable effect on birth outcomes in the full sample. In fact, Moderate regulation was associated with an adverse effect (decrease) on birthweight in the full sample while Limited had no effect. None of the regulations had any effect on prenatal smoking in the full sample.
Sub-Group Analyses
The effects of all smokefree regulations varied by maternal age (Table 4), marital status (Table 5), and smoking status (Table 6). Comprehensive’s favorable effects extended to most maternal groups, particularly mothers 21+ years and non-smokers (BW, GA, VLBW, PTB) as well as unmarried mothers (BW, GA, PTB), but also married mothers (GA, PS) and smokers (GA), with its greatest magnitude of impact on unmarried mothers and smokers. Comprehensive was associated with increased BW and decreased PTB among 21+ years, unmarried, and non-smokers, with increased GA among all maternal groups other than mothers <21 years, and with decreasedVLBW among 21+ years and non-smokers. Comprehensive was, however, associated with an adverse effect (increase) on VLBW among <18 years—one of two maternal groups that experienced only adverse effects (the other being 18–20 years). Finally, Comprehensive was the only regulation associated with a change in PS in any group, a small decline among married mothers.
Less restrictive regulations demonstrated a more complex picture. Restrictive had a mixed effect: a small reduction in VLBW among 21+ years, but an adverse effect (decrease) on BW among <18 years. Moderate had only adverse effects on birth outcomes, including a decrease in BW among most maternal groups (18–20 years, 21+ years, married, smokers, non-smokers). Moderate also increased VLBW in both maternal age groups <21 years. Additionally, Moderate was the only regulation with any effect on LBW, an increase among smokers. The final regulation, Limited, had mixed effects: a very small reduction in VLBW among 21+ years, but a small increase among 18–20 years; and, an increase in BW among smokers, but a decrease among non-smokers.
Discussion
West Virginia has among the highest prenatal smoking prevalence in the United States at 26 % as compared to 11 % in the US population during the study period (1995–2010). Notably, smoking prevalence in West Virginia exceeds 40 % among mothers with low education, late/no prenatal care, and/or unmarried in contrast to 19 % in the US population. Of the state’s four county-level smokefree regulations, Limited was the only regulation adopted before 1999 and was the first regulation for 37 counties, with 30 progressing to more restrictive regulations. Seven counties began with Moderate, five remained unchanged, and six other counties used as an interim regulatory step. Ten counties began with Restrictive, nine remained unchanged, and 14 other counties transitioned from less restrictive regulations to Restrictive. Only one county began with Comprehensive, but 19 counties ultimately transitioned to this most restrictive regulation.
All policies have the potential to achieve their desired effect, but also have the potential for unintended consequences that are ineffective, undesirable, or perverse (i.e., contrary to the desired effect) [37]. That risk for perverse or adverse effect is, therefore, a risk for smokefree regulations—a risk that was realized among our findings. Our analyses indicate that only more comprehensive smokefree regulations—Comprehensive and Restrictive—were associated with statistically significant favorable effects on birth outcomes in the full sample, but all regulations varied in impact by maternal sub-group. Comprehensive had the most consistently favorable effects across maternal groups, with improvements extending to nearly all outcome variables and to most maternal groups. Restrictive was associated with a single improvement in one maternal group. Both regulations were associated with an isolated adverse effect on <18 years. Moderate was the only other regulation associated with a statistically significant effect in the full sample—an adverse effect on BW that extended to all maternal groups except <18 years and unmarried mothers. In fact, Moderate was the only regulation associated with only adverse effects on birth outcomes. Limited regulation had no effect on the full sample, but offered a mixed set of findings among maternal groups—opposite effects on groups within one maternal characteristic.
All maternal groups, other than those <21 years, experienced at least one improvement with at least one regulation; unmarried mothers were the only group to experience only improvements, while mothers <21 years (<18, 18–20) were the only groups to experience only adverse effects. The broadest set of improvements extended to mothers 21+ years, non-smokers, and unmarried mothers, though married mothers and smokers experienced some benefits as well. The greatest magnitude of impact occurred among unmarried mothers and smokers—two maternal groups with among the worst birth outcomes. Only married women experienced a change in prenatal smoking, though without improvement in birth outcomes beyond increased GA (experienced by most maternal groups).
Outcomes related to gestation had the most consistent improvements (GA more than PTB), and were never adversely affected. Outcomes related to birthweight (BW, LBW, VLBW), however, were mixed—with improvements and adverse effects noted in various maternal groups (though LBW had a single adverse effect among smokers). Prenatal smoking (PS) showed very limited effect, with a small decrease in married women with Comprehensive. These findings appear consistent with the existing literature evaluating comprehensive smokefree regulations: nearly universal improvement in gestation-related outcomes and mixed effects on birthweight-related outcomes. The general lack of effect on PS may also be consistent with the literature: at least one study’s findings suggested the decrease in PS following smokefree regulation may have been transient [31]. No previous evaluation has included an extended timeframe; the length of timeframe provided in our study assesses the overall long-term effect on PS rather than any short-term, transient impact. Also, the adverse effects on birthweight noted with Moderate may be consistent with the paradoxical birthweight findings of two evaluations of workplace smokefree regulations. Overall, the gradient effect in birth outcome improvements among the regulations in the general absence of any change in PS, suggests that more restrictive regulations improve birth outcomes through greater reductions in SHS exposure.
The variation in effects among maternal groups with all regulations—without corresponding changes in PS—suggests there exist variations in exposure to SHS given maternal socio-demographic factors.Footnote 13 Maternal age and marital status can contribute to differential exposure to SHS in the three regulated venues (workplace, restaurants, bars) as well as in the home (an unregulated environment). This study is limited, however, by the inability to directly measure SHS exposure; a discussion follows of surrogate measures for SHS exposures in these venues.
Workplace: Employment data (Footnote 8) suggest that smokefree workplace regulations (Comprehensive, Restrictive, Moderate) would have the greatest impact on mothers 21+ years, particularly those 24+ years. Our findings were generally consistent with this—far more favorable effects on birth outcomes for 21+ years with Comprehensive and Restrictive than for either maternal group <21 years. There was also a very small improvement in VLBW among 21+ years with Limited not seen in younger maternal groups; given this regulation’s partial smokefree workplace, this could support a gradient effect for regulation impact based upon degree of workplace protection. Notably, Moderate—like Comprehensive and Restrictive—provides a smokefree workplace (but only the workplace) with no favorable effects found.
Restaurant: Patterns of restaurant patronage show a strong interplay between age, income, and macroeconomic conditions. U.S. data indicate that restaurant dining is highest among younger age groups steadily declining with age, suggesting smokefree restaurant environments would impact younger mothers more [39]. Eating out, however, has declined among younger Americans (18–34 year olds) since 2007 as U.S. economic conditions have changed [21]. Without WV data, it is difficult to interpret how these U.S. trends have impacted WV’s prenatal population over the study period or the effect on variations in SHS exposure in restaurants.
Bar: The WV legal age for purchasing alcohol has been 21 years since 1986, but individual private clubs and bars may choose to allow entrance to individuals 18 + years (Footnote 9). Bar patronage, therefore, is likely highest among 21+ years, then 18–20 years, and nonexistent among <18 years; smokefree bars would have a greater effect on 21+ years, then 18–20 years, but none on <18 years. Our findings are consistent with this: Comprehensive was associated with improvements in birth outcomes among 21+ years, but adverse effects on <18 years and none on 18–20 years. Both Restricted and Limited, however, had the same pattern of findings despite no regulation of bars.
Home: Following implementation of smokefree regulation, smoking patterns could change among other inhabitants of the mother’s home: SHS could increase (given potential “displacement” of smoking from public places (work) to private spaces (home)), could decrease (given reduced prevalence, frequency, or quantity of smoking), or could remain unchanged. Our findings could suggest a role of “displacement:” Unmarried women realized far greater improvements in birth outcomes than did married women (despite their small decrease in prenatal smoking), and mothers 21+ years realized far greater improvements than did mothers <21 years (who experienced only adverse effects). Married mothers would nearly universally have another inhabitant in their home, and younger mothers (<18 years and to a lesser extent 18–20 years) are less likely to be financially self-sufficient and, therefore, more likely to live with others. Additionally, because both teen pregnancy and smoking prevalence are higher among lower socioeconomic status individuals, younger mothers may have a higher risk of SHS at home. Without data on SHS exposure in the home, however, it is difficult to fully understand the pattern of improvements in birth outcomes.
Limitations
Despite the strength of our findings, there are limitations in our study. First, our prenatal smoking variableFootnote 14 is a “Yes/No” binary variable, and does not measure the quantity, frequency, or duration of active smoking. The data, therefore, would not capture any changes in smoking status or smoking intensity during the pregnancy.Footnote 15 Next, importantly, we cannot measure SHS exposure in the regulated venues or in private spaces. Future research projects that include SHS exposure could further elaborate on the relationship between smokefree regulations and birth outcomes. Finally, this study does not include measures of policy implementation, enforcement, or penalties, which are all potentially influential in policy compliance. Including measures of implementation effectiveness [19] and consequences of policy non-compliance can expand our understanding of the impact of smoking restrictions.
Conclusions
The degree of regulation restrictiveness was a determining factor in the impact of smokefree regulations on birth outcomes. Only more comprehensive smokefree regulations (Comprehensive and Restrictive) were associated with favorable effects on birth outcomes in the full sample, while the less restrictive Moderate (workplace) regulation was associated with an adverse effect and the least restrictive regulation, Limited, had no impact. All four regulations varied in impact by maternal group (age, marital status, smoking status). Comprehensive had the most consistently favorable effects across maternal groups, with improvements extending to nearly all outcome variables and to nearly all maternal groups (except mothers <21 years). Consistent with the current literature, gestation-related outcomes demonstrated more consistent improvements, while birthweight-related outcomes had mixed effects. The broadest set of improvements extended to mothers 21+ years, non-smokers, and unmarried mothers, though married mothers and smokers experienced some benefits. Mothers <21 years experienced only adverse effects on birth outcomes with multiple regulations. The greatest magnitude of impact occurred among unmarried mothers and smokers—maternal groups with among the worst underlying birth outcomes. There was no change in prenatal smoking other than a small decrease among married mothers with Comprehensive.
This study suggests comprehensive smokefree regulations (ban in workplaces/restaurants/bars)—but not less restrictive smokefree regulations (complete or partial ban in workplaces only)—show promise in improving birth outcomes. The pattern of findings in the absence of PS changes suggests the impact of smokefree regulations on birth outcomes stems from decreased SHS exposure rather than lower smoking prevalence, with comprehensive regulations improving birth outcomes through greater reductions in SHS. Additionally, our findings may be consistent with “displacement” of smoking from public places to private spaces following regulation, with less benefit accruing to younger mothers and married women (all of whom are more likely to live with others). Future research would benefit from the inclusion of measures of SHS exposures; measures of smoking quantity, frequency, and duration; and variables assessing policy implementation and enforcement.
Notes
Defined here as no state-level smoking restriction in any of the following three venues: private workplaces, restaurants, or bars. These states include: Alabama, Kentucky, Mississippi, South Carolina, Texas, West Virginia, and Wyoming.
While the majority of local Boards of Health govern a single county, several Boards of Heath govern combined municipal-county units with a very few Boards of Health governing multiple counties.
These actions have been upheld by the West Virginia Supreme Court (Foundation for Independent Living, Inc. v. Cabell-Huntington Board of Health. (2003). 214 W.Va. 818, 519 S.E.2d. 744).
This includes both in-state and out-of-state births to WV residents. WV borders five states (Ohio, Pennsylvania, Maryland, Virginia, and Kentucky) making out-of-state births more routine than in most states.
Information on smoking regulations was obtained through an online search of each county’s regulations, and supplemented with historic data provided by the Smoke-Free Initiative of WV, a division of the West Virginia Department of Health and Human Resources.
West Virginia employment rates for females, 16–54 years (2002): 16–19 years = 33 %, 20–24 years = 54.5 %, 25–34 years = 67.3 %, 35–44 years = 68.1 %, 45–54 years = 63.9 %. U.S. Department of Labor, Bureau of Labor Statistics (--). Employment Status of the Civilian Noninstitutionalized Population by Sex, Race, Hispanic Origin, and Detailed Age, 2002 Annual Averages. http://www.bls.gov/lau/Table12full02.pdf. Additionally, high school enrollment is estimated at 86 % for 15–18 year-olds (96 % in 9th grade declining each year to 79 % in 12th grade; graduation rate is 74 %); while post-secondary enrollment is estimated at 44 % the Fall after high-school graduation, with a 75 % first-year persistence rate and a 16 % graduation rate within 6 years. Estimated from data available from Southern Regional Education Board (http://www.sreb.org) and National Center for Education Statistics (http://nces.ed.gov).
The legal age for purchasing alcohol in West Virginia has been 21 years since 1986; private clubs/bars, however, may choose to allow entrance to individuals 18 years of age and older. Alcohol Beverage Control Commissioner, Series 2–Private Club Licensing (§175-2-4.12).
Data obtained from the U.S. Environmental Protection Agency: http://www.epa.gov/airquality/airdata. Data on other pollutants are not available.
U.S. comparison data were obtained from the Centers for Disease Control and Prevention (CDC) “Natality Files” and “Linked Birth/Infant Death System” on CDC WONDER. http://wonder.cdc.gov. Note, however, these datasets did not provide information on Live Birth Order prior to 2003. Additionally, birth certificates (from which the CDC data were derived) changed tobacco use questions in 2003, complicating comparisons of data prior to versus after 2003.
Note the smoking prevalence of 32 % among mothers <18 years, despite the legal age of 18 for purchasing tobacco in West Virginia.
There could also exist variations in biological response to SHS based upon maternal characteristics, but a survey of the existing literature did not support this.
Note, smoking prevalence data is based upon self-reported smoking status among women at time of delivery. While self-reports carry the risk of inaccuracies, there is no indication that these errors would be systematic across time or place.
Some research suggests that a decrease in quantity of cigarettes smoked follows implementation of a smokefree regulation, even when the prevalence of smoking does not decrease [31]. Smokefree regulations could, therefore, potentially reduce prenatal smoking quantity without any apparent change in smoking prevalence. Our data, however, would not capture any change in quantity, frequency, or duration of prenatal smoking.
References
Adda, J. & Cornaglia, F. (2005). Taxes, cigarette consumption, and smoking intensity. IZA Discussion Paper No. 1849. Retrieved from http://papers.ssrn.com/sol3/papers.cfm?abstract_id=859005. Accessed 28 Mar 2013.
Adda, J., & Cornaglia, F. (2010). The effect of bans and taxes on passive smoking. Applied Economics: Journal of Applied Economics, 2, 1–32.
Amaral, M. (2009). The effect of local smoking ordinances on fetal development: evidence from California. Retrieved from http://www.pacific.edu/Documents/school-college/economics/smokingban_paper_Amaral.pdf. Accessed 21 Oct 2012.
American Lung Association (ALA). (2012). State of Tobacco Control. Retrieved from http://www.stateoftobaccocontrol.org/state-grades. Accessed 27 Nov 2012.
Barreca, A. I. (2010). The long-term economic impact of in utero and postnatal exposure to malaria. Journal of Human Resources, 45, 865–892.
Bartecchi, C., Alsever, R. N., Nevin-Woods, C., Thomas, W. M., Estacio, R. O., Bartelson, B. B., & Krantz, M. J. (2006). Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation, 114, 1490–1496.
Bernstein, I. M., Mongeon, J. A., Badger, G. J., Solomon, L., Heil, S. H., & Higgins, S. T. (2005). Maternal smoking and its association with birth weight. Obstetrics and Gynecology, 106, 986–991.
Bharadwaj, P., Johnsen, J. V., & Loken, K. V. (2012). Smoking bans, maternal smoking and birth outcomes. IZA Discussion Paper No. 7006 (Nov 2012). Retrieved from http://ftp.iza.org/dp7006.pdf. Accessed 27 Nov 2012.
Briggs, R. J. & Green T. (2012). The impact of workplace smoking bans on infant health: is less more? In review at Journal of Public Economics. Retrieved from http://www.eme.psu.edu/faculty/briggs_workplacesmokingbans.pdf. Accessed 28 Sept 2012.
Carpenter, C., Postolek, S., & Warman, C. (2011). Public-place smoking laws and exposure to environmental tobacco smoke (ETS). American Economics Journal, 3, 35–61.
Centers for Disease Control and Prevention (CDC). (2011). Behavioral Risk Factor Surveillance System: Prevalence and Trends Data. Retrieved from http://apps.nccd.cdc.gov/brfss/. Accessed 29 Nov 2012.
Chaloupka, F. (1992). Clean indoor air laws, addiction and cigarette smoking. Applied Economics, 24, 193–205.
Cox, B., Martens, E., Nemery, B., Vangronsveld, J., & Nawrot, T. S. (2013). Impact of a stepwise introduction of smokefree legislation on the rate of preterm birth: Analysis of routinely collected data. BMJ, 346, f441. doi:10.1136/bmj.f441.
Dejmek, J., Solansky, I., Podrazilova, K., & Sram, R. J. (2002). The exposure of nonsmoking and smoking mothers to environmental tobacco smoke during different gestational phases and fetal growth. Environmental Health Perspectives, 110, 601–606.
England, L. J., Kendrick, J. S., Gargiullo, P. M., Zahniser, S. C., & Hannon, W. H. (2001). Measures of maternal tobacco exposure and infant birth weight at term. American Journal of Epidemiology, 153, 954–960.
Erazo, M., Iglesias, V., Droppelmann, A., Acuna, M., Peruga, A., Breysse, P. N., & Navas-Acien, A. (2010). Secondhand tobacco smoke in bars and restaurants in Santiago, Chile: Evaluation of partial smoking ban legislation in public places. Tobacco Control, 19, 469–474.
Evans, W. N., Farrelly, M. C., & Montgomery, E. (1999). Do workplace smoking bans reduce smoking? American Economic Review, 89, 728–747.
Fernandez, E., Fu, M., Pacual, J. A., Lopez, M. J., Perez-Rios, M., Schiaffino, A., et al. (2009). Impact of the Spanish smoking law on second-hand smoke and respiratory health in hospitality workers: A cohort study. PLoS ONE, 4, e4244. doi:10.1371/journal.pone.0004244.
Hahn, E. J. (2010). Smokefree legislation: A review of health and economic outcomes research. American Journal of Preventive Medicine, 39, S66–S76.
Horta, B. L., Victora, C. G., Menezes, A. M., Halpern, R., & Barros, F. C. (1997). Low birthweight, preterm birth and intrauterine growth retardation in relation to maternal smoking. Paediatric and Perinatal Epidemiology, 11, 140–151.
Horovitz, B. (4 Nov 2012). Millenials eating out less. USA Today. Retrieved from http://www.usatoday.com/story/money/business/2012/11/04/millennials-eating-habits-npd-group/1665923/. Accessed 10 Sept 2013.
Huss, A., Kooijman, C., Breuer, M., Bohler, P., Zund, T., Wenk, S., & Roosli, M. (2010). Fine particulate matter measurements in Swiss restaurants, cafes and bars: What is the effect of spatial separation between smoking and non-smoking areas? Indoor Air, 20, 52–60.
Institute of Medicine (IOM). (2009). Secondhand smoke exposure and cardiovascular effects: Making sense of the evidence. Washington, D.C.: National Academy of Sciences.
Jaddoe, V. W., Troe, E. J. W., Hofman, A., Mackenbach, J. P., Moll, H. A., Steegers, E. A., & Witteman, J. C. (2008). Active and passive maternal smoking during pregnancy and the risks of low birthweight and preterm birth: The generation R study. Paediatric and Perinatal Epidemiology, 22, 162–171.
Kabir, Z., Clarke, V., Conroy, R., McNamee, E., Daly, S., & Clancy, L. (2009). Low birthweight and preterm birth rates 1 year before and after the Irish workplace smoking ban. British Journal of Obstetrics and Gynaecology, 116, 1782–1787.
Kabir, Z., Daly, S., Clarke, V., Keogan, S., & Clancy, L. (2013). Smoking bans and small-for-gestational age births in Ireland. PLoS ONE, 8, e57441. doi:10.1371/journal.pone.0057441.
Khuder, S. A., Milz, S., Jordan, T., Price, J., Silvestri, K., & Butler, P. (2007). The impact of a smoking ban on hospital admissions for coronary heart disease. Preventive Medicine, 45, 3–8.
Kramer, M. S. (1987). Determinants of low birth weight: Methodological assessment and meta-analysis. Bulletin of the World Health Organization, 65, 663–737.
Lipperman-Kreda, S., Friend, K. B., & Grube, J. W. (2014). Rating the effectivenss of local tobacco policies for reducing youth smoking. The Journal of Primary Prevention, 35, 85–91.
Mackay, D., Haw, S., Ayres, J. G., Fischbacher, C., & Pell, J. P. (2010). Smoke-free legislation and hospitalizations for childhood asthma. New England Journal of Medicine, 363, 1139–1145.
Mackay, D. F., Nelson, S. M., Haw, S. J., & Pell, J. P. (2012). Impact of Scotland’s smoke-free legislation on pregnancy complications: Retrospective cohort study. PLoS Med, 9, e1001175. doi:10.1371/journal.pmed.1001175.
Markowitz, S., Adams, E. K., Dietz, P. M., Kanna, V., & Tong, V. (2011). Smoking policies and birth outcomes: estimates from a new era. NBER Working Paper No. 17160 (Jun 2011). Retrieved from http://www.nber.org/papers/w17160. Accessed 28 Sept 2012.
Martin, T. R., & Brachen, M. B. (1986). Association of low birth weight with passive smoke exposure in pregnancy. American Journal of Epidemiology, 124, 633–642.
Ohsfeldt, R. L., Boyle, R. G., Capilouto, E. I. (1998). Tobacco taxes, smoking restrictions, and tobacco use. NBER Working Paper No. 6486 (Mar 1998). Retrieved from http://www.nber.org/papers/w6486. Accessed 28 Mar 2013.
Page, R. L., Slejko, J. F., & Libby, A. M. (2012). A citywide smoking ban reduced maternal smoking and risk for preterm births: A colorado natural experiment. Journal of Women’s Health, 21, 621–627.
Raphael, S., & Winter-Ebmer, R. (2001). Identifying the effect of unemployment on crime. The Journal of Law and Economics, 1, 259–284.
Sunstein, C. R. (1994). Political equality and unintended consequences. Columbia Law Review, 94, 1390–1414.
Tan, C. E., & Glantz, S. A. (2012). Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: A meta-analysis. Circulation, 126, 2177–2183.
Taylor, P., Funk, C., & Craighill, P. (2006). Eating More; Enjoying Less. Retrieved from http://pewsocialtrends.org/files/2010/10/Eating.pdf. Accessed 10 Sept 2013.
Tong, V. T., Dietz, P. M., Morrow, B., D’Angelo, D. V., Farr, S. L., Rockhill, K. M., & England, L. J. (2013). Trends in smoking before, during, and after pregnancy—Pregnancy risk assessment monitoring system, United States, 40 sites, 2000–2010. MMWR Surveillance Summaries, 62(SS06), 1–19.
U.S. Department of Health & Human Services (DHHS), Office of the Surgeon General. (2001). Women and smoking: A report of the surgeon general. Rockville, MD: DHHS.
U.S. Department of Health & Human Services (DHHS), Office of the Surgeon General. (2006). The health consequences of involuntary exposure to tobacco smoke: A report of the surgeon general. Rockville, MD: DHHS.
Ward, M., Currie, L. M., Kabir, Z., & Clancy, L. (2013). The efficacy of different models of smoke-free laws in reducing exposure to second-hand smoke: A multi-country comparison. Health Policy, 110, 207–213.
Wasserman, J., Manning, W. G., Newhouse, J. P., & Winkler, J. D. (1991). The effects of excise taxes and regulations on cigarette smoking. Journal of Health Economics, 10, 43–64.
Wolfers, J. (2006). Did unilateral divorce laws raise divorce rates? A reconciliation and new results. The American Economic Review, 96, 1802–1820.
Acknowledgments
The authors wish to extend our great appreciation to Mr. Tom Light of the WV Department of Health and Human Resources Health Statistics Center for his assistance with the dataset, and to Ms. Christina Mickey of Smoke-Free Initiative of WV for information provided on historical smokefree regulations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bartholomew, K.S., Abouk, R. The Effect of Local Smokefree Regulations on Birth Outcomes and Prenatal Smoking. Matern Child Health J 20, 1526–1538 (2016). https://doi.org/10.1007/s10995-016-1952-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-1952-x