Abstract
Introduction Physical inactivity is prevalent in pregnant women, and innovative strategies to promote physical activity are strongly needed. The purpose of the study was to test a 12-week mobile health (mHealth) physical activity intervention for feasibility and potential efficacy. Methods Participants were recruited between December 2012 and February 2014 using diverse recruitment methods. Thirty pregnant women between 10 and 20 weeks of gestation were randomized to an intervention (mobile phone app plus Fitbit) or a control (Fitbit) group. Both conditions targeted gradual increases in physical activity. The mHealth intervention included daily messages and a mobile phone activity diary with automated feedback and self-monitoring systems. Results On monthly average, 4 women were screened for initial eligibility by telephone and 2.5 were randomized. Intervention participants had a 1096 ± 1898 step increase in daily steps compared to an increase of 259 ± 1604 steps in control participants at 12 weeks. The change between groups in weekly mean steps per day during the 12-week study period was not statistically significant (p = 0.38). The intervention group reported lower perceived barrier to being active, lack of energy, than the control group at 12-week visit (p = 0.02). The rates of responding to daily messages and using the daily diary through the mobile app declined during the 12 week study period. Discussion It was difficult to recruit and randomize inactive women who wanted to increase physical activity during pregnancy. Pregnant women who were motivated to increase physical activity might find using mobile technologies in assessing and promoting PA acceptable. Possible reasons for the non-significant treatment effect of the mHealth intervention on physical activity are discussed. Public awareness of safety and benefits of physical activity during pregnancy should be promoted. Clinicaltrials.Gov Identifier NCT01461707.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Despite numerous benefits of physical activity during pregnancy, physical inactivity is prevalent among pregnant women. Only a few interventions have shown positive results for physical activity during pregnancy.
What this study adds? Pregnant women who decided to increase their physical activity levels found using mobile technologies in receiving the physical activity program acceptable. However, it was hard to reach physically inactive women who were motivated to increase physical activity during pregnancy from the community. This small study of the mHealth physical activity intervention did not detect a statistically significant effect on physical activity, but did suggest its potential in lowering perceived barriers to being active.
Introduction
Physical inactivity is a major risk factor for non-communicable diseases including cardiovascular diseases and type 2 diabetes. However, nearly 58 % do not achieving the recommended amount of activity to be considered physically active (2.5 h/week) [1]. According to the 2000 Behavioral Risk Factor Surveillance System, the prevalence of those who participating in the recommended amount of activity was much lower among pregnant women than non-pregnant women (15.8 vs. 26.1 %) [2]. Despite the health benefits including possible prevention of gestational diabetes, support of healthy gestational weight gain, and improved mental health, apparent shifts from recommended activity to insufficient activity or inactivity are noted for pregnant women [3–5].
In the past decade, behavioral interventions designed to improve physical activity (PA) among pregnant women have increased [6]. In a recent systematic review of randomized controlled trials that measured the efficacy of a PA intervention targeted at pregnant women, only three out of nine interventions reported statistically and clinically significant results for increasing physical activity. However, no unique strategies or techniques consistently associated with positive outcomes were identified from the review [7]. Thus, randomized controlled trials to test effective PA promotion intervention strategies for pregnant women are urgently needed.
Strategies using mobile health (mHealth) capabilities to deliver intervention became popular due to their potential for effectiveness and scalability, but it is too early to assure its effectiveness in promoting PA in pregnant women. Although pregnancy is viewed as “teachable moment” for pregnant women to adopt health-promoting behaviors, they are still a hard-to-reach population for research due to the nature of pregnancy—the challenging, transitional period of life. Given that there is widespread use of mobile phones in women of childbearing age, use of mobile application as a tool to give prompts, provide self-monitoring, and give feedback has potential to be used widely to increase physical activity. Thus, the primary goal of this pilot study was to examine the feasibility of subject recruitment, randomization, and intervention and the potential efficacy of a 12-week mHealth PA program, the MoTHER (Mobile Technologies to Help Enhance Regular Physical Activity) trial in physically inactive pregnant women. It was not designed to have sufficient power to test for between-group differences.
Methods
Study Design and Sample
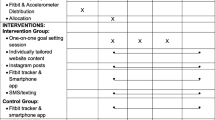
This was a pilot, 12-week randomized controlled trial (RCT) with two groups; (1) Intervention (mobile phone application developed by a research team and Fitbit Ultra [8] (accelerometer) based PA intervention) and (2) Control (Fitbit Ultra only). The study protocol was approved by the University of California, San Francisco (UCSF) Institutional Review Board prior to participant enrollment. Participants were recruited from the prenatal clinics and communities in the San Francisco Bay area. Inclusion criteria were (1) 18–40 years of age; (2) pregnant, 10–20 weeks of gestation; (3) sedentary lifestyle; (4) intent to be physically active; (5) access to a home telephone or a mobile phone; (6) access to a computer; and (7) ability to communicate in English. Exclusion criteria were (1) known medical or obstetric complication that restricts physical activity and (2) current participation in lifestyle modification programs that may potentially confound results of this study.
Screening/Baseline (S/B) Visit and Run-in Period
After obtaining a written informed consent, participants’ sociodemographic characteristics and health literacy were assessed [9]. Body weight and height was measured without shoes. Eligible participants received instructions for the 1–2 week run-in period along with run-in versions of the mobile phone application (app) and Fitbit Ultra (Fitbit). Women were instructed to download a Fitbit installation program onto a computer at home, and asked to wear the Fitbit at least 10 h daily, except when showering, bathing, and swimming. Fitbit was preprogrammed not to show any PA data. Women were also asked to use app, either on their own phones or phones borrowed from the research team. The run-in data were used to calculate average daily steps, used as a baseline in the analysis, and for individual goal setting. The run-in app was designed to mimic the trial app, but without any content to promote PA. Each night (between 7 pm and midnight), women were asked to guess how many steps they took for a day. In addition, the daily messages included questions that were not relevant to PA such as “did you have your breakfast?” Thus, participants neither tracked nor downloaded their activity during the run-in period.
Randomization and Blinding
Randomization was computer-generated and stratified by body mass index category based on self-reported pre-pregnancy weight and height: normal and overweight/obese. Allocation was concealed in opaque envelopes. Due to the nature of the intervention, blinding of participants and research staff was not possible.
Intervention
Initial Brief In-Person Session
During a 30-min in-person session, participants were informed of the American College of Obstetricians and Gynecologists’ guideline, which recommends at least 30 min of moderate-level PA a day on most days of the week [10]. Consistent with Social Cognitive Theory [11], the topics covered include short and long-term goal setting, problem-solving skills, techniques for developing and maintaining social support for PA, and a plan for lapses in the process of increasing PA. Women were asked to increase their steps by 10 % each week until they reached at least 8500 steps/day 5 days or more per week [12]. We encouraged participants to exercise on their own at home using brisk walking as their primary form of PA. Information was also provided on healthy diets with fewer high-fat foods and healthier alternatives. Women were informed of the IOM recommendations for gestational weight gain [13] and asked to weigh themselves twice a week before breakfast. In addition, a safety instruction about increasing PA during pregnancy was given.
Trial App with Fitbit
In contrast to the run-in version, the trial version of the Fitbit displayed steps, distance, flights of stairs climbed, and estimated calories expended. In the trial app, a daily message, either as a text message or short video script, was available between 10 am and 7 pm, and the activity diary was available after 7 pm to midnight everyday. Daily messages were prompts to support PA or to reinforce the topics of the initial in-person session. For example, when a woman responded “no” to the daily message, “you and your baby deserve good health. Can you make time for a 30-min brisk walk this afternoon?” a feedback message such as “try just a 15-min walk to see how you feel.” was shown on the app. Women were also asked to enter their daily steps assessed by Fitbit and report the type and duration of PA that they engaged in on that day into the activity dairy. Feedback was given on their progress in steps according to their prescheduled weekly step goal and a weekly graph of daily steps was available. The tips for PA, healthy diet, and weight management during pregnancy, as well as images and short video clips regarding posture and stretching, were available on the summary menu of the app.
Control Group (Fitbit Only Group)
The control group also used the trial version of Fitbit, as described above. During the initial brief in-person session, the control group received only the IOM recommendations for gestational weight gain and safety instruction for promoting PA during pregnancy. Women were asked to increase their steps gradually until they reach at least 8500 steps/day 5 days or more per week. However, problem-solving skills, techniques for developing and maintaining social support for PA, and a plan for lapses were not discussed. Women in the control group were not given access to the trial app or to any intervention components available on the summary menu of the app.
Measures
The Stanford Brief Physical Activity Survey was used to screen those who are inactive [14] and Physical Activity Stages of Change was used to screen those who are considering being physically active in the future or the near future [15]. The primary outcome was weekly mean steps per day for the prior week, as measured by Fitbit. Daily steps <1000 counts were treated as invalid, possibly due to Fitbit not being worn at all times, and excluded from data analysis. The minimum of 1000 counts was selected based on previous studies using pedometers [16, 17].
Other study measures include the Self-Efficacy for Physical Activity [18], the Social Support and Exercise Survey [19], the Barriers to Being Active Quiz [20], and the Center for Epidemiological Studies Depression Scale [21]. Physical and emotional pregnancy symptoms were assessed with the Pregnancy Discomfort Checklist [22]. The original instrument assesses the frequency of 29 symptoms occurring during pregnancy. We modified the instrument by assessing severity and distressfulness of symptoms in addition to frequency and by adding three symptoms related to sleep disturbance and restless legs syndrome.
Body weight and height was measured with the Healthometer Professional Floor Scale and the Healthometer PORTROD Height Rod at the S/B and 12-week visits. Adherence of the MoTHER trial app usage was assessed by the number of responses to the daily messages and activity diary during the 12-week study period in the intervention participants. Possible adverse events were assessed at the 12-week visit.
Data Management
The questionnaire data were managed using REDCap (Research Electronic Data Capture), a secure web-based application for research studies, hosted at the UCSF [23]. Email accounts were created for each Fitbit. Fitbit data were remotely monitored and extracted through Fitabase, a tool to mirror the data obtained from the Fitbit Application Programming Interface (API). The app data, which did not include any personal identifier information, were also transmitted in real-time directly from mobile phones to the secure server.
Statistical Analysis
To estimate the yield of the various recruitment methods, characterized by how people heard about the study, we calculated the number of people who completed telephone screenings, the number meeting the eligibility criteria, the number completed the S/B visits, and the number randomized. The baseline characteristics of the two groups were compared using t or Chi square tests. We examined the effect of the intervention versus control condition on study outcomes using ANCOVAs controlling for the baseline value of the outcome of interest. We also ran sensitivity analyses adjusting for baseline covariates that differed between groups at p < 0.05, and using the bootstrap for inference for non-normal outcomes. Analyses were conducted using an intent-to-treat approach, without regard to adherence to the intervention. Analyses were performed using SPSS 22 and STATA 13. A 2-sided level of significance of 0.05 was used.
Results
Feasibility of Recruitment and Randomization
Potential participants were recruited between December 2012 and February 2014 using diverse methods. First, we posted study flyers or placed study brochures in public as well as private places including university campuses, public libraries, obstetrician offices, outpatient clinics, health education centers, local Mothers of Preschoolers (MOPS) meetings, Women, Infants, and Children (WIC) offices, local preschools, community recreation facilities, community exercise gyms, and university shuttle buses. The study advertisement was also placed in 5 local subway stations for 4 weeks. Secondly, the study information was disseminated through online networks for families with young children and online community boards. The study advertisement was also listed in a local magazine for parents for a month. Thirdly, the study team gave out study brochures at a local exposition oriented to parents of babies and children, as well as prenatal group meetings (e.g., Black Infants Health Program, Centering Pregnancy Program). Last, some potential participants contacted the study team after an obstetrician’s referral or word of mouth from family, friends, or colleagues.
In Table 1, we present the number of people who completed a telephone screening, the number of people who were eligible for the study, the number completed the S/B visits, and the number randomized. One hundred ten telephone as well as email inquiries led to 57 telephone screenings, which was on average 4 per month, and 47 women who met the inclusion criteria were invited to visit S/B visits. Nearly 44 % of those who completed screening (25/57) heard about it through flyer/brochure in public and private locations. The proportion to reach those who meet the eligibility criteria was highest in obstetrician’s referral (6/6), followed by flyers/brochures (21/25), online/offline networks (14/17), and word of mouth (6/8). Figure 1 presents the flowchart of recruitment. Thirty-five out of 47 women made S/B visits and participated in run-ins. Of 35 women completed run-ins, 4 were determined to be ineligible: miscarriage (n = 1) and being too physically active (n = 3), and a woman decided to withdraw due to her work schedule. Thus, 30 women were randomly assigned in a 1:1 ratio to either intervention group or control group between February 2013 and February 2014, on average 2.5 per month.
Participant Characteristics
Table 2 shows baseline sample characteristics of participants randomized in the study. Mean (±SD) age of all the participants was 33.7 ± 2.6 years and 56 % were ethnic minorities. The intervention and control groups were generally similar. Control women were slightly older (p = 0.08), and more time elapsed between the S/B and 12-week visits among intervention participants (p < 0.001).
Changes in Objectively Measured Physical Activity Over 12 weeks
Twenty-nine women (96.7 %) completed the 12-week visit: 14 intervention and 15 control participants. Overall the intervention participants and control participants wore the Fitbit 78 % (5.5 days/week) and 80 % (5.7 days/week) of 12-week study period, respectively. Table 3 shows the baseline as well changes in weekly mean steps per day, as measured by Fitbit. There were no significant differences between groups in steps or self-reported physical activity at baseline (p = 0.77, p = 0.98, respectively). Both groups increased their steps from baseline to 1–4 weeks, by 1166.6 (SD ± 1709.4) for the intervention group and 1062.6 (SD ± 2325.5) for the control group. The increased steps were maintained for the intervention group, 1092.1(SD ± 1925.3) at 5–8 weeks and 1096.2 (SD ± 1898.1) at 9–12 weeks, but diminished for the control group, 804.3 (SD ± 1752.9) at 5–8 weeks and 258.7 (SD ± 1603.7) at 9–12 weeks. The group difference in changes of steps was not significant in this small sample (p = 0.23).
Changes in TV/Computer, Self-Efficacy, Barriers, Social Support, Depressive Symptoms, and Pregnancy Symptoms Over 12 weeks
Baseline values of study outcomes were generally similar during the run-in period (Table 4). However, intervention women had higher self-efficacy (p = 0.05) and were more likely to report lack of resources as a barrier to being active (p = 0.05) at the S/B visit.
Over the 12 weeks of follow-up, we found statistically significant evidence that the intervention reduces lack of energy as a barrier to exercise (p = 0.02). We also found weak evidence for reductions in barriers including lack of time (p = 0.08) and lack of willpower (p = 0.06), as well as decreased severity of pregnancy symptoms (p = 0.10). Results were unaffected in sensitivity analyses adjusting for between-group differences at baseline in self-efficacy and/or lack of resources, as well as analyses using the bootstrap for inference for non-normal outcomes.
Adherence to Trial App
As shown in Fig. 2, women showed 76 % (5 days/week) and 81 % (6 days/week) of the response rates for daily messages and activity diary, respectively, on the first week. On the second week, the response rates for daily messages and activity diary dropped to 60 and 67 % and maintained for the next few weeks.
Adverse Events
There were no serious adverse events (hospitalization or emergency visits) associated with the intervention.
Discussion
We conducted a pilot RCT to examine the feasibility and potential efficacy of a 12-week mHealth PA intervention in physically inactive pregnant women. Substantial outreach efforts were needed to recruit the sample of 30 women, but eligibility rates were high among those who were screened, retention through 12 weeks was excellent, and adherence to the mobile app was good. Although we did not find a statistically significant between-group difference in step in the increases in step counts, we did find some evidence for beneficial intervention effects on selected barriers to exercise as well as pregnancy symptoms.
This pilot study was not powered to detect an intervention effect on step counts. However, there are several difficulties faced by interventions promoting PA among pregnant women. First, a majority of these women are physically inactive, and even women who were physically active prior to their pregnancy are reported to reduce their activity as their pregnancy progresses [24]. Second, due to their physically inactive lifestyle prior to pregnancy, the goal for daily steps and the pace to achieve the goal were cautiously set, based on prior PA intervention studies in pregnant women. For this study, 8500 steps/day as a final goal and a weekly increase of 10 % from baseline steps were used, in contrast to the daily goal of 10,000–12,000 steps and 20 % used for other populations, including physically inactive women [25] and pre-diabetic populations [26]. In addition, the active control condition, including a wearable activity monitor and the same final goal steps as the intervention group, may itself have had substantial effects, although our results suggest that this effect may not be long-lasting.
Lack of energy is one of the major barriers to being active in pregnant women. In a survey study of 1535 pregnant women and 13 focus groups with a total of 58 pregnant women, lack of energy or tiredness was a main barrier to PA across all ethnic groups regardless of BMI [27]. In a retrospective study of 74 postpartum women, tiredness or fatigue was frequently reported as a barrier to exercise during pregnancy [28]. Improved overall mood and increased energy, however, were reported as major benefits of exercise during pregnancy in the study. That is, some women view lack of energy as a barrier to physical activity while others view PA as a way to relieve this symptom. After the 12-week study period, the intervention women reported significantly lower level of a barrier to PA, especially, lack of energy, than the control women. The perceived symptom experience of fatigue or tiredness in terms of frequency, severity, and distress, however, was not statistically different between the intervention and control groups (data not shown). That is, the way they perceive fatigue as barriers may be changed among the intervention women since they had a chance to review their barriers and specific strategies to overcome those barriers in a session with research staff. In addition, daily messages may play a role of positive reinforcement and reminder for the participants to be more aware of their barriers and strategies.
Although statistically insignificant in this small sample, the intervention participants reported lower level of barriers to PA including lack of time and lack of willpower and lower severity of pregnancy-related symptoms than the control participants over the 12-week study period. The intervention may provide women encouragement and support to initiate regular PA and this experience may influence their perspectives in time and willpower in doing PA. This positive experience may be necessary for them to maintain their newly adopted PA behavior. Physical limitations or restrictions were the most frequently reported barriers to exercise [27]. Women in the both groups experienced physical as well as emotional symptoms similarly in terms of frequency and distress. However, the severity of the symptom experience was improved in the intervention women. This may be mediated by the production of endorphins or by the diversion provided by increased PA [29]. Changes in barriers to PA and symptoms need to be further explored by frequent assessments using mobile technologies in future research.
Overall, using the mobile technologies in the PA program was acceptable to the women in our pilot study. The response rate of daily messages and the usage rate of activity diary in the intervention group were comparable with other studies using mobile technologies. For example, the short message service (SMS) response rates dropped from 78 % (at 2 weeks) to 24 % (at 10 weeks) in a PA intervention with postpartum women [30]. When goal check text messages were sent out once a week over the 12-week physical activity intervention, the text message response rates ranged from 86 % (at 2 weeks) and 64 % (at 10 weeks) in women with young children [31], Since the causal relationships between the adherence of mHealth programs and behavioral changes have not been fully supported, it is difficult to suggest what would be considered optimal use. However, declining response or usage rates may reflect the diminished treatment effect of the intervention. Therefore, strategies to increase adherence of the program need to be tested in future research.
Despite diverse and fairly intensive outreach, approximately 4 women per month were telephone screened and <3 women per month were randomized in this pilot study. This indicates that it is hard to reach physically inactive women who want to increase their physical activity levels during pregnancy. Given that a majority of pregnant women do not meet the recommended level of physical activity in this society, public awareness about safety and health benefits of physical activity during pregnancy needs to be promoted. Obstetrician’s referrals were the most effective method to reach women meeting the eligibility criteria for the study. Advice from health care providers that pregnant women should increase physical activity may be a strong motivator. Prenatal health care professionals should inform, educate, and communicate with pregnant women and their families about the benefits of physical activity. While the recruitment of physically inactive pregnant women was difficult in the pilot study, the retention rate was about 97 % (only one drop-out), indicating that women find interventions like ours acceptable, once they have decided to increase their physical activity levels.
Study findings should be interpreted with caution given the small sample size and the program’s focus on short-term behavior change. To increase the generalizability of the study findings, we recruited both smart phone and non-smart phone users and diverse racial/ethnic minorities to this pilot study. However, the sample of the study represents only English-speaking physically inactive women who were willing to use the mobile phone app and/or wear a Fitbit for 12 weeks. Thus, findings may not be generalizable to non-English speakers or women who are not motivated to use those technologies.
Conclusions
The mHealth PA intervention appeared to be feasible and acceptable, but this small pilot study was unable to show statistically significant effects on PA between the intervention and control groups. It appeared to reduce lack of energy, a perceived barrier to being physically active. It was hard to recruit inactive women who wanted to increase physical activity level during pregnancy, but pregnant women who were motivated to increase physical activity found using mobile technologies promoting PA acceptable. Public awareness of safety and benefits of physical activity during pregnancy should be promoted and the role of prenatal care professionals in this effort is greatly needed.
References
Physical Activity Guidelines Advisory Committee (2008). Physical Activity Guidelines Advisory Committee Report, 2008. Washington (DC): United States Department of Health and Human Services (USDHHS).
Evenson, K. R., Savitz, D. A., & Huston, S. L. (2004). Leisure-time physical activity among pregnancy women in the US. Paediatric and Perinatal Epidemiology, 18, 400–407.
ACOG. (2002). Exercise during pregnancy and the postpartum period. ACOG Committee Opinion No. 267. Obstetrics and Gynecology, 99, 171–173.
Davies, G., Wolfe, L., Mottola, M., et al. (2003). Joint SOGC/CSEP clinical practice guideline: Exercise in pregnancy and the postpartum period. Canadian Journal of Applied Physiology, 28, 330–341.
(2006). Impact of physical activity during pregnancy and postpartum on chronic disease risk. Medicine and Science in Sports and Exercise, 38 (5), 989–1006.
Mudd, L. M., Owe, K. M., Mottola, M. F., et al. (2013). Health benefits of physical activity during pregnancy: An international perspective. Medicine and Science in Sports and Exercise, 45(2), 268–277.
Pearce, E. E., Evenson, K. R., Downs, D. S., et al. (2013). Strategies to promote physical activity during pregnancy. American Journal of Lifestyle Medicine, 7(1), 38–50.
Noah, J. A., Spierer, D. K., Gu, J., Bronner, S., et al. (2013). Comparison of steps and energy expenditure assessment in adults of Fitbit Tracker and Ultra to the Actical and indirect calorimetry. Journal of Medical Engineering and Technology, 37, 456–462.
Weiss, B., Mays, M. Z., Martz, W., et al. (2005). Quick assessment of literacy in primary care: The newest vistal sign. The Annals of Family Medicine, 3(6), 514–522.
ACOG Committee Obstetric Practice. (2002). ACOG Committee opinion. Number 267, January 2002: Exercise during pregnancy and the postpartum period. Obstetrics and Gynecology, 99, 171–173.
Bandura, A., Adams, N. E., Hardy, A. B., et al. (1980). Tests of generality of self-efficacy theory. Cognitive Therapy and Research, 4, 39–66.
USDHHS. Stay Active and Be Fit! A guide to fitness and activity fundamentals. www.presidentschallenge.org/pdf/getfit.pdf.
Institute of Medicine. (2009). Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: National Academies Press.
Taylor-Piliae, R. E., Norton, L. C., Haskell, W. L., et al. (2006). Validation of a new brief physical activity survey among men and women aged 60–69 years. American Journal of Epidemiology, 164(6), 598–606.
Marcus, B. H., & Forsyth, L. (2009). Motivating people to be physically active (2nd ed.). IL: Human Kinetics, Urbana-Champaign.
Craig, C. L., Tudor-Locke, C., Cragg, S., et al. (2010). Process and treatment of pedometer data collection for youth: The Canadian physical activity levels among youth study. Medicine and Science in Sports and Exercise, 42(3), 430–435.
Mutrie, N., Doolin, O., Fitzsimons, C. F., et al. (2012). Increasing older adults’ walking through primary care: Results of a pilot randomized controlled trial. Family Practice, 29(6), 633–642. doi:10.1093/fampra/cms038.
Marcus, B. H., Selby, V. C., Niaura, R. S., et al. (1992). Self-efficacy and the stages of exercise behavior change. Research Quarterly for Exercise and Sport, 63(1), 60–66.
Sallis, J. F., Grossman, R. M., Pinski, R. B., et al. (1987). The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine, 16(6), 825–836.
Centers for Disease Control and Prevention (CDC). Barrier to being active. www.cdc.gov/nccdphp/dnpa/physical/life/barriers_quiz.pdf.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Wallace, A. M., Boyer, D. B., Dan, A., et al. (1986). Aerobic exercise, maternal self-esteem, and physical discomforts during pregnancy. Journal of Nurse Midwifery, 31(6), 255–262.
Harris, P. A., Taylor, R., Thielke, R., et al. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381.
Evenson, K. R., Savitz, D. A., & Huston, S. L. (2004). Leisure-time physical activity among pregnant women in the US. Paediatric and Perinatal Epidemiology, 18, 400–407.
Fukuoka, Y., Vittinghoff, E., Jong, S. S., et al. (2010). Innovation to motivation-Pilot study of a mobile phone intervention to increase physical activity among sedentary women. Preventive Medicine, 51, 287–289.
Fukuoka, Y., Gay, C. L., Joiner, K. L., et al. (2015). A novel diabetes prevention intervention using a mobile app: A randomized controlled trial with overweight adults at risk. American Journal of Preventive Medicine, 49(2), 223–237.
Evenson, K. R., Moos, M. K., Carrier, K., et al. (2008). Perceived barriers to physical activity among pregnant women. Maternal and Child Health Journal, 13(3), 364–375.
Symons-Downs, D., & Hausenblas, H. A. (2004). Women’s exercise beliefs and behaviors during their pregnancy and postpartum. Journal of Midwifery and Womens Health, 49(2), 138–144.
Fox, K. R. (1999). The influence of physical activity on mental well-being. Public Health Nutrition, 2(Supplement 3a), 411–418.
Fjeldsoe, B. S., Miller, Y. D., & Marshall, A. L. (2010). MobileMums: A randomized controlled trial of an SMS-based physical activity intervention. Annals of Behavioral Medicine, 39, 101–111.
Fjeldsoe, B. S., Miller, Y. D., & Graves, N. (2015). Randomized controlled trial of an improved version of MobileMums, an intervention for increasing physical activity in women with young children. Annals of Behavioral Medicine, 5(4), e007226. doi:10.1136/bmjopen-2014-007226.
Acknowledgments
This study was supported by the National Heart, Lung, Blood Institution (3R01HL104147-02S1) from the National Institutes of Health (NIH); the National Institutes of Health (NIH), through UCSF-CTSI Grant Number UL1 RR024131. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. We also thank Victoria Phan, BS, Joelle Takahashi, BA, Stephen Weinstein, MD, Joanne Vogel, MD, and the MoTHER Study participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, J., Lee, J.h., Vittinghoff, E. et al. mHealth Physical Activity Intervention: A Randomized Pilot Study in Physically Inactive Pregnant Women. Matern Child Health J 20, 1091–1101 (2016). https://doi.org/10.1007/s10995-015-1895-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1895-7