Abstract
Context
Ecological research, from organismal to global scales and spanning terrestrial, hydrologic, and atmospheric domains, can contribute more to reducing health vulnerabilities. At the same, ecological research directed to health vulnerabilities provides a problem-based unifying framework for urban ecologists.
Objective
Provide a framework for expanding ecological research to address human health vulnerabilities in cities.
Methods
I pose an urban ecology of human health framework that considers how the ecological contributions to health risks and benefits are driven by interacting influences of the environment, active management, and historical legacies in the context of ecological self-organization. The ecology of health framework is explored for contrasting examples including heat, vector borne diseases, pollution, and accessible greenspace both individually and in a multifunctional landscape perspective.
Results
Urban ecological processes affect human health vulnerability through contributions to multiple hazard and well-being pathways. The resulting multifunctional landscape of health vulnerability features prominent hotspots and regional injustices. A path forward to increase knowledge of the ecological contributions to health vulnerabilities includes increased participation in in interdisciplinary teams and applications of high resolution environmental sensing and modeling.
Conclusions
Research and management from a systems and landscape perspective of ecological processes is poised to help reduce urban health vulnerability and provide a better understanding of ecological dynamics in the Anthropocene.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Human health vulnerability and urban ecology
The migration of people from a rural to urban lifestyle is leading to extensive change in the drivers and systems of human health vulnerability. Within cities, the ecological contributions to urban health vulnerability depend on the coupling among biological communities, ecologically mediated material and energy exchanges, diverse social networks, and highly engineered technological features (Townsend et al. 2003; Jenerette et al. 2016; Frumkin et al. 2017; Metcalf and Lessler 2017). In many cases the consequences of urban ecological processes lead to increased burdens of health vulnerability in disadvantaged communities. Reducing urban health vulnerabilities is an important societal challenge that also serves as a problem-based unifying framework for advancing a theory. Expanding the knowledge base of how urban ecosystems function is needed (Groffman et al. 2017) and a human health orientation allows an integrative and systems approach for better understanding urban ecological dynamics. Simultaneously, improvements to urban ecological models can contribute to public health benefits through better forecasts of urban ecological dynamics and their responses to management. While much work has been conducted that addresses ecological components of human health vulnerability (e.g. Juliano and Lounibos 2005; Camargo and Alonso 2006; Jenerette et al. 2016), a systems and landscape perspective across multiple dimensions of health will increasingly allow ecological research to contribute more than it has to reducing health vulnerabilities in cities.
Urban health vulnerability will likely become more unpredictable in time and across landscapes as urban health hazards are increasingly novel: involving larger range of variances, new organisms, and synthetic chemicals than any natural analog ecosystem (Curriero et al. 2001; Sutherst 2004; Bernhardt et al. 2017). Intended and unintended ecological consequences of individual and societal activities can have a large influence on many components of health and lead to variable and dynamic landscapes of health vulnerability. The extensive hydrological plumbing of the modern “sanitary city” (Melosi 1999) provides a canonical example of large-scale urban technological manipulations to modify ecological processes of ecohydrologic flows, nutrient cycling, and microbial communities specifically for reducing health vulnerabilities. Failures of technological infrastructure in modern cities can rapidly increase urban health risks through many ecological processes (Reiner et al. 2012; Childers et al. 2014). Urban flooding can lead to acute and persisting ecological responses that contribute to a cascading series of potential health risks: drowning during the event, increased microbial diseases immediately, increased mosquito habitat and potential vector borne diseases for months, and inundated surfaces contributing to mold-derived air pollution for years (Hubalek and Halouzka 1999; Ahern et al. 2005; Rao et al. 2007; Sinigalliano et al. 2007). Both in response to chronic conditions and acute disturbances, a better understanding of how ecological processes contribute to health will improve society’s capacity to reduce health vulnerabilities.
While the concept of human health is a contested term, increasingly definitions of health include physical, mental, and social dimensions and are evaluated in terms of an “ability to adapt and self-manage” (Huber et al. 2011). Within this broad definition, ecological processes influence health vulnerability through multiple pathways influencing both hazards and well-being. Health vulnerability in response to specific environmental conditions results from an interaction between exposure to the hazard, sensitivities of individuals and populations, and capacities for coping with or adapting to consequences (Romero-Lankao et al. 2012; Harlan et al. 2013). The environmental distribution of potential hazard exposure, or the riskscape, is a primary component of health vulnerabilities, especially for residents with high sensitivities and limited coping capacity to mitigate exposure to a hazard (Romero-Lankao et al. 2012; Harlan et al. 2013; Jenerette et al. 2016). Sensitivities to hazards are shaped by physiological, as predisposition to disease, and social circumstance and varies greatly among healthy adults, children, elderly, and infirm (Harlan et al. 2014; Vanos 2015). Coping capacity differs among residents based primarily on affordability of appropriate technology but also as influenced by social networks that can provide financial and care-giving support (Harlan et al. 2013). In contrast to environmental hazard risks, which pose health risks, functional green space is correlated with human well-being through a suite of positive physical, mental, and social health indicators that may improve lived experiences and reduce sensitivities to many hazards (Alcock et al. 2014; Frumkin et al. 2017). While environmental risks, health sensitivities, and coping capacities are distinct drivers of health vulnerability, frequently their distributions are correlated such that they each increase health vulnerability in neighborhoods with high poverty and minority residents (Harlan et al. 2013; Jenerette et al. 2013; Dadvand et al. 2014). Notably, access to green space is frequently restricted in low-income and minority dominated neighborhoods leading to substantial environmental justice implications (Dadvand et al. 2014; Tan and Samsudin 2017). Reconciling the multidimensional contributions of ecological processes to urban health vulnerability and equity remains a compelling research challenge.
The contributions of ecological processes to health hazards and benefits span the traditional hierarchy of ecological processes as well as traditional independent emphases on terrestrial, hydrologic, and atmospheric domains (Fig. 1). Ecosystem processes of material and energy storage and transformation can lead to the release or sequestration of hazards (Townsend et al. 2003; Jenerette et al. 2011; Oikawa et al. 2015). Population and community processes influence other hazards through organismal growth, dispersal, and species interactions including competition, predation, and host–pathogen relationships (O’Neil et al. 2012; Metcalf and Lessler 2017). Landscape processes influence many health-related outcomes through transport and spatial organization that can introduce, concentrate or disperse hazards and influence urban riskscape connectivity. Landscape configuration can have large influences on ecological processes and corresponding influences to health as shown for both heat distributions (Zhou et al. 2017) and pollutant flowpaths (Townsend et al. 2003). Throughout a landscape, riskscape connectivity may lead to patchy distributions of risks with discrete pathway connecting risk across a landscape. Transcending specific suites of processes, many risks involve the fate and transport of pollutants, which include exchanges between terrestrial, aquatic, and atmospheric phases and environments (Townsend et al. 2003; Oikawa et al. 2015). Life histories for many organismal-related hazards, such as vector-borne diseases, span combinations of aquatic, terrestrial, and atmospheric environments (Metcalf and Lessler 2017). Orientating urban ecology toward health outcomes will necessarily lead to a better systems integration across the traditional ecological disciplinary boundaries and differences among habitats and will reflect a multifunctional landscape ecological framework that integrates across diverse processes (Mastrangelo et al. 2014; Meerow and Newell 2017).
Urban health is connected many ecological processes and spans traditionally separated ecological subdisciplines. a Ecosystem, population, and landscape processes together influence health through several mechanisms. b Ecological processes within terrestrial, aquatic, and atmospheric settings contribute to health through both biometerological and ecohydrological interactions
Reflecting the diverse and frequently non-linear ecological influences on health vulnerability landscapes, ecological contributions to health vulnerability vary over short and long time scales. Differences across temporal scales result from both dynamics of underlying drivers and self-organization of ecological processes. Chronic and geographically dispersed riskscapes can suddenly transform into acute and highly localized risks, for example health risks following urban flooding (Ahern et al. 2005). Some risks are strongly influenced by historical legacies and may persist for decades, such as soil contamination (Clarke et al. 2015), while others become more prominent during discrete events, such as heat waves (Li and Bou-Zeid 2013). In some cases hazards emerge from undetectable levels to epidemics through rapid organismal population growth rates, such as with some vector borne diseases (Johnson et al. 2015). More broadly, cities are teleconnected systems and urban health risks can arise from interactions between a city and more distal ecosystems, for example outlying agricultural emissions can lead to degradation of urban air quality (Oikawa et al. 2015). The multiple scales of variation in health risks reflect the hierarchical organization of ecological systems and multiple scales over which ecological processes operate.
Toward an ecology of health framework
Here I pose an ecological urban health framework that connects drivers of ecological processes to changes in both human health risks and benefits with associated impacts to public health vulnerability in cities (Fig. 2). This ecology of health framework is informed by advances in both urban ecosystem science and urban landscape sustainability, which provide both a systems and spatio-temporal perspective for health vulnerability (Pickett et al. 2001; Childers et al. 2014; Wu 2014; Groffman et al. 2017). Urban ecosystem science emphasizes explaining and predicting the assembly and function of novel communities with novel drivers, larger ranges of environmental variation, and chemical inputs with no natural analogs (Tanner et al. 2014; Groffman et al. 2017). A landscape sustainability perspective emphasizes pathways to urban sustainability that depend on relationships between spatial structure and ecological processes occurring across a hierarchy of scales, from individual households, neighborhoods, cities, and extended teleconnected ecosystems (Wu 2013; Opdam et al. 2018). Together the complementary theoretical frameworks provided by urban ecosystem science and landscape sustainability perspectives can be harnessed to reduce health vulnerabilities and improve well-being. Their integration leads to a systems level appreciation for the controls to ecological processes that contribute to health vulnerability and also recognition that outcomes from ecological processes reflect underlying spatial heterogeneity and emergent ecological structure at multiple scales.
Framework and scale dependence of ecological contributions to public health through multiple risk and benefit pathways. Ecological processes influence health outcomes on both hazards and sensitivity in. Ecological contributions to health are influenced by both external drivers, the designed landscape, and historical legacies. Frequently the ecological-health system is shaped by socioeconomics and can result in environmental justice health inequities. The scales of ecological processes influence health span the continuum from personal and localized experiences to teleconnected influences of hinterland ecosystems
Drivers of ecological contributions to health vulnerability comprise the nonhuman environment, active human management, and legacies of historical social conditions (Pickett et al. 2001). Environmental drivers, including climate, bedrock geology, and native biodiversity, have a prominent role in many ecological processes that affect health (Reiner et al. 2012; Clarke et al. 2015; Shiflett et al. 2017). Management activities resulting from human-induced modifications to environmental conditions, transport networks, and demographic characteristics of key species can also influence ecological processes (Johnson et al. 2015; Larsen 2015). Active management in the urban system, including engineered transport, irrigation, and chemical spraying, can be directly implemented for health benefits or changes reducing health vulnerability, may be a secondary consideration for management, or even have unintended negative health consequences. Historical legacies reflect how the distribution of present-day risks are shaped by past land uses or disturbances and can be prominent drivers of urban ecological processes (Grimm et al. 2017; Roman et al. 2018). Histories of environmental injustices also illustrate legacy effects of a segregated society in which built infrastructure differs greatly between white and black communities (Grove et al. 2018). In many cases legacies may not be readily apparent and highly variable, such as with soil contamination (Clarke et al. 2013). Individually and interactively the environment, management, and historical legacies of ecological processes, can have a strong influence on how ecological processes contribute to or detract from human health.
In response to conditions imposed by environmental, management, and historical drivers a complex series of feedbacks among many ecological agents and interaction networks influence health risks and well-being. Individual ecological processes respond to unique combinations of drivers and nonlinear responses. Ecological self-organization across processes may lead to systems robust to large changes in a driver but near a threshold small changes may lead to switches between alternate stable states (Folke et al. 2004). For individual processes or from a multifunctional perspective the resulting ecological contributions to health often exhibit strong spatial and temporal heterogeneities occurring across multiple scales in health vulnerabilities. Differences in ecological risks may vary at scales of meters or be correlated across neighborhoods and cities within a metropolitan region. Similarly, risks may vary within hours in response to acute events or persist in chronic condition for decades. In the following section, I use four examples to demonstrate the diversity of processes and scales where ecological processes contribute to health vulnerability and how the ecology of health framework can be used for each example.
Multiple dimensions of ecological influence on human health in cities
Many ecological processes are connected with health and a landscape perspective can help predict and manage health vulnerability. Using four examples I show how unique combinations of drivers and ecological responses shape ecological contributions to health vulnerability in a case study of southern California, USA. While each example highlights distinct ecological-health subsystems, in many cases the ecological contributions to urban health are coupled through linked processes and lead to multifunctional hotspots of potential health vulnerability with environmental justice implications. These examples all illustrate how research at the public health—urban ecology nexus can contribute both to development of more robust and general ecological theory and valued applications of urban ecological science.
Heat
The frequency of high urban temperature events is increasing through reinforcing combinations of global, greenhouse gas related, warming leading to more heat waves that are magnified by regional, urban heat island related, warming (Li and Bou-Zeid 2013). Correspondingly, increased urban temperatures are associated with increasingly negative health impacts (Patz et al. 2005; Weinberger et al. 2017). Approximately 30% of the world’s population are already exposed to climate conditions exceeding mortality thresholds (Mora et al. 2017). Heat load to an individual is a hazard that can directly contribute to mortality and morbidity as well as contribute indirectly to other health impacts including cardiovascular and respiratory distress (Patz et al. 2005). Heat loading is affected by radiant energy and air temperatures during the daytime with greater contribution of air temperatures at night. Correspondingly, heat related health impacts are associated with both warmer air temperatures (Harlan et al. 2014) and recently have also been associated with warmer daytime surface temperatures (Harlan et al. 2013; Vanos 2015; Jenerette et al. 2016).
Within a city, temperature distributions associated with vegetated cooling can result in substantial variation to urban thermal riskscapes. Within cities the cooling effects of vegetation can exceed more than 5° C air temperature differences at night and more than 25° C surface temperature differences during the day (Jenerette et al. 2016; Shiflett et al. 2017). The ecological processes contributing to temperature variation influence heating primarily through energy balance dynamics associated with vegetation shading and evapotranspiration (Zhou et al. 2017). The consequences of environmental variation, along with coping and sensitivity differences, contribute to a broad range of heat related illnesses in Phoenix, AZ from less than 10% of residents in some, primarily affluent and white, neighborhoods to affecting more than 50% of residents in other, high poverty and minority resident, neighborhoods (Harlan et al. 2014; Jenerette et al. 2016). Because of the direct influence of vegetation on environmental heat and corresponding relationships with heat related health outcomes, urban heat mitigation strategies increasingly include expanding vegetation as one mechanism for reducing vulnerability for many cities (Larsen 2015).
The environmental controls on the capacity of vegetation to reduce heat vulnerability are most evident in response to regional meteorological conditions, such as heat-waves. Vegetation cooling effects can become stronger in both hotter periods and locations, which may act as a negative climate feedback (Jenerette et al. 2011; Shiflett et al. 2017). Active management, especially irrigation but also other landscaping activities, is generally not directed to heat reductions but nonetheless directly affects shading and transpiration contributions to cooling. Legacies of vegetated landscaping and irrigation practices can have a large influence on the magnitude and distribution of vegetation cooling through planting and growth. In the context of these drivers, ecological self-organization is evident in ecophysiological cooling responses to meteorological conditions and the potential negative cooling feedback.
Vector borne diseases
Vector borne diseases have been a component of urban health for millennia with current increases of vectors and diseases occurring in many temperate regions (Rochlin et al. 2016). Dynamics of vector borne diseases result from interactive population and community ecological processes responding to multiple drivers (Juliano and Lounibos 2005; Johnson et al. 2015; Metcalf and Lessler 2017). A combination of globalization induced dispersal and regional changes to land use and climate are leading to range expansions of many disease vectors and pathogens from tropical origins into more temperate regions (Sutherst 2004). The spread of West Nile Virus into the United States beginning in 1999 serves as a recent example and informs responses to vector range expansion for currently invasive mosquito species including Aedes aegyptae and Aedes albopictus, which are hosts to Dengue, Chikungunya, and Zika (Metcalf and Lessler 2017). Limiting current and emerging urban vector borne diseases requires managing a suite of ecological interactions in the context of primarily constructed ecosystems and dynamic social interactions. Population control approaches from insecticide spraying to Wolbachia infection require extensive ecological knowledge and models for effective application (Johnson et al. 2015). Improving the predictive understanding of vector borne disease responses to interacting global change drivers has become a pressing research challenge (Metcalf and Lessler 2017).
In the ecology of health framework, the environmental drivers for vector borne diseases are important for determining health vulnerabilities with climate posing a restriction for many species distributions. Tools that evaluate climate filtering, such as habitat suitability models, are becoming widely used for identifying locations and time when vectors may be present (Fischer et al. 2011). Active management, through reductions in open water for breeding habitat to insecticide spraying, is used explicitly to reduce the potential exposure to disease. The historical legacy of past invasion and naturalization of a vector is a central determinant of vector-borne disease risk—preventing establishment of a vector and the pathogen provides a first line of control to vulnerability. In response to ecological drivers, self-organization ecological processes through networks of interactions among multiple species and habitats leading to thresholds and state change responses to environmental drivers (Juliano and Lounibos 2005; Johnson et al. 2015; Metcalf and Lessler 2017). Through responses to interactive drivers and ecological responses, health risks from vector borne diseases can rapidly change while also persisting indefinitely once established.
Air, soil, water pollution
Pollution, broadly resulting from anthropogenic inputs, can directly impact human health or promote pathogens in water and soil that then contribute to disease or toxins (Townsend et al. 2003; Camargo and Alonso 2006; Johnson et al. 2010). Increasingly new industrial and pharmaceutical classes of pollutants, including nanoparticles and pharmaceutical compounds, may contribute to health consequences that are increasing globally at rates comparable with increases in nitrogen fertilizers (Bernhardt et al. 2017). Ecological processes can influence many pollutant-based health risks through processes spanning ecosystem material transformation, population dynamics of potential disease causing organisms, and landscape redistribution of pollutants. The magnitude of ecological health effects and specific processes associated with health outcomes varies dramatically among pollutants and in most cases how these processes influence health outcomes have large uncertainties. For example, ground level ozone (O3) concentrations, associated with extensive health risks, are influenced by ecological processes that produce O3 precursors including nitric oxides (NOx), generated in part through biogeochemical nitrogen transformations in soils, and volatile organic compounds emitted from urban vegetation at rates that are not well constrained (Calfapietra et al. 2013; Oikawa et al. 2015). Particulate matter (PM2.5) may be released from fires or deposited on vegetation. Combined, air pollution from both O3 and PM2.5 were associated with 4.5 million deaths globally (Cohen et al. 2017). Within soils and water, extensive biological processing and uptake can influence the form, bioavailability, and distribution of many pollutants. Population dynamics and ecohydrological connectivity in response to pollutants can have important consequences for the spread of soil or water borne illnesses with examples including infections Vibrio cholera and toxins from cyanobacteria (Curriero et al. 2001; Cottingham et al. 2003; O’Neil et al. 2012). As one indicator of polluted drinking water, an estimate 1.8 billion people use drinking water suffering from fecal contamination (Bain et al. 2014).
Environmental drivers have a large influence on many pollutants with regional meteorology, geomorphology, and lithology controlling many chemical reactions and transport. Active management can remove, reroute, or immobilize many pollutants. Historical legacies are extensive and reflect long-life span of infrastructure and many chemical that influences contaminants and their movement. Self-organization associated with pollutants is present, the regulation of pollutants associated with oxygen availability and its influence on oxidation–reduction reactions is a prominent example. Improved understanding of the residence times, transport pathways, and transformations for many pollutants is needed to reduce their health risks by minimizing exposure to pollutants.
Green space and well-being benefits
In contrast to hazards, broad spectra of physical, mental, and social health and well-being benefits are associated with green space exposure (Gascon et al. 2016; Shanahan et al. 2016). Green space broadly refers to components of urban landscapes that include vegetation and spans systems managed as a more natural preserve and urban features with mixes of plant and engineered surfaces such as bioswales, city parks, and community gardens (Frumkin et al. 2017). The health benefits of green space exposure have been correlated with improvements to many physiological indicators of health vulnerabilities, mental health, and overall well-being (Alcock et al. 2014; Shanahan et al. 2016). While the mechanisms for health benefits derived from green space are not well characterized, several health benefit pathways may include opportunities for exercise and access to fresh food, social engagement, and altered human microbiomes (Dallimer et al. 2012; Shanahan et al. 2016; Frumkin et al. 2017). Green space is highly diverse in species composition, structure, rates of functioning, and phenology (Fig. 3) and the impacts to health vulnerability are also likely diverse among different types of green space. Understanding how exposure to green spaces and their ongoing ecological processes contribute to public health outcomes remains an important research challenge.
As green spaces are functioning ecosystems, they are affected by interactions between environmental drivers and self-organizing ecological processes as any ecological system. As part of an urban ecosystem, active management and historical legacies also influence both environmental drivers and ecological processes directly. Active management is frequently directed to enhancing sustainability of desired plant and wildlife communities. Management includes many activities such as resource amendments, limiting disturbances, or conservation and restoration actions. Historical legacies affecting greenspaces include planting decisions, neighborhood matrix, and placement of infrastructure; these historical legacies can affect both the environment and ecological sensitivity to the environment. In aggregate the resulting availability and functioning of green space is correlated with socio-economic and racial distributions reflecting pervasive environmental inequity as shown in many regions throughout the world (Jenerette et al. 2013; Dadvand et al. 2014; Shanahan et al. 2014). Identifying what components of greenspace most contribute to health benefits and how to ensure disadvantaged communities have equitable access to sustainable greenspace without subsequently leading to gentrification remain key research challenges.
Mutifunctional landscape of health
The ecological underpinnings of health vulnerability reflect multiple health dimensions and span ecophysiological controls to organismal functioning, biogeochemical processing, landscape connectivity, and maintenance of biodiversity. Within any location, vegetation and soils may directly influence heat, diseases, and pollutant riskscapes by providing vegetated cooling (Zhou et al. 2017), habitat for vector species (Hamilton et al. 2014), and opportunities for transforming or concentrating pollutants (Clarke et al. 2015), while at the same time providing benefits to well-being through greenspace exposure. Across a region, the overlapping and often independent landscape structure of individual hazards lead to a multifunctional landscape of health vulnerability. A multifunctional perspective links the landscape distributions of multiple axes of ecosystem functioning (Mastrangelo et al. 2014) that similarly provides an opportunity for synthetic evaluation of health vulnerability. Southern California, USA with more than 18 million residents and high social and biological diversity, serves as a useful case study for visualizing multifunctional health landscapes (Fig. 4). High temperatures, invasive disease vectors, air quality and accessible greenspace are all health challenges in the region. Each of these health components exhibit distinct landscape distributions that feature coastal to inland gradients and localized influences of individual factors. By considering multifunctional landscapes of urban health, trade-offs in hazards and benefits can be considered simultaneously. Together their joint distributions lead to hotspots of multiple factors contributing to health vulnerability and other locations with reduced health threats related to ecological processes.
Multifunctional landscape of ecological contributions to health in the urbanized region of Los Angeles, CA County in southern California. Individual contributors of surface temperature (a), mosquito detections for both recently invaded A. aegypti and A. albopictus (b), atmospheric ozone (c), and local availability of urban parks (d). Each of the individual variables of ecological contribution to health were combined as a suite of indicators varying from 0 to 1 to show a combined landscape distribution of ecological risk contributors (e). Original data and range for use as ecological health indictor is shown for each panel. Surface temperature data were obtained for 2015. Mosquito distributions are from full historical records. These data represent best estimates of detection although areas without detected mosquitos include surveys that have not detected and areas that have not conducted surveys. Ozone distributions were generated from interpolated of a limited network and do not show fine scale variation in ozone distributions. Park accessibility was obtained from accessible open space from the county of Los Angeles
Prognosis: urban landscape ecological research for improved human health
Where is progress in moving towards an ecological science of urban health vulnerabilities? Through an increasing emphasis on convergence research—research deeply interdisciplinary and driven by specific problems (National Research Council 2014)—new teams are increasingly providing opportunities for ecologists to contribute to reducing human health vulnerability. These teams are generating new decision support tools that can rapidly identify changes in risk, communicate risk states, and evaluate likely benefits of alternative interventions (Rieb et al. 2017). Examples within the United States of success from integrated urban health risk analysis include water borne disease (Reiner et al. 2012) and urban heat (Harlan et al. 2014). Ongoing convergence research that brings together interdisciplinary teams for reducing health risks are including ecologists throughout a broad scale-continuum spanning the individual (Kuras et al. 2017), household (Jenerette et al. 2016), neighborhood (Harlan et al. 2013), and extending to regional teleconnections (Oikawa et al. 2015). The increasing knowledge base and predictive skill derived from these collaborative endeavors can be used to providing decision support for urban planning to create persistent infrastructures that promote more healthful environments (Larsen 2015). Increasing engagement between ecologists and planners is facilitating urban design processes that incorporate and build on ecological knowledge (Felson et al. 2013; Ross et al. 2015). Expanding these efforts to further include engineers and health scientists is an important step. Such collaborations will in some cases require new funding mechanisms that facilitate integration between basic ecological and health sciences.
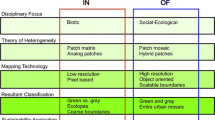
Another avenue of progress in identifying ecological contributions to health has occurred through improved high-resolution data and modeling resources. Recent examples across multiple hazards have identified large riskscape variation at fine scales of less than 10 m, in some cases more than a doubling of risk as with climate (Jenerette et al. 2016; Patton et al. 2017) and in other cases more than an order of magnitude variation in risk as with soil contamination in some urban greenspaces (Clarke et al. 2015). Including health outcome data with assessments of risks are still rare but are essential for assessing impacts of environmental risk (Jenerette et al. 2016). High resolution data and models are allowing evaluations of health vulnerabilities approaching scales of individual experiences that have historically only been available at coarser neighborhood or whole city scales. New opportunities with high-resolution remote sensing and high density embedded sensor networks provide examples of approaches for evaluating risks at high spatial and temporal resolution (Jenerette et al. 2016; Shiflett et al. 2017). New satellite- and airborne-based sensors are providing improved capabilities to assess within-city distributions of climate (Li et al. 2015) and air quality (Zoogman et al. 2017). Individual-scale environmental assessments through wearable sensors may be useful for evaluating health outcomes with notable progress occurring for heat and air quality risks (Steinle et al. 2013; Kuras et al. 2017). Similarly, urban models are becoming increasingly refined and are providing an individual-scale resolution of some risk distributions (Middel et al. 2014; Patton et al. 2017). Assessments of risk-response differences among individuals, especially sensitive groups, such as children and elderly, will further improve individualized health vulnerability assessments (Harlan et al. 2014; Vanos 2015). A continued emphasis on quantifying ecological-health interactions at fine spatial and temporal scales will likely facilitate a transition from correlations with unclear causes to mechanisms with useful predictive skill for improving human health.
Central to expanding an ecology of health perspective are systems- and mechanistic-oriented evaluations of how ecological processes contribute to health vulnerabilities and the effectiveness of management to improve health outcomes (Liddicoat et al. 2016; Grimm et al. 2017). Improved assessments of systems-level dynamics are central for understanding how connectivity and feedbacks lead to large differences in ecological dynamics (Folke et al. 2004) and their contributions to health vulnerability. Examples of integrative assessments and responses to vector-borne diseases and heat reflect the benefits of systems perspectives. As part of a systems perspective, a better characterization of how ecological contributions to health vulnerability are spatially distributed and how the configuration of ecosystems can improve forecasting health vulnerabilities and developing interventions that contribute to health (Rieb et al. 2017). Examples where configuration plays a prominent role in the dynamics of the ecological health system include climate distributions (Zhou et al. 2017) and pollutant flowpaths (Townsend et al. 2003). The multifunctional perspective (Mastrangelo et al. 2014; Meerow and Newell 2017) will be useful to link system dynamics that involve multiple pathways of health impacts and their loosely correlated landscape structures. Intersecting the multifunctional landscapes of ecological contributions to health with a better characterization of the distribution of people’s coping capacity, exposure, and sensitivity may help address health vulnerabilities as much or more than many ecological processes alone. The geographic correlations of ecological and societal drivers to health vulnerability often results in social inequity of public health vulnerability that itself may be an important contributor to increased health vulnerability (Jenerette et al. 2011; Harlan et al. 2013; Tan and Samsudin 2017).
The framework developed here looks toward a coherent approach to evaluate and forecast ecological contributions to health vulnerability that relies on pattern-process relationships, multiple-scale interactions, and integrative place-based analyses. A human health orientation of urban ecology for cities will generate a better basic understanding of how ecological processes in a city contribute to well-being and foster improved management of urban ecosystems to reduce multiple health vulnerabilities. Using health as a problem-based, or convergence, research agenda for ecology will provide opportunities to integrate across ecological subfields while also connecting ecological science more deeply with health, engineering, and social sciences.
References
Ahern M, Kovats RS, Wilkinson P, Few R, Matthies F (2005) Global health impacts of floods: epidemiologic evidence. Epidemiol Rev 27:36–46
Alcock I, White MP, Wheeler BW, Fleming LE, Depledge MH (2014) Longitudinal effects on mental health of moving to greener and less green urban areas. Environ Sci Technol 48:1247–1255
Bain R, Cronk R, Hossain R, Bonjour S, Onda K, Wright J, Yang H, Slaymaker T, Hunter P, Prüss-Ustün A, Bartram J (2014) Global assessment of exposure to faecal contamination through drinking water based on a systematic review. Tropical Med Int Health 19:917–927
Bernhardt ES, Rosi EJ, Gessner MO (2017) Synthetic chemicals as agents of global change. Front Ecol Environ 15:84–90
Calfapietra C, Fares S, Manes F, Morani A, Sgrigna G, Loreto F (2013) Role of biogenic volatile organic compounds (BVOC) emitted by urban trees on ozone concentration in cities: a review. Environ Pollut 183:71–80
Camargo JA, Alonso A (2006) Ecological and toxicological effects of inorganic nitrogen pollution in aquatic ecosystems: a global assessment. Environ Int 32:831–849
Childers DL, Pickett STA, Grove JM, Ogden L, Whitmer A (2014) Advancing urban sustainability theory and action: challenges and opportunities. Landsc Urban Plan 125:320–328
Clarke LW, Jenerette GD, Davila A (2013) The luxury of vegetation and the legacy of tree biodiversity in Los Angeles. CA Landsc Urban Plan 116:48–59. https://doi.org/10.1016/j.landurbplan.2013.04.006
Clarke LW, Jenerette GD, Bain DJ (2015) Urban legacies and soil management affect the concentration and speciation of trace metals in Los Angeles community garden soils. Environ Pollut 197:1–12
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH (2017) Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet 389:1907–1918. https://doi.org/10.1016/S0140-6736(17)30505-6
Cottingham KL, Chiavelli DA, Taylor RK (2003) Environmental microbe and human pathogen: the ecology and microbiology of Vibrio cholerae. Front Ecol Environ 1:80–86
Curriero FC, Patz JA, Rose JB, Lele S (2001) The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948-1994. Am J Public Health 91:1194–1199
Dadvand P, Wright J, Martinez D, Basagana X, McEachan RRC, Cirach M, Gidlow CJ, de Hoogh K, Grazuleviciene R, Nieuwenhuijsen MJ (2014) Inequality, green spaces, and pregnant women: Roles of ethnicity and individual and neighbourhood socioeconomic status. Environ Int 71:101–108. https://doi.org/10.1016/j.envint.2014.06.010
Dallimer M, Irvine KN, Skinner AMJ, Davies ZG, Rouquette JR, Maltby LL, Warren PH, Armsworth PR, Gaston KJ (2012) Biodiversity and the Feel-Good Factor: Understanding Associations between Self-Reported Human Well-being and Species Richness. Bioscience 62:47–55. https://doi.org/10.1525/bio.2012.62.1.9
Felson AJ, Pavao-Zuckerman M, Carter T, Montalto F, Shuster B, Springer N, Stander EK, Starry O (2013) Mapping the design process for urban ecology researchers. Bioscience 63:854–865
Fischer D, Thomas SM, Niemitz F, Reineking B, Beierkuhnlein C (2011) Projection of climatic suitability for Aedes albopictus Skuse (Culicidae) in Europe under climate change conditions. Glob Planet Change 78:54–64
Folke C, Carpenter S, Walker B, Scheffer M, Elmqvist T, Gunderson L, Holling CS (2004) Regime shifts, resilience, and biodiversity in ecosystem management. Annu Rev Ecol Evol Syst 35:557–581.
Frumkin H, Bratman GN, Breslow SJ, Cochran B, Kahn PH, Lawler JJ, Levin PS, Tandon PS, Varanasi U, Wolf KL, Wood SA (2017) Nature contact and human health: A research agenda. Environ Health Perspect. https://doi.org/10.1289/EHP1663
Gascon M, Triguero-Mas M, Martinez D, Dadvand P, Rojas-Rueda D, Plasencia A, Nieuwenhuijsen MJ (2016) Residential green spaces and mortality: a systematic review. Environ Int 86:60–67
Grimm NB, Pickett STA, Hale RL, Cadenasso ML (2017) Does the ecological concept of disturbance have utility in urban social–ecological–technological systems? Ecosyst Health Sustain. https://doi.org/10.1002/ehs2.1255
Groffman PM, Cadenasso ML, Cavender-Bares J, Childers DL, Grimm NB, Grove JM, Hobbie SE, Hutyra LR, Jenerette GD, McPhearson T, Pataki DE, Pickett STA, Pouyat RV, Rosi-Marshall E, Ruddell BL (2017) Moving towards a new urban systems science. Ecosystems 20:38–43. https://doi.org/10.1007/s10021-016-0053-4
Grove M, Ogden L, Pickett S, Boone C, Buckley G, Locke DH, Lord C, Hall B (2018) The legacy effect: understanding how segregation and environmental injustice unfold over time in Baltimore. Ann Am Assoc Geogr 108:524–537. https://doi.org/10.1080/24694452.2017.1365585
Hamilton AJ, Burry K, Mok HF, Barker SF, Grove JR, Williamson VG (2014) Give peas a chance? Urban agriculture in developing countries. A review. Agron Sustain Dev 34:45–73
Harlan SL, Chowell G, Yang S, Petitti DB, Butler EJM, Ruddell BL, Ruddell DM (2014) Heat-related deaths in hot cities: estimates of human tolerance to high temperature thresholds. Int J Environ Res Public Health 11:3304–3326
Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB (2013) Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ Health Perspect 121:197–204
Hubalek Z, Halouzka J (1999) West Nile fever—a reemerging mosquito-borne viral disease in Europe. Emerg Infect Dis 5:643–650
Huber M, Knottnerus JA, Green L, van der Horst H, Jadad AR, Kromhout D, Leonard B, Lorig K, Loureiro MI, van der Meer JWM, Schnabel P, Smith R, van Weel C, Smid H (2011) How should we define health? Br Med J. https://doi.org/10.1136/bmj.d4163
Jenerette GD, Harlan SL, Buyantuev A, Stefanov WL, Declet-Barreto J, Ruddell BL, Myint SW, Kaplan S, Li XX (2016) Micro-scale urban surface temperatures are related to land-cover features and residential heat related health impacts in Phoenix, AZ USA. Landsc Ecol 31:745–760. https://doi.org/10.1007/s10980-015-0284-3
Jenerette GD, Greg M, Alexander B, Diane EP, Thomas WG, Stephanie P (2013) Urban vegetation and income segregation in drylands: a synthesis of seven metropolitan regions in the southwestern United States. Environ Res Lett 8:044001
Jenerette GD, Harlan SL, Stefanov WL, Martin CA (2011) Ecosystem services and urban heat riskscape moderation: water, green spaces, and social inequality in Phoenix, USA. Ecol Appl 21:2637–2651
Johnson PTJ, Townsend AR, Cleveland CC, Glibert PM, Howarth RW, McKenzie VJ, Rejmankova E, Ward MH (2010) Linking environmental nutrient enrichment and disease emergence in humans and wildlife. Ecol Appl 20:16–29. https://doi.org/10.1890/08-0633.1
Johnson PTJ, De Roode JC, Fenton A (2015) Why infectious disease research needs community ecology. Science. https://doi.org/10.1126/science.1259504
Juliano SA, Lounibos LP (2005) Ecology of invasive mosquitoes: effects on resident species and on human health. Ecol Lett 8:558–574
Kuras ER, Richardson MB, Calkins MM, Ebi KL, Hess JJ, Kintziger KW, Jagger MA, Middel A, Scott AA, Spector JT, Uejio CK, Vanos JK, Zaitchik BF, Gohlke JM, Hondula DM (2017) Opportunities and challenges for personal heat exposure research. Environ Health Perspect. https://doi.org/10.1289/EHP1556
Larsen L (2015) Urban climate and adaptation strategies. Front Ecol Environ 13:486–492
Li D, Bou-Zeid E (2013) Synergistic interactions between urban heat islands and heat waves: the impact in cities is larger than the sum of its parts. J Appl Meteorol Climatol 52:2051–2064
Li J, Carlson BE, Lacis AA (2015) How well do satellite AOD observations represent the spatial andtemporal variability of PM2.5 concentration for the United States? Atmos Environ 102:260–273. https://doi.org/10.1016/j.atmosenv.2014.12.010
Liddicoat C, Waycott M, Weinstein P (2016) Environmental change and human health: can environmental proxies inform the biodiversity hypothesis for protective microbial-human contact? Bioscience 66:1023–1034.
Mastrangelo ME, Weyland F, Villarino SH, Barral MP, Nahuelhual L, Laterra P (2014) Concepts and methods for landscape multifunctionality and a unifying framework based on ecosystem services. Landscape Ecol 29:345–358.
Meerow S, Newell JP (2017) Spatial planning for multifunctional green infrastructure: growing resilience in Detroit. Landsc Urban Plan 159:62–75.
Melosi MV (1999) The sanitary city: urban infrastructure in America from colonial times to the present. The Johns Hopkins University Press, Baltimore
Metcalf CJE, Lessler J (2017) Opportunities and challenges in modeling emerging infectious diseases. Science 357:149–152.
Middel A, Hab K, Brazel AJ, Martin CA, Guhathakurta S (2014) Impact of urban form and design on mid-afternoon microclimate in Phoenix Local Climate Zones. Landsc Urban Plan 122:16–28.
Mora C, Dousset B, Caldwell IR, Powell FE, Geronimo RC, Bielecki CR, Counsell CW, Dietrich BS, Johnston ET, Louis LV, Lucas MP, McKenzie MM, Shea AG, Tseng H, Giambelluca T, Leon LR, Hawkins E, Trauernicht C (2017) Global risk of deadly heat. Nat Clim Chang 7:501. https://doi.org/10.1038/nclimate3322
National Research Council (2014) Convergence: Facilitating transdisciplinary integration of life sciences, physical sciences, engineering, and beyond. The National Academies Press, Washington, DC
Oikawa PY, Ge C, Wang J, Eberwein JR, Liang LL, Allsman LA, Grantz DA, Jenerette GD (2015) Unusually high soil nitrogen oxide emissions influence air quality in a high-temperature agricultural region. Nat Commun. https://doi.org/10.1038/ncomms9753
O’Neil JM, Davis TW, Burford MA, Gobler CJ (2012) The rise of harmful cyanobacteria blooms: the potential roles of eutrophication and climate change. Harmful Algae 14:313–334.
Opdam P, Luque S, Nassauer J, Verburg PH, Wu JG (2018) How can landscape ecology contribute to sustainability science? Landscape Ecol 33:1–7.
Patton AP, Milando C, Durant JL, Kumar P (2017) Assessing the suitability of multiple dispersion and land use regression models for urban traffic-related ultrafine particles. Environ Sci Technol 51:384–392.
Patz JA, Campbell-Lendrum D, Holloway T, Foley JA (2005) Impact of regional climate change on human health. Nature 438:310–317
Pickett STA, Cadenasso ML, Grove JM, Nilon CH, Pouyat RV, Zipperer WC, Costanza R (2001) Urban ecological systems: linking terrestrial ecological, physical, and socioeconomic components of metropolitan areas. Annu Rev Ecol Syst 32:127–157
Rao CY, Riggs MA, Chew GL, Muilenberg ML, Thorne PS, Van Sickle D, Dunn KH, Brown C (2007) Characterization of airborne molds, endotoxins, and glucans in homes in New Orleans after hurricanes Katrina and Rita. Appl Environ Microbiol 73:1630–1634. https://doi.org/10.1128/aem.01973-06
Reiner RC, King AA, Emch M, Yunus M, Faruque ASG, Pascual M (2012) Highly localized sensitivity to climate forcing drives endemic cholera in a megacity. Proc Natl Acad Sci USA 109:2033–2036
Rieb JT, Chaplin-Kramer R, Daily GC, Armsworth PR, Bohning-Gaese K, Bonn A, Cumming GS, Eigenbrod F, Grimm V, Jackson BM, Marques A, Pattanayak SK, Pereira HM, Peterson GD, Ricketts TH, Robinson BE, Schroter M, Schulte LA, Seppelt R, Turner MG, Bennett EM (2017) When, where, and how nature aatters for ecosystem services: challenges for the next generation of ecosystem service models. Bioscience 67:820–833. https://doi.org/10.1093/biosci/bix075
Rochlin I, Faraji A, Ninivaggi DV, Barker CM, Kilpatrick AM (2016) Anthropogenic impacts on mosquito populations in North America over the past century Nature. Communications. https://doi.org/10.1038/ncomms13604
Roman LA, Pearsall H, Eisenman TS, Conway TM, Fahey RT, Landry S, Vogt J, van Doorn NS, Grove JM, Locke DH, Bardekjian AC, Battles JJ, Cadenasso ML, van den Bosch CCK, Avolio M, Berland A, Jenerette GD, Mincey SK, Pataki DE, Staudhammer C (2018) Human and biophysical legacies shape contemporary urban forests: a literature synthesis. Urban For Urban Green 31:157–168. https://doi.org/10.1016/j.ufug.2018.03.004
Romero-Lankao P, Qin H, Dickinson K (2012) Urban vulnerability to temperature-related hazards: a meta-analysis and meta-knowledge approach global environmental change-human and policy. Dimensions 22:670–683
Ross MRV, Bernhardt ES, Doyle MW, Heffernan JB (2015) Designer ecosystems: incorporating design approaches into applied ecology. In: Gadgil A, Tomich TP (eds) Annual review of environment and resources, vol 40. Annual Reviews, Palo Alto, pp 419–443
Shanahan DF, Bush R, Gaston KJ, Lin BB, Dean J, Barber E, Fuller RA (2016) Health benefits from nature experiences depend on dose. Sci Rep. https://doi.org/10.1038/srep28551
Shanahan DF, Lin BB, Gaston KJ, Bush R, Fuller RA (2014) Socio-economic inequalities in access to nature on public and private lands: a case study from Brisbane, Australia. Landsc Urban Plan 130:14–23
Shiflett SA, Liang LYL, Crum SM, Feyisa GL, Wang J, Jenerette GD (2017) Variation in the urban vegetation, surface temperature, air temperature nexus. Sci Total Environ 579:495–505
Sinigalliano CD, Gidley ML, Shibata T, Whitman D, Dixon TH, Laws E, Hou A, Bachoon D, Brand L, Amaral-Zettler L, Gast RJ, Steward GF, Nigro OD, Fujioka R, Betancourt WQ, Vithanage G, Mathews J, Fleming LE, Solo-Gabriele HM (2007) Impacts of hurricanes Katrina and Rita on the microbial landscape of the New Orleans area. Proc Natl Acad Sci U S A 104:9029–9034. https://doi.org/10.1073/pnas.0610552104
Steinle S, Reis S, Sabel CE (2013) Quantifying human exposure to air pollution-Moving from static monitoring to spatio-temporally resolved personal exposure assessment. Sci Total Environ 443:184–193
Sutherst RW (2004) Global change and human vulnerability to vector-borne diseases. Clin Microbiol Rev. https://doi.org/10.1128/cmr.17.1.136-173.2004
Tan PY, Samsudin R (2017) Effects of spatial scale on assessment of spatial equity of urban park provision. Landsc Urban Plann 158:139–154
Tanner CJ, Adler FR, Grimm NB, Groffman PM, Levin SA, Munshi-South J, Pataki DE, Pavao-Zuckerman M, Wilson WG (2014) Urban ecology: advancing science and society. Front Ecol Environ 12:574–581. https://doi.org/10.1890/140019
Townsend AR, Howarth RW, Bazzaz FA, Booth MS, Cleveland CC, Collinge SK, Dobson AP, Epstein PR, Keeney DR, Mallin MA, Rogers CA, Wayne P, Wolfe AH (2003) Human health effects of a changing global nitrogen cycle. Front Ecol Environ 1:240–246. https://doi.org/10.2307/3868011
Vanos JK (2015) Children’s health and vulnerability in outdoor microclimates: a comprehensive review. Environ Int 76:1–15
Weinberger KR, Haykin L, Eliot MN, Schwartz JD, Gasparrini A, Wellenius GA (2017) Projected temperature-related deaths in ten large US metropolitan areas under different climate change scenarios. Environ Int 107:196–204
Wu JG (2013) Landscape sustainability science: ecosystem services and human well-being in changing landscapes. Landscape Ecol 28:999–1023
Wu JG (2014) Urban ecology and sustainability: the state-of-the-science and future directions. Landsc Urban Plan 125:209–221
Zhou WQ, Wang J, Cadenasso ML (2017) Effects of the spatial configuration of trees on urban heat mitigation: a comparative study. Remote Sens Environ 195:1–12
Zoogman P, Liu X, Suleiman RM, Pennington WF, Flittner DE, Al-Saadi JA, Hilton BB, Nicks DK, Newchurch MJ, Carr JL, Janz SJ, Andraschko MR, Arola A, Baker BD, Canova BP, Miller CC, Cohen RC, Davis JE, Dussault ME, Edwards DP, Fishman J, Ghulam A, Abad GG, Grutter M, Herman JR, Houck J, Jacob DJ, Joiner J, Kerridge BJ, Kim J, Krotkov NA, Lamsal L, Li C, Lindfors A, Martin RV, McElroy CT, McLinden C, Natraj V, Neil DO, Nowlan CR, O'Sullivan EJ, Palmer PI, Pierce RB, Pippin MR, Saiz-Lopez A, Spurr RJD, Szykman JJ, Torres O, Veefkind JP, Veihelmann B, Wang H, Wang J, Chance K (2017) Tropospheric emissions: Monitoring of pollution (TEMPO). J Quant Spectrosc Radiat Transf 186:17–39. https://doi.org/10.1016/j.jqsrt.2016.05.008
Acknowledgements
I appreciate the thoughtful comments of Sharon Harlan on a draft of this manuscript. I thank Robert Johnson for making Fig. 2. This work was supported by National Aeronautics and Space Administration (NNX12AQ02G), and National Science Foundation (DEB – 1656062; CBE – 1444758).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenerette, G.D. Ecological contributions to human health in cities. Landscape Ecol 33, 1655–1668 (2018). https://doi.org/10.1007/s10980-018-0708-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10980-018-0708-y