Abstract
Differential scanning calorimetry (DSC), isothermal stress testing–Fourier transform infrared spectroscopy (IST–FTIR), isothermal stress testing–high-performance liquid chromatography, and powder X-ray diffraction (PDRX) were used as screening techniques for assessing the compatibility of tobramycin with some currently employed ophthalmic excipients. In the first phase of the study, DSC was used as a tool to detect any interaction. The absolute value of the difference between the enthalpy of the pure tobramycin melting peak and that of its melting peak in the different analyzed mixtures was chosen as a parameter of the drug–excipient interaction degree. DSC results demonstrated that benzalkonium chloride, monobasic sodium phosphate, boric acid, edetate disodium, sodium metabisulfite, thimerosal, and potassium sorbate interact with tobramycin. Taking into account these results, it could be suggested that some of the changes observed in the IST–FTIR spectra of binary blends of tobramycin and some of the excipients would account for a possible interaction between the mixture component. In this study, PDRX did not provide much information, since only tobramycin–thimerosal interactions could be detected. DSC and IST–FTIR are suitable and simple methods for the detection of potential incompatibilities between active pharmaceutical ingredient (API) and excipients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Studies of active pharmaceutical ingredient (API)–excipient compatibility represent an important study in the preformulation stage of the development of new dosage forms. The potential physical and chemical interactions between an API and the excipients can affect the chemical nature, the stability, and bioavailability of the former and, consequently, its therapeutic efficacy and safety [1]. Solid dosage forms are generally less stable than their API components. Despite the importance of API–excipient compatibility testing, there is no universally accepted protocol to assess such interactions [2, 3].
Changes in color, taste, odor, polymorphic form, or crystallization of an API are some of the alterations caused by its interaction with the excipient (pharmaceutical incompatibility) [4].
On the other hand, a chemical interaction involves a chemical reaction between the excipient and the API, which leads to an increase in the chemical degradation rate of the API [4]. Formulation scientists have employed different thermoanalytical techniques to predict the suitability of the excipients to be employed in dosage forms to minimize the untoward reactions (stability issues) caused by API–excipient incompatibility [4].
Differential scanning calorimetry (DSC) has been suggested as a simple and rapid method for evaluating physicochemical interactions between the API and excipients in order to select the most compatible combinations [5,6,7,8,9,10,11,12,13,14,15,16]. However, Liltorp et al. [17] have suggested that the data obtained by thermal techniques are difficult to interpret and that they may be misleading. Moreover, the interactions observed at high temperatures during DSC assays may not represent those occurring under normal storage conditions. These authors recommend isothermal stress testing (IST) and Fourier transform infrared spectroscopy (FTIR) as simple techniques for the detection of interactions between the API and the excipients. A reduction in the peak intensity, the disappearance of an absorption peak, or the appearance of new peaks give a clear proof for interactions between the excipient and the API under study [17,18,19,20].
Other methods that are commonly employed for evaluating the API–excipient compatibility are the isothermal stress testing–high performance liquid chromatography (IST–HPLC), and powder X-ray diffraction (PDRX). The IST–HPLC involves storing the API–excipient blends at high temperature and determining the API content by HPLC [19, 21,22,23,24]. The PDRX can be used to evaluate compatibility of API with excipients [15, 22, 25,26,27,28].
Tobramycin, d-streptamine, O-3-amino-3-deoxy-α-d-glucopyranosyl-(1 → 6)-O-[2,6-diamino-2,3,6-trideoxy-α-d-ribo-hexopyranosyl-(1 → 4)]-2-deoxy is a water-soluble aminoglycoside antibiotic produced by the fungus Streptomyces tenebrarius. This antibiotic is used in a variety of pharmaceutical applications including ophthalmic solutions; suspensions and ointments; inhalation solutions; and solutions for intravenous administration [29, 30]. It is active against a broad spectrum of Gram-negative bacteria. Eye drops formulations are commercially available in the Argentinian pharmaceutical market. These formulations require different conservation conditions (ambient temperature or refrigerator). Previously, we formulated six eye drops solutions and studied their stability at 2–8, 25, and 40 °C, 75% relative humidity (RH). The USP method was followed to quantitate the API. Only three formulations were found to be stable for 2 years at ambient temperature. The expected expiry date for the formulations is within this time span. Only one formulation was stable for 2 years under the same conditions. In refrigerator, five formulations were found to be stable for more than 4 years. One system was unstable under the three conservation conditions studied [31]. In order to investigate the mechanisms governing the stability of the proposed formulations, a compatibility study with the excipients was also performed. Differential scanning calorimetry (DSC), isothermal stress testing–Fourier transform infrared spectroscopy (IST–FTIR), isothermal stress testing–high performance liquid chromatography (IST–HPLC), and powder X-ray diffraction (PDRX) were used as screening techniques for assessing the compatibility of tobramycin with the ophthalmic excipients employed.
Experimental
Materials
The following chemicals were employed: tobramycin (955.9 μg g−1 calculated with reference to the dried substance, Cross Chem, China), benzalkonium chloride (Merck, Germany), sodium chloride (Merck, USA), dibasic sodium phosphate anhydrous (Anedra, Argentina), monobasic sodium phosphate dihydrate (Anedra, Argentina), boric acid (J.T Baker, Mexico), anhydrous sodium sulfate (Anedra, Argentina), tyloxapol (Sigma-Aldrich, India), edetate disodium (Merck, Germany), sodium hydroxide (Anedra, Argentina), sodium metabisulfite (J.T. Baker, Mexico), thimerosal (Ningbo Hi-Tech, China), sodium hyaluronate (CPN SPOL SRO, Czech Republic), granular potassium sorbate (Merck, Germany), sulfuric acid (Merck, Germany), TRIS buffer (Tris (hydroxymethyl) aminomethane, BioPack, Argentina), 2,4-dinitrofluorobenzene (Sigma-Aldrich, USA), p-naphtholbenzein (Sigma-Aldrich, USA), and distilled water. All chemicals used were pharmaceutical grade, except for sulfuric acid, TRIS buffer, 2,4-dinitrofluorobenzene, and p-naphtholbenzein, which were analytical grade, and acetonitrile and water, which were HPLC grade. Solvents were filtered through a 0.45-μm membrane and degassed before used.
Differential scanning calorimetry
A differential scanning calorimeter (DSC 822, Mettler Toledo, Switzerland) was used for thermal analysis of tobramycin and excipients. A general 1:1 excipient–API ratio was used in the present study [31]. API and excipient samples, as well as physical mixtures, were weighed directly in the pierced DSC aluminum pan and scanned in a temperature range of 40–270 °C under a dry nitrogen atmosphere. A heating rate of 10 °C min−1 was used. The DSC cell was calibrated with indium (m.p. 156.6 °C; ΔHmelt 28.5 J g−1) and zinc (m.p. 419.6 °C) as standards. Curves were then analyzed for the presence of interactions.
Fourier transform infrared spectroscopy (FTIR)
Infrared spectra (4000–400 cm−1) were recorded on a Nicolet iS10 FTIR spectrometer (Thermo Scientific, USA). Solid samples were placed over a diamond attenuated total reflectance (ATR) accessory (Smart iTR, USA), without any grinding or KBr. Spectra were collected with 32 scans at 4 cm−1 resolution.
Tobramycin and physical mixtures with excipients were subsequently placed in a sealed glass container and kept at ambient temperature, at 40 °C and 75% RH and at 40 °C and 75% RH with the addition of 100 μL of distilled water, both during 4 days. Before recording the infrared spectra, samples were vacuum-dried at 40 °C.
Isothermal stress testing
For IST studies, tobramycin and different excipients were weighed directly in 5-mL glass vials (n = 2) and mixed on a vortex mixer for 2 min. The API–excipient blend was further mixed with a glass capillary (both the ends of which were heat sealed). To prevent any loss of material, capillary was broken and left inside the vial. Each vial was sealed using a Teflon-lined screw cap and stored at 40 °C in a hot-air oven (Ionomex, Argentina). Samples were periodically examined for any color change. After 1 month of storage under the conditions specified above, samples were quantitatively analyzed by HPLC [32]. API–excipient blends without added water and stored in refrigerator served as controls. For sample preparation, the mixture was dissolved in 20 mL of water and then taken to volume with water in a 25-mL flask. One milliliter was then withdrawn and diluted with water to volume in a 25-mL volumetric flask and mixed. Solutions were filtered through a 0.45-μm nylon membrane before injection (25-mm disposable filter; Cat. N° R04SP02500 Osmonics Inc., Minnesota, USA).
For the preparation of the standard, an accurately weighed quantity of 33 mg of tobramycin was transferred to a 50-mL volumetric flask, and 1 mL of 1 N sulfuric acid was added and dissolved in 20 mL of water. The mixture was then taken to volume with water. Ten milliliters was then transferred to a 50-mL volumetric flask, diluted with water to volume, and mixed. Solutions were filtered through a 0.45-μm nylon membrane before injection (25-mm disposable filter; Cat. N° R04SP02500 Osmonics Inc., Minnesota, USA).
Derivatization
A 10 mg mL−1 solution of 2,4-dinitrofluorobenzene in ethyl alcohol was prepared and maintained during 5 days in refrigerator.
A 15 mg mL−1 stock solution of TRIS was prepared in water. Forty milliliters was then transferred to a 200-mL volumetric flask and diluted to volume with dimethyl sulfoxide. This reagent was used within 4 h.
To separate 50-mL volumetric flask, 4.0 mL of standard preparation, 4.0 mL of sample preparation, and 4.0 mL of water were transferred, and 10 mL of 2,4-dinitrofluorobenzene solution plus 10 mL of TRIS solution was added. The volumetric flasks were kept in a water bath at 60 ± 2 °C during 50 ± 5 min. The flask was then removed from the bath and allowed to stand for 10 min. Acetonitrile was then added to about 2 mL below the 50-mL mark, and the mixture was then allowed to cool to room temperature, then diluted with acetonitrile to volume, and mixed.
The resolution solution was prepared by transferring 2 mL of a fresh solution of p-naphtholbenzein in acetonitrile (0.24 mg mL−1) to a 10-mL volumetric flask and diluted with the derivatized standard preparation to volume and used immediately.
A blank injection of the mobile phase was followed by another injection of the derivatization solution diluted as the standard and the resolution solutions. The relative retention times were about 0.6 for p-naphtholbenzein and 1.0 for tobramycin, and the resolution (R) value between the two peaks was ≥ 4.0. The derivatized standard preparation was chromatographed, and the responses were recorded until the relative standard deviation for replicates was < 2.0%. Equal volumes of the derivatized standard and the derivatized assay preparations were then injected separately. Major peak areas were measured for compounds quantification.
Instrumentation
For the analysis of API–excipient mixtures, an HPLC system equipped with a dual-piston reciprocating Thermo Finnigan pump (Waltham, Massachusetts, USA, Model P2000), a Rheodyne injector (Model 7125), and a UV–Vis KONIK detector (Barcelona, Spain, Model KNK-027-757) operating with the WinPCCChrom XY software (Buenos Aires, Argentina) was used.
A C18 reversed-phase column (Phenomenex, Torrance, CA, USA) 300 × 4.6 mm, 10 μm, was employed. The separation was carried out under isocratic elution conditions with acetonitrile–TRIS buffer. For the preparation of the mobile phase, 2 g of TRIS was dissolved in 800 mL of water. To this solution, 20 mL of sulfuric acid was added and diluted to 2000 mL with acetonitrile. The flow rate was 1.1 mL min−1. Elution was monitored at 365 nm, and the injection volume was 20 μL. The HPLC device was operated at ambient temperature. Under these conditions, the retention time (Rt) for tobramycin was roughly 6 min.
Before injecting the solutions, the column was stabilized for at least 30 min with the mobile phase flowing through the system. The compounds quantification was accomplished using the external standard method. Each solution was prepared in duplicate and injected in triplicate. The relative standard deviation (RSD) was < 2.0%.
Powder X-ray diffraction (PXRD)
PXRD data were collected at room temperature (RT) using a D8 Advance X-ray diffractometer (Bruker AXS, Germany). The target was a copper tube (Cu Kα radiation θ = 1.5418 Å) and a post-diffraction graphite monochromator. The X-ray generator was set at a voltage of 40 kV and current of 40 mA. Samples were subjected to PXRD analysis in step mode with a step size of 0.05° 2θ and a step time of 3 s over an angular range of 2°–50° 2θ. The sample holder was rotated in a plane parallel to its surface at the speed of 30 rpm during the measurements. The diffractograms obtained were analyzed with the DIFFRACplus EVA diffraction software (Bruker AXS, Germany).
Results and discussion
API–excipient compatibility testing
DSC has been proposed as a simple method for evaluating physicochemical interactions between components of a formulation through the comparison of thermal curves of tobramycin with those obtained with a 1:1 physical mixture with excipients.
Interactions between tobramycin and excipients are deduced from DSC curves by analyzing the appearance, shift, or disappearance of the DSC peaks, especially the API melting peak, and/or variations in the expected enthalpy (∆H) values. It was assumed that interactions occurred when either a decrease or an increase in ∆H was observed in the case of overlapping. Modifications in the peak shape, peak onset, or maximum temperature peak may also indicate the existence of an interaction. However, it must occur in mind that a broadening of the peaks occurs as a result of a low purity of each component in the mixture and may not necessarily indicate potential incompatibility [33]. Variations in the enthalpy values for binary mixtures can be attributed to heterogeneity in the small samples used for the experiments (3–4 mg) [21].
Thermal events obtained by DSC of tobramycin and excipient in simple and binary systems are presented in Tables 1 and 2.
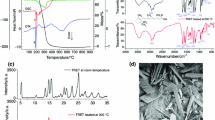
The DSC curve of tobramycin showed three endothermic peaks at 115.64, 176.70, and ~ 230 °C, and one exothermic peak at 206.94 °C. The thermal events in Fig. 1 are labeled 1–4 and correspond to: first endothermic peak (1), which can be attributed to dehydration of tobramycin monohydrate base to a metastable anhydrous polymorph; second endothermic peak (2), which can be attributed to the melting of the metastable form of tobramycin; and an exothermic peak (3), which corresponds to the crystallization of the stable anhydrous form before melting [34]. The DSC curve of tobramycin showed a sharp endotherm peak (4) at 235.69 °C due to the API melting, which presented an associated enthalpy of − 63.90 J g−1. In the 1:1 physical mixtures, in the absence of any interaction between tobramycin and excipient, the Tpeak values of the melting curve and the Tonset values are very similar to those corresponding to the API alone. In this case, the thermal profiles of tobramycin and the mixture with adequate excipients are superimposed.
In DSC curves of sodium chloride and sodium sulfate, no peak was observed in the temperature range of 40–270 °C. When tobramycin was mixed either with sodium chloride or sodium sulfate, the peaks corresponding to tobramycin were the same as those corresponding to the API alone. The DSC curves of tobramycin and sodium chloride are shown in Fig. 2.
The DSC curve corresponding to dibasic sodium phosphate showed an endothermic peak at 90.56 °C (corresponding to the loss of water). In the DSC curve of tobramycin and dibasic sodium phosphate, all peaks were observed.
In the case of tyloxapol, no peak was observed in the temperature range of 40–270 °C, while in the curve corresponding to the mixture, all the tobramycin peaks were observed, with the melting endotherm at 234.77 °C.
Sodium hyaluronate presented an exothermic peak at 239.90 °C due to thermal decomposition [35], while the tobramycin–sodium hyaluronate mixture presented an endothermic peak at a lower temperature (230.57 °C) and an exothermic peak at 238.55 °C. The enthalpy value obtained was the average of both substances (Fig. 3).
The DSC curve corresponding to benzalkonium chloride presented an endothermic peak at 47.78 °C, which corresponded to the melting point. The tobramycin–benzalkonium chloride mixture presented only one peak at 42.06 °C corresponding to benzalkonium chloride and no tobramycin peak was observed.
Two endothermic peaks at 151.77 and 171.74 °C were observed for boric acid, the second corresponding to the melting point. The mixture of tobramycin and boric acid presented a shift in the boric acid peaks toward a lower temperature (147.06 and 168.63 °C). The melting endotherm for tobramycin was retained in the curves obtained for the tobramycin-boric acid (233.57 °C) mixture, with a significant reduction in the enthalpy value.
Potassium sorbate displayed an endothermic peak at 160.59 °C (corresponding to the melting point) [36]. In the mixture, the potassium sorbate peak was observed, while the tobramycin melting peak shifted toward a lower temperature (226.25 °C), with a significant reduction in the enthalpy value.
Monobasic sodium phosphate presented three endothermic peaks: 77.46, 123.95, and 212.09 °C, which corresponded to compound dehydration [37]. In the mixture, monobasic sodium phosphate displayed the dehydration peaks, and the tobramycin melting peak was observed together with a significant reduction in the enthalpy value.
The curve corresponding to edetate disodium presented an endothermic peak at 252.68 °C, which corresponded to the melting point with thermal decomposition. In the mixture, the peak of edetate disodium is split, and the melting peak of tobramycin shifted toward a lower temperature (233.27 °C), with a significant reduction in the enthalpy value.
Sodium metabisulfite presented an endothermic peak at 212.98 °C, which corresponded to thermal decomposition. In the curves corresponding to the mixture of tobramycin and sodium metabisulfite, the peaks of sodium metabisulfite shifted toward a lower temperature (209.68 °C). The melting endotherm of tobramycin shifted toward 230.49 °C, with a significant reduction in the enthalpy value.
Thimerosal presented an endothermic peak at 232.16 °C, which corresponded to the melting point. The DSC curve of tobramycin–thimerosal mixture presented a shift of the tobramycin melting peak toward a lower temperature (215.32 °C), with a significant reduction in the enthalpy value (Fig. 4).
The appreciable decrease in the melting temperature and its corresponding fusion enthalpy values suggest the occurrence of a process taking place with low intensity or even the melting endotherms disappears. (This is the case of the binary tobramycin–thimerosal mixture.) The difference in enthalpy for the binary mixtures of tobramycin with benzalkonium chloride, boric acid, potassium sorbate, monobasic sodium phosphate, edetate disodium, sodium metabisulfite, and thimerosal suggest the existence of a physical interaction which does not determine an incompatibility.
Isothermal stress testing: HPLC
All the excipients were tested by IST. Quantitative results are shown in Table 3. As it can be observed in the table, important changes occur in the API content after storage of the active principle–excipient blends under stress conditions. Such is the case of benzalkonium chloride, sodium hyaluronate, boric acid, potassium sorbate, monobasic sodium phosphate, edetate disodium, tyloxapol, and thimerosal.
Powder X-ray diffraction (PXRD)
PXRD is a useful method for fast identification of new crystalline phases in the solid state. The pure tobramycin presented the characteristic diffraction peaks at 2θ of 17.7, 18.3, 18.8, indicating the presence of a crystalline structure [38, 39]. The same diffraction peaks were observed for 1:1 binary mixtures of tobramycin and the excipients, thus demonstrating that no significant changes took place in the physical binary mixtures with respect to the chemical structure of the active component (Fig. 5). The PXRD analysis of the physical mixture of tobramycin and sodium hyaluronate presented a decrease in crystallinity due to the presence of an amorphous excipient (Fig. 6). On the other hand, when tobramycin was mixed with thimerosal, only the characteristic peak of 17.7 was observed (Fig. 7). An PXRD analysis of the tobramycin–tyloxapol mixture was not possible due to the liquid nature of the excipient.
Isothermal stress testing–FTIR
The Fourier transform infrared spectroscopy (FTIR) spectrum of pure tobramycin displayed bands at 3400–3200 cm−1 due to the N–H or the O–H stretching, bands at 2921–2899 cm−1 due to the C–H stretching, a band at 1576–1598 cm−1 due to N–H bending, a typical band at 1461 cm−1 due to CH2 scissoring, bands at 1349–1380 cm−1 due to O–H in-plane bending vibration and a band at 1032 cm−1 due to C–N or C–O stretching [39]. The FTIR spectra of tobramycin revealed no changes after API exposure at 40 °C, 75% RH during 4 days neither with nor without the addition of water.
Binary mixtures of tobramycin and sodium sulfate, sodium chloride (Fig. 8), tyloxapol, dibasic sodium phosphate, or sodium hyaluronate (Fig. 9) rendered the characteristic bands corresponding to tobramycin alone kept under each condition. These results suggest that tobramycin remains unaltered in these blends.
DSC studies indicated that the changes observed in the FTIR spectra of binary blends of tobramycin and some of the excipients (Fig. 10) are suggestive of a possible interaction between the mixture components, in agreement with the thermal analysis findings (Table 4).
Based on the DSC results alone, an interaction was suspected between tobramycin and benzalkonium chloride, boric acid, potassium sorbate, monobasic sodium phosphate, edetate disodium, sodium metabisulfite, and thimerosal. These results were confirmed by the IST–FTIR studies.
The IST–HPLC analysis demonstrated a decrease in the recovery of tobramycin when this API was blended with sodium hyaluronate and the tyloxapol. This phenomenon might be attributed to the mucilaginous nature of both excipients. No incompatibilities between tobramycin and tyloxapol were detected when methodologies other than IST–HPLC were employed. In the case of PDRX, the physical mixture of tobramycin and sodium hyaluronate presents a decrease in crystallinity because of the mixture with an amorphous excipient.
Discrepancies between the results obtained with different methods assessing compatibility are frequently encountered [17]. Particularly, in this study, tobramycin was found to be incompatible with sodium metabisulfite when DSC and IST–FTIR were employed, while incompatibilities were detected in this blend by neither IST–HPLC nor PDRX. The presence of high temperatures and humidity could explain the results obtained by DSC and IST–FTIR. The addition of water into the vial mimics the manufacturing conditions of tobramycin eye drops. It is known that the presence of water in the formulation favors the degradation reactions.
The excipients that proved to be incompatible with tobramycin also display incompatibility with other compounds containing amino or hydroxyl functional groups. Sodium metabisulfite is a strong nucleophilic antioxidant capable of catalyzing drug degradation [40]. In water, sodium metabisulfite is immediately converted to sodium and bisulfite ions. Sodium metabisulfite reacts with either ortho- or para-hydroxybenzyl alcohol derivatives to form sulfonic acid derivatives with little or no pharmacological activity [41]. The sulfite ion is a more efficient catalyst than phosphate salts [42]. Edetate salts are incompatible with amphotericin [43]. It is known that thimerosal forms precipitates with many alkaloids [44]. Kamin et al. [45] have reported that cromolyn and colistin are incompatible with benzalkonium chloride. Boric acid gives exothermic reactions with amines [46]. Sorbic acid and its salts have a conjugated double-bond system which can undergo nucleophilic addition reactions. In fact, Ferrand et al. [47] have described the interaction between sorbic acid and amine groups.
Conclusions
This study also demonstrates that DSC and IST–FTIR can detect potential incompatibilities between an API and pharmaceutical excipients. The use of DSC has been proposed as a rapid method for evaluating the physicochemical interactions between two components. The IST–FTIR provides information on the main absorption bands, mainly those corresponding to the API. Any changes detected in these bands may account for degradation processes taking place in the sample. The information provided by these methodologies is critical in preformulation studies. In summary, this study, which is in line with a previous work carried out in our laboratory [31], demonstrates that tobramycin is incompatible with benzalkonium chloride, boric acid, potassium sorbate, monobasic sodium phosphate, edetate disodium, sodium metabisulfite, and thimerosal.
References
Bharate SS, Bharate SB, Bajaj AN. Interactions and incompatibilities of pharmaceutical excipients with active pharmaceutical ingredients: a comprehensive review. J Excip Food Chem. 2010;1:3–26.
Moyano MA, Broussalis AM, Segall AI. Thermal analysis of lipoic acid and evaluation of the compatibility with excipients. J Therm Anal Calorim. 2010;99:631–7.
Ceresole R, Han Y, Rosasco MA, Orelli LR, Segall AI. Drug–excipient compatibility studies in binary mixtures of Avobenzone. J Cosmet Sci. 2013;64:317–28.
Chadha R, Bhandari S. Drug–excipient compatibility screening—role of thermoanalytical and spectroscopic techniques. J Pharm Biomed Anal. 2014;87:82–97.
McDaid FM, Barker SA, Fitzpatrick S, Petts CR, Craig DQM. Further investigations into the use of high sensitivity differential scanning calorimetry as a means of predicting drug–excipient interactions. Int J Pharm. 2003;252:235–40.
O’Neill MA, Gaisford S. Application and use of isothermal calorimetry in pharmaceutical development. Int J Pharm. 2011;417:83–93.
Ferraz Pinto M, Afonso de Moura E, Santos de Souza F, Oliveira Macêdo R. Thermal compatibility studies of nitroimidazoles and excipients. J Therm Anal Calorim. 2010;102:323–9.
Oliveira Santos AF, Basilio ID Jr, Souza FS, Medeiros FD, Ferraz Pinto M, de Santana DP, Macêdo RO. Application of thermal analysis of binary mixtures with metformin. J Therm Anal Calorim. 2008;93:361–4.
Chou YP, Huang JY, Tseng JM, Cheng SY, Shu CM. Reaction hazard analysis for the thermal decomposition of cumene hydroperoxide in the presence of sodium hydroxide. J Therm Anal Calorim. 2008;93:275–80.
Sashima ES, Janowska G, Zaborski M, Vnuchkin AV. Compatibility of fibroin/chitosan and fibroin/cellulose blends by thermal analysis. J Therm Anal Calorim. 2007;89:887–91.
Medeiros AFD, Santos AFO, de Souza FS, Jùnior IDB, Valdilânio J, Procópio JVV, de Santana DP, Macêdo RO. Thermal studies of pre-formulates of metronidazole obtained by spray drying technique. J Therm Anal Calorim. 2007;89:775–81.
Silva MAS, Kelmann RG, Foppa T, Cruz AP, Bertol CD, Sartori T, Granada A, Carmignan F, Murakami FS. Thermoanalytical study of fluoxetine hydrochloride. J Therm Anal Calorim. 2007;87:463–7.
Lira AM, Araújo AAS, Basílio IDJ, Santos BLL, Santana DP, Macedo RO. Compatibility studies of lapachol with pharmaceutical excipients for the development of topical formulations. Thermochim Acta. 2007;457:1–6.
Mura P, Furlanetto S, Cirri M, Maestrelli F, Marras AM, Pinzauti S. Optimization of glibenclamide tablet composition through the combined use of differential scanning calorimetry and d-optimal mixture experimental design. J Pharm Biomed Anal. 2005;37:65–71.
Araújo AAS, Storpirtis S, Mercuri LP, Carvalho FMS, dos Santos Filho M, Matos JR. Thermal analysis of the antirretroviral zidovudine (AZT) and evaluation of the compatibility with excipients used in solid dosage forms. Int J Pharm. 2003;260:303–14.
Matos APS, Costa JS, Boniatti J, Seiceira RC, Pitaluga A, Oliveira DL, Vicosa AL, Holandino C. Compatibility study between diazepam and tablet excipients. J Therm Anal Calorim. 2017;127:1675–82.
Liltorp K, Larsen TG, Willumsen B, Holm R. Solid state compatibility studies with tablet excipients using non thermal methods. J Pharm Biomed Anal. 2011;55:424–8.
Monajjemzadeh F, Hassanzadeh D, Valizadeh H, Siahi-Shadbad MR, Mojarrad JS, Robertson TA, Roberts MS. Compatibility studies of acyclovir and lactose in physical mixtures and commercial tablets. Eur J Pharm Biopharm. 2009;73:404–13.
Verma RK, Garg S. Selection of excipients for extended release formulations of glipizide through drug–excipient compatibility testing. J Pharm Biomed Anal. 2005;38:633–44.
da Silva EP, Pereira MAV, de Barros Lima IP, Pereira Barros Lima NG, Guimarães Barbosa E, Soares Aragão CF, Barreto Gomes AP. Compatibility study between atorvastatin and excipients using DSC and FTIR. J Therm Anal Calorim. 2016;123:933–9.
Verma RK, Garg S. Compatibility studies between isosorbide mononitrate and selected excipients used in the development of extended release formulations. J Pharm Biomed Anal. 2004;35:449–58.
Stulzer HK, Rodrigues PO, Cardoso TM, Matos JSR, Silva MAS. Compatibility studies between captopril and pharmaceutical excipients used in tablets formulations. J Therm Anal Calorim. 2008;91:323–8.
Silva LAD, Teixeira FV, Serpa RC, Esteves NL, dos Santos RR, Lima EM, da Cunha-Filho MSS, de Souza Araújo AA, Taveira SF, Marreto RN. Evaluation of carvedilol compatibility with lipid excipients for the development of lipid-based drug delivery systems. J Therm Anal Calorim. 2016;123:2337–44.
Veiga A, Oliveira PR, Bernardi LS, Mendes C, Silva MAS, Sangoi MS, Janissek PR, Murakami FS. Solid-state compatibility studies of a drug without melting point. J Therm Anal Calorim. 2017. https://doi.org/10.1007/s10973-017-6756-8.
Rus LM, Tomuta I, Iuga C, Maier C, Kacso I, Borodi G, Bratu I, Bojita M. Compatibility studies of indapamide/pharmaceutical excipients used in tablet preformulation. Farmacia. 2012;60:92–101.
Tomassetti M, Catalani A, Rossi V, Vecchio S. Thermal analysis study of the interactions between acetaminophen and excipients in solid dosage forms and in some binary mixtures. J Pharm Biomed Anal. 2005;35:949–55.
Ding T, Chen L, Zhai LH, Fu Y, Wang-Sun B. Compatibility study of rivaroxaban and its pharmaceutical excipients. J Therm Anal Calorim. 2017;130:1569–73.
Pires SA, Mussel WN, Yoshida MI. Solid-state characterization and pharmaceutical compatibility between citalopram and excipients using thermal and non-thermal techniques. J Therm Anal Calorim. 2017;127:535–42.
Hanko VP, Rohrer JS. Determination of tobramycin and impurities using high-performance anion exchange chromatography with integrated pulsed amperometric detection. J Pharm Biomed Anal. 2006;40:1006–12.
Manyanga V, Elkady E, Hoogmartens J, Adams E. Improved reversed phase liquid chromatographic method with pulsed electrochemical detection for tobramycin in bulk and pharmaceutical formulation. J Pharm Anal. 2013;3:161–7.
Rosasco MA, Segall AI. Determination of the chemical stability of various formulations of tobramycin eye-drops by HPLC method and data analysis by R-GUI stability software. J Appl Pharm Sci. 2015;5:8–13.
The United States Pharmacopeia 38th Ed. (Spanish version) U.S. Pharmacopeial Convention, Rockville; 2015. p. 6020–21.
Tita B, Fulias A, Bandurb G, Marianc E, Tita E. Compatibility study between ketoprofen and pharmaceutical excipients used in solid dosage forms. J Pharm Biomed Anal. 2011;56:221–7.
Zhu B, Padroni M, Colombo G, Phillips G, Crapper J, Young PM, Traini D. The development of a single-use, capsule-free multi-breath tobramycin dry powder inhaler for the treatment of cystic fibrosis. Int J Pharm. 2016;514:392–8.
Benešová K, Pekař M, Lapčík L, Kučerík J. Stability evaluation of n-alkyl hyaluronic acid derivates by DSC and TG measurement. J Therm Anal Calorim. 2006;83:341–8.
Baldino L, Cardea S, Reverchon E. Production of antimicrobial membranes loaded with potassium sorbate using a supercritical phase separation process. Innov Food Sci Emerg. 2016;34:77–85.
de Jager HJ, Prinsloo LC. The dehydration of phosphates monitored DSC/TGA and in situ Raman spectroscopy. Thermochim Acta. 2001;376:187–96.
Dash AK, Suryanarayanan R. Solid-state properties of Tobramycin. Pharmaceut Res. 1991;8:1159–65.
Dash AK. Tobramycin. In: Brittain H, editor. Analytical profiles of drug substances and excipients, vol. 24. San Diego: Academic Press; 1996. p. 579–613.
Munson JW, Hussain A, Bilous R. Precautionary note for use of bisulfite in pharmaceutical formulations. J Pharm Sci. 1977;66:1775–6.
Rowe RC, Sheskey PJ, Quinn ME, editors. Handbook of pharmaceutical excipients. 6th ed. London: Pharmaceutical Press; 2009. p. 654–6.
Akers MJ. Excipient–drug interactions in parenteral formulations. J Pharm Sci. 2002;91:2283–300.
Rowe RC, Sheskey PJ, Quinn ME, editors. Handbook of pharmaceutical excipients. 6th ed. London: Pharmaceutical Press; 2009. p. 242–4.
Martindale, The Complete Drug reference, 32th edn. Pharmaceutical Press, London; 1999. p. 1126.
Kamin W, Schwabe A, Krämer I. Inhalation solutions—which one are allowed to be mixed? Physico-chemical compatibility of drug solutions in nebulizers. J Cyst Fibros. 2006;5:2015–213.
Pohanish RP, Greene SA. Wiley guides to chemical incompatibilities. 3rd ed. Hoboken: Wiley; 2009.
Ferrand C, Marc F, Fritsch P, De Saint Blanquat G. Interactions of sorbic acid and sorbates with food amines: role of light, oxygen, temperature and the presence of glycerol and emulsifier. Sci Aliments. 1998;18:603–16.
Acknowledgements
This work was supported by Grant 20020130100342BA from UBA to A. I. Segall.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosasco, M.A., Bonafede, S.L., Faudone, S.N. et al. Compatibility study of tobramycin and pharmaceutical excipients using differential scanning calorimetry, FTIR, DRX, and HPLC. J Therm Anal Calorim 134, 1929–1941 (2018). https://doi.org/10.1007/s10973-018-7282-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-018-7282-z