Abstract
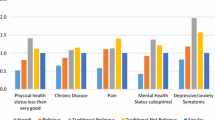
Numerous studies have identified religious correlates of health indicators, but relatively few have been conducted among Jewish populations in Israel or the diaspora. This study investigates the possibility of a religious gradient in physical and mental health and well-being across the familiar categories of Jewish religious identity and observance in Israel: hiloni (secular), masorti lo dati (traditional, non-religious), masorti (traditional), dati (religious or Orthodox), and charedi (ultra-Orthodox). Data are from Jewish respondents aged 18 and over (N = 2916) from the Israeli sample of the new, 22-nation Global Flourishing Study, which used stratified, probability-based sampling and assessed demographic, socioeconomic, political, religious, health-related, and other variables. This analysis investigated religious differences in nine indicators of physical and mental health and well-being among Israeli Jews. Using a strategy of one-way ANOVA and ANCOVA, adjusting for complex sampling design components, a statistically significant “dose-response”-like gradient was found for eight of the outcome measures, validated by additional multiple comparison tests. For four “positively” worded indicators (physical and mental health, happiness, and life satisfaction), scores increased consistently from the hiloni to the charedi categories. For four of five “negatively” worded indicators (bodily pain, depression, anxiety, and suffering), scores decreased across the same categories. Results withstood adjusting for effects of age, sex, education, marital status, urbanicity, income, and nativity (whether born in Israel). Among Israeli Jews, greater religiousness was associated with higher levels of health and well-being and lower levels of somatic and psychological distress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many determinants have been observed to drive population health disparities, including socioeconomic status, access to medical care, and various behavioral risk factors (Braverman, 2023). Often overlooked is the substantial, if not fully understood, body of empirical research findings on religious correlates and determinants of health, illness, and morbidity, both physical and mental (Koenig et al., 2024). Thousands of studies have identified lower rates of many chronic and acute conditions and higher rates of health and well-being by religiousness, across religions, nations, and social and demographic groups, dating back decades (Levin, 2018). Most have been conducted among Christians or in the general population, so the extent to which such findings apply to Jews is inconclusive. Research has been relatively sparse among Jewish populations, in both Israel and the Jewish diaspora, although existing findings are suggestive of an association (Levin, 2013).
Such an association, if validated, may be of potential relevance to epidemiologists, health services researchers, and healthcare policymakers. In Israel, especially, it has been noted that “a person’s affiliation on the religious-secular continuum is increasingly recognized in the research literature as the most accurate predictor on a broad range of topical issues” (Cohen, 2021, p. 165), including political identity, public policy stances, marital and family relations, use of mental health services, prosocial behavior, military service, and other outcomes. Research in Israel, the U.S., and elsewhere since the 1990s suggests that levels of Jewish observance may also influence rates of morbidity, both physical (Levin, 2012a; Shmueli, 2007) and mental (Pirutinsky & Rosmarin, 2022; Rosmarin et al., 2009a, 2009b), and even mortality (Kark et al., 1996), such that greater observance is associated with greater well-being and longevity, depending upon the particular health indicators being examined as well as the specific populations under study.
Interestingly, there is some evidence for a religious gradient here—akin to a “dose-response” relationship (Porta, 2014, p. 83)—when it comes to Jewish observance (Levin, 2011), although this metaphor is invoked here cautiously. Still, a considerable number of pasukim (verses) in the Torah describe certain religious beliefs and practices as consequential for health (Preuss, 1993), and the chazal (rabbinic sages) and later rabbis devoted considerable attention to the possible health impact of fidelity to halachah (Jewish law), a notable example being the Rambam (Bar-Sela et al., 1964). While such a perspective may be challenging for some secular physicians and health scientists, authoritative rabbinic interpretations of Jewish religious tenets inform the derivation of Jewish bioethical principles (Steinberg, 2001) and thus the decision-making calculus and actions of religious Jews when it comes to health-impacting behaviors (Feldman, 1986).
Longstanding research suggests that Jewish religious observance may influence physical health, or at least perceptions of one’s health, both overall (Levin, 2015) and in terms of specific symptoms such as pain (Mechanic, 1963), perhaps through providing psychosocial resources for positive religious coping (Pargament, 2001). There is also some evidence that religious Jews tend to experience less depression (Pirutinsky & Rosmarin, 2018) and anxiety (Rosmarin et al., 2009a, 2009b) than the non-religious, findings consistent with decades of research among non-Jews (Koenig, 2018). This may indicate a protective effect of religiousness, epidemiologically speaking, such as through “the regulative and integrative function of belonging to a religious community” (Anson et al., 1991, p. 119). Alternatively, Jewish beliefs and practices may provide a lens to reinterpret one’s suffering in a way that reframes and perhaps lessens its psychological impact (Heilman & Witztum, 2000). As well, there may be a stigma among the most religious Jews which could lead to an underreporting of psychological symptoms (Baruch et al., 2014; Pirutinsky & Rosmarin, 2022) compared to liberal or secular Jews. Finally, additional research among both Israeli and diaspora Jews has identified religious correlates of affective and cognitive markers of general well-being, such as happiness and life satisfaction (Levin, 2012b), again perhaps operating through “a strong sense of belonging to a community [which] enables individuals to prioritize more hedonic aspects of their lives” (Russo-Netzer & Bergman, 2020, p. 233).
The present study was encouraged by an unprecedented opportunity to validate these observations using data from the brand new Global Flourishing Study (GFS), a 22-nation, multiwave population survey which includes demographic, social, economic, political, religious, personality, childhood, community, health- and well-being-related, and character-based measures (Johnson & VanderWeele, 2022). In some nations, the sample size is as great as 10,000 respondents. The GFS is one of the largest and most expensive global studies of its type ever conducted, and it serendipitously contains a large, nationally representative population sample of Israeli adults and assessment of physical and mental health and Jewish religious identity and observance, among other religious variables (Johnson et al., 2023). This sample enables examination of Jewish religious differences in multiple physical and mental health indicators, as well as validation of a possible Jewish religious gradient in these outcomes.
Method
The Global Flourishing Study
As noted, the GFS is a multinational, household population survey of adults aged 18 or over which includes an Israeli sample. It is a joint project of Baylor University and Harvard University, in conjunction with the Gallup Organization which, at present, has collected the first of five annual waves of panel data. Sampling and data collection methodology varied across countries, including probability- and non-probability-based samples, with and without random digit dialing, and various forms of interviewing (Ritter et al., 2023). The GFS is administered in partnership with the Center for Open Science, which is overseeing data access to the project’s nearly 50 investigators. One year after each wave of data collection is completed, the previous wave’s data will become publicly accessible. This will become a great resource for the scientific community, enabling investigation of both within-country and between-country patterns of and associations among numerous well-being-related measures (Case et al., 2023).
The Israeli survey used a stratified, probability-based sampling design (N = 3669), with data collected through Computer-Assisted Personal Interviews in Hebrew or Arabic, utilizing a professionally translated and piloted questionnaire. It had an AAPOR Response Rate 3 of 66.6% for the final sample. Fieldwork was conducted from November 7, 2022, to November 23, 2023. The analyses reported below account for complex survey design components including weight, primary sampling unit (PSU), and strata variables provided by Gallup. Analyses were restricted to self-identified Jewish respondents (N = 2958, or 80.62% of the sample) (Ritter et al., 2023) who were asked about the Israel-specific Jewish religious category or tradition with which they identify. Of these, factoring out nonresponses, out of a total of 2916 respondents, 1220 (41.8%) identified as hiloni (secular), 564 (19.3%) as masorti lo dati (traditional, non-religious), 308 (10.6%) as masorti (traditional), 403 (13.8%) as dati (religious or Orthodox), and 421 (14.4%) as charedi (ultra-Orthodox). These five categories are an expansion of the familiar four-category taxonomy used to classify Israeli Jews in national data collection efforts, such as the Israel Social Survey and other studies (Cooperman et al., 2016). In contrast to how religiously practicing Jews are classified in North America (e.g., Reform, Reconstructionist, Conservative, Orthodox, etc.), these categories are not denominations or movements, strictly speaking, but rather labels or clusters which have religious as well as social and cultural significance (Zuckerman, 1996).
Measures
Nine single-item indicators are investigated in the present study. These include physical health and mental health (both assessed by a self-rating ladder scale coded: 0 = poor health to 10 = excellent health), presence of health problems that restrict activity (coded: 0 = no, 1 = yes), bodily pain during the past 4 weeks (coded: 1 = none at all, 2 = not very much, 3 = some, 4 = a lot), feelings of depression and anxiety in the last 2 weeks (both coded: 1 = not at all, 2 = several days, 3 = more than half the days, 4 = nearly every day), any type of physical or mental suffering (coded: 1 = not at all, 2 = not very much, 3 = some, 4 = a lot), happiness (a self-rating ladder coded: 0 = extremely unhappy to 10 = extremely happy), and life satisfaction (a self-rating ladder coded: 0 = not all satisfied with your life to 10 = completely satisfied with your life).
Analyses adjust for effects of several known sociodemographic correlates of physical and/or mental health. These are age (in years), sex (coded: 0 = male, 1 = female), education (9 categories coded: 0 = no formal education to 8 = Ph.D.), marital status (6 categories collapsed to: 0 = not married, 1 = married), urbanicity (coded: 1 = a rural area or on a farm, 2 = a small town or village, 3 = a suburb of a large city, 4 = a large city), nativity (coded: 0 = born in another country, 1 = born in Israel), and income (an assessment of feelings about household income, coded: 1 = finding it very difficult on present income, 2 = finding it difficult on present income, 3 = getting by on present income, 4 = living comfortably on present income). This latter measure was used in lieu of the survey’s more standard monthly household income variable due to numerous missing values that would have lowered the available sample size considerably.
Data Analysis
Descriptive statistics for the study’s health and well-being indicators and sociodemographic covariates include means, standard deviations, and Pearson (r) correlations as calculated using Stata 18. These analyses partial out (i.e., adjust for effects of) three complex sampling design variables (accounting for annual nation-specific weight, PSU, and sampling strata), which by default requires listwise deletion of missing values (N = 2801).
Differences in health and well-being across Jewish categories are analyzed through a strategy of one-way ANOVA (bivariate) and ANCOVA (multivariable) analyses conducted separately for each outcome variable, again using Stata 18. The ANCOVAs adjust for effects of the sociodemographic covariates (age, sex, education, marital status, urbanicity, nativity, and income). Both sets of analyses also adjust for effects of the three sample weighting variables. The F-test and P-value results reported in Table 2 are based on the “Type III” solution, which is calculated adjusting for effects of all other variables in a respective model (Littell et al., 2002). Additionally, multiple comparison tests are run to identify any statistically significant differences among each pair of the five respective religious categories, not just overall across all of them. There are many types of such tests (Midway et al., 2020), and the present analyses are run with a Bonferroni correction (Abdi, 2007), which uses a corrected p-value of 0.005 (i.e., 0.05/10, for the ten different comparisons among the five religious categories for each dependent variable), an appropriate choice for this type of analysis (VanderWeele & Mathur, 2019). Due to missing values, N’s vary modestly across outcome variables (from 2808 to 2824).
Results
The results in Table 1 present descriptive statistics for all of the outcome and sociodemographic variables, as well as the correlations among them. There is much more to report than can be summarized here in the text. However, among the most interesting findings are that self-rated physical health is higher among younger, male, urban, higher-income, and native-born respondents; while, self-rated mental health is higher among the same groups plus married individuals. Depression and anxiety are higher among older, female, unmarried, non-urban, lower-income, and non-native respondents. Happiness and life satisfaction are higher among younger, male, married, urban, higher-income, and native-born respondents.
Differences in physical and mental health and well-being across categories of Jewish identity and observance show a consistent gradient for eight of the nine indicators such that identifying with a category characterized by greater religiousness is associated with greater health and well-being and less illness and distress (see Table 2). For the four “positively” worded indicators (physical and mental health, happiness, and life satisfaction), scores increase from the hiloni to the charedi categories. For four of the five “negatively” worded indicators (bodily pain, depression, anxiety, and suffering), scores decrease across the same categories. Only for health problems is there no consistent gradient, although results nonetheless point to a statistically significant difference across categories. Further, adjusting for effects of well-known sociodemographic correlates of these outcomes does not eliminate the statistical significance of these findings. Finally, results of multiple comparisons tests (see Table 2 footnote) underscore the presence of a health-promoting gradient from the least religious (hilonim) to the most religious (charedim) respondents for eight of the nine outcome variables.
Discussion
As anticipated, based on prior research on Jewish and other populations, a generally salutary association is observed between the five categories of religious identity and observance and several indicators of health and well-being among Israeli Jews. Besides the ability to validate this observation using a nationally representative population sample, what the present findings show are the uniformity of such an association regardless of the indicators examined as well as the consistency of this association in almost a “dose-response” fashion across the five religious categories used for Israeli Jews. Based on these results, which mostly confirm and elaborate on those of earlier studies using smaller samples and a more limited set of outcomes, positive findings among Israeli Jews can be safely (if cautiously) read into the ongoing empirical research literature on religion and health.
Limitations
A few study limitations can be identified, but we do not believe that they significantly diminish the value of these findings. These include issues related to study design, measurement, and data collection.
First, an important limitation is the use of a prevalence survey (i.e., cross sectional) design and reliance on single-item outcome measures. As with all prevalence surveys, this design feature limits attribution of positive findings to etiologic or other causal mechanisms, and inhibits accurate estimation of risk or odds (Lash & Rothman, 2021). This concern, however, generally does not come into play in a prevalence survey, as the intention is not to estimate associations but to document the magnitude of “caseness” in a population for respective disease or health outcomes at one point in time (point prevalence) or over a period of time (period prevalence) (Habibzadeh & Habibzadeh, 2020). In this instance, the first wave of the GFS data simply served to identify cases of the outcomes under study roughly during the year of 2023.
Regardless, this putative limitation is countered in the present study with significant advantages: use of a nationally representative probability-based sample of the adult Israeli population; a large sample totaling nearly 3000 Jewish respondents; and the potential to compare findings, on health and other constructs, to data from the other 21 countries surveyed in the GFS. Because the GFS will eventually consist of five waves of panel data, the present findings can also serve as a baseline that may be validated longitudinally and prospectively. Through epidemiologic methods there thus will be an opportunity to estimate true risk or odds, not solely prevalence-based associations, as well as to map trajectories of physical and mental health and well-being in the Israeli population over time stratified by any of the other socioeconomic, behavioral, psychosocial, and religious measures in the study. This alone promises to be a major contribution to population-health research in Israel.
Second, there is a lack of conceptual specificity in certain indicators due to their wording. For example, one of the health indicators assesses “health problems that restrict activity,” and it is measured on a binary (yes/no) metric. There is no probe, however, to identify what such health problems are, although the main target of what is assessed is specifically whether such problems restrict activity. In that sense, this variable is roughly equivalent to a standard, single-item, self-report indicator of activity limitation or overall disability or what is sometimes termed functional health (Haley & Andel, 2010).
Third, as data collection took place in Israel through November 23, 2023, the study was thus still in the field following the October 7th terrorist attacks. No data are available on whether or how either the response rate or actual responses to questions (e.g., on mental health) in this study differed among respondents sampled before and after the attacks, although there is evidence from other research that reports of psychopathology were elevated among some Israelis post-attack, but not primarily Israeli Jews (Groweiss et al., 2024). Regarding the present study, as these events occurred at the tail end of the first year’s wave of data collection, 11 months in, we do not believe that this would have appreciably impacted on the overall findings from the entire sample reported in these analyses. To be clear, however, this is conjecture; there is no way to know for certain. Perhaps something here may be deduced when comparing these findings to those from the subsequent waves of data.
Implications
The magnitude and consistency of these findings suggest some useful applications. First, they may provide helpful information on Jewish religion for healthcare planners and policymakers in Israel (Halevy & Halevy, 2015). The distribution and utilization of health and mental health services varies by religious subgroups, including among Jews, an observation first made decades ago in the U.S. in the famous Midtown Manhattan Study (Srole & Langner, 1962).Some evidence exists of disparities in healthcare use in Israel by ethnic origin and religion (Clarfield et al., 2017), although this has not been as widely studied or documented.
Second, these findings can inform the work of clinicians, especially mental health providers who treat religious Jews (Loewenthal, 2006). The gradient observed here, reinforced by the consistent findings of the multiple comparison tests, may provide insights that better direct clinical and pastoral resources to particular individuals and geographical enclaves where they can have the greatest impact. The needs of charedi patients, especially, may differ from those of other Jews and thus require special sensitivity (Stolovy et al., 2013), although, at least according to the present study, they appear to be doing very well compared to other Israeli Jews.
Third, observation of a religious gradient, and its direction, may challenge prevailing perceptions about the psychological status and quality of life of religious Jews and those whose lives are organized around strict observance of religious rituals (Dein & Loewenthal, 2013). Social and behavioral scientists in Israel and the diaspora may have jaundiced views about mental health and well-being among datim and charedim, and among religious patients or clients in general, based on secular perspectives that, historically, have tended to dominate the psychiatry and the mental health professions (Nissen et al., 2018). There is evidence that this is less the case today than it has been in the past (Curlin et al., 2007), so, also taking into account the present findings, these tacit views about mental health among very religious patients may require some updating.
Fourth, Israeli demographers may find these results instructive for understanding the complex and dynamic relationships over time among religion, population age structure, economic development, and population health (Deaton, 2011). A study using data from the 2004 Israel National Health Survey found the association between religiousness and physical and mental health among Israeli Jews to be U-shaped—that is, better among hilonim and charedim and worse among those in the middle (Brammli-Greenberg et al., 2018), a finding also observed in a 2005 analysis of self-reported mental health in a sample of Jewish Israeli students (Vilchinsky & Kravetz, 2005). The present findings suggest that the situation has since evolved, such that health and well-being increase consistently as one moves “rightward” on the religious spectrum. As the most religious Jews also exhibit the highest total fertility rate (Stone, 2023)—i.e., the average number of live births per woman over her lifetime—it will be interesting to observe how demographic changes over the next couple generations impact on the health of the Israeli population.
Conclusion
Findings from the nationally representative Israeli sample of the population-based Global Flourishing Study point to a consistent religious gradient in multiple indicators of physical and mental health and well-being. The greater the level of one’s Jewish religious observance, according to self-reported religious identity, the higher the ratings of “positive” indicators (physical health, mental health, happiness, life satisfaction) and the lower the ratings of “negative” indicators (health problems, bodily pain, depression, anxiety, suffering). These findings have implications for policymakers, clinicians, social scientists, and demographers in Israel.
Data Availability
The data that support the findings of this study are available from the Gallup Organization, but restrictions apply such that they will become publicly available one year after the initial release of each wave of data collection. For the first wave of the GFS will this occur in 2025. Information related to the GFS as well as the official citation can be found at https://doi.org/10.17605/OSF.IO/3JTZ8.
References
Abdi, H. (2007). Bonferroni and Šidák corrections for multiple comparisons. In N. Salkind (Ed.), Encyclopedia of measurement and statistics (pp. 103–107). Sage Publications.
Anson, O., Levenson, A., Maoz, B., & Bonneh, D. Y. (1991). Religious community, individual religiosity, and health: A tale of two kibbutzim. Sociology, 25(1), 119–132. https://doi.org/10.1177/0038038591025001
Bar-Sela, A., Hoff, H. E., & Faris, E. (1964). Moses Maimonides’ Two Treatises on the Regimen of Health: Fī Tadbīr al-Sihhah and Maqālah fi Bayān Ba’d al-A’rād wa-al-Jawāb ’anhā. Transactions of the American Philosophical Society, 54(4), 3–50. https://doi.org/10.2307/1005935
Baruch, D. E., Kanter, J. W., Pirutinsky, S., Murphy, J., & Rosmarin, D. H. (2014). Depression stigma and treatment preferences among Orthodox and non-Orthodox Jews. Journal of Nervous and Mental Disease, 202(7), 556–561. https://doi.org/10.1097/NMD.0000000000000158
Brammli-Greenberg, S., Glazer, J., & Shapiro, E. (2018). The inverse U-shaped religion-health connection among Israeli Jews. Journal of Religion and Health, 57(2), 738–750. https://doi.org/10.1007/s10943-018-0577-3
Braverman, P. (2023). The social determinants of health and health disparities. Oxford University Press.
Case, B., Counted, V., Ritchie-Dunham, J., Cowden, R., Gibson, C., Koga, H., Lomas, T., & Padgett, N. (2023). Beyond a single story: The heterogeneity of human flourishing in 22 countries. International Journal of Wellbeing, 13(4), 3555. https://doi.org/10.5502/ijw.v13i4.3555
Clarfield, M. A., Manor, O., Bin Nun, G., Shvarts, S., Azzam, Z. S., Afek, A., Basis, F., & Israeli, A. (2017). Health and health care in Israel: An introduction. The Lancet, 389(10088), P2503–P2513. https://doi.org/10.1016/S0140-6736(17)30636-0
Cohen, A. (2021). Religion, society, and politics in Israel. In R. Y. Hazan, A. Dowty, M. Hofnung, & G. Rahat (Eds.), The Oxford handbook of Israeli politics and society (pp. 161–178). Oxford University Press.
Cooperman, A., Sahgal, N., & Schiller, A. (2016). Israel’s religiously divided society. Pew Research Center. https://www.pewresearch.org/religion/wp-content/uploads/sites/7/2016/03/Israel-Survey-Full-Report.pdf.
Curlin, F. A., Odell, S. V., Lawrence, R. E., Chin, M. H., Lantos, J. D., Meador, K. G., & Koenig, H. G. (2007). The relationship between psychiatry and religion among U.S. physicians. Psychiatric Services, 58(9), 1193–1198. https://doi.org/10.1176/ps.2007.58.9.1193
Deaton, A. S. (2011). Aging, religion, and health. In D. A. Wise (Ed.), Explorations in the economics of aging (pp. 237–262). University of Chicago Press.
Dein, S., & Loewenthal, K. M. (2013). The mental health benefits and costs of sabbath observance among Orthodox Jews. Journal of Religion and Health, 52(4), 1382–1390. https://doi.org/10.1007/s10943-013-9757-3
Feldman, D. M. (1986). Health and medicine in the Jewish tradition. Crossroad.
Groweiss, Y., Blank, C., Hamdan, S., Neria, Y., & Levi-Belz, Y. (2024). The mental health impact of the October 7th terror attack on Jews and Arabs in Israel: A nationwide prospective study. Psychiatry Research, 337, 115973. https://doi.org/10.1016/j.psychres.2024.115973
Habibzadeh, F., & Habibzadeh, P. (2020). The mean prevalence. Epidemiologic. Methods, 9(1), 20190033. https://doi.org/10.1515/em-2019-0033
Halevy, J., & Halevy, A. (2015). Jewish religious perspectives in the Israeli healthcare system. Studia Bioethica, 8(1), 25–29. https://riviste.upra.org/index.php/bioethica/article/view/3048/2261
Haley, C., & Andel, R. (2010). Correlates of physical activity participation in community-dwelling older adults. Journal of Aging and Physical Activity, 18(4), 375–389. https://doi.org/10.1123/japa.18.4.375
Heilman, S. C., & Witztum, E. (2000). All in faith: Religion as the idiom and means of coping with distress. Mental Health, Religion and Culture, 39(2), 115–124. https://doi.org/10.1080/713685606
Johnson, B. R., & VanderWeele, T. J. (2022). The Global Flourishing Study: A new era for the study of well-being. International Bulletin of Mission Research, 46(2), 272–275. https://doi.org/10.1177/23969393211068096
Johnson, K. A., Moon, J. W., VanderWeele, T. J., Schnitker, S., & Johnson, B. R. (2023). Assessing religion and spirituality in a cross-cultural sample: Development of religion and spirituality items for the Global Flourishing Study. Religion Brain and Behavior, 1–14. https://doi.org/10.1080/2153599X.2023.2217245
Kark, J. D., Shemi, G., Friedlander, Y., Martin, O., Manor, O., & Blondheim, S. H. (1996). Does religious observance promote health?: Mortality in secular vs religious kibbutzim in Israel. American Journal of Public Health, 86(3), 341–346. https://doi.org/10.2105/AJPH.86.3.341
Koenig, H. G. (2018). Religion and mental health: Research and clinical applications. Academic Press.
Koenig, H. G., VanderWeele, T. J., & Poteet, J. R. (2024). Handbook of religion and health (3rd ed.). Oxford University Press.
Lash, T. L., & Rothman, K. J. (2021). Measures of occurrence. In T. L. Lash, T. J. VanderWeele, S. Haneuse, & K. J. Rothman (Eds.), Modern epidemiology (4th ed., pp. 53–77). Wolters Kluwer.
Levin, J. (2011). Religion and psychological well-being and distress in Israeli Jews: Findings from the Gallup World Poll. Israel Journal of Psychiatry and Related Sciences, 48(4), 252–261.
Levin, J. (2012a). Religion and physical health among older Israeli Jews: Findings from the SHARE-Israel study. Israel Medical Association Journal, 14(10), 595–601.
Levin, J. (2012b). Religion and positive well-being among Israeli and diaspora Jews: Findings from the World Values Survey. Mental Health Religion and Culture, 15(7), 709–720. https://doi.org/10.1080/13674676.2011.617002
Levin, J. (2013). Population research on Judaism, health, and well-being. In J. Levin & M. F. Prince (Eds.), Judaism and health: A handbook of practical, professional and scholarly resources (pp. 282–297). Jewish Lights Publishing.
Levin, J. (2015). Religious differences in self-rated health among US Jews: Findings from five urban population surveys. Journal of Religion and Health, 54(2), 765–782. https://doi.org/10.1007/s10943-014-9998-9
Levin, J. (2018). The epidemiology of religion. In J. Levin (Ed.), Religion and the social sciences: Basic and applied research perspectives (pp. 259–286). Templeton Press.
Littell, R. C., Stroup, W. W., & Freund, R. J. (2002). SAS for linear models (4th ed.). SAS Institute.
Loewenthal, K. M. (2006). Orthodox Judaism: Features and issues for psychotherapy. In E. T. Dowd & S. L. Nielsen (Eds.), The psychologies in religion: Working with the religious client (pp. 203–217). Springer Publishing Company.
Mechanic, D. (1963). Religion, religiosity, and illness behavior: The special case of the Jews. Human Organization, 22(3), 202–208. https://doi.org/10.17730/humo.22.3.n413264p32280q03
Midway, S., Robertson, M., Flinn, S., & Kaller, M. (2020). Comparing multiple comparisons: Practical guidance for choosing the best multiple comparisons test. Peer J Life and Environment, 8, e10387. https://doi.org/10.7717/peerj.10387
Nissen, R. D., Gildberg, F. A., & Hvidt, N. C. (2018). Psychiatry, a secular discipline in a postsecular world?: A review. Religions, 9(1), 32. https://doi.org/10.3390/rel9010032
Pargament, K. I. (2001). The psychology of religion and coping: Theory, research, practice (revised). Guilford Press.
Pirutinsky, S., & Rosmarin, D. H. (2018). Protective and harmful effects of religious practice on depression among Jewish individuals with mood disorders. Clinical Psychological Science, 6(4), 601–609. https://doi.org/10.1177/21677026177484
Pirutinsky, S., & Rosmarin, D. H. (2022). A comparative study of mental health diagnoses, symptoms, treatment, and medication use among Orthodox Jews. Transcultural Psychiatry, 59(6), 756–766. https://doi.org/10.1177/13634615211068607
Porta, M. (2014). A dictionary of epidemiology (6th ed.). Oxford University Press.
Preuss, J. (1993). Biblical and Talmudic medicine [1911]. Rosner, F. (Ed.). Northvale, NJ: Jason Aronson.
Ritter, Z., Srinivasan, R., Han, Y., Chattopadhyay, M., Honohan, J., Johnson, B., & VanderWeele, T. J. (2023). Global Flourishing Study: Methodology. Gallup.
Rosmarin, D. H., Pargament, K. I., & Mahoney, A. (2009a). The role of religiousness in anxiety, depression, and happiness in a Jewish community sample: A preliminary investigation. Mental Health, Religion and Culture, 12(2), 97–113. https://doi.org/10.1080/13674670802321933
Rosmarin, D. H., Pirutinsky, S., Pargament, K. I., & Krumrei, E. J. (2009b). Are religious beliefs relevant to mental health among Jews? Psychology of Religion and Spirituality, 1(3), 180–190. https://doi.org/10.1037/a0016728
Russo-Netzer, P., & Bergman, Y. S. (2020). Prioritizing patterns and life satisfaction among ultra-Orthodox Jews: The moderating role of the sense of community. Journal of Psychology, 154(3), 233–248. https://doi.org/10.1080/00223980.2019.1704392
Shmueli, A. (2007). Health and religiosity among Israeli Jews. European Journal of Public Health, 17(1), 104–111. https://doi.org/10.1093/eurpub/ckl105
Srole, L., & Langner, T. (1962). Religious origin. In L. Srole, T. S. Langner, S. T. Michael, M. K. Opler, & T. A. C. Rennie (Eds.), Mental health in the metropolis: The Midtown Manhattan Study (pp. 300–324). McGraw-Hill.
Steinberg, A. (2001). Encyclopedia of Jewish medical ethics: A compilation of Jewish medical law, on all topics of medical interest, from the most ancient sources to the most current deliberations and decisions, with a concise medical and historical background, and a comprehensive comparative analysis of relevant general ethical approaches, volumes I-III. Rosner, F. (Trans.). Jerusalem: Feldheim Publishers.
Stolovy, T., Levy, Y. M., Doron, A., & Melamed, Y. (2013). Culturally sensitive mental health care: A study of contemporary psychiatric treatment for ultra-orthodox Jews in Israel. International Journal of Social Psychiatry, 59(8), 819–823. https://doi.org/10.1177/0020764012461206
Stone, L. (2023). Ultra-Orthodox fertility and marriage in the United States. Demographic Research, 49, 769–782. https://doi.org/10.4054/DemRes.2023.49.29
VanderWeele, T. J., & Mathur, M. B. (2019). Some desirable properties of the Bonferroni correction: Is the Bonferroni correction really so bad? American Journal of Epidemiology, 188(3), 617–618. https://doi.org/10.1093/aje/kwy250
Vilchinsky, N., & Kravetz, S. (2005). How are religious belief and behavior good for you?: An investigation of mediators relating religion to mental health in a sample of Israeli Jewish students. Journal for the Scientific Study of Religion, 44(4), 459–471. https://doi.org/10.1111/j.1468-5906.2005.00297.x
Zuckerman, P. (1996). Israeli Judaism [book review]. Sociology of Religion, 57(4), 419–420. https://link.gale.com/apps/doc/A19178615/AONE
Acknowledgements
The authors would like to thank Dr. Tyler J. VanderWeele, co-PI of the GFS, for his comments on an earlier draft of the present manuscript.
Funding
The GFS was supported by funding from the John Templeton Foundation (grant #61665), Templeton Religion Trust (#1308), Templeton World Charity Foundation (#0605), Well-Being for Planet Earth Foundation, Fetzer Institute (#4354), Well Being Trust, Paul L. Foster Family Foundation, and the David and Carol Myers Foundation. The opinions expressed in this publication are those of the authors and do not necessarily reflect the views of these organizations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
This study involved secondary analysis of existing, anonymized population-based survey data containing no personal identifiers, and all procedures were in accordance with the ethical standards of the human subjects review committees at Baylor University, Harvard University, and the Gallup Organization.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Levin, J., Bradshaw, M. & Johnson, B.R. Religious Differences in Physical and Mental Health among Israeli Jews: Findings from the Global Flourishing Study. J Relig Health 63, 2544–2558 (2024). https://doi.org/10.1007/s10943-024-02078-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-024-02078-5