Abstract
Religion and body weight was explored at two time points among overweight and obese African-American adults. Baseline and follow-up data were collected from 26 adults participating in a weight loss intervention and analyzed using multiple regression analyses of religious measures, body weight, and other variables. Frequent church attendance was significantly associated with greater weight lost from baseline to 16-week follow-up. In this exploratory study, religious interactions and experiences may be involved in shaping body weight among African-Americans attempting to lose weight.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Research about religion and health generally reports significant relationships between multiple dimensions of religion and better health (Hummer et al. 1999; McCullough et al. 2000; Powell et al. 2003; Strawbridge et al. 2001), although the literature has also documented religion’s deleterious associations with health (Kim and Koenig 2007). In the context of these findings, a growing number of studies have examined religion’s relationship with body weight (Koenig et al. 2012).
It is difficult to infer causal relationships between religion and health measures.
Religion may be associated with body weight through behavioral, psychosocial, and theological mechanisms. Religious individuals have lower rates of smoking and drinking (Ellison and Levin 1998; Hummer et al. 1999; Sherkat and Ellison 1999), which have associations (albeit mixed) with body weight (Chen et al. 1993; Flegal et al. 1995; Klesges et al. 1989; Liu et al. 1994; Suter et al. 1997). In a cross-sectional, national study of religion and body weight, smoking was a mediator in religion’s direct relationship with body weight (Kim et al. 2003). The differing dietary practices of some religions may also influence body weight (Fraser 1999; Kim and Sobal 2004).
Stress and social support are potential psychosocial mediators in religion’s relationship with body weight (Kim and Sobal 2004). Religion helps some adherents cope with stress (Mickley et al. 1995), and religious communities can offer positive support (Ellison and Levin 1998; Koenig et al. 1997a; Sherkat and Ellison 1999). By offering positive social support and coping mechanisms for stress, religion may buffer those with higher body weight from stress-induced eating (Epel et al. 2001) and provide needed support for weight loss and maintenance (Parham 1993). In contrast, religious communities’ also may produce lack of support or negative support by making demands from their members that may increase stress, which may lead to higher weight and less successful weight loss attempts among overweight and obese adherents trying to lose weight. Negative religious coping through beliefs of God’s abandonment and punishment may promote stress among adherents and deter weight loss efforts.
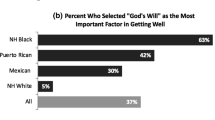
Components of religious theology that view the body as sacred and made in God’s image (Coakly 1997; Synnott 1992) may also influence lower body weight through encouraging adherents to take better care of their health by having a healthy body weight, including overweight and obese adherents attempting to lose weight. Religion may also influence adherents’ perception of control regarding body weight-related health behaviors (Debnam et al. 2012; Ellison and Levin 1998; Holt et al. 2015; Sherkat and Ellison 1999). Belief in a relationship with a divine being who will help them become healthy may galvanize weight control efforts, particularly among those attempting to lose weight. Likewise, belief that God has control of their health despite their behavioral choices may deter weight control efforts and demotivate overweight and obese adherents attempting to lose weight (Chatters 2000; Debnam et al. 2012; Holt et al. 2015).
Researchers have quantitatively surveyed adults about religion and body weight for at least 50 years (e.g., (Goldblatt et al. 1965). Koenig et al. (2001) compiled 7 studies of religion and weight, and Koenig et al. (2012) compiled 29 studies of religion and weight for a total of 36 studies, and about half of those studies found assorted associations between several measures of religion and body weight. Most studies of religion and body weight have examined religious affiliation, often finding that members of some denominations were heavier than others (Kim et al. 2003). Some studies have also examined religious involvement, with mixed findings (Cline and Ferraro 2006; Ferraro 1998). Many aspects of relationships between religion and body weight remain to be examined.
Almost all of these studies were cross-sectional, with the few longitudinal studies reporting significant results (e.g., Cline and Ferraro 2006). Although some of these previous studies analyzed large representative samples, there is a paucity of studies examining religion’s relationship with body weight in underserved samples that are not necessarily represented, such as the rural, poor, and minority (Yeary et al. 2009). Further, to the authors’ knowledge, there are no studies examining religion’s relationships within religious populations attempting to lose weight, which may have important implications for obesity interventions in faith-based settings. More research is needed to better understand associations between the many dimensions of religion and body weight, particularly those including underserved populations such as African-Americans and those involving changes in body weight over time.
Therefore, the goal of this exploratory study is to contribute to knowledge about relationships between religion and body weight in an underserved sample that involves changes in body weight over time by examining multiple components and dimensions of religion and body weight and body weight changes among overweight and obese African-American adults attempting to lose weight. We hypothesized the following: Given the most recent longitudinal study of religious attendance and body weight (Cline and Ferraro 2006), we hypothesized that (1) higher levels of church attendance would be associated with lower baseline body weight and greater weight loss from baseline to follow-up. Based on the literature regarding the influences of stress and social support on body weight (Epel et al. 2001; Kim et al. 2009; Parham 1993), and evidence of religion providing positive support and buffering stress (Kim and Koenig 2007), we hypothesized that (2) higher levels of private religiousness, daily spiritual experiences, positive religious social support, and perceived sacredness of body would be associated with lower baseline body weight and greater weight loss from baseline to follow-up. Consistent with the literature regarding religion’s potentially deleterious effects on health through increasing stress and providing negative support (Kim and Koenig 2007), we also hypothesized that (3) negative religious social support (e.g., congregation made demands of you, were critical of you) and negative religious coping (e.g., questioning God’s love, power) would be associated with higher baseline body weight and less weight loss from baseline to follow-up. Finally, we drew from the God and spiritual locus of control literature (Debnam et al. 2012; Holt et al. 2015) to hypothesize that (4) locus of control that entailed a passive approach (e.g., whatever happens in my health is in God’s control) would be associated with higher baseline body weight and less weight loss from baseline to follow-up. We used secondary data analysis from an intervention study to explore these relationships between religion and body weight.
Methods
A preexisting data set was used for secondary data analysis to explore associations between religion and body weight among African-American adults. The data set was from a study that examined the feasibility of an evidence-based behavioral weight loss intervention that was culturally adapted for rural, African-American adults attending church (Yeary et al. 2011).
Data Set
The data set included participants who were overweight [body mass index (BMI) ≥ 25 kg/m2], African-American adults enrolled in a 16-week, evidence-based, behavioral weight loss program. The intervention was a cultural adaptation of the Diabetes Prevention Program (Group 2002) and focused on dietary and physical activity habits, with a strong emphasis on goal setting and problem solving to achieve successful behavior change (Wadden and Butryn 2003). The intervention was implemented in three small African-American churches in the Lower Mississippi Delta that together had a total of 172 members. Specific study methods and results regarding the intervention have been reported in detail elsewhere (Yeary et al. 2011). Participants in this analysis were associated with one of the three African-American churches where similar numbers of people were recruited from each church (Church 1 participant n = 7, Church 2 participant n = 9, Church 3 participant n = 10), and a total of 26 participants enrolled in the study. A total of 22 of enrolled participants provided 16-week follow-up data. Dropouts did not significantly differ from non-dropouts in demographics or baseline BMI. Thus, a total of 26 participants were included for baseline data analyses and a total of 22 participants were included in analyses involving change in BMI from baseline to follow-up.
Measures
Members of the research team collected data at baseline and 16-week follow-up the following measures:
Body Weight
Anthropometric measurements were collected from all participants at baseline and follow-up. Height was measured using a stadiometer. Weight was assessed with a Tanita scale (Jebb et al. 2000). Body mass index (BMI) was calculated from dividing weight in kg by height in meters squared (Dalton 1997). Other prior studies exploring religion’s relationship with body weight have also conceptualized body weight as a continuous variable (e.g., Kim et al. 2003). Weight change was calculated as the difference in weight between baseline and 16 weeks.
Church Attendance
Church attendance is a common religion variable that has been used in religion and body weight analyses (Koenig et al. 2012). Church attendance was assessed using an item from the Duke University Religion Index (DUREL) (Koenig et al. 1997b). Subjects were asked how often they attended church or other religious meetings using response options ranging from ‘Never’ to ‘More than once a week.’ Given the high levels of religious attendance in the sample, religious attendance was coded as ‘More than once a week’ versus ‘Once a week or less,’ whereby subjects who reported attending religious services ‘once a week’ or ‘more than once a week’ were coded in the ‘Once a week or more’ category, and subjects reporting either ‘Never,’ ‘Once a year or less,’ or ‘A few times a month,’ coded in the ‘Less than once a week a week category.’
Private Religiosity
Private religiosity is also commonly assessed in the religion and body weight literature (Koenig et al. 2012) and was assessed using an item from the Duke University Religion Index (DUREL) (Koenig et al. 1997a) that asked participants how often they spent time in prayer, meditation, or Bible Study. Responses ranged from ‘Rarely or Never’ to ‘More than once a day.’ Due to the high levels of private religious activity, private religious activity was coded as ‘At least daily’ versus ‘Less than daily.’
Daily Spiritual Experiences
Although measures used to assess private religiosity (e.g., prayer, Bible study, commitment) have been included in some examinations of religion and body weight, these private religiosity measures do not directly assess an adherent’s interaction and relationship with the divine. Measures that directly assess one’s interaction with the supernatural may be more strongly related to body weight as the intensity of a person’s relationship with a divine being may be a source of support, self-efficacy, and control that may influence weight loss attempts (Kim and Koenig 2007). Thus, daily spiritual experiences were assessed by the 8-item Daily Spiritual Experiences Scale (Underwood and Teresi 2002), which assesses the extent that one perceives and interacts with a supernatural reality in their day-to-day life. Examples of questions from the scale are ‘how often do you feel God’s presence?’ and ‘how often are you spiritually touched by the beauty of creation?’, with Likert response options ranging from ‘never or almost never’ to ‘many times a day.’ The Cronbach’s alpha was .83 for the total sample.
Religious Social Support
Given that religion may be a provider of social support (Kim and Koenig 2007) and social support has been associated with body weight (Parham 1993), four dimensions of religious social support (received, given, negative, and anticipated) were assessed using the 8-item religious social support scale by Krause and colleagues (Krause 1999). Received social support (2 items) assessed the extent the subject reported receiving social support from their congregation. An example question is ‘How often do the people in your congregation make you feel loved and cared for?’ Cronbach’s alpha for received social support was low (.39) for the total sample; thus, received social support was not included in the analyses. Given social support (2 items) assessed the extent the subject reported giving social support to their congregation. An example question is ‘How often do you listen to the people in your congregation talk about their private problems and concerns?’ Cronbach’s alpha for given social support was .64 for the total sample. Negative social support (2 items) assessed the extent the subject reported the congregation being critical and demanding. An example question is ‘How often do the people in your congregation make too many demands on you?’ Cronbach’s alpha for negative social support was .67 for the total sample. Anticipated social support (2 items) assessed the extent the subject reported anticipating social support from their congregation. An example question is ‘If you were ill, how much would the people in your congregation be willing to help out?’ Cronbach’s alpha for anticipated social support was .88 for the total sample. The Likert response options for all religious social support items ranged from ‘Never’ to ‘Very Often.’
Religious Coping
Given the role of stress in body weight and religion’s potential role in reducing or exacerbating stress (Kim and Koenig 2007) and some literature reporting significant relationships between religious coping and health behaviors (Allen et al. 2014), the Brief RCOPE scale that assesses both positive and negative religious coping was included (Pargament et al. 2011). The 14-item scale asks participants how they coped with a recent negative event in their life and then are presented with a list of coping strategies. Thus, the scale focuses on situationally specific coping (i.e., a recent negative event) instead of dispositional coping. Positive religious coping refers to the positive use of religion (religion as eliciting positive emotions such as hope and perseverance) in coping situations, whereas negative religious coping refers to the negative use of religion (religion as eliciting negative emotions in the individual, such as anger and abandonment) in coping situations (Koenig et al. 2012). Examples of positive religious coping strategies in the measure are prayer, looking for a stronger connection with God, and trying to put action plans together with God. Cronbach’s alpha for positive religious coping (7 items) was .49 for the total sample. Given the low Cronbach’s alpha, positive religious coping was not included in the analysis. Examples of negative coping strategies in the measure are feeling punished by God by lack of devotion, questioning God’s love, and deciding the devil made the stressful event happen. Cronbach’s alpha for negative religious coping (7 items) was .63 for the total sample. Likert response options for all religious coping items ranged from ‘Not at all’ to ‘A great deal.’
Perceived Sacredness of the Body
Adherents who perceive their body as sacred may have more motivation to have a healthy weight. Thus, perceived sacredness of the body was assessed through the 12-item Manifestation of God in the Body scale (Mahoney et al. 2005). The measure assesses the extent participants perceive God to be connected to or expressed through their body (e.g., my body is a gift from God, my body is united with God, my body is an instrument of God). Likert response options ranged from ‘Strongly Disagree’ to ‘Strongly Agree.’ Cronbach’s alpha for the Manifestation of God in the Body scale was .93 for the total sample.
Religious Locus of Control
Given the associations between spiritual and God locus of control and weight-related health behaviors (Debnam et al. 2012; Holt et al. 2015; Karvinen and Carr 2014), religious locus of control was assessed through two measures, the spiritual locus of control (Holt et al. 2003) and God locus of control (Wallston et al. 1999) scales. The 4-item Spiritual Locus of Control Scale assessed the extent participants drew upon God’s strength to care for their own health (active) and the extent they relied on God to care for their health regardless of their actions (passive). An example item is ‘If I lead a good spiritual life, I will stay healthy’ with Likert response options ranging from ‘Strongly disagree’ to ‘Strongly agree.’ The 6-item God Locus of Control Scale asked subjects to what extent God determined their health. An example item is ‘Whatever happens to my health is God’s will,’ with Likert response options ranging from ‘Strongly disagree’ to ‘Strongly agree.’ We conceptualized higher levels of God Locus of Control as higher levels of passive religious locus of control, whereby individuals relied on God for their health apart from their own behavior. Cronbach’s alphas for Spiritual Locus of Control and God Locus of Control were .83 and .73 for the total sample, respectively.
Demographics
Gender, age, education, employment, marital status, and income were also assessed using self-reported direct questions.
Statistical Analyses
All analyses were conducted using SAS statistical software (version 9.3). Descriptive statistics about the sample were generated. Pearson and Spearman correlations were calculated to explore potential associations with religion variables. Pearson correlations were conducted when both variables were continuous. Spearman correlations were conducted when one variable was categorical and the other variable was continuous. Partial Pearson and Spearman correlations were also calculated adjusting for gender and age. Baseline BMI was included as an additional covariate when calculating partial correlations that explored the association between change from baseline BMI and religious variables.
Unadjusted general linear regression models were used to examine cross-sectional and longitudinal relationships between religion and weight; additionally, adjusted models were conducted to examine these relationships while controlling for gender and age based on the literature about the social epidemiology of obesity (Cawley 2011). Two sets of unadjusted and adjusted regression models were generated using each of the two dependent variables of interest: baseline body weight (BMI) and weight change (BMI change between pre- and post-intervention or BMI1–BMI2). Eleven individual religion variables at baseline were each independent variables in separate general linear regression models. Baseline BMI was also included as a covariate in models where weight change was the dependent variable of interest (Kim et al. 2008, 2009).
Results
Full descriptive data are presented in Table 1. In this African-American sample, the majority (85%) were female with a mean age of 51 years. About half (58%) were employed, and about half (58%) were married. A little more than a half (58%) completed at least some college education, and the majority (69%) reported an income of less than $30,000 (see Table 1). The average baseline and follow-up BMI of the sample were in the category of being obese (baseline BMI: mean = 35.8, median = 34.3; follow-up BMI: mean = 35.1, median = 34.6; change from baseline BMI to follow-up BMI: mean = −.87, SD = 1.97, median = −.49, IQR = 2.31). A total of 100% of the participants in this sample was Black Protestant (Steensland et al. 2000) due to the purposive sampling of black churches in the context of the intervention study. The majority reported attending religious services at least once a week (62%), engaging in private religious activity (e.g., prayer, Bible reading) at least once a day (85%), and a mean of 40.5 daily spiritual experiences (max = 48). The people in the sample reported mean levels of religious social support received, given, and anticipated as 7.0, 6.9, and 7.3, respectively (max = 8). In contrast, the sample reported a mean of 4.0 of negative religious social support (max = 8). Participants reported mean values of 26.7 and 13.6 positive and negative coping, respectively (max = 28). The mean score for manifestation of the body was 79.1 for the sample (max = 84). The sample’s means for active spiritual locus of control and passive spiritual locus of control were 8.3 and 9.1 (max = 10), respectively. The mean God locus of control was 24.6 (max = 36).
Demographic characteristics were examined for associations with baseline religion and weight, and there was statistical trend in the correlation between age and religious social support given (r = .39; P = .05), supporting the inclusion of age and gender as controls in adjusted models (Cawley 2011). All longitudinal models examining baseline religion and weight change controlled for baseline weight. Given the exploratory nature of the study, only correlations between independent and dependent variables are reported in Table 2.
In regression models (Table 2), negative religious social support at baseline was significantly related to baseline BMI, with higher levels of negative religious social support at baseline associated with higher BMI (P = .04). This relationship was no longer significant in the adjusted model (P = .06). There was no statistically significant relationship between negative religious coping at baseline and higher baseline BMI in the adjusted model only (P = .09).
In models examining religion with weight change, participants attending religious services at least once a week at baseline had greater weight loss compared to participants who attended religious services less than once a week (least squares (LS)-mean BMI change of 1.63 vs. − .47; P = .01) after controlling for baseline BMI. This relationship persisted when controlling for baseline BMI and demographics (P = .01), and had an R2 of .36.
Discussion
In our small sample of overweight African-American adults attempting to lose weight, negative religious social support and coping were associated with higher BMI at baseline. Social support is a common component in behavioral weight loss programs and is recognized as an important factor in weight loss and maintenance (Parham 1993). African-American church-going adults who perceive their fellow congregation members as critical and too demanding may not seek out the support they need to be healthier and may eat more to cope with their fellow adherent’s demands. Negative coping may also operate similarly, in that those who perceive God as abandoning them, punishing them, and not loving them may not draw strength from their faith to be healthier and cope with such perceptions of God through stress-induced eating. Given the cross-sectional nature of the association, reverse causality may be possible, with those experiencing weight problems potentially being more critical of themselves and thus perceive God and others more critically compared to those with lower body weight. Unmeasured third variables, such as neuroticism, may also be responsible for significant associations between negative religious coping and higher body weight. In addition to supporting our hypotheses regarding negative religiousness and higher body weight, these results are consistent with other cross-sectional studies that have reported religion’s relationship with higher BMI (Ferraro 1998; Gillum and Ingram 2006; Kim et al. 2003), although it should be noted that most other cross-sectional studies have not examined underserved samples, not surveyed rural populations, and did not examine weight change. It is unclear why specific negative religiousness measures (social support, coping) were associated with body weight whereas specific positive religiousness measures (social support) were not. Negative religious coping and social support may reflect lower levels or religious involvement, which is associated with beneficial health outcomes (Koenig et al. 2012). Negative emotions elicited through the use of negative religious coping and experienced from negative religious support may also play a more powerful role in health outcomes, such as body weight, compared religious measures that elicit neutral or positive emotions.
Regarding weight change, adults who reported attending religious services at least once a week lost more weight than those attending church less than once a week. In the context of trying to lose weight, adults attending church more frequently may have received more support to lose weight. However, religious social support variables were not significant in weight change analyses; thus, support through religious attendance is not a compelling explanatory hypothesis. Adults attending church more often may also be more likely to attend intervention meetings more often and those who were more engaged in the intervention lost more weight than those who were less engaged (Yeary et al. 2011). However, in supplemental analyses where intervention attendance and demographics were controlled for in examining religious attendance’s relationship with weight change, greater religious attendance at baseline was still significantly associated with greater weight loss over the course of the intervention. Religious attendance may indicate adherents who are motivated by their faith and translate this similar behavioral motivation of church attendance into health weight loss behavioral changes. Likewise, adherents who attend church more frequently may hold faith beliefs whereby their faith serves to empower change. Our results are consistent with Cline and Ferraro (2006) and support our hypothesis of greater religious attendance and greater weight loss over the course of the intervention.
Different religious variables were associated with baseline weight versus change in weight during the intervention. These results are consistent with Cline and Ferraro (2006) who reported significant relationships between some aspects of religion and body weight cross-sectionally that did not remain significant over time. There is also the possibility that our results are not very robust given the number of analyses; thus, replication of these analyses is needed.
Overall, very few aspects of religion were associated with baseline body weight and weight change over time. The null findings of the study may be due to the small sample size and should be examined further future studies of larger samples.
While this is not a typical longitudinal study because an intervention was involved, our results are consistent with some other longitudinal studies (i.e., Cline and Ferraro 2006) whereby religiosity is associated with higher body weight in cross-sectional analyses, and lower body weight in longitudinal analyses. Future longitudinal studies of religiosity and body weight are needed to more fully understand these relationships in a variety of ethnic groups.
Besides the restricted range of religiosity in the sample, several limitations must be kept in mind in interpreting the study’s results. The study’s small sample may have offered low statistical power that precluded the identification of meaningful effects between religion and body weight. Although the design included measures of body weight over time, the study also cannot provide strong evidence about the direction of causality. A future longitudinal study could better establish whether religion causes changes in body weight among overweight and obese adherents attempting to lose weight. Given that multiple aspects of religion were examined separately in their relationship to body weight without adjusting for multiple hypothesis testing, the findings should be interpreted in light of the exploratory nature of the study. The exploratory approach also merits caution in interpreting results, as the study’s data are secondary and lack information regarding long-term change. There is also the potential confounding impact of the faith-based intervention on weight change, in that the faith-based aspect of the intervention may have influenced participants’ religiosity, thus confounding examinations between religion and weight change. The relatively poor internal consistency measurements of religious given social support and negative religious coping are weaknesses as well. Further, the external validity of this study is limited to overweight and obese African-American adults in one Delta county attempting to lose weight.
The sample enrolled in the current study differed in meaningful ways from those studied in previous research exploring religion and body weight. The current sample consisted of African-American overweight and obese adults who had elected and were able to participate in an intensive weight loss program. These factors collectively or individually may have resulted in a sample more homogeneous than the samples studied by others. Further, the somewhat restricted range in baseline body weight within our sample may have precluded detection of cross-sectional relationships between baseline body weight and other variables. The null findings suggest that it may be useful to carefully consider weight-specific religion measures in future research.
To our knowledge, this is the first published study to assess the relationship between religion and body weight change specifically in an African-American sample. Broad generalization of study results must be tempered by consideration of the nature and size of the sample, which included only a small number of overweight, African-American adults. Nonetheless, the findings substantively advance current understandings about the cross-sectional and longitudinal relationships between religion and body weight.
This exploratory study found that individuals who had negative religious coping and negative religious social support had higher body weights. Future studies examining negative religious coping and religious social support at baseline as a predictor of body weight are needed to further understand the role of negative religiousness in body weight. Greater religious attendance at baseline was also associated with greater weight loss over the course of the intervention. This suggests that experiencing religion, interactions through religion, and the social context of religious institutions may be involved in processes surrounding weight loss among adherents. Those attending church more often may experience their faith more saliently through behavioral action, which may translate to making behavioral weight loss changes. Likewise, attending church may magnify adherents’ faith through collective worship and this increased faith may serve as a source of strength for adherents to make healthy changes. These findings need to be further investigated in larger and more diverse samples in future hypothesis-driven studies of the important topic of religion and weight.
References
Allen, J. D., Perez, J. E., Pischke, C. R., Tom, L. S., Juarez, A., Ospino, H., et al. (2014). Dimensions of religiousness and cancer screening behaviors among church-going Latinas. Journal of Religion and Health,53(1), 190–203.
Cawley, J. (2011). The Oxford handbook of the social science of obesity. Oxford: Oxford University Press.
Chatters, L. M. (2000). Religion and health: Public health research and practice. Annual Review of Public Health,21, 335–367.
Chen, Y., Horne, S. L., & Dosman, J. A. (1993). The influence of smoking cessation on body weight may be temporary. American Journal of Public Health,83(9), 1330–1332.
Cline, K. M., & Ferraro, K. F. (2006). Does religion increase the prevalence and incidence of obesity in adulthood? Journal for the Scientific Study of Religion,45(2), 269–281.
Coakly, S. (1997). Religion and the body. Cambridge: Cambridge University Press.
Dalton, S. (1997). Body weight terminology, definitions, and measurement. In S. Dalton (Ed.), Overweight and weight management: The health professional’s guide to understanding and practice. Gaithersburg, MD: Aspen’s Publisher’s Inc.
Debnam, K. J., Holt, C. L., Clark, E. M., Roth, D. L., Foushee, H. R., Crowther, M., et al. (2012). Spiritual health locus of control and health behaviors in African Americans. American Journal of Health Behavior,36(3), 360–372.
Diabetes Prevention Program (DPP) Research Group. (2002). The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care,12, 2165–2171.
Ellison, C. G., & Levin, J. S. (1998). The religion-health connection: Evidence, theory, and future directions. Health Education and Behavior,25(6), 700–720.
Epel, E., Lapidus, R., McEwen, B., & Brownell, K. (2001). Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology,26(1), 37–49.
Ferraro, K. F. (1998). Firm believers? Religion, body weight, and well being. Review of Religious Research,39, 224–244.
Flegal, K. M., Troiano, R. P., Pamuk, E. R., Kuczmarski, R. J., & Campbell, S. M. (1995). The influence of smoking cessation on the prevalence of overweight in the United States. New England Journal of Medicine,333(18), 1165–1170.
Fraser, G. E. (1999). Diet as primordial prevention in Seventh-Day Adventists. Preventive Medicine,29(6 Pt 2), S18–S23.
Gillum, F. R., & Ingram, D. D. (2006). Frequency of attendance at religious services, hypertension, and blood pressure: The Third National Health and Nutrition Examination Survey. Psychosomatic Medicine,68(3), 382–385.
Goldblatt, P. B., Moore, M. E., & Stunkard, A. J. (1965). Social factors in obesity. Journal of the American Medical Association,192(12), 97–102.
Holt, C. L., Clark, E. M., Kreuter, M. W., & Rubio, D. M. (2003). Spiritual health locus of control and breast cancer beliefs among urban African American women. Health Psychology,22(3), 294–299.
Holt, C. L., Roth, D. L., Huang, J., & Clark, E. M. (2015). Gender differences in the roles of religion and locus of control on alcohol use and smoking among African Americans. Journal of Studies on Alcohol and Drugs,76(3), 482–492.
Hummer, R. A., Rogers, R. G., Nam, C. B., & Ellison, C. G. (1999). Religious involvement and U.S. adult mortality. Demography,36(2), 273–285.
Jebb, S. A., Cole, T. J., Doman, D., Murgatroyd, P. R., & Prentice, A. M. (2000). Evaluation of the novel Tanita body-fat analyser to measure body composition by comparison with a four-compartment model. British Journal of Nutrition,83(2), 115–122.
Karvinen, K. H., & Carr, L. J. (2014). Does the perception that God controls health outcomes matter for health behaviors? Journal of Health Psychology,19(4), 521–530.
Kim, K. H., Bursac, Z., DiLillo, V., White, D. B., & West, D. S. (2009). Stress, race, and body weight. Health Psychology,28(1), 131–135.
Kim, K. H., & Koenig, H. G. (2007). Religion and health. In S. Ayers, A. Baum, C. McManu, S. Newman, K. Wallston, J. Weinman, & R. West (Eds.), Cambridge Handbook of psychology, health and medicine (2nd ed.). Cambridge: Cambridge University Press.
Kim, K. H., Linnan, L., Campbell, M. K., Brooks, C., Koenig, H. G., & Wiesen, C. (2008). The WORD (wholeness, oneness, righteousness, deliverance): A faith-based weight-loss program utilizing a community-based participatory research approach. Health Education & Behavior,35(5), 634–650.
Kim, K. H., & Sobal, J. (2004). Religion, social support, fat intake, and physical activity. Public Health Nutrition,7, 773–781.
Kim, K. H., Sobal, J., & Wethington, E. (2003). Religion and body weight. International Journal of Obesity and Related Metabolic Disorders,27(4), 469–477.
Klesges, R. C., Meyers, A. W., Klesges, L. M., & LaVasque, M. E. (1989). Smoking, body weight, and their effects on smoking behavior: A comprehensive review of the literature. Psychological Bulletin,106(2), 204–230.
Koenig, H. G., Hays, J. C., George, L. K., Blazer, D. G., Larson, D. B., & Landerman, L. R. (1997a). Modeling the cross-sectional relationships between religion, physical health, social support, and depressive symptoms. American Journal of Geriatric Psychiatry,5(2), 131–144.
Koenig, H. G., King, D. E., & Carson, V. B. (2012). Handbook of religion and health (2nd ed.). New York: Oxford University Press.
Koenig, H. G., McCullough, M. E., & Larson, D. B. (2001). Handbook of religion and health (1st ed.). New York: Oxford University Press.
Koenig, H. G., Meador, K., & Parkerson, G. (1997b). Religion index for psychiatric research: A 5-item measure for use in health outcome studies. American Journal of Psychiatry,154, 885–886.
Krause, N. (1999). Religious support. In Multidimensional measurement of religiousness/spirituality for use in health research: A report of the Fetzer Institute-National Institute on aging working group (pp. 57–63). Kalamazoo, MI: Fetzer Institute. http://fetzer.org/sites/default/files/images/resources/attachment/%5Bcurrent-date%3Atiny%5D/Multidimensional_Measurement_of_Religousness_Spirituality.pdf.
Liu, S., Serdula, M. K., Williamson, D. F., Mokdad, A. H., & Byers, T. (1994). A prospective study of alcohol intake and change in body weight among US adults. American Journal of Epidemiology,140(10), 912–920.
Mahoney, A., Carels, R. A., Pargament, K. I., Wachholtz, A., Eleeper, L. E., Kaplar, M., et al. (2005). The sanctification of the body and behavioral health patterns of college students. The International Journal for the Psychology of Religion,15, 221–238.
McCullough, M. E., Hoyt, W. T., Larson, D. B., Koenig, H. G., & Thoresen, C. (2000). Religious involvement and mortality: A meta-analytic review. Health Psychology,19(3), 211–222.
Mickley, J. R., Carson, V., & Soeken, K. L. (1995). Religion and adult mental health: State of the science in nursing. Issues in Mental Health Nursing,16(4), 345–360.
Pargament, K., Feuille, M., & Burdzy, D. (2011). The brief RCOPE: Current psychometric status of a short measure of religious coping. Religions,2(1), 51–76t.
Parham, E. S. (1993). Enhancing social support in weight loss management groups. Journal of the American Dietetic Association,93(10), 1152–1156 (quiz 1157–1158).
Powell, L. H., Shahbi, L., & Thoresen, C. E. (2003). Religion and spirituality: Linkages to physical health. American Psychologist,58, 36–52.
Sherkat, D. E., & Ellison, C. G. (1999). Recent developments and current controversies in the sociology of religion. Annual Review of Sociology,25, 363–394.
Steensland, B., Park, J. Z., Regnerus, M. D., Robinson, L. D., Wilcox, W. B., & Woodberry, R. D. (2000). The measure of American religion: Toward improving the state of the art. Social Forces,79, 291–318.
Strawbridge, W. J., Shema, S. J., Cohen, R. D., & Kaplan, G. A. (2001). Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Annals of Behavioral Medicine,23(1), 68–74.
Suter, P. M., Hasler, E., & Vetter, W. (1997). Effects of alcohol on energy metabolism and body weight regulation: Is alcohol a risk factor for obesity? Nutrition Reviews,55(5), 157–171.
Synnott, A. (1992). Tomb, temple, machine and self: The social construction of the body. The British Journal of Sociology,43(1), 79–110.
Underwood, L. G., & Teresi, J. A. (2002). The Daily Spiritual Experience Scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Annals of Behavioral Medicine,24(1), 22–33.
Wadden, T. A., & Butryn, M. L. (2003). Behavioral treatment of obesity. Endocrinology and Metabolism Clinics of North America,32, 981–1003.
Wallston, K. A., Malcarne, V. L., Flores, L., Hansdottir, I., Smith, C. A., Stein, M. J., et al. (1999). Does God determine your health? The God Locus of Health Control Scale. Cognitive Therapy and Research,23(2), 131–142.
Yeary, K. H. K., Chan-hee, J., Simpson, P., Gossett, J., Johnson, G. S., McCabe-Sellers, B., et al. (2009). Religion and body weight in an underserved population. Race, Gender, and Class,16(3–4), 82–98.
Yeary, K. H. K., Cornell, C. E., Turner, J., Moore, P., Bursac, Z., Prewitt, E., et al. (2011). Feasibility test of an evidence-based weight loss intervention translated for a faith-based, rural, African American population. Preventing Chronic Disease,8(6), 1–12.
Funding
This study was funded by Award Number P20MD002329 from the National Institute on Minority Health and Health Disparities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yeary, K.Hc.K., Moore, P.C. & Sobal, J. Religion and Body Weight Among African-American Adults Attempting to Lose Weight: An Exploratory Study. J Relig Health 59, 758–771 (2020). https://doi.org/10.1007/s10943-018-0633-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-018-0633-z