Abstract
Early sexual initiation is a catalyst for sexually transmitted infection and unintended pregnancy. American Indian/Alaska Native (AI/AN) youth initiate sex prior to age 13 more often than other U.S. youth, contributing to current inequalities in sexual health. Identifying what factors were associated with lifetime sexual experience among AI/AN youth can inform the development of primary prevention programming to delay sexual initiation, alleviate the costs of early sexual activity, and improve sexual health outcomes in this population. We analyzed cross-sectional data from 267 AI youth ages 13–19, recruited from a rural, reservation-based community. We used multivariate logistic regression models to estimate associations between independent variables and lifetime sexual experience (vaginal and/or anal sex) across the following categories: sociodemographic, knowledge, attitudes/perceptions, beliefs, intentions, skills, behaviors, and theoretical constructs. The sample was 56.2% female, mean age 15.1 years (SD = 1.7), and 22.5% were sexually experienced. In our final model, condom use self-efficacy (attitude/perception factor) and intentions to remain abstinent until marriage (intention factor) were associated with lower odds of lifetime sexual experience. Age (sociodemographic factor), intention to have sex (intention factor), use of any contraception (behavior factor), and higher response efficacy (theoretical construct) were associated with lifetime sexual experience. Of these, intention to have sex was the strongest indicator. These results both corroborate and contrast with other research conducted among rural, reservation-based AI/AN youth. Our findings show programs targeting intentions may have the greatest impact among reservation-based AI youth, and justify program delivery stratified by age group in this setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sexual and reproductive health disparities affect the American Indian and Alaska Native (AI/AN) youth population. While sexually transmitted infections (STIs) and unintended pregnancy are public health issues of concern for youth of all racial backgrounds, there is a dearth of effective prevention programming developed specifically for and with AI/AN youth.
In 2014, AI/ANs had the second highest Chlamydia and Gonorrhea rates in the U.S. [649.5/100,000 and 157.74/100,000, respectively; Centers for Disease Control & Prevention (CDC), 2015a]. In the Phoenix Indian Health Service Area where the tribal community that participated in this study resides, the average annual Chlamydia rate was nearly double the U.S. all races’ rate in 2014 (787.5/100,000 vs. 397.0/100,000; Indian Health Service, 2014). In 2011, AI/AN females ages 15–19 and 20–24 had the highest Chlamydia rates in the nation at 3638.8/100,000 and 4773.6/100,000, respectively (CDC, 2014; Indian Health Service, 2014). For AI/ANs between 2007 and 2011, 69% of all Chlamydia cases and 59% of all Gonorrhea cases were among those ages 13–24 years old (Walker et al., 2015).
Of all U.S. groups, AI/ANs have the poorest survival rates 12, 24, and 36 months post-HIV diagnosis (CDC, 2014; Indian Health Service, 2014). Between 2008 and 2012 AI/AN females were the only racial group in which HIV diagnosis rates increased (from 3.8 to 4.9/100,000; Nwangwu-Ike, Hernandez, An, Huang, & Hall, 2015). In 2010 and 2011, AI/AN females also had the lowest proportion linked to care within 3 months of an HIV diagnosis (0.1%), the lowest retention in care, and the lowest viral suppression of all female racial groups (Nwangwu-Ike et al., 2015).
In 2014, AI/AN females ages 15–19 had the third highest teen birth rate (27.3/1000) and in 2010, they had the highest prevalence of repeat teen births (CDC, 2013; Hamilton, Martin, Osterman, Curtin, & Matthews, 2015). Nearly half (41%) of AI females begin childbearing as teens and within their lifetime bear twice as many children as the general U.S. population (Martin, Hamilton, Osterman, Curtin, & Matthews, 2013). AI/AN birth data are derived from national-level statistics and do not include regional, state or tribal variations. Since health conditions vary widely across tribes, national data may not accurately capture STI or teen birth rates in specific AI/AN communities (Wingo et al., 2012).
Early sexual initiation increases the likelihood of STIs and unintended teen pregnancy by extending the length of time and frequency with which youth are engaged in unprotected sex. Youth who initiate sex prior to age 14 are more likely than those who initiate later to have multiple lifetime partners, have greater frequency of sex, use alcohol or drugs before sex, and to have sex without a condom or other contraception (Flanigan, 2003; Kaestle, Halpern, Miller, & Ford, 2005; Markham et al., 2012; Mitchell et al., 2007; O’Donnell, O’Donnell, & Stueve, 2001). National data show that AI/AN youth are more likely to initiate sex before age 13 than all other groups except Black/African American youth (Centers for Disease Control & Prevention [CDC], 2015b).
Among AI/AN youth specifically, early sexual initiation has been associated with starting alcohol and substance use at a young age, exposure to high risk situations, and experiencing violence and sexual abuse (Hellerstedt, Peterson-Hickey, Rhodes, & Garwick, 2006; Kaufman et al., 2007a, b; Mitchell et al., 2007). Factors identified that protect against early sexual debut among AI/AN youth include female sex, higher academic achievement and valuing school performance, self-efficacy to abstain from sex, and greater sexual health knowledge (Chewning et al., 2001; Kaufman et al., 2007a, b; Mitchell et al., 2007; Mitchell, Kaufman, & The Pathways of Choice, & Healthy Ways Project Team, 2002).
The disparities mentioned above in disease burden, teen pregnancy, and early sexual initiation, indicate the need for primary prevention programming for AI/AN youth before they become sexually active (Markham et al., 2010; Poobalan et al., 2009; Tingey et al., 2015a, b). Such programming should strive to postpone sexual initiation and develop youth’s knowledge, attitudes, beliefs, and skills to make productive sexual and reproductive health decisions as they move through adolescence (Markham et al., 2010; Poobalan et al., 2009). Further, programming should be specific to the present generation of AI/AN youth, who may differ substantially from previous generations, on which current prevention programming is based (Kaufman et al., 2007a, b; Markham et al., 2015).
To be effective for delaying sexual initiation as well as STI and pregnancy incidence, prevention programming should target known risk and protective factors. A review by Buhi and Goodson (2007) specifies the more well-studied factors affecting sexual behavior among adolescents of diverse racial backgrounds, to guide development of prevention programming. In the review, these factors are organized into beliefs, attitudes/perceptions, and sexual intentions, with intention identified as the most consistent predictor of sexual behavior (Buhi & Goodson, 2007).
In the literature specific to AI/AN youth, numerous risk factors are associated with negative sexual health outcomes (i.e., early age of sexual initiation, multiple sexual partners, teen pregnancy and STIs) including substance use, poverty, experiencing trauma, and barriers to accessing health care resources (Chewning et al., 2001; Griese, Kenyon, & McMahon, 2016; Kaufman et al., 2004; Markham et al., 2015; Walker, Kelly, Doshani, Saduvala, & Prejean, 2014). Despite these identified risk factors, few studies have explored the simultaneous impact of protective factors on sexual health outcomes among AI/AN youth (Chewning et al., 2001; Griese et al., 2016; Markham et al., 2015; Walker et al., 2014).
Examining protective factors (and not just risk) can help develop interventions that foster resilience, which may be particularly salient for AI/AN communities in which a larger proportion of people are young, as compared with other racial groups (Chewning et al., 2001; Hellerstedt et al., 2006). In a study by Markham et al. (2015) conducted with American Indian youth, lower next-year intentions to have oral or vaginal sex, avoidance of risky situations, and nonuse of alcohol were associated with lower odds of lifetime sexual intercourse. Chewning et al. (2001) found that factors significantly associated with abstention from intercourse and/or consistent use of birth control included: perceived lower health-risk behavior of friends, higher perceived parental support, higher perceived parental knowledge and monitoring of adolescent’s activities and friends, higher value on scholastic achievement, higher reported academic performance, and higher self-efficacy for safer sexual behaviors.
Our study was designed to seek a broader understanding of risk and protective factors for sexual experience among a rural, reservation-based sample of AI youth, a group potentially at high risk for STIs/HIV and unintended pregnancy, who were participating in an evaluation of a comprehensive sexual and reproductive health intervention called Respecting the Circle of Life. Briefly, our study team utilized a formative participatory research approach with the partnering tribal community to adapt an existing evidence-based intervention (EBI) for HIV risk reduction, select the study design for its evaluation, and guide analyses of results (Tingey et al., 2015a). We conducted fourteen focus groups, nine with youth and five with parents, and three community advisory board meetings that explored youth’s knowledge, attitudes and behaviors related to sexual risk taking in addition to the historical, social, cultural, and environmental factors they experience to guide program development and outcomes to be measured. For more information about our tribal-academic partnership to develop and evaluate Respecting the Circle of Life please see Chambers et al. (2016) and Tingey et al. (2015a).
The EBI we chose for adaptation and evaluation was selected through our tribal-academic participatory process because it focused on a variety of domains affecting sexual health outcomes, specifically: knowledge, attitude/perceptions, beliefs, intentions, skills, and high-risk behaviors. We selected the EBI for its theoretical underpinnings promoting protective factors, capacity for delivery by trained community members, non-school-based intervention setting, and history of productive cross-cultural replication (Tingey et al., 2015a). The intervention we selected for adaptation is rooted in Protection Motivation Theory (PMT), which has been has used successfully to develop efficacious sexual risk reduction interventions for adolescents in a variety of sociocultural contexts (Chen et al., 2010; Kaljee et al., 2005; Stanton et al., 1996).
PMT posits two cognitive pathways combine to form protection motivation, or the intention to protect oneself from a potential threat. Response to a threatening situation can either be protective (adaptive) or risky (maladaptive), and is influenced by a balance between the two pathways: threat appraisal and coping appraisal. The threat appraisal pathway considers intrinsic (internal) and extrinsic (external) rewards resulting from the maladaptive behavior together with perceived severity (degree of harm resulting from the threat) and vulnerability (probability a person will experience harm from the threat). The coping appraisal pathway considers self-efficacy (perceived ability to complete the adaptive behavior) and response efficacy (belief that the adaptive response will be effective protecting against the threat) along with response cost (sacrifice associated with the adaptive behavior; Rogers, 1983).
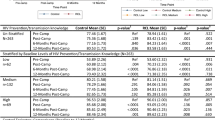
For this analysis, we sought to identify individual characteristics, PMT constructs, and modifiable intra- and interpersonal risk and protective factors associated with lifetime sexual experience organized by domains of potential intervention impact: knowledge, attitude/perceptions, beliefs, intentions, skills, and behaviors. Based on previous findings in studies assessing risk and protective factors among AI/AN youth, we hypothesized that having ever had sexual intercourse would be negatively associated with the variables specified in Table 1, which is organized by domain.
We hypothesized that having ever had sexual intercourse would be positively associated with older age, ever suspended, smoking cigarettes, drinking alcohol and using marijuana in the last 6 months, use of contraception, intention to have sex, and the PMT constructs of extrinsic and intrinsic rewards. Study findings are expected to contribute to the AI/AN adolescent sexual health research base and inform the development of targeted prevention programming to delay sexual initiation and improve sexual health outcomes in this population.
Methods
Participants
American Indian youth ages 13–19 from a rural reservation-based community in Arizona were the participants in this study. Youth were participating in a randomized controlled trial to evaluate Respecting the Circle of Life and completed a baseline survey (Tingey et al., 2015a, b). We recruited youth for the study through local schools and at public events through the use of flyers, handouts, radio PSAs and ads in the local newspaper. Trained research assistants from the participating tribal community described the purpose, general design and enrollment criteria to eligible participants. For those interested, written informed consent (if at least 18 years old) or assent/parental permission (if < 18 years old) was completed. The study was approved by relevant tribal, and university research review boards. This manuscript was approved by the governing body of the participating tribal community which includes a separate review and approval by both the Tribal Health Advisory Board and Tribal Council.
Survey
We utilized the self-report Youth Health Risk Behavior Inventory (YHRBI; Stanton et al., 1995), which contains sociodemographic items as well as measures of the risk and protective factors and PMT constructs specified in Table 1. We tailored and pilot tested the YHRBI based on feedback from the participating tribal community to ensure cultural and linguistic relevance (Tingey et al., 2015a). We included definitions of sexual behaviors (i.e., vaginal sex, anal sex) in the pilot testing to clarify concepts and increase comprehension (Tingey et al., 2015a). Factor analyses and internal reliability testing using Chronbach’s alpha coefficients were utilized to confirm that the validated YHRBI subscales used for data collection were appropriate for this study population. Items were only removed if they greatly impacted the internal consistency of the subscale. Chronbach’s alpha coefficients are presented in Table 1. We collected data between July 2011 and July 2012.
Data Collection
Participants completed the baseline survey on hard-copy in a private room. The survey took approximately 30–45 min to complete. To ensure confidentiality, hard-copy data were entered into a secure database. All data were collected using a unique participant identification number. Youth did not receive any incentive for completing the baseline survey.
Dependent Variable
We analyzed the dependent variable, lifetime sexual experience, as a composite variable comprising lifetime experience of either vaginal or anal sex. We defined vaginal sex as “When a boy puts his penis inside the girl’s vagina” and anal sex as “When a boy puts his penis in the butt of another person.” If participants answered “no” to both questions they were categorized as no lifetime sexual experience.
Independent Variables
We organized independent variables to reflect inherent recipient characteristics as well as modifiable risk and protective factors. These categories included sociodemographic, knowledge, attitudes/perceptions, beliefs, intentions, skills, behaviors and PMT constructs. The PMT constructs included self-efficacy, response efficacy, and response cost (coping appraisal pathway), and extrinsic rewards, intrinsic rewards, severity and vulnerability (threat appraisal pathway; Stanton, Aronson, Borgatti, Galbraith, & Feigelman, 1993, Stanton et al., 1995, 1996, 1997). Please see Table 1 for a complete description of these independent variable measures.
Statistical Analysis
We first examined bivariate associations between each individual independent variable and the outcome, lifetime sexual experience. We tested independent variables that were significantly associated with lifetime sexual experience at the p < 0.1 level in the context of other covariates in a multivariate regression model. We present both the complete multivariate model and the final multivariate model, which includes only those variables with p values < 0.05.
We carried out bivariate and multivariate analyses using generalized estimating equations (GEE) with a Poisson family, log link, exchangeable correlation and robust variance. We chose to use the Poisson distribution in our analyses because more than 20% of youth enrolled reported having lifetime sexual experience. Using logistic regression with outcomes this common can lead to an overestimate of relative risks (McNutt, Wu, Xue, & Hafner, 2003). We adjusted all models for self-selected peer group clusters which were formed after baseline assessment and prior to randomization. Self-selected peer group clusters were sex and age-group specific (13–15 or 16–19). Although this analysis examines baseline data only, we adjusted for peer group clusters because potential participants were instructed to enroll in the study with friends, peers, and/or family members. Therefore, those within the same self-selected peer group cluster were more similar in their responses to questions and study outcomes than to those in other groups. Standard errors in regression models were adjusted for cluster randomization by identifying the team number as the cluster variable and specifying robust variance. Robust variance specifies the use of the Huber/White sandwich estimator of variance and corrects for any misspecification of the correlation structure. We conducted all analyses using Stata 14 statistical software (StataCorp, 2015).
Results
Participant Characteristics
The analytic sample included 267 self-identified AI youth ages 13–19. The sample was 56.2% female, with a mean age of 15.1 years (SD = 1.7); 22.5% reported ever having had vaginal or anal sex (see Table 2). Of the sample, 93.3% were currently in school, 29.8% had ever been suspended, and 23.6% reported skipping school in the last semester. In the last 6 months, just over 10% had smoked cigarettes and almost a quarter had used alcohol or marijuana (19.6 and 22.2%, respectively). A little over 20% reported the use of any type of contraception in the last 6 months (including condoms, birth control pills, Depo-Provera, IUD, gel/spermicide or emergency contraception).
Bivariate Analyses
In the bivariate analyses displayed in Table 3, we found the following factors to be associated with a greater likelihood of lifetime sexual experience (risk ratio > 1): older age, ever suspended, skipped school in last semester (sociodemographic factors); HIV prevention and transmission knowledge (knowledge factor); sometimes sex just happens (attitude/perception factor); belief condoms prevent STI/HIV (belief factor); intention to drink alcohol, intention to use marijuana, intention to have sex, intention to use condoms (intention factors); partner negotiation on condom use (skills factor); used cigarettes, drank alcohol, used marijuana, used any contraception, used the pill, Depo or IUD (behavior factors in last 6 months); and the protection motivation theoretical constructs of response efficacy, extrinsic and intrinsic rewards, and vulnerability. Condom use self-efficacy (attitude/perception factor), intention to remain abstinent until marriage (intention factor); and self-efficacy (theoretical construct) were associated with a lower likelihood of lifetime sexual experience (risk ratio < 1). No other variables were significantly associated with lifetime sexual experience (see Table 3).
Multivariate Analysis
In the final multivariate model displayed in Table 4, we found that older age, intention to have sex in the next 6 months, use of any contraception in the last 6 months, and response efficacy were associated with greater likelihood of lifetime sexual experience (p < 0.05). Condom use self-efficacy and intention to remain abstinent until marriage were associated with a lower likelihood of lifetime sexual experience (p < 0.05). No other variables were significantly associated with lifetime sexual experience in the final model.
Discussion
This analysis explored baseline risk and protective factors associated with lifetime sexual experience among rural, reservation-based AI youth participating in a sexual health intervention trial. Our findings corroborate and extend those found in other research with AI/AN youth, with some differences that are expounded upon here (Buhi & Goodson, 2007; Chewning et al., 2001; Hellerstedt et al., 2006; Markham et al., 2015; Markham, Fleschler Peskin, Addy, Baumler, & Tortolero, 2009; Mitchell et al., 2007).
Ever being suspended and skipping school did not remain significant risk factors for lifetime sexual experience in our final model, contradicting similar research conducted with predominately reservation-based AI/AN youth. Specifically, poor grades, lower school attachment and dropout rates have been demonstrated as risk factors, while sense of belonging at school and connection to school activities have been found protective of early sexual initiation (Dickens, Dieterich, Henry, & Beauvais, 2012; Griese et al., 2016; Mitchell et al., 2007). It is possible that being suspended and skipping school are functioning as precursors to poor academic performance and drop-out in this sample, but not yet significantly associated with the initiation of sexual activity.
The belief that condoms prevent STI/HIV and pregnancy did not remain significant in our final model. This result may validate qualitative data collected by Kaufman et al. (2007a, b) with other reservation-based AI/AN youth describing how actual condom use may not be tied to understanding the importance of condoms for prevention, but rather to access, convenience, and whether or not youth carry condoms with them. Additional qualitative research concerning AI youth substantiates how the intention to use condoms and actual condom use may be moderated by inconsistent access to condoms and confidentiality concerns (Chambers et al., 2016; Kaufman et al., 2004). AI youth in that study described not wanting to purchase condoms or pick them up at the local Indian Health Service hospital (even though condoms were free) because “everyone knows you,” and “someone might know their parents” (Chambers et al., 2016, p. 4). Limited access to prevention methods and fears about lack of privacy when utilizing public health services are important considerations in reservation-based and other rural communities.
Finally, the self-efficacy theoretical construct dropped out of our final model as a protective factor. Past research is mixed on the impact of self-efficacy on sexual experience. One study conducted with rural, reservation-based AI youth showed a protective effect, while a meta-analysis of studies with youth from a variety of racial backgrounds showed no relationship (Buhi & Goodson, 2007; Chewning et al., 2001). Perhaps self-efficacy is more powerfully associated with action-specific behaviors (i.e., actual condom use) than the initiation of sexual activity in general (Baele, Dusseldorp, & Maes, 2001).
Interestingly, the use of cigarettes, alcohol, or marijuana in the last 6 months did not remain a significant risk factor for lifetime sexual experience in our final model, despite several quantitative and qualitative studies conducted with AI/AN youth that demonstrated the inextricable link between these behaviors (Chambers et al., 2016; Hellerstedt et al., 2006; Kaufman et al., 2007a, b; Markham et al., 2015). Specifically, Markham et al. (2015) found that lifetime alcohol abstinence had a protective effect on lifetime sexual experience among a mixed sample of urban and rural AI/AN youth. Further, using illicit drugs in the past 30 days has been associated with lifetime sexual experience for both AI/AN girls and boys, while binge drinking in the past 2 weeks has been associated with lifetime sexual experience for boys only (Hellerstedt et al., 2006).
In our final model, the statistically significant factors associated with increased likelihood of sexual experience were older age (sociodemographic factor); intention to have sex in the next 6 months (intention factor); use of any contraception in the last 6 months (behavior factor); and higher response efficacy (theoretical construct). Of these, intention to have sex was the strongest indicator of lifetime sexual experience. The factors associated with decreased likelihood of lifetime sexual experience in the final model included condom use self-efficacy (attitude/perception factor) and intention to remain abstinent until marriage (intention factor).
Our results substantiate results from other studies with AI/AN and non-AI/AN youth demonstrating that older youth are more likely to be sexually experienced and that in the context of all factors that were analyzed, intention to have sex had the strongest association with sexual experience (Buhi & Goodson, 2007; Markham et al., 2009, 2015). Intention to remain abstinent until marriage and condom use self-efficacy were the significant protective factors for sexual experience in the context of all other factors, also underscoring prior research in this reservation-based community and other study populations (Buhi & Goodson, 2007; Chambers et al., 2016; Chewning et al., 2001; Tingey et al., 2015b). Specifically, positive attitudes towards abstinence have been associated with lower likelihood of sexual initiation and delayed onset of initiation (Buhi & Goodson, 2007; Chewning et al., 2001).
Response efficacy, or the belief that an adaptive response (i.e., condoms, contraception) will be effective protecting against the threat (i.e., STI/HIV, pregnancy), was the only theoretical construct associated with lifetime sexual experience in our final model. The items constituting this variable included: “condoms are important to prevent pregnancy,” “condoms are important to prevent STI/HIV,” and “if a girl says no to sex, a boy would think its ok.” Participants who agreed with these statements had a greater likelihood of being sexually experienced. The interpretation of this result requires careful consideration, especially with regard to the potential for collinearity between the belief variable that condoms prevent STI/HIV and pregnancy (which was not significant in our final model), and the possible implications of the role consent plays in sexual initiation. It may be that sexually experienced youth are more likely to believe that various adaptive responses (e.g., condom use, contraceptive use) will protect against infection and pregnancy because they might have used these methods with success in the past.
Implications
The results of this study have several implications concerning intervention development and delivery. First, programming should be age-appropriate and target delivery to youth prior to sexual debut, in order to teach important skills before youth engage in sex, and ideally to postpone initiation. Changing intentions to initiate sex, postpone initiation, and/or reduce the frequency of unprotected sexual activity should be key intervention targets. To accomplish this, programs can teach goal setting, decision making, problem solving, and staying true to personal and family values, which programs can then reinforce by role playing exercises so that participants can practice communicating goals and values with peers, parents and partners. Further, even though youth with higher condom use self-efficacy were more likely to not be sexually experienced, sexually experienced youth were more likely to believe condoms and other protective behaviors work, and to have used contraception in the last 6 months. Taking these results together, prevention programs should include information about various protective methods and include hands-on skill building activities to ensure that youth can correctly and consistently use their protective method(s) of choice when the time arises to do so.
Limitations
There are several limitations to this study. First, the data were cross-sectional and do not allow for exploring the temporal relationship between risk and protective factors and sexual initiation. Second, while appropriate for the study design, data were collected via self-report and may be affected by bias in social desirability. Third, although these findings make an important contribution to the growing body of AI/AN adolescent sexual health literature, data were collected with only one tribal community, thus limiting generalizability. Fourth, while it is difficult to capture every domain worthy of investigation without causing undue participant burden, future studies of sexual experience and initiation with AI/AN youth should include school performance and drop-out rates (Dickens et al., 2012; Griese et al., 2016; Mitchell et al., 2007), experience of trauma and possible sexual abuse (Hellerstedt et al., 2006; Kaufman et al., 2004), and impulsivity or sensation-seeking, all of which have been associated with early sexual initiation (Kalichman, Heckman, & Kelly, 1996). Finally, our survey did not examine the extent of involvement in cultural traditions or practices of participating AI youth; we are therefore unable to describe cultural assets or traditional beliefs and values that may positively affect their sexual and reproductive health. Additional research is needed to identify important cultural and community ties associated with the sexual health attitudes, beliefs and behaviors of AI/AN youth.
Conclusions
Our goal was to identify potential points of intervention by exploring contextually relevant risk and protective factors, some of which are modifiable, and constructs of the PMT influencing sexual experience among rural, reservation-based American Indian adolescents. This study is one of few to concurrently examine both intra- and interpersonal risk and protective factors as well as theoretical associations with adolescent sexual behaviors (Protogerou & Johnson, 2014; Shneyderman & Schwartz, 2013). The analysis identified factors associated with lifetime sexual experience, including age, use of contraception, intention to have sex and the theoretical construct of response efficacy, and factors protective of sexual experience including condom use self-efficacy and intention to remain abstinent. Our findings suggest that primary prevention programs for AI/AN youth targeting intentions may have greater effects than those targeting other factors (Buhi & Goodson, 2007), and support delivery of such programs to specific age groups in reservation-based settings (Protogerou & Johnson, 2014). Our results suggest that programs should address both intra- and interpersonal factors (i.e., knowledge, attitudes, beliefs, intentions, skills and behaviors) and be rooted in a theoretical framework, to delay sexual initiation or lessen the costs of early unprotected sexual activity (Markham et al., 2009, Chewning et al., 2001; Hellerstedt et al., 2006; Markham et al., 2015; Protogerou & Johnson, 2014). Programs that account for and respond to these identified risk and protective factors may have potential to postpone or delay sexual initiation among AI/AN youth in rural tribal communities (Shneyderman & Schwartz, 2013).
References
Baele, J., Dusseldorp, E., & Maes, S. (2001). Condom use self-efficacy: Effect on intended and actual condom use in adolescents. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 28(5), 421–431. https://doi.org/10.1016/S1054-139X(00)00215-9.
Buhi, E. R., & Goodson, P. (2007). Predictors of adolescent sexual behavior and intention: A theory-guided systematic review. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 40, 4–21. https://doi.org/10.1016/j.jadohealth.2006.09.027.
Centers for Disease Control and Prevention (CDC). (2013). Vital signs: Repeat births among teens—United States, 2007–2010. Morbidity and Mortality Weekly Report, 62, 249–255.
Centers for Disease Control and Prevention (CDC). (2015a). Sexually Transmitted Disease Surveillance 2014. Atlanta, GA: Division of STD Prevention, U.S. Department of Health and Human Services. https://www.cdc.gov/std/stats15/std-surveillance-2015-print.pdf. Accessed December 23, 2015.
Centers for Disease Control and Prevention (CDC). (2015b). 1991–2013 High School Youth Risk Behavior Survey data. http://nccd.cdc.gov/youthonline/. Accessed December 23, 2015.
Centers for Disease Control and Prevention, & Indian Health Service. (2014). Indian Health Surveillance report—Sexually transmitted diseases 2011. Atlanta, GA: US Department of Health and Human Services.
Chambers, R., Tingey, L., Mullany, B., Parker, S., Lee, A., & Barlow, A. (2016). Exploring sexual risk taking among American Indian adolescents through Protection Motivation Theory. AIDS Care, 28(9), 1089–1096.
Chen, X., Stanton, B., Gomez, P., Lunn, S., Deveaux, L., Brathwaite, N., et al. (2010). Effects on condom use of an HIV prevention programme 36 months postintervention: A cluster randomized controlled trial among Bahamian youth. International Journal of STD and AIDS, 21(9), 622–630. https://doi.org/10.1258/ijsa.2010.010039.
Chewning, B., Douglas, J., Kokotailo, P. K., LaCourt, J., Clair, D. S., & Wilson, D. (2001). Protective factors associated with American Indian adolescents’ safer sexual patterns. Maternal and Child Health Journal, 5, 273–280.
Dickens, D. D., Dieterich, S. E., Henry, K. L., & Beauvais, F. (2012). School bonding as a moderator of the effect of peer influences on alcohol use among American Indian adolescents. Journal of Studies on Alcohol and Drugs, 73, 597–603. https://doi.org/10.15288/jsad.2012.73.597.
Flanigan, C. M. (2003). Sexual activity among girls under age 15: Findings from the national survey of family growth. In B. Albert, S. Brown, & C. M. Flanigan (Eds.), 14 and younger: The sexual behavior of young adolescents (pp. 57–64). Washington DC: National Campaign to Prevent Teen Pregnancy.
Griese, E. R., Kenyon, D. B., & McMahon, T. R. (2016). Identifying sexual health protective factors among Northern Plains American Indian youth: An ecological approach utilizing multiple perspectives. American Indian and Alaska Native Mental Health Research (Online), 23, 16–43. https://doi.org/10.5820/aian.2304.2016.16.
Hamilton, B. E., Martin, J. A., Osterman, M. J., Curtin, S. C., & Matthews, T. J. (2015). Births: Final data for 2014. National vital statistics reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 64, 1–64.
Hellerstedt, W. L., Peterson-Hickey, M., Rhodes, K. L., & Garwick, A. (2006). Environmental, social, and personal correlates of having ever had sexual intercourse among American Indian youths. American Journal of Public Health, 96, 2228–2234. https://doi.org/10.2105/AJPH.2004.053454.
Kaestle, C. E., Halpern, C. T., Miller, W. C., & Ford, C. A. (2005). Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. American Journal of Epidemiology, 161, 774–780. https://doi.org/10.1093/aje/kwi095.
Kalichman, S. C., Heckman, T., & Kelly, J. A. (1996). Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Archives of Sexual Behavior, 25, 141–154.
Kaljee, L., Genberg, B., Riel, R., Cole, M., Tho, L. H., Thi Kim Thoa, L., et al. (2005). Effectiveness of a theory-based risk reduction HIV prevention program for rural Vietnamese adolescents. AIDS Education and Prevention, 17(3), 185–199. https://doi.org/10.1521/aeap.17.4.185.66534.
Kaufman, C., Beals, J., Mitchell, C. M., Lemaster, P., Fickenscher, A., & The Pathways of Choice and Healthy Ways Project Teams. (2004). Stress, trauma, and risky sexual behaviour among American Indians in young adulthood. Culture, Health & Sexuality, 6(4), 301–318.
Kaufman, C., Desserick, J., Big Crow, C. K., Holy Rock, B., Keane, E., & Mitchell, C. M. (2007a). Culture, context, and sexual risk among Northern Plains American Indian youth. Social Science and Medicine, 64, 2152–2164.
Kaufman, C. E., Shelby, L., Mosure, D. J., Marrazzo, J., Wong, D., de Ravello, L., et al. (2007b). Within the hidden epidemic: Sexually transmitted diseases and HIV/AIDS among American Indians and Alaska Natives. Sexually Transmitted Diseases, 34, 767–777. https://doi.org/10.1097/01.olq.0000260915.64098.cb.
Markham, C. M., Craig Rushing, S., Jessen, C., Lane, T. L., Gorman, G., Gaston, A., et al. (2015). Factors associated with early sexual experience among American Indian and Alaska Native youth. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 57, 334–341. https://doi.org/10.1016/j.jadohealth.2015.06.003.
Markham, C. M., Fleschler Peskin, M., Addy, R. C., Baumler, E. R., & Tortolero, S. R. (2009). Patterns of vaginal, oral, and anal sexual intercourse in an urban seventh-grade population. The Journal of School Health, 79, 193–200. https://doi.org/10.1111/j.1746-1561.2008.00389.x.
Markham, C. M., Lormand, D., Gloppen, K. M., Peskin, M. F., Flores, B., Low, B., et al. (2010). Connectedness as a predictor of sexual and reproductive health outcomes for youth. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 46, S23–S41. https://doi.org/10.1016/j.jadohealth.2009.11.214.
Markham, C. M., Tortolero, S. R., Peskin, M. F., Shegog, R., Thiel, M., Baumler, E. R., et al. (2012). Sexual risk avoidance and sexual risk reduction interventions for middle school youth: A randomized controlled trial. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 50, 279–288. https://doi.org/10.1016/j.jadohealth.2011.07.010.
Martin, J. A., Hamilton, B. E., Osterman, M. J., Curtin, S. C., & Matthews, T. J. (2013). Births: Final data for 2012. National Vital Statistics reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 62, 1–68.
McNutt, L. A., Wu, C., Xue, X., & Hafner, J. P. (2003). Estimating the relative risk in cohort studies and clinical trials of common outcomes. American Journal of Epidemiology, 157, 940–943.
Mitchell, C. M., Kaufman, C. E., & The Pathways of Choice and Healthy Ways Project Team. (2002). Structure of HIV knowledge, attitudes, and behaviors among American Indian young adults. AIDS Education and Prevention, 14(5), 401–418.
Mitchell, C. M., Whitesell, N. R., Spicer, P., Beals, J., Kaufman, C. E., & The Pathways of Choice and Healthy Ways Project Team. (2007). Cumulative risk for early sexual initiation among American Indian youth: A discrete-time survival analysis. Journal of Research on Adolescence, 17, 387–412. https://doi.org/10.1111/j.1532-7795.2007.00527.x.
Nwangwu-Ike, N., Hernandez, A. L., An, Q., Huang, T., & Hall, H. I. (2015). The epidemiology of human immunodeficiency virus infection and care among adult and adolescent females in the United States, 2008–2012. Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health, 25, 711–719. https://doi.org/10.1016/j.whi.2015.07.004.
O’Donnell, L., O’Donnell, C. R., & Stueve, A. (2001). Early sexual initiation and subsequent sex-related risks among urban minority youth: The Reach for Health Study. Family Planning Perspectives, 33, 268–275. https://doi.org/10.2307/3030194.
Poobalan, A. S., Pitchforth, E., Imamura, M., Tucker, J. S., Philip, K., Spratt, J., et al. (2009). Characteristics of effective interventions in improving young people’s sexual health: A review of reviews. Sex Education, 9, 319–336. https://doi.org/10.1080/14681810903059185.
Protogerou, C., & Johnson, B. T. (2014). Factors underlying the success of behavioral HIV-prevention interventions for adolescents: A meta-review. AIDS and Behavior, 18, 1847–1863. https://doi.org/10.1007/s10461-014-0807-y.
Rogers, R. W. (1983). Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In T. Cacioppi & R. E. Petty (Eds.), Social Psychology (pp. 153–176). New York: Guilford.
Shneyderman, Y., & Schwartz, S. J. (2013). Contextual and intrapersonal predictors of adolescent risky sexual behavior and outcomes. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 40, 400–414. https://doi.org/10.1177/1090198112447800.
Stanton, B. F., Aronson, R., Borgatti, S., Galbraith, J., & Feigelman, S. (1993). Urban adolescent high-risk sexual behavior: Corroboration of focus group discussions through pile-sorting. The AIDS Youth Research Team. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education, 5, 162–174.
Stanton, B., Black, M., Feigelman, S., Ricardo, I., Galbraith, J., Li, X., et al. (1995). Development of a culturally, theoretically and developmentally based survey instrument for assessing risk behaviors among African-American early adolescents living in urban low-income neighborhoods. AIDS Education and Prevention, 7, 160–177.
Stanton, B., Fang, X., Li, X., Feigelman, S., Galbraith, J., & Ricardo, I. (1997). Evolution of risk behaviors over 2 years among a cohort of urban African American adolescents. Archives of Pediatrics and Adolescent Medicine, 151, 398–406. https://doi.org/10.1001/archpedi.1997.02170410072010.
Stanton, B. F., Li, X., Ricardo, I., Galbraith, J., Feigelman, S., & Kaljee, L. (1996). A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Archives of Pediatrics and Adolescent Medicine, 150, 363–372.
StataCorp. (2015). Stata statistical software: Release 14. College Station: StataCorp.
Tingey, L., Mullany, B., Strom, R., Hastings, R., Barlow, A., & Rompalo, A. (2015a). The Respecting the Circle of Life trial for American Indian adolescents: Rationale, design, methods and baseline characteristics. AIDS Care, 27(7), 885–891.
Tingey, L., Mullany, B., Strom, R., Hastings, R., Lee, A., Parker, A., et al. (2015b). Respecting the Circle of Life: One year outcomes from a randomized controlled comparison of an HIV risk reduction intervention for American Indian adolescents. AIDS Care, 27(9), 1087–1097.
Walker, F. J., Kelly, J. M., Doshani, M., Saduvala, N., & Prejean, J. (2014). Epidemiology of HIV among American Indians and Alaska Natives—United States, 2008–2011. Journal of Health Disparities Research and Practice, 8, Article 7.
Walker, F. J., Llata, E., Doshani, M., Taylor, M. M., Bertolli, J., Weinstock, H. S., et al. (2015). HIV, Chlamydia, Gonorrhea, and primary and secondary Syphilis among American Indians and Alaska Natives within Indian health service areas in the United States, 2007–2010. Journal of Community Health, 40, 484–492. https://doi.org/10.1007/s10900-014-9961-4.
Wingo, P. A., Lesesne, C. A., Smith, R. A., de Ravello, L., Espey, D. K., Arambula Solomon, T. G., et al. (2012). Geographic variation in trends and characteristics of teen childbearing among American Indians and Alaska Natives, 1990–2007. Maternal and Child Health Journal, 16, 1779–1790. https://doi.org/10.1007/s10995-011-0924-4.
Acknowledgements
The authors respectfully acknowledge the youth, families, community members, and tribal leaders from the participating tribal community for their innovation and leadership in pioneering research strategies. The authors give thanks to the Native American Research Centers for Health for funding this research.
Funding
This work was supported by the Native American Research Centers for Health (Grant Number U26IHS300286/03).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Tingey, L., Chambers, R., Rosenstock, S. et al. Risk and Protective Factors Associated With Lifetime Sexual Experience Among Rural, Reservation-Based American Indian Youth. J Primary Prevent 39, 401–420 (2018). https://doi.org/10.1007/s10935-018-0517-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10935-018-0517-8