Abstract
Purpose In most industrialized countries, the share of workers in the age 55+ age group is increasing while there is a shortage of young workers. Although data suggest that at least one in five older workers suffers from chronic musculoskeletal pain, most will continue working despite pain. The objective of this study is to explore factors associated with staying at work for workers with musculoskeletal pain. Methods An interpretive descriptive method was used. Semi-structured individual interviews were conducted. Inclusion criteria were: manual/mixed occupations, persistent musculoskeletal pain, and working 28 h weekly or more. Analysis was performed using themes from the conceptual model created. Results Fourteen participants were included, ages 55–70. They ranged from self-employed individuals to employees of large organizations. For most, the perception of being useful, having peer recognition and feeling that work contributes to health were essential drivers for staying at work. Flexibility at work was deemed essential by all but took various forms. Individual cost of staying at work varied from low to high. Conclusion This study identified both personal and work-related factors associated with working in the presence of pain. New concept of cost of staying at work appears promising.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many people work despite having musculoskeletal pain. A study conducted in Québec (Canada) in 2011 found that over 60% of the workers interviewed experienced musculoskeletal pain at least occasionally and that 80% of them stayed at work, taking no sick leave for the pain [1]. In Europe, similar results were obtained in a 14-country study of adult workers who had experienced pain for at least 6 months. In fact, of those working full- or part-time (n = 2100), 55% continued to work without taking any sick leave [2]. In addition, a French study of aging workers found that nearly 60% of salaried employees aged 50 years and over who were questioned by occupational health physicians reported experiencing pain while working [3].
Other studies have sought to identify more clearly the factors associated with individuals staying at work despite pain. A systematic review [4] of articles published between 1991 and 2011 identified seven studies (five quantitative and two qualitative) on adults (aged 18 to 65 years) who remained at work despite experiencing pain for 3 months or longer. In the quantitative studies, two main factors were associated with their staying at work: low levels of perceived physical disability and of emotional distress. The two qualitative studies revealed that the presence of support and leeway in the workplace and the reduction of personal activities outside work were the main factors associated with workers ability to stay at work. Four more recent studies (2010–2018) [5,6,7,8] confirm these factors, while adding others. These studies suggest that having the possibility to negotiate with partners (health care system, workplace) represents another key factor in workers staying at work, along with the possibility of obtaining modifications to the physical work environment. However, in both the literature review [4] and the more recent studies, the participants were mostly recruited through the medical system or patient associations (e.g., fibromyalgia, arthritis), attesting to the presence of an established diagnosis, severity of the symptoms and an active medical consultation process. No particular attention was paid to the aging worker population.
Other studies, however, specifically broach the subject of workers staying at work in connection with aging but not with pain [9,10,11,12]. They state that, apart from employer modifications to the work environment, other factors such as level of education, financial preparation for retirement and employment sector are associated with the decision to stay at work. Workers’ health was another factor found to affect their decision to stay at work or not. Its influence was described primarily in relation to how long they stayed at work: generally speaking, good health appeared to be associated with staying at work for longer, while poor health promoted earlier retirement or the decision to work part-time. Also, in a study on workers working beyond retirement age, Sewdas et al. [12] found the two most important motives for staying at work longer were maintaining daily routines and financial benefits. The effect of health and pain problems on how individuals manage to stay at work was not examined in these studies.
Thus, to date, studies have studied either factors associated with workers who stay at work despite pain but without examining age, or factors associated with their staying at work in connection with aging but not with pain.
Yet the fact is that Western societies are facing a phenomenon of demographic aging [13,14,15]. A number of countries are therefore anticipating a labour force shortage due to insufficient numbers of younger workers to replace retirees. Several groups and government agencies in Europe and North America are proposing to implement vigorous measures to improve labour force participation and stay-at-work rates among people aged 55 years and over [16,17,18,19,20].
In the current context of labour force scarcity [21, 22], aging workers’ contribution is becoming even more vital to society [13, 15], making it imperative for us to improve our understanding of the factors that contribute to their staying at work despite pain. The objective of this study was therefore to explore the factors associated with individuals aged 55 years and over staying at work despite musculoskeletal pain.
A transdisciplinary conceptual framework was developed for this purpose, integrating literature from the fields of sociology, occupational rehabilitation and ergonomics and focussing on two populations: individuals with pain and aging workers [5, 9, 23]. The dimensions of the conceptual framework were as follows: the employment market, the legal context, the worker (i.e., personal/financial situation, health/coping skills, values associated with work) and the work itself (i.e., demands and social environment, organizational and financial factors) (Fig. 1).
Materials and methods
An interpretive descriptive qualitative study design was used. This design is indicated when the purpose is to describe a phenomenon and account for its significance particularly when little knowledge exists on the topic [24]. Also, interpretive description allows exploration of a phenomenon “with the goal of identifying themes and patterns among subjective perspectives, while also accounting for variations between individuals” [25]. Although mostly described for use in clinical contexts, this design appeared well adapted to the context of individuals working with pain.
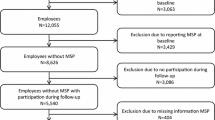
Participants were selected in two cities (Montreal and Sherbrooke) in the province of Québec, Canada, using purposive quota sampling [26]. The characteristics used to establish the quotas, based on the literature survey, were size of the organization (small, medium, or large), level of physical demands of the work (manual or mixedFootnote 1) [27] and participant gender. The inclusion criteria were (1) 55 years of age and over; (2) having worked for at least 1 year for the same employer; (3) currently working 28 h a week or more; (4) having had musculoskeletal pain often or all the time for at least 6 months, and (5) not having been on sick leave for more than 15 days in the past year. The exclusion criteria were having an acute or unstable condition, a degenerative disease or a retirement date planned within the following 6 months.
Several recruitment strategies were used. A list of employers was made available for the study, who had collaborated on previous research on work rehabilitation over the previous 10 years and had agreed to be contacted again. Human resources of these organisations were contacted directly either by telephone or email and potential participants were invited to contact the researcher via email. Social media of workers’ unions and associations were also used to reach aging workers directly. Finally, information bookmarks were distributed via the snowball sampling strategy to the participants recruited [26].
This study was approved by the Research Ethics Committee of the Centre hospitalier de l’Université de Sherbrooke (CHUS) (Canada) on November 30, 2016.
Data Collection
First, an interview guide was developed using the conceptual framework. The questions were pre-tested on individuals with characteristics similar to those of the participants sought in order to ensure clarity. Interview questions were linked to the dimensions of the conceptual framework. The interview started with questions on pain. For example, the participant was asked: How did the pain start and when? Other themes discussed were: values associated with work (e.g. What importance does work have in your life?); work means and demands (e.g. What is a regular day at work and how does it vary? What equipment is available to help you?); work organisation (e.g. What possibilities do you have to make a change in your work schedule?); managing pain at work (e.g. How do you manage working when pain gets worse?).
Each participant was met at a venue that ensured confidentiality and of his/her own choosing. A consent form was presented first and signed by the participant. Then, a one-on-one, 60-min semi-structured interview was conducted. Lastly, the participant was asked to complete two self-administered questionnaires: one on sociodemographic data and the other on pain (short version of the Nordic Musculoskeletal Questionnaire) [28, 29]. A summary of the interview was transmitted to the participant by telephone or email a week or two after the interview to obtain his/her comments. The interviews were audio-taped.
Analysis
The content of the interviews was first transcribed in its entirety by a specialized external resource. For purposes of analysing the interviews, a mixed grid was developed using the dimensions of the conceptual framework. A priori categories were developed based on the conceptual framework. For example, in the category “means demands and social environment at work”, sub-dimensions were: availability of tools or equipment, physical environment, flexibility of working hours/task organisation, work strategies, help from colleague, or other. A companion document presenting definitions and examples of each of the dimensions and sub-dimensions was also created to facilitate coding. Qualitative data analysis software was used (Atlas.ti, version 7.5). A first interview was initially coded separately by the two authors (MJD, MCR) using the coding grid, and the level of intercoder agreement was then assessed. The minimum level sought was 80% [30]. To obtain it, any points of disagreement were discussed and the definitions in the companion document were clarified as needed. The same process was followed with some of the other interviews until the desired level of agreement was obtained. A single coder (MCR) then performed the analysis.
For the actual analysis, the main steps proposed by Miles and Huberman [30] were followed: data condensation; data display; and drawing and verifying conclusions. Generally speaking, these three steps were carried out iteratively, with each one providing data for the other two.
Data Condensation
The complete transcripts were read several times to obtain an overview of the data. Points of interest were noted during the process. The content of each interview was coded using the previously developed coding grid. Emerging themes were noted and discussed throughout the coding process, and themes were clarified accordingly or added to the coding grid.
Data Display
The themes covered in each of the interviews were then presented in the form of matrices and subsequently discussed by the research team members. Each participant’s health and work trajectory was also presented in graphic form and discussed. These steps brought to light emergent themes or configurations, going beyond the results of first cycle coding of the previous step. Back-and-forth excursions took place between the data display and condensation steps to further clarify certain themes.
Drawing/Verifying Conclusions
Various groupings were tried out, based on the themes raised by the participants, in order to identify subgroups with common characteristics. For example, the type of work demands, duration of pain, social situation, and participants’ gender were used as characteristics to discern pertinent groupings. Discussions were held among team members throughout this process to draw and verify the conclusions proposed.
Results
Participants
Fourteen participants were interviewed one-on-one to discuss their experience of staying at work despite persistent musculoskeletal pain. The participants, comprising six women and eight men, were between 55 and 70 years old. The average age was 59 years (range: 55–70 years) and their pain had generally been present for a long time, in fact, for an average of 12 years (range: 2–45 years). The results of the short version of the Nordic Musculoskeletal Questionnaire [28, 29] clarified certain characteristics. The participants generally had more than one pain site, and seven of them had pain in five or more body regions. Pain intensity at interview time was rated at 6/10 or more by five participants. The body regions most frequently affected by pain were the lumbar region (11 workers), knees (9) and upper extremities (7) (Tables 1, 2).
Themes
Several themes emerged in relation to the factors associated with workers aged 55 years and over staying at work despite pain. These themes were grouped under two main dimensions of the conceptual framework: the individual and the work situation.
Individual Dimension
Three main themes were examined: the benefits of work, work representations and strategies outside work.
Benefits of Work
For the most part, the participants identified work as a source of various benefits in their lives. They saw it as bringing them—in addition to financial independence—the possibility of interpersonal relationships, self-fulfilment and recognition from others. These benefits became motivators for staying at work.
In fact, most of the participants stressed the importance of work in their lives in terms of the scope of the interpersonal relationships created: they had contact with other people, got out of the house, laughed with co-workers and even created a social network for life outside work. A change in work had enabled certain individuals to create a new social network following a divorce: … it’s the social environment, we laugh, we have fun. Now that I’m on my own … (M11).
Several also saw their work as a means of fulfilling themselves, being recognized and being useful to others, to teammates and to society at large. One participant reported it this way: … with the experience I’ve got, I bring something more to the team (M1). This participant regarded his age and experience as assets and considered that he had acquired considerable knowledge worth sharing with his co-workers. Pride in doing quality work despite their pain was also a point raised by several participants: My job is to straighten things out so that the customer no longer has to call. So that it all works (M13).
Lastly, most of the participants raised the importance of the financial benefits associated with working. They were concerned mainly about preparing financially for retirement. More than half confirmed that they had not accumulated enough money to be able to stop working immediately. Furthermore, most of the workers mentioned either being alone or having one or more dependants. A number of them intended to work for several more years so that they could eventually retire with a better income: … financially, I’m going to have to work for longer (M11). For most, while financial benefits were deemed essential, they nonetheless seemed less important than the other benefits associated with work, such as creating interpersonal relationships or feeling useful to others.
Work Representations
The participants’ mental representations of their work also appeared to be an important theme associated with their staying at work. Several of them expressed the idea that work helped them maintain their health. After having had to reduce some of their activities due to the onset of pain, these workers saw work as a means of staying in good health and even of controlling their pain. As one participant put it: It’s important not to just sit around at home. Find yourself something [to do]. Muscles need to move (M5). Other participants saw work as a way of thinking less about the pain so that it took up less room in their lives: [You have to] learn to live with the pain. Sitting at home I’m going to be in pain too. I’d prefer to still be active a bit (M3). In other words, they saw their work as a way of both improving their health and keeping their mind on other things.
Strategies Outside Work
All the participants discussed strategies they developed to stay at work and cope with the pain. In fact, on the individual level, the pain coping strategies were inextricably linked with their staying at work. They all discussed strategies, whether passive or more active, that they implemented to control their pain. Among the more passive strategies, the majority of the participants mentioned the following: consulting health professionals regularly or occasionally, taking prescription or over-the-counter pain-alleviating medication and reducing certain personal activities (e.g., housework, eating out in restaurants, small chores): … at home, I do the minimum. It’s always in the back of my mind that I need to protect my back (M1). The active pain management strategies cited included changing posture to reduce the pain and doing physical activity on a regular or an occasional basis: … I have to do my exercises every single day. Otherwise… I feel it (M5). Most of the participants chose a combination of strategies depending on their perceived efficacy and the fluctuations in their pain.
Work Situation Dimension
Two interrelated themes were examined under this dimension: all the means provided by the workplace to facilitate the workers’ staying at work and the strategies used by the workers to succeed in staying there.
Means Provided and Strategies Used at Work
The participants discussed the importance of having access to certain means or possibilities (i.e., what was offered or possible) in their work situation. Depending on the availability of these means, the workers developed stay-at-work strategies that involved their work schedule, the content of their tasks or the tools provided.
Most of the participants had access to one or more means of adapting their work schedules, such as flexible arrival or departure times, or the possibility of reducing their working hours or of taking leave as needed. Several participants mentioned using a strategy of condensing their working hours during more intense pain periods in order to have an extra day off at the end of the week. It depends on my schedule, but in any case, it’s me who decides… I try to condense it into three days … And even with that, I see the difference [strategy for having four consecutive days of rest] (M14).
All the participants also had varying degrees of access to possibilities of modifying their work tasks. These possibilities were sometimes formal, i.e., decided by the workplace, such as officially delegating a demanding task to a co-worker or avoiding assigning tasks that required too much moving around. Many task adjustments, however, were made informally and thus appeared more as individual work strategies. This could take the form of participants alternating or redistributing certain tasks in their schedule, changing their work method, taking time to plan how to perform a complex task, seeking a co-worker’s help temporarily or avoiding certain tasks altogether: Anything that’s heavy, I arrange things so that I no longer… to avoid it whenever possible (M6). Some of these strategies were made possible by a climate of goodwill within the work team: Well, we all get along. And everybody knows that we don’t want to do that all day long (M11). The participants mentioned that by using these strategies, they generally succeeded in meeting their work demands. Some individuals deployed a longer-term modification strategy, such as trying to diversify their skills in order to qualify for less demanding tasks. One participant mentioned having told his supervisor that he was interested in new tasks involving less onerous physical demands: … I told him that I’m interested … [by this other task]. When you perform that [task], you’re sitting down (M1).
Another means provided by workplaces to facilitate work was access to small pieces of equipment or tools. For example, several participants faced with mixed work demands had access to equipment such as headphones, stools or adjustable chairs, while most of the participants faced with manual tasks had access to power tools (with wires or wireless) to facilitate their work. Some workers had used the strategy of asking their direct supervisor for access to such tools following the onset of pain, while a few did not even have to make the request: … she [my supervisor] changed it for me to a slightly more ergonomic chair. More comfortable. I appreciated her gesture. She said to herself, ‘ … You can’t work on a chair like that!’ Because she could see perfectly well that I wasn’t able to find a position … (M2). Others already had access to equipment before their problem began. A handful who faced particularly heavy physical demands mentioned that it was the complete mechanisation of certain tasks that had allowed them to stay at work despite their pain.
The presence of recognized expertise in the job sector also appears to influence the possibility of having access to certain accommodations at work. This flexibility provides access to certain work adjustments, i.e., in the task content, work schedule or availability of tools and equipment. One participant, a manual labourer, mentioned having access to less physically demanding tasks because of his expertise: I’m kind of an expert. Manufacturers ask me to determine where the problem is (M13). Another reported that his current employer had recruited him for his rare expertise, and for this reason, offered him certain accommodations: reducing the number of working hours per week and avoiding weekend work, certain tasks and trips (M3).
Dimensions of the Employment Market and Legal Context
The participants did not share information about these two dimensions.
Groupings of Results
Three groupings of results emerged and were characterized by three levels of “stay-at-work cost”: low, moderate and high. This cost was determined by combining the level of difficulty experienced in meeting the work demands (from low to high) with the level of impact that staying at work had on activities outside work (from low to high), seen from the worker’s perspective (Fig. 2).
The first grouping (n = 5) corresponded to a low stay-at-work cost. The participants in this grouping gradually succeeded in performing all their work tasks in the allotted time, with intermittent symptoms that diminished to an acceptable level with rest. They generally had some means and strategies at work for distributing their tasks or enlisting help. These workers continued their usual activities outside work with relatively few limitations. They came mostly from the public sector and experienced intermittent, gradual-onset pain.
The second grouping (n = 4), associated with a moderate stay-at-work cost, included participants who experienced some difficulty meeting their work demands, but who experienced increased pain that continued after work. Moreover, these workers had to adapt their activities outside work by, for example, changing their sports or recreational activities, or dividing up the time they spent on housework or outside home maintenance. In this sub-group associated with moderate cost, three of the four participants were from the private sector, had manual-type jobs and experienced sudden-onset pain.
Lastly, in the third grouping (n = 5), associated with a high stay-at-work cost, the participants experienced difficulty performing all their work tasks. Each work day increased their symptoms despite the strategies they developed. In some instances, these symptoms diminished with rest, while in others, they remained very present. However, the biggest impact for these individuals was on their personal activities. In fact, they limited all their activities outside work to conserve their energy for staying at work. For example, some of them dropped all their sports activities, social outings and recreational activities, and significantly cut back on their household activities even when they had no help at home. This sub-group of workers took medication (both over-the-counter and prescription drugs), generally consulted health professionals in an effort to control their pain level and worked mainly in the private sector.
Discussion
This aim of this study was to explore the factors associated with individuals aged 55 years and over staying at work despite musculoskeletal pain. To date, studies have focussed on this phenomenon in connection either with pain or with aging [4, 9]. To our knowledge, ours is the first study to examine a population of aging workers who have stayed at work despite musculoskeletal pain.
The participants reported numerous factors associated with the fact of their staying at work, some related to the reasons for their decision to stay (why), and others related to the strategies and means they deployed in order to stay (how).
First, the factors cited as reasons for why they stayed, i.e., the importance of interpersonal relationships at work, the perception of being useful to their work team or to society and the need for financial independence, concur with both Limoges’ [31] findings on the benefits of work and Morin’s findings [32] on the meaningfulness of work. In fact, according to Limoges, the fact that adults hold jobs is associated with seven major benefits: financial independence, opportunity to form interpersonal relationships, self-fulfilment, time and space management, social status, the central role that work plays in an adult’s life and the fact that it gives meaning to life [31]. Our results clearly concur with the first three benefits of work described by this author. Morin [32] further underscores the characteristics of work that is meaningful to a person, including primarily relationships, usefulness and recognition, which also supports our results. Again, according to this author, the meaningfulness of work would appear to have a positive impact on workers’ commitment to their work organization and their attendance at work. This reflects the situation of the workers in our study, who were off work for fewer than 15 days during the preceding 12 months despite persistent pain.
Second, with regard to the factors influencing how they stay at work, the participants had means available or deployed strategies in the workplace or outside work. The means offered at work were either organizational (e.g., flexibility in the work schedule) or physical (e.g., availability of tools). The strategies used at work sometimes derived directly from the organizational or physical means available, i.e., the workers decided to use (or not) the means offered, depending on their needs. Other strategies were possible, in the form of more informal flexibility present in the work organization. These factors concur with the results obtained in a study by Oakman et al. (2017) on people who stayed at work despite having arthritic pain [6]. In a mixed-methods study of 35 Australian workers, the factors found to facilitate work included support from the employer, physical adjustments to the work station and possibilities of modifying the work environment.
Outside the work context, the means and strategies used by our study participants concerned mainly pain management. In fact, all of them had developed strategies for either reducing the sources of pain in their personal lives (modifying, reducing, redistributing or stopping activities) or finding external ways of reducing their symptoms (seeking medical advice, taking medication or doing exercise). Once again, these results concur with those obtained by Oakman [6], who identified the ability to develop pain management strategies as a factor associated with workers staying at work despite their arthritis. In a qualitative study of workers with musculoskeletal pain, De Vries [5] also described pain coping strategies—including taking medication, avoiding certain movements, remaining active and adopting an attitude of pain acceptance—as playing a key role in the ability to stay at work.
In summary, the factors related to the “whys and hows” associated with workers staying at work despite pain described in this study are both personal and organizational. A multiple-case study by Sanders [33] described a similar combination of work-related and personal adaptations by older manufacturing workers to help them meet work demands. This finding corresponds perfectly to the stay-at-work framework for the end of a person’s working life described by Limoges, from the guidance counselling perspective [34, 35]. This framework puts forward the notion that for individuals to stay at work, they must also implement a combination of strategies, both work-related and personal (i.e., outside work). However, as it comes from the disciplinary field of guidance counselling sciences, this framework does not factor in the impact of health problems on the stay-at-work situation of individuals in the workplace.
Our results also pointed to a factor specific to aging workers: workers whose experience and expertise are recognized by their organization appear to benefit from greater flexibility in their work. This is convergent with results from Seing et al. [36], who found that employer’s perception of the worker’s value influenced the support offered in the workplace. Such flexibility can in turn facilitate their pain management and ultimately, their ability to stay at work. This factor had not been described in the literature to date on older adults who stay at work despite pain.
Moreover, our results brought an additional notion to light: the stay-at-work cost for workers aged 55 years and over who have pain. This notion holds particular promise in a context of demographic aging where there are many such individuals in workplaces and given the inevitable rise in their numbers over the next few years [37]. For individuals associated with a low stay-at-work cost, staying at work poses no major challenge. By contrast, for workers associated with a high stay-at-work cost, a certain tension could arise as they grapple with two extremes: holding on by staying at work, or letting go by leaving their jobs. The presence of this tension in workers can be examined in light of the findings of Scheier and Carver [38] on goal attainment. According to these authors, when an illness is present, a tension exists between holding on and letting go with respect to the individual’s goals. Depending on the goal, the person will adopt a certain behaviour, then assess whether he/she is moving closer to or further away from that goal. For aging workers with pain, it would therefore be a matter of constantly assessing whether or not they are approaching their goal of staying at work and at what cost. It seems plausible that if the individual cost of staying at work becomes too high, the workers could rethink the behaviours they have adopted to attain that goal. If their pain increases, they could decide to stop all recreational activities, request certain adjustments to their work schedule or increase their doses of medication. The presence of financial pressure could also affect this tension. Thus, the behaviour chosen in order to stay at work despite a high cost could have other consequences for the person’s health and, ultimately, for workplace productivity. This also concurs with the Fear-Avoidance Model of Chronic Pain, as revised by Crombez et al. [39]. These authors state that pain avoidance behaviours cannot be examined separately as they co-exist with other (sometimes contradictory) goals pursued by the workers, which would further compound this tension experienced when they stay at work.
In addition, this notion of individual stay-at-work cost appears to complement that of the margin of manoeuver available in a work situation, as described by St-Vincent et al. [40]. According to this concept, to remain healthy, workers should benefit from some leeway for developing a variety of work strategies to meet production requirements. A sufficient margin of manoeuver would also be necessary for a healthy, sustainable return to work following sick leave for musculoskeletal disorders [23, 41]. The combination of difficulties in meeting production demands with the impact on their activities outside work means that workers associated with a high stay-at-work cost appear to have a reduced margin of manoeuver, which would likely put them at greater risk of sick leave. Yet sick leaves for MSDs in workers aged 55 and over are usually longer [42], which can create production problems for workplaces.
Lastly, this notion of stay-at-work cost, developed in the context of this study, appears promising both for pinpointing the actions needed to support staying at work and for identifying individuals at greater risk for sick leave. Health professionals could use this concept to help identify workers having most difficulty staying at work and offer them tailored support. Given that the relative weight of the factors associated with staying at work varies, as does the associated cost per person, it appears that interventions designed to facilitate staying at work should be personalized inasmuch as possible [43]. For all these reasons, individual strategies and motivations should be identified first in order to more effectively target the actions needed to support workers staying at work, while work accommodations should also be made available to all aging workers, having pain or not [44].
Strengths and Limitations
Several measures were put in place to ensure the rigour of this study: inclusion criteria chosen on the basis of the scientific literature, transcription of the interviews by a specialized external research person, validation of the interview content by the participants and assessment of intercoder reliability. Analysis was also performed systematically by following the three steps described by Miles and Huberman [30].
The composition of the sample population posed some limitations. Despite opting for a heterogeneous sample, recruitment did not allow for the participation of several women with manual jobs or several self-employed workers. The fact that participants were recruited on a voluntary basis may also have influenced the participants’ discourse in a positive direction. Moreover, the sample was only composed of French-speaking, Caucasian participants and did not include workers from other ethnocultural background. This may be linked to different socioeconomic conditions and could have influenced the reasons mentioned for staying at work. This should be considered in future research on aging workers working with pain [45].
Conclusion
Aging workers with pain stay at work for a variety of reasons and using various means and strategies. Despite common factors, the factors appear to bear different weight, depending on the person. To encourage workers to stay at work, interventions should be adapted to their motives, propose means to help them and support the strategies they adopt. It also appears essential that the individual stay-at-work cost be taken into account if we are to reduce the risk of sick leave and avoid aggravating the health consequences.
Notes
Manual occupations: in which physical activity plays a predominant role (construction jobs, unskilled labour, specialized workers, etc.).
Mixed occupations: that require the performance of either light and continuous or intense but occasional physical activities (nursing personnel, haircutters, technicians, etc.) [26].
References
Vézina M, Cloutier E, Stock S, et al. Enquête québécoise sur des conditions de travail, d’emploi, et de santé et de sécurité du travail (EQCOTESST) (Québec Survey on Working and Employment Conditions and Occupational Health and Safety) 12. Quebec: Institut de recherche Robert-Sauvé en santé et sécurité du travail, INSPQ, ISQ; 2011.
Breivik H, Collettt B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333.
Molinié AF. La santé au travail des salariés de plus de 50 ans (Health at Work for Workers over 50). In: Institut national de la statistique et des études économiques, editor. Données sociales - La société française. France 2006.
de Vries HJ, Reneman MF, Groothoff JW, et al. Factors promoting staying at work in people with chronic nonspecific musculoskeletal pain: a systematic review. Disabil Rehabil. 2012;34(6):443–458.
de Vries H, Brouwer S, Groothoff J, et al. Staying at work with chronic nonspecific musculoskeletal pain: a qualitative study of workers’ experiences. BMC Musculoskelet Disord. 2011;12(1):126.
Oakman J, Kinsman N, Briggs AM. Working with persistent pain: an exploration of strategies utilised to stay productive at work. J Occup Rehabil. 2017;27:4–14.
Smith-Young J, Solberg S, Gaudine A. Constant negotiating: managing work-related musculoskeletal disorders while remaining at the workplace. Qual Health Res. 2014;24(2):217–231.
Tveito TH, Shaw WS, Huang Y, et al. Managing pain in the workplace: a focus group study of challenges, strategies and what matters most to workers with low back pain. Disabil Rehabil. 2010;32(24):2035–2045.
Hasselhorn HM, Apt W. Understanding employment participation of older workers: creating a knowledge base for future labour market challenges. Joint Programming Initiative: More years, better lives. The potential and challenges of demographic changes. Germany: Federal Ministry of Labour and Social Affairs; 2015.
Hayutin A, Beals M, Borges E. The aging US workforce. A chartbook of demographic shifts. Stanford: CA: Stanford Center on Longevity; 2013.
Bélanger A, Carrière Y, Sabourin P. Understanding employment participation of older workers: the Canadian perspective. Can Public Policy/Anal Polit. 2016;42(1):94–109.
Sewdas R, de Wind A, van der Zwaan LGL, et al. Why older workers work beyond the retirement age: a qualitative study. BMC Public Health. 2017;17(1):672. https://doi.org/10.1186/s12889-017-4675-z.
Demers G. Le vieillissement de la main d’oeuvre et l’avenir de la retraite: Des enjeux pour tous, un effort de chacun (Workforce Aging and the Future of Retirement). In: Commission nationale sur la participation au marché du travail des travailleuses et travailleurs expérimentés de 55 ans et plus, editor. Quebec: Ministère de l’emploi et la solidarité sociale du Québec; 2011.
Stanford Center on Longevity, editor. Adapting to an aging workforce 2014. Stanford: Stanford Center on Longevity; 2014.
European Commission. Active aging and gender equality policies. The employment and social inclusion of women and men of late working and early retirement age. In: Expert group on gender equality social inclusion healthcare and long-term care issues (EGGSI), editor. Luxembourg: Publications Office of the European Union; 2010.
Federal/Provincial/Territorial Ministers Responsible for Seniors Forum. Age-friendly workplaces: promoting older worker participation. Canada: Human Resources and Skills Development Canada; 2012.
Canadian Chamber of Commerce. Encourager les aînés à continuer de travailler (Support Older Worker to Continue Working). Branché - Le porte-parole des entreprises canadiennes; 2011.
Conseil des aînés du Québec. Avis sur le maintien en emploi des travailleurs âgés de 55 ans ou plus et le retour au travail des jeunes retraités (Staying at Work for Workers age 55 and Over and Return-to-Work for Young Retirees). Quebec: Gouvernement du Québec; 2009.
European Commission. Communication from the Commission Europe 2020: A strategy for smart, sustainable and inclusive growth. Brussels: European Commission; 2010.
Gouvernement du Québec. Stratégie nationale sur la main d’oeuvre 2018–2023 (National Workforce Strategy 2018-2023). In: Ministère de l’emploi et la solidarité sociale, editor. Quebec: Gouvernement du Québec; 2018.
Emploi Québec. Bulletin sur le marché du travail au Québec - année 2017 (2017 Quebec Labour Market Bulletin). Quebec: Gouvernement du Québec; 2017.
Statistics Canada. Job vacancies third quarter 2017. Canada: Gouvernement du Canada; 2018.
Durand MJ, Vézina N, Richard MC. Concept of margin of manoeuvre in return to work. In: Schultz IZ, Gatchel RJ, editors. Handbook of return to work. From research to practice. New York: Springer; 2015.
Thorne S. Interpretive description. Qualitative research for applied practice. 2nd ed. New York: Taylor and Francis (Routledge); 2016.
Hunt MR. Strengths and challenges in the use of interpretive description: reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual Health Res. 2009;19(9):1284–1292.
Patton MQ. Qualitative research and evaluation methods. 4th ed. Thousand Oaks, CA: SAGE; 2015.
Duguay P. Lésions professionnelles indemnisées au Québec en 2005–2007. Profil statistique par industrie - catégorie professionnelle (Compensated Occupational Injuries in Quebec, 2005-2007. Statistical Profile by Industry and Professional Category) Études et recherches. Montréal: Institut de recherche Robert-Sauvé en santé et sécurité du travail (IRSST); 2012.
Descatha A, Roquelaure Y, Aublet-Cuvelier A, et al. Le questionaire de type Nordique. Intérêt dans la surveillance des pathologies d’hypersollicitation du membre supérieur (Nordic-Type Questionnaire and its Use for Upper Limb Overuse Disorder Surveillance). Documents pour le médecin du travail 2007:509–517; TF165.
Kuorinka I, Jonsson B, Kilbom A, et al. Analyse des problèmes de l’appareil locomoteur: questionnaire scandinave (Analysis of Locomotor System Disorders with the Scandinavian Questionnaire). Documents pour le médecin du travail. 1994;58:167–170.
Miles MB, Huberman AM, Saldana J. Qualitative data analysis. A method sourcebook. 3rd ed. Thousand Oaks, CA: SAGE; 2014.
Limoges J, Lemaire R, Dodier F. Trouver son travail (Finding Your Own Work). Montréal: Montreal Fides - CIM; 1987.
Morin E. Sens du travail, santé mentale et engagement organisationnel (Meaning at Work, Mental Health and Organizational Commitment). Montreal, Quebec: Institut de recherche Robert-Sauvé en santé et sécurité du travail; 2008.
Sanders M. Older manufacturing workers and adaptation to age-related changes. Am J Occup Ther. 2018;72(3):1–11.
Limoges J. Stratégies de maintien au travail et dans d’autres situations de vie (Strategies to Stay at Work and in Other Life Situations). Québec: Les éditions Septembre; 2001.
Limoges J. Pour un troisième tiers de carrière porteur de vie (For a Meaningful Last Third of Career). Vade Mecum. Sherbrooke: GGC editions; 2008.
Seing I, MacEachen E, Stahl C, et al. Early-return-to-work in the context of an intensification of working life and changing employment relationships. J Occup Rehabil. 2015;25:74–85.
Employment rate by age group-indicator [Internet]. OECD; 2018.
Scheier Michael F, Carver Charles S. Goals and confidence as self-regulatory elements underlying health and illness behavior. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. New York: Routledge; 2003. p. 17–41.
Crombez G, Eccleston C, Van Damme S, et al. Fear-avoidance model of chronic pain: The next generation. Clin J Pain. 2012;28(6):475–483.
St-Vincent M, Vézina N, Bellemare M, et al. L’intervention en ergonomie (The Ergonomic Intervention). MultiMondes IRSST, editor. Quebec; 2011.
Durand MJ, Vézina N, Baril R, et al. Relationship between the margin of manoeuvre and the return to work after a long-term absence due to a musculoskeletal disorder: an exploratory study. Disabil Rehabil. 2011;33:1245–1252.
Commission de la santé et de la sécurité du travail (CSST). Portrait des lésions professionnelles chez les travailleurs de 55 ans et plus 2002-2011 (Professional Injuries in Workers Age 55 and Over, from 2002 to 2011). In: Équipe des études et analyses du Centre de la statistique, editor. Quebec: CSST; 2014.
Kooij DTAM, Tims M, Kanfer R. Successful aging at work: the role of job crafting. Aging workers and the employee–employer relationship. Cham: Springer; 2014.
Gignac M, Kristman V, Smith P, et al. Are there differences in workplace accommodation needs, use and unmet needs among older workers with arthritis, diabetes and no chronic conditions? Examining the role of health and work context. Work Ageing Retire. 2018;4(4):381–398.
Coté D, Dubé J, Gravel S, et al. Cumulative stigma among injured immigrant workers: a qualitative exploratory study in Montreal (Quebec, Canada). Disabil Rehabil. 2019;26:1–14.
Acknowledgements
The authors wish to thank the following organizations for their financial support: the Équipe de recherche interdisciplinaire sur la prévention et la réduction de l’incapacité au travail (ÉRIPRIT, or Interdisciplinary research team on work disability and reduction), the Institut de recherche Robert-Sauvé en santé et sécurité du travail (IRSST) and the Fonds de recherche du Québec en santé (FRQS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Richard, MC., Durand, MJ. Workers Age 55 and over Working with Pain. A Descriptive Interpretive Study. J Occup Rehabil 30, 211–220 (2020). https://doi.org/10.1007/s10926-019-09865-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-019-09865-y