Abstract
Purpose To describe factors associated with RTW in patients 2–5 years after stroke. Methods Cross sectional study, including patients 2–5 years after hospitalization for a first-ever stroke, who were <65 years and had been gainfully employed before stroke. Patients completed a set of questionnaires on working status and educational level, physical functioning (Frenchay Activities Index, FAI), mental functioning (Hospital Anxiety and Depression Scale, HADS), Coping Orientations to Problems Experienced, (COPE easy) and quality of life (Short-Form(SF)-36 and EQ(Euroqol)-5D). Caregivers completed the Caregiver Strain Index (CSI). Baseline stroke characteristics were gathered retrospectively. Baseline characteristics and current health status were compared between patients who did and did not RTW by means of logistic regression analysis with odds ratios (OR) and 95 % confidence intervals (CI), adjusted for age and gender. Results Forty-six patients were included, mean age of 47.7 years (SD 9.7), mean time since stroke of 36 months (SD 11.4); 18 (39 %) had RTW. After adjusting for age and gender a shorter length of hospitalization was associated with RTW (OR 0.87; CI 0.77–0.99). Of the current health status, a lower HADS depression score (0.76; 0.63–0.92), a less avoidant coping style (1.99; 0.80–5.00), better scores on the FAI (1.13; 1.03–1.25), the mental component summary score of the SF36 (1.07; 1.01–1.13), the EQ5D (349; 3.33–36687) and the CSI (0.68; 0.50–0.92) were associated with the chance of RTW. Conclusions A minority of working patients RTW after stroke; a shorter duration of the initial hospitalization was associated with a favorable work outcome. The significant association between work status and activities, mental aspects and quality of life underlines the need to develop effective interventions supporting RTW.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to data from the World Health Organization, 9.0 million people experience a first-ever stroke each year; the estimated prevalence of moderate and severe disability due to stroke worldwide, concerns the age group 0–60 years in 43 %, as compared to the age group of 60 years and older. [1]. Despite important improvements in the treatment of stroke including thrombolysis, its impact on patients’ lives is often considerable in different domains of functioning, due to significant cognitive, emotional and/or physical impairments in many patients [2–5]. Work disability is a major consequence of stroke at the participation level. In four systematic reviews, return to work rates after stroke reported in clinical studies varied between 11–85 % [6], 19–73 % [7], 22–53 % [8] and 0–100 % [9], respectively. This variation is explained by differences among the study populations, the definitions of work, and the duration of follow-up.
Work disability resulting from stroke may have considerable negative consequences for quality of life and self-esteem in individual patients [10–12]. In addition, loss of gainful work and productivity has an important impact on the societal level, contributing substantially to the economic burden of stroke [13, 14]. Therefore, it is important to examine which factors are associated with return to work, some of which may be modifiable.
Several health outcome factors were found to be related to the chance of return to work including fatigue [15], physical disability [8, 19], independence in activities of daily life (ADL) [6, 17] and depression [6, 7]. Furthermore, prestroke characteristics such as socioeconomic status [18], educational level [7], and work characteristics such as factory size [19] were of influence. Study populations in literature consist of patients admitted to a hospital [15–17], of patients who successfully resumed work after stroke [18] or were population based [19, 20]. Mean follow up period in the hospital based studies was less than 2 years, which is relatively short considering the procedures that can be involved in the process of resuming work.
Little is known about the chances of returning to work on the longer term. The objective of this study was to determine factors associated with sustained return to work 2–5 years after stroke in a hospital based population in the Netherlands.
Methods
Study Design
The present study on return to work was part of a larger, cross sectional study on the long-term outcomes of stroke, executed at the Medical Centre Haaglanden (MCH), a large teaching hospital in The Hague, The Netherlands. This hospital has a specialized neurovascular department.
Data about the actual situation of patients at time of the study were collected by means of a questionnaire. Additional medical information was extracted retrospectively from the participants’ medical records. As the study concerned the completion of a survey once-only, and patients were free to respond or not, the study was judged to fall outside the remit of the Medical Research Involving Human Subjects Act by the Medical Ethics Review Committee South West Netherlands, and a written exemption from ethical approval was obtained. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 [21]. Informed consent was obtained from all patients for being included in the study.
Patients
For the larger cross sectional study, all patients hospitalized for a stroke in the hospital between January 2008 and December 2010 were identified from the hospital registries. From patients who had been hospitalized for a stroke more than once during the study period, only the first hospitalization was taken into account. Then, a further selection was done using the following inclusion criteria: a. first ever ischemic or haemorrhagic stroke; b. age 18–65 years at the time of hospitalization; c. having a paid job at the time of hospitalization. Exclusion criteria were: a) traumatic brain injury, cerebral neoplasms or transient ischemic attack (TIA); b) medical condition not allowing participation (patients in a vegetative state); c) insufficient Dutch language skills; and d) age retired at time of the study. Subsequently, of all potentially eligible patients the hospital and town council registries were checked to identify any deceased patients.
The patients who were subsequently considered eligible were invited by the treating physician to participate by means of a letter and an information leaflet. Participation included a questionnaire about their current health status and the completion of one questionnaire by their spouse or other caregiver, if applicable. They were asked to return the questionnaire and a signed informed consent form using a pre-stamped envelope. In case of no response after 4 weeks patients were contacted by telephone by a research nurse.
Assessment Methods
Stroke Characteristics
Data about the type of stroke (hemorrhagic/ischemic), lateralization (left hemisphere/right hemisphere/vertebrobasilar), impairment at stroke onset and at discharge from hospital (Barthel Index; score range 0–20) [22], and duration of hospitalization were collected retrospectively from the medical records of the hospital.
Sociodemographic Characteristics
The survey comprised questions on the following sociodemographic characteristics: age, sex, and educational level (Low: up to and including lower technical and vocational training; Medium: up to and including secondary technical and vocational training; and High: up to and including higher technical and vocational training and university).
Work Status Before Stroke and at Present
Work status (working yes/no) before stroke was extracted from the medical records. Patients were asked to fill in the Work Productivity and Activity Impairment Questionnaire General Health (WPAI) [23]. The WPAI was created as a patient-reported quantitative assessment of the amount of absenteeism (absent from work due to health problems), presenteeism (present at work) and daily activity impairment attributable to general health (Dutch version: http://www.reillyassociates.net/WPAI_Translations.html; accessed October 23, 2015). The questionnaire has 6 questions: Q1 = currently employed; Q2 = hours missed due to health problems; Q3 = hours missed due to other reasons; Q4 = hours actually worked; Q5 = degree health affected productivity while working (0 = no effect, 10 = work not possible); and Q6 = degree health affected regular activities other than work (0 = no effect, 10 = daily activities not possible). Patients without paid employment answered only the first question and the last question of the WPAI.
Psychological and Physical Functioning
Anxiety and depression were measured by means of a Dutch version of the Hospital Anxiety and Depression Questionnaire (HADS [24], Dutch version [25]) which contains two 7-item scales, one for anxiety and one for depression, both with a score range of 0–21. A higher score means higher level of depression or anxiety. For screening purposes on depression in stroke patients a cut off >5 is recommended [26].
Coping was measured using the CopeEasy (Coping Orientations to Problems Experienced), a self-reported questionnaire of 32 items, in an ordinal scale from 1 to 4 [27, 28]. It describes the extent to which three different types of coping strategies are used by patients to deal with their situation: Active, Avoiding and Seeking Support. Higher scores mean the patient uses this coping strategy more.
Physical functioning was measured using the FAI (Frenchay Activity Index) [29, 30]. This inventory scores the frequency of 15 activities on a 4 point scale (range 0–3, never—frequently). The maximum score is 45 points and represents the highest level of functioning.
Health Related Quality of Life
The SF-36 is a generic instrument with 36 items covering eight domains (physical function, role physical, bodily pain, general health, vitality, social function, role emotional, and mental health). The SF-36 subscale scores range from 0 to 100, with a higher score indicating better health status. From these, a physical and a mental summary scale can be computed. Scoring of the summary scales is undertaken by weighting and summing the original eight dimensions. These weights are gained from factor analysis of data from a general population. The SF-36 has been translated and validated by Aaronson et al. [31] into a Dutch version.
Patients described their general health status using the EuroQol classification system (EQ5D), consisting of 5 questions on mobility, self-care, usual activities, pain/discomfort, and anxiety/depression [32]. From the EQ5D classification system, the EQ5D utility index was calculated. The five 3-point Likert questions of the EQ-5D yield a summary score ranging from −0.329 (no health) to 1 (full health).
Caregiver Strain
Caregiver strain was measured using the Caregiver strain index (CSI): This questionnaire consists of 13 items to assess the subjective care load of the caregiver [33], range from 0 to 13; higher means more caregiver strain. A score of seven or more indicates a high level of strain. The CSI was validated in a Dutch stroke population [34].
Analysis
Descriptive statistics were used for the sociodemographic and stroke characteristics, work status, measures of functioning and quality of life, and caregiver strain [mean (SD) or median (inter quartile range; IQR)]. Differences among working (RTW group) and non-working (non-RTW group) stroke patients at 2–5 year follow-up were analyzed by means of logistic regression analyses. Analyses were done by univariate logistic regression (crude OR) and again per variable by multivariable logistic regression to adjust for potential confounders (age, gender). Independent variables were categorized into characteristics of stroke at baseline (type of stroke, localization, length of hospitalization, and Barthel Index at admission and discharge) and into measures of the patient’s current health status and caregiver strain (HADS, CopeEasy, FAI, SF-36, EQ5D, and CSI). Results were reported as odds ratios (OR) with the 95 % confidence interval (CI).
Statistical analyses were performed using IBM SPSS Statistics, version 22 (Leiden, the Netherlands, 2015).
Results
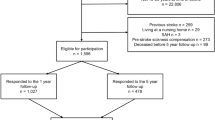
The flow of participants in this study is shown in Fig. 1. Out of 576 subjects who were considered eligible and were invited to participate in the larger study, 207 (36 %) responded.
Of those, 102 (49 %) were under 65 years at the time of stroke, of whom 57 (56 %) were gainfully employed at that time. At follow up 11 were retired (age related), so 46 patients met the inclusion criteria and were eligible for the present analysis.
Baseline Characteristics and Chance of Return to Work
The baseline characteristics of the 46 patients are presented in Table 1. Mean age was 47.7 years (SD 9.7, range 20–90 years) and the mean time since stroke was 36.0 months (SD 11.4). Logistic regression showed a significant difference in the length of stay in the hospital; the RTW group was hospitalized shorter than the non-RTW group (median 6.5 days (IQR 6) vs. 10 days (9); OR 0.87, CI 0.77–0.99). No significant differences were found with respect to age, gender, educational level, and type and localisation of the lesion. After adjustment for age and gender the results did not change in general. Only the Barthel Index at discharge showed a trend towards group difference, the RTW group had better scores but this was not significant (p < 0.10).
Current Health Status and Chance of Return to Work
The RTW group scored better on most outcome measures 2–5 years after stroke compared to the non-RTW group (Table 2). RTW patients scored lower than the non-RWT group on depression and anxiety (HADS; depression [mean 3.3 (SD 3.1) vs. 8.6 (5.4); anxiety 4.9 (3.4) vs. 8.7 (5.7)] and were less avoidant in their coping [Cope Easy 1.6 (0.6) vs 2.1 (0.6)]. The RTW patients performed better in daily life activities [FAI 30.6 (7.3) vs 22.6 (9.9)] and had a better quality of life [MCS of the SF-36 48.8 (10.3) vs. 37.3 (15.4); EQ5D 0.86 (0.12) vs. 0.64 (0.28)]. Their caregivers showed a lesser burden [CSI 2.4 (2.3) vs. 6.3 (3.8)]. These differences remained unaltered after correcting for age and gender, except for anxiety (OR 0.85, CI 0.73–1.00).
Work Status and Work Productivity
Eighteen of the 46 patients (39 %) returned to work. Table 3 shows the amount of absenteeism, presenteeism and daily activity among these patients as measured with the WPAI. On average patients worked 29.6 h a week. Only one patient missed working hours in the week before follow up due to health problems and one due to other factors. Patients reported only a mild effect of health problems on productivity while working. Question 6 of the WPAI was answered by all patients (degree health affected regular activities other than work, 0 = no effect—10 = daily activities not possible). The RTW group scored significantly better on this aspect compared to the non-RTW group (median 1 (IQR 4) versus 6 (IQR 5); OR 0.68 (CI 0.53–0.87).
Discussion and Conclusions
This cross sectional study among 46 premorbidly employed stroke patients showed that after a follow up of 2–5 years, 39 % was able to return to work. The patients that returned to work scored better on the Hospital Anxiety and Depression Scale, were less avoidant in their coping, and showed a higher quality of life and a higher level of daily activities.
Previous studies reported varying RTW rates. Daniel et al. [9] reported in a review of 70 studies (8810 patients) an average RTW rate of 44 % (range 0–100 %). These studies were performed in different countries all over the world and in a large timeframe (1962–2008); study populations were hospital based, population based or originated from rehabilitation centres. In hospital based populations return to work varied from 55 to 75 % [15–17]. Our data, showing a lower RTW rate (i.e. 39 %), were collected in a period of economic decline and higher unemployment rates in the Netherlands which may be of influence; the unemployment rate doubled from 2008 to 2013 [35]. Furthermore, social security in the Netherlands offers a sufficient allowance for those who cannot return to work; this can also influence the RTW rate. In accordance with our results are the results of a study in an urban population using data from the South London Stroke Register, which reported a RTW rate of 35 % at 1 year post-stroke [36].
Current literature mentions severity of stroke as an important negative predictor of return to work. The length of hospitalization is mentioned previously as a relevant indicator for RTW in stroke [8], as could be confirmed in our results. A strong association was found between RTW and regular daily activities, as measured by the FAI. The actual score on the FAI, a measure of daily activities, reflects the impact of stroke at the time of follow up. The FAI seems stable in the chronic phase of stroke (>1 year after stroke) and appears to be a good indicator of social activity, e.g., work, in the long term [37].
Quality of life as assessed by the SF-36 MCS was also lower in the non-RTW group, while the physical component score of the SF-36 did not differ significantly. High scores for depression on the HADS were found in the non-RTW group. This could reflect the importance of mental factors in the process of returning to work and may lead to consequences in terms of treatment strategies. Depression after stroke is associated with lower RTW rates at a later stage [6, 7, 38]. On the other hand, unemployment probably has a negative influence on mental health [10–12].
A clinical cut off was provided for the HADS (>7) by Zigmond et al. [24]. Based on this cut off a majority of the patients in the non-RTW group (15 patients, 54 %) was at risk of a clinical relevant depression. Three patients in the non-RTW group consulted a psychiatrist in the last 6 months; in the RTW group no patient did.
Failure to return to work is correlated to a higher strain for their caregivers. The common factor could be the HADS which is in our results closely related to RTW as well as to the CSI. This is in line with results of Smeets et al. [39] where the HADS and the CSI were correlated 1 year after acquired brain injury.
There are limitations that have to be considered. Due to the cross sectional design of this study causal relations can not be inferred. Moreover, the study population of 46 patients is relatively small. Detailed information about work prior to stroke was not available, nor the moment patients were able to resume their work. It is possible that patients were not able to return to work for other reasons. The longer the follow up period is, the more influence will be seen from other factors such as comorbidity. A larger prospective study can shed more light on factors that are of influence in the process of returning to work, but still will have limitations to which extent relations can be accounted for as causal.
In conclusion, the chance of return to work after stroke relates positively to less initial stroke severity and better outcomes with respect to activities, mental aspects and quality of life. The inability to return to work is related to a high caregiver strain. These results may give guidance to the rehabilitation goals of patients. In the patient group that did not RTW in the chronic phase after stroke, extra attention should be paid to mood disturbances and to the caregivers.
References
The Global Burden of Disease. 2008. Available from (http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf).
Nakayama H, Jørgensen HS, Raaschou HO, Olsen TS. Recovery of upper extremity function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil. 1994;75:394–8.
Jang SH. The recovery of walking in stroke patients: a review. Int J Rehabil Res. 2010;33(4):285–9.
Kwakkel G, Kollen BJ. Predicting activities after stroke: what is clinically relevant? Int J Stroke. 2013;8(1):25–32.
D’Aniello GE, Scarpina F, Mauro A, Mori I, Castelnuovo G, Bigoni M, et al. Characteristics of anxiety and psychological well-being in chronic post-stroke patients. J Neurol Sci. 2014;338(1–2):191–6.
Wozniak MA, Kittner SJ. Return to work after ischemic stroke: a methodological review. Neuroepidemiology. 2002;21(4):159–66.
Treger I, Shames J, Giaquinto S, Ring H. Return to work in stroke patients. Disabil Rehabil. 2007;29(17):1397–403.
Wang YC, Kapellusch J, Garg A. Important factors influencing the return to work after stroke. Work. 2014;47(4):553–9.
Daniel K, Wolfe CD, Busch MA, McKevitt C. What are the social consequences of stroke for working-aged adults? A systematic review. Stroke. 2009;40(6):e431–40.
Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. J Rehabil Med. 2003;35(3):127–31.
Roding J, Glader EL, Malm J, Lindstrom B. Life satisfaction in younger individuals after stroke: different predisposing factors among men and women. J Rehabil Med. 2010;42(2):155–61.
Morris R. The psychology of stroke in young adults: the roles of service provision and return to work. Stroke Res Treat. 2011;534812.
Saka O, McGuire A, Wolfe C. Cost of stroke in the United Kingdom. Age Ageing. 2009;38(1):27–32.
Di Carlo A. Human and economic burden of stroke. Age Ageing. 2009;38(1):4–5.
Andersen G, Christensen D, Kirkevold M, Johnsen SP. Post-stroke fatigue and return to work: a 2-year follow-up. Acta Neurol Scand. 2012;125(4):248–53.
Saeki S, Toyonaga T. Determinants of early return to work after first stroke in Japan. J Rehabil Med. 2010;42(3):254–8.
Hackett ML, Glozier N, Jan S, Lindley R. Returning to paid employment after stroke: the Psychosocial Outcomes In StrokE (POISE) cohort study. PLoS ONE. 2012;7(7):e41795.
Brey JK, Wolf TJ. Socioeconomic disparities in work performance following mild stroke. Disabil Rehabil. 2015;37(2):106–12.
Hannerz H, Ferm L, Poulsen OM, Pedersen BH, Andersen LL. Enterprise size and return to work after stroke. J Occup Rehabil. 2012;22(4):456–61.
Walsh ME, Galvin R, Loughnane C, Macey C, Horgan NF. Community re-integration and long-term need in the first 5 years after stroke: results from a national survey. Disabil Rehabil. 2014;13:1–5.
http://www.wma.net/en/30publications/10policies/b3. Accessed 23 Oct 2015.
Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10:61–3.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–65.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatry Scand. 1983;67:361–70.
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–70.
Turner A, Hambridge J, White J, Carter G, Clover K, Nelson L, Hackett M. Depression screening in stroke: a comparison of alternative measures with the structured diagnostic interview for the diagnostic and statistical manual of mental disorders, fourth edition (major depressive episode) as criterion standard. Stroke. 2012;43(4):1000–5.
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–83.
Kleijn WC, Heck GLv, Waning Av. Ervaringen met een Nederlandse bewerking van de COPE copingvragenlijst [Use of the Dutch version of the COPE questionnaire]. De COPE_Easy. Gedrag en Gezondheid. 2000;28:213–26.
Wade DT, Legh-Smith J, Langton Hewer R. Social activities after stroke: measurement and natural history using the Frenchay Activities Index. Int Rehabil Med. 1985;7(4):176–81.
Post MW, de Witte LP. Good inter-rater reliability of the Frenchay Activities Index in stroke patients. Clin Rehabil. 2003;17(5):548–52.
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–68.
EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
Robinson BC. Validation of a Caregiver Strain Index. J Gerontol. 1983;38(3):344–8.
van Exel NJ, Scholte op Reimer WJ, Brouwer WB, van den Berg B, Koopmanschap MA, van den Bos GA. Instruments for assessing the burden of informal caregiving for stroke patients in clinical practice: a comparison of CSI, CRA, SCQ and self-rated burden. Clin Rehabil. 2004;18(2):203–14.
http://www.cbs.nl/nl-NL/menu/themas/arbeid-sociale-zekerheid/publicaties/arbeidsmarkt-vogelvlucht/default.htm. Accessed 16 Jan 2016.
Busch MA, Coshall C, Heuschmann PU, McKevitt C, Wolfe CD. Sociodemographic differences in return to work after stroke: the South London Stroke Register (SLSR). J Neurol Neurosurg Psychiatry. 2009;80(8):888–93.
Jansen HE, Schepers VP, Visser-Meily JM, Post MW. Social activity one and three years post-stroke. J Rehabil Med. 2012;44(1):47–50.
Glozier N, Hackett ML, Parag V, Anderson CS. The influence of psychiatric morbidity on return to paid work after stroke in younger adults: the Auckland Regional Community Stroke (ARCOS) Study, 2002 to 2003. Stroke. 2008;39(5):1526–32.
Smeets SM, van Heugten CM, Geboers JF, Visser-Meily JM, Schepers VP. Respite care after acquired brain injury: the well-being of caregivers and patients. Arch Phys Med Rehabil. 2012;93(5):834–41.
Acknowledgments
We are indebted to Anne Hanschke, research nurse Landsteiner Institute, The Hague for her assistance with the data collection and to Cedric Kromme, data manager of Sophia Rehabilitation Centre, for his support with the electronic database.
Funding
This study was financially supported by the Research fund Medical Center Haaglanden, the Netherlands.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HJ Arwert declares he has no conflict of interest. M Schults declares he has no conflict of interest. J Meesters declares he has no conflict of interest. R Wolterbeek declares he has no conflict of interest. J Boiten declares he has no conflict of interest. T Vliet Vlieland declares she has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Arwert, H.J., Schults, M., Meesters, J.J.L. et al. Return to Work 2–5 Years After Stroke: A Cross Sectional Study in a Hospital-Based Population. J Occup Rehabil 27, 239–246 (2017). https://doi.org/10.1007/s10926-016-9651-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-016-9651-4