Abstract
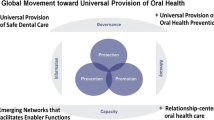
Oral health is a critical component to overall quality of life. Recommendations and guidelines for oral health continue to evolve while remaining underutilized worldwide. Still, oral healthcare parity and equity are achievable. This public health priority must be supported with stronger research, service delivery must be equitable and transparent, and the impact of oral healthcare must be fully understood. Data, surveillance, evidence and translation must be improved for oral health specialties as well as for greater global governance. Further, interdisciplinary coordination between orthodontic, dentistry, medical, biotechnology and research organizations must be prioritized. With dedication and consistent approach, oral healthcare can achieve the best outcomes for quality of life and cost effective public health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Oral healthcare is as important as general medicine for health quality of life. The provision and integration of oral health must be delivered in a manner that is accessible, evidential and impactful. Achievement of oral health parity can be accomplished through stronger research, innovation funding, workforce preparation and delivery improvement.
Oral healthcare has increasingly become a focus for public health services. Proper dental and oral care continue to remain out of reach for much of the global population. In fact, it was over a decade ago that the United States Surgeon General highlighted major findings and key action items for oral health. Agendas within Healthy People 2020 and World Health Organization (WHO) have matched goals to encourage oral healthcare through policy development, public health infrastructure build-outs, access to oral healthcare, preventative services and monitoring/surveillance systems. Specific targets of these goals include fluoride programs, oral health education campaigns, reduction of dental caries and periodontal disease, reduction of oral and pharyngeal cancers, and general protection from oral injury [1, 2]. Notably, the proposed framework continues to be part of national and global aspiration rather than a realization [3].
In the past, oral health was poorly defined and often focused on teeth and mouth care. Research, surveillance, services and education were segregated in a less than ideal system. Modern acceptance of oral healthcare includes the prevention and attention to diseases of the mouth, teeth, craniofacial tissues and surrounding areas. Expanded definitions have been addressed in the U.S. Surgeon General report from 2000. In 2016, an expanded definition was adopted by the Fédération Dentaire Internationale (FDI) World Dental Federation. This expanded definition of oral healthcare has determined that oral healthcare consists of an individual’s ability to speak, smile, swallow, taste, touch, chew and convey emotions through facial expressions without pain, discomfort or disease of the craniofacial complex [4]. The individual’s oral health changes throughout the lifespan. All components, including physiological, social and psychological, are pillars of this care [4].
Current Trends
The current issues that surround oral healthcare must be understood as recommendations and guidance for improvements are introduced. Oral health impacts overall individual health. Despite this evidence, oral healthcare remains out of reach for much of the world’s population. Cost is a major barrier. Inequalities among populations persist. Additionally, expanded definitions and stronger understanding of interdisciplinary needs have brought the vast, varied wide range of oral health to light. With this comprehensive interpretation comes expanded analyses, intervention and surveillance. Still, expansion of definition has brought major opportunity to greatly improve overall human health through integrated, targeted oral health improvements. The future has never been brighter. Understanding of current oral health issues is a necessary foundation to this bright future.
Oral health research continues to evolve. Though there is evidence of oral health impact on general disease, it is known that oral healthcare is associated with systemic disease. Periodontal infection may be an independent risk factor for diseases including cancer, cardiovascular disease, pulmonary disease, dementia, adverse pregnancy outcomes and diabetes [5, 6]. Poor oral health can be painful, reduce quality of life, affect self confidence and create psychological stress. Orofacial pain impairs oral health-related quality of life [7,8,9]. Further, poor oral health impacts nutritional intake. Around the world, 30% of people aged 65–74 have no natural teeth [1], and this is a clear contributor to malnourishment. Poor nutrition can increase mortality and affect quality of life [5]. Delays in care, as well as substandard guideline development and adherence, contribute to poor oral cancer prognosis. These issues also contribute to advanced cancer trajectories [10, 11]. Finally, poor oral health impacts infectious disease processes. Aspiration of bacteria can cause lung infections, and aspirated biological mediators can stimulate inflammation and increase susceptibility of infection [12]. The prevention of pneumonia and bacterial lung infections have been the focus even in hospital care, where specific orders for administered oral care have become standard and accompanied by evidence [13].
Oral health and dental care remain out of reach for many people. Oral cancer and caries increases of an average of 45.6% from 1990 to 2010 were similar to that of the non-communicable disease increase of 69% during the same period [14]. During this time, the extent of unmet oral healthcare needs continued to be captured. In 2008, 4.6 million children in the United States did not receive necessary dental care due to affordability [15]. Within the U.S. Surgeon General’s report, it was found that the ratio of medically uninsured children to those without dental insurance was one to 2.6, and for every adult without health insurance there were 3 adults without dental insurance [6]. Globally, lack of access to oral care and improper oral healthcare remain major public health burdens.
A primary measure to determine access and delivery is that of dental caries and decay, missing and filled teeth (DMFT). Other statistics also assist in delivery analyses. Around the world, 60–90% of children and 100% of adults have dental cavities, 15–20% of middle aged adults have severe periodontal disease and between 1 and 10 per 100,000 persons is affected by oral cancer [1]. Preventative and restorative care are not often priorities in many countries worldwide, even among those with a high prevalence of insurance coverage. While there is a significant lack of data in access and utilization of oral healthcare worldwide, labor ratios provide insight. For example, the dentist to population ratio for Africa is about 1:150000, while in industrialized countries the ratio averages 1:2000 [16].
There are many barriers to oral healthcare. These barriers primarily center on access, cost and public health prioritization. Barriers to medical oral healthcare are similar to barriers in any other aspect of medical care, including access, cost and treatment limitations.
Barriers to dental care are also just as clear. According to a recent Health Resources and Services Administration (HRSA) report, over half of the U.S. population didn’t see a dentist within the past year. Dental care and oral maxillofacial care can be costly, even for industrialized countries that experience reimbursements through insurance. In the U.S., 38% of retired persons do not have dental coverage. Additionally, there are over 4000 geographic locations in the U.S. that are considered shortage areas without enough dental professionals [17]. In fact, most countries do not have sufficient dental labor to maintain demand [18]. Notably, WHO calculates dentist to population ratios as 1 dentist for 1000 persons, WHO acknowledges industrialized country average ratios of 1:2000 and HRSA uses a standard ratio of 1 dentist to 3000 persons [17, 18]. Access to care and the standardization of access expectations are varied, and access is a primary barrier to oral healthcare.
Dental care is costly. In a recent study of low and middle income countries (LMIC), 35% incurred a household dental expense within a 4 week time period, and 7% of households insured a catastrophic expense. A catastrophic expense is defined as 40% or higher of household capacity to pay [19]. In LMIC, the impact of dental payments is similar to other general healthcare financial impacts, yet lower than hospitalizations and medication cost impacts [20]. Direct global costs of dental treatment due to diseases are estimated at USD $298 billion annually, and indirect costs are estimated at USD $144 billion annually [21]. Costs are factored into access and care, and costs are a major barrier for individual oral healthcare.
Preventative care is a main focus of oral healthcare, with emphasis on artificial fluoride in water, evidence based home care, oral health screenings and regular professional dental services. Secondary and tertiary oral healthcare emphasize proper dental procedures, proper oral maxillofacial diagnosis, treatment trajectories and the continued improvements in oral healthcare innovation. Overall, there has been great achievement in oral healthcare with many improvement opportunities on the horizon.
Preventative action is often maximized for the public regardless of access to professional services. A primary means to achieve dental health without professional dentist labor is that of fluoridation. Fluoride treatments in public drinking water are considered a major contributor to the protection against dental caries. Additionally, fluoride additions in toothpaste assist in protecting teeth. However, access to toothpaste and proper dental care is limited in various countries and dependent on cost. Access to fluoride in drinking water also depends on a country’s resources. In 2012, 377,655,000 persons in 25 countries received artificial fluoridation, or about 5% of the world’s population. An additional 280 million people reside in countries with natural fluoridation, though not all these countries experience natural fluoridation at best levels [22]. Efforts to maximize proper fluoridation of water must be balanced with evidence and risk. Excessive fluoride levels in water also may contribute to major dental issues, and many countries do not have capabilities to safely remove this harm. To add to the consideration, variant levels of access to in home routine care, such as mouthwash and toothpaste, contribute to proper or improper oral healthcare [23]. These variants may affect fluoride success. There are major fluctuations in the world’s public health approaches to fluoridation and there is wide variance in barriers in the achievement of proper care.
As global oral health expands, care must be taken to align specialties in scope, credentialing and definition. Expanded definitions of oral health have brought greater depth in accounting of the specialty. Throat and neck diseases are often incorporated into ear, nose and throat (ENT) and otolaryngology specialities. In the oral health expanded definition, pharyngitis, esophageal cancer, facial muscle disorders, vocal cord disorders and trigeminal neuralgia must all be accounted for. Yet, these disorders are not widely reported in current oral health analyses; they are often placed in rare disease, ENT or communication disorder specialities.
Oral and maxillofacial care is broad yet specialized. As previously stated, oral health definitions have expanded to include oral and maxillofacial disease, as well as diseases requiring craniomaxillofacial surgery. Oral and maxillofacial surgery (OMS) is considered a specialty, with or without cranial influence, and current training in OMS varies by country. Within the U.S. some OMS training does not include a medical degree, while in other developed countries there is a requirement of general surgery involved [24]. Additionally, an oral surgeon may or may not have specialties in head and neck issues such as cancer or genetic disease. Wide variances in training and scope of practice cause fraction in care, confusion in reimbursement and policies and these variances threaten data surveillance and analysis accuracy. It is difficult to set standards, quality metrics, reimbursement policies or supply and demand without accuracy in credentialing. It is nearly impossible to create evidence based guidance in service delivery. It is difficult to implement, interpret and coordinate interdisciplinary research as well. Oral and maxillofacial specialities that include cosmetic surgery trauma care, oncology, pathology and dentistry all should be standardized and well understood by both academia and service industry.
Inequalities in oral health services are severe worldwide. Resource inequalities are substantial and intense. It has been projected that if left unaddressed, the level of dental caries in disadvantaged countries and populations will increase [23]. Inequitable care in LMIC are rooted in access to services and lack of preventative care. Inequities in the U.S. have been observed for quite some time, with the U.S. Surgeon General’s 2000 report providing a detailed analysis on the issue. The CDC reports that poor oral health is seen most in minority populations, specifically those categorized as non-hispanic blacks, hispanics, american indians and alaskan natives [25]. Children of immigrants and refugees in the U.S. experience poorer dental outcomes [26] compared to the general population, information that is consistent with worldwide refugee research. Researchers have determined that refugees bear significant oral healthcare burden compared to general public populations [27]. Too, parents of children with public insurance in the U.S. report more often that their children have dental problems [28]. This mirrors CDC reports that there are health disparities among children, with reports that Mexican American and black, non-hispanic children are more likely to experience dental decay [25]. Education status is also a determinant of inequity in the U.S. Adults in the U.S. without a high school education are three times more likely to have untreated dental decay and destructive periodontal disease [25]. Income inequality appears to be tied to oral health disparity on many levels, and a recent U.K. study found income inequality as a contributor both independent of and alongside other variables [29]. Worldwide, those in less developed countries experience worse oral health outcomes such as decay, advanced cancer and total loss of teeth [1]. Understanding and addressing disparities in oral healthcare are of continued effort.
There is also significant variance in oral cancer seen worldwide, including variance in specific types of cancer. Even between regions in the United States, the difference in oral cancer mortality can be as high as five fold. Differences between countries in the European Union are reportedly even greater in variance. Countries that experience higher rates of smoking, tobacco use and alcohol use may see higher rates of oral cancer, though there is a significant lack of consistent data [30]. Minorities and those without adequate health insurance or access are often disproportionately affected by advanced oral cancer disease, as well. In the United States, five year survival rates are higher for white persons than black persons [11]. Delays in diagnostics, delays in specialty follow up visits and lack of consistent guidance all contribute to oral cancer progression [31]. These are delays also studied in healthcare inequity and disparity observations. European five- year survival rates for oral and oropharynx cancers are 50%, while developing countries are projected to have lower rates [31].
Although action items, surveillance and oral health interventions continue worldwide, there is no consistent follow up on set agendas. In fact, the Surgeon General report from 2000 has not been formally updated. Too, specific measures provided in WHO and Healthy People 2020 reports are not annually evaluated and reported on. Notably, interdisciplinary oral health strategies are not commonly found in medical, dental or surgical professional organizations. There is great opportunity to advance oral health science, research in medicine and strategic planning through professional alignment. Consistent follow up is key to global movement on oral healthcare and thorough evaluation of recommendations is necessary.
Recommendations
There are several recommendations to improve national and global oral healthcare. Reviewed and implemented thoroughly, each approach can be individually achieved for comprehensive system improvement. Guidelines to address prevention, health behaviors, research, data analytics, service delivery and overall global oral health costs will establish successful progress for human health.
First, oral health must be a standard definition in practice. Statements and association guidelines may encompass all oral health, including sensory and motor issues, yet oral health is still heavily focused on dentistry and cancer. Data that strengthens the full picture, including variant diagnoses, interconnected illnesses and comorbidities is crucial. Equally, data that clarifies vocal, neuromuscular, autoimmune and genetic disease must be a part of oral health in the future. This requires determination from oral maxillofacial, ENT and neurological collaboration as well as stronger epidemiology and internationally coordinated research agenda.
The current spotlight on dentistry and oral health can also be improved upon. Healthy behaviors drastically improve oral health, and improving healthy behaviors through education is identified in action plans such as in Healthy People 2020 and WHO agendas. In order to increase knowledge, an accurate assessment of current education must be available. Knowledge on oral health has been assessed by topic, practice and educator. Some research has demonstrated that knowledge is increased specifically through patient connection to dental professionals and dentist visits [32]. Still, much assessment of oral health knowledge is through measurement of words, statements and practices rather than a comprehensive assessment of an individual’s understanding. There is also a paucity of data in an assessment of education best practices. In instance, recent studies assessed U.S. and Taiwanese caregivers’ dental health knowledge based on surveys and behavior practices. Yet these studies did not assess how knowledge was obtained [33, 34]. Interventions to improve caregiver knowledge of oral health were found in 3 of 32 studies in a recent literature review involving immigrants [26]. Specific, targeted research on oral health education and knowledge is helpful, and there is opportunity to benefit from stronger behavior research.
Tools used to assess oral health literacy have also been studied and compared, and these tools should be agreed upon. Critiques of widely used tools, such as the Rapid Estimate of Adult Literacy in Medicine (REALM), the Test of Functional Health Literacy in Adults (TOFHLA) and its spin-off the The Test of Functional Literacy in Dentistry (TOFHLiD) focus on word recognition and reading skills. There is less focus on health behaviors and service utilization [35, 36]. Moreover, some recent tools have been tested without a scaled sample. In instance, a Norwegian study on a new oral health literacy tool was conducted utilizing only those in which Norwegian speakers evaluated their own ability to participate. This method narrowed the sample size to those who spoke Norwegian with an ability to read oral health and research language [36]. Detailed ability to measure decision making, service utilization and intervention impact are recommended for the improvement of research in oral health knowledge and behavior [35]. Acces to tools could even be expanded for inclusion in ENT, otolaryngology and neuromuscular assessment of oral health. In fact, comprehensive evaluation and adoption of assessment tools is a gold standard. As example, the oral health assessment tool (OHAT) used by speech pathologists was studied as it was incorporated into swallowing examinations. Feasibility as well as reliability were demonstrated [37]. Oral health literacy can be assessed and shaped to desired levels, with tool standardization and use for expanded oral health scope.
Access to oral health care must be detailed in measure. Surveillance and data must improve. Ways to improve could include public health measures, insurance review and medical home information sharing. Worldwide, access to oral care should mirror guidelines. Long term travelers, volunteerism and citizens outside of their home country should be afforded similar care, under similar expectations worldwide. Labor supply should be agreed upon in credentialing, ratio of clinical to public and scope of practice. Access measures should take care to incorporate variances in labor and seek to align best practices. LMIC should be encouraged to utilize funding for international training, with reimbursement tied to home country contracts. Measurement of access to care could be a performance measure for this intervention.
Access to oral health care must also be measured through public health initiatives. Agreements and disagreements for major programs, like fluoridation, directly impact global health. Progress should be measured, with stronger evidence-based guidance down the line.
Supplies and needed products should be monitored at local levels and reported through governance to global agencies. Surveillance and data on access can utilize current epidemiology, as well as anticipatory analyses based on prior movement. Should an expansion of Medicaid coverage become policy in the U.S., skilled labor reimbursement must be budgeted and followed accordingly. Should global guidance for oral cancer screening take effect, information dissemination and measures of practice adoption should swiftly follow. Detailed monitoring should also include access to diagnostics, therapeutics and service delivery process measures of neuromuscular conditions involving the head and neck. Too, there should be a system to monitor travelers who cannot locate or afford adequate, needed dental care. Future systems should not only incorporate traveling insurance; systems should incorporate cross-specialty coverage of evidence based care. Finally, innovations that seek to promote at home dental care can be utilized and reviewed, with these variant populations in mind.
Equitable care in oral health can be achieved and must continue to be evaluated. Dental care equity should be a part of medical surveillance in LMIC medical home construction. Expansion of public coverage, such as expansion of Medicaid to include oral healthcare, must be implemented alongside access and infrastructure build. In fact, building equitable care in oral health through epidemiology and data is a way in which expanded oral health definition can contribute. As an example, one recent study assessed oral cancer alongside housing stability in England. Those living in deprived areas, compared to the general population of England, had worse survival outcomes and worse quality of life outcomes following treatment of head and neck cancer. Interestingly, there was no association between stage of cancer at presentation and social deprivation, yet those with lower socio-economic position were more likely to be selected for palliative treatment [38]. Equitable care is not only important for dental caries, it is important for oral health prevention and intervention guidance. Guidance is not only important for the health service industry, it is important for policy makers, those driving reimbursement practices and public health administration officials responsible for equitable care. Integrated oral health through shared ENT, otolaryngology, communication and neuromuscular diagnoses of the face, head and neck should be a primary priority for all coverage systems.
It is important to understand the reasons for, and tailor interventions to, disparities within community context. In instance, refugee children in the U.S. may experience disproportionate oral health burden, just as refugees do globally [26, 27]. Yet researchers have found that parental literacy improvement in the U.S. may strengthen equity [26], while researchers of refugee camps and major migration events worldwide determined that refugees in these alternative areas may primarily benefit from access to services. It is also important to take logical approaches without delay, centered on community context, for disadvantaged populations. Medical home models that include primary care education on dental and oral health are vital. Quality metrics that assure inequalities are reduced are critical. Quality metrics to provide structure, benchmarking and a means to process improvement for oral cancer must be built, funded and fine tuned throughout health systems design reform. As cancer disparity research advances, guidelines and recommendations must be incentivized. This can also create new pathways for oral healthcare access and treatment that provide opportunities for equitable care. The assurance of oral healthcare is a cost effective approach to public health that also provides for quality of life. Worldwide, surveillance and service delivery research can be built in systems that mimic developed country service research and surveillance.
Oral cancer prevention and treatment must improve. While efforts to modify human behaviors such as tobacco use should be continued, screening diagnostics, guidance and early treatment should be researched and developed. Currently, oral cancer screening and guidance is not developed from the strongest evidence. Efforts are underway to sharpen these processes [39]. Better diagnostics, guidance and innovation should be developed for oral cancer, and reimbursement for oral health services should be funded globally. Additionally, oral cancer speciality divisions should be interdisciplinary, supporting dentists and oral health professionals with a consistent approach.
The impact of oral health must be better understood to affect individual and policy change. This impact can best be understood through coordinated health research. Coordination is reliant on interdisciplinary services as well as interdisciplinary medical academia. Quality of life is an impact measure that must be a priority. Quality of life measures, alongside interventions, can also drive new protocols in service delivery. Tools that measure quality of life such as the Oral Health Impact Profile have been found to be limited by bias [40]. Too, quality of life is often measured within scope of orthodontic specialty or within one specialty such as oral cancer. Improvements to measures and inclusion across multiple specialties could greatly impact individual and collection quality of life.
Interventional improvements that drive oral health quality of life should be adopted in policy and regulation. As an example, end of life has been found to be a time when oral health needs change and multiply. Hospice and palliative policies, reimbursement and guidelines can specify stronger oral health interventions alongside this research, research driven from impact determinations [41].
The impact of oral health in relation to overall health should be understood and intervened upon not only from a causative view but from a consequential view. As an example, those with short sleep duration have been found to have an increased incidence of gingival inflammation [42]. Whether this is a cause, consequence or correlation would need further conclusive evidence. Should gingival inflammation be a result of shortened sleep, those with sleep disorders could be provided a stronger, sustained oral health plan.
Future work should strive to incorporate all components and afflictions of the head, neck and oral arena. In instance, one recent report indicated that regardless of dental pain cause between four major conditions, temporomandibular disorder (TMD), acute dental pain (ADP), trigeminal neuralgia (TN) and persistent dentoalveolar pain disorder (PDAP), quality of life was affected similarly. Despite differences in anatomical impact, these disorders affected patients similarly. Treatment of malocclusion has been shown to improve oral health quality of life [43]. Treatments of other oral health and head, neck and throat issues should be measured for similar impacts, comparatively, utilizing standardized tools and methodology.
There has been insight into brain and neurological research with oral health. Trigeminal neuralgia has been studied alongside altered brain structure and function [44]. There has also been insight into hospital service delivery. Preoperative oral health care was demonstrated to decrease the duration of hospital stay and potentially prevent infectious complications from orthognathic surgery [45]. Studies like these could be expanded for clear guidance in preventative surgical measures. Should research expand into head, neck, vocal and throat issues, it is not only for the benefit of the profession. Partnerships can be created for interdisciplinary system structure. In order to fully realize research capabilities and intervention strategies, interdisciplinary coordination between dentistry, orthodontics, oral health and general medicine must be aggressively encouraged.
Both quality and transparency in dental health research are also impacted by lack of compliance in good research guidelines [46]. Compliance to oral health research guidelines can be increased with interdisciplinary medical academia research, as resources are available for research compliance. Additionally, oral health journals must take care in publication. Grant reviewers, funding and evidence based dissemination could all require compliance to research guidelines by way of a global method, such as a rating system. These intermediaries must, however, require compliance as a condition of movement.
Moreover, dental health research must abide by the same movement in publication quality as general medical research. A major component of this movement is the transparency of negative and unanticipated data. This transparency is important not only in clinical trial research; it is important in service research as well. In instance, despite some studies that have demonstrated a possible relation between shortened sleep and gingivitis, research on obstructive sleep apnea found no differences in gingival inflammation nor dental plaque [47]. It is important to review the quality and strength of data.
Too, oral health recommendations must be expanded to all oral health, including otolaryngology and neuromuscular disorders. In instance, a literature review on oral health and stroke patients found a paucity of international literature in nurse-driven oral hygiene protocols for the reduction of pneumonia. There was also evidence that nurses alongside speech pathology can assist in dysphagia outcomes [48]. Inclusion can assist in better guidelines for otolaryngology and neuromuscular disorders related to oral health.
Oral health for those with structural and birth disorders can also benefit from an integrated medical approach. Those with cleft palate experience significant issues with oral health and report a worse oral health quality of life. Stratified, those with fistula experienced significantly lower oral health quality of life and worse self-reported speech scores [49]. Quality of life analysis has also been conducted between adults, adolescents and children with cleft lip and/or palate. This analysis has described psychological impact and reported negative psychological health for adults [50]. Negative oral health quality of life is also seen within those diagnosed with cerebral palsy. Understanding the importance of intervention should drive policy, reimbursement and innovation in general medicine. Speech and communication innovation can partner for extensive work toward equitable oral health quality of life and self-reported speech. Policies that address quality of life issues for those with poor oral health trajectories can significantly enhance well-being for individuals and populations.
Dental service utilization also drastically impacts oral health, from fluoride and periodontal disease assessments to cancer screenings. Yet service utilization, insurance coverage and out of pocket expenses are rarely reported as transparently as other health utilization lines. Dental expenses, from fees to household expenses, should be available to the public. Additionally, oral and maxillofacial medical care expenses should be available, from insurance payments to household data. Finally, data can be stifled by diagnoses, coding and utilization reporting borders. Future efforts in data collection must strive to capture all oral health and specialty care metrics. Should a person have a facial nerve disorder or a vocal cord disorder, the data should be captured comprehensively.
It is important to understand the numbers of the public that seek dental care, ENT care or primary care for a disorder in which guidelines could have provided a better pathway to quality care. Once understood, new pathways, partnerships and collaborative service delivery methods can be reimbursed and structured.
Workforce planning must be agreed upon in order for policymakers to advance systems forward. Dentist education and residency requirements, hygienist scope of practice, workforce ratios and primary medical care training in oral health should be standardized both within the U.S. and globally. Educational advances, especially in dental schools and within oral maxillofacial interdisciplinary education, should be available through academic medical center surveillance. Academic medicine must assure that specialist definitions do not limit future service delivery collaborations, as well. ENT and otolaryngology must strive to be included in, and inclusive of, oral health. Too, global and government reports on access to services should include surveillance data on workforce in annual updates.
Finally, interdisciplinary medical services can positively affect oral health policy and public health changes through data extraction. There are also opportunities for surveillance and coordination of care. In 2014, the HRSA issued a report on integrating primary care and oral healthcare. This report details the importance of competencies in oral health assessment for primary care, inclusion of interdisciplinary practice in primary care settings and implementation of oral health services in safety net care [15]. The data should drive change.
Too, setting guidance and recommendations can and should be followed with ongoing surveillance. In example, despite the opportunity to abide by the UK guidelines for oral health with cleft palate patients, the guidelines were found to be interpreted differently. Within this wide variance to compliance it was found that there was not a difference in prevalence of untreated caries nor in the average of decayed, missing and filled teeth for those with cleft palate [51]. If guidelines are rooted in evidence, adherence to guidelines should reflect evidentiary improvement. Notably, one of the major areas of noncompliance to the UK guidelines for those with cleft palate was crystal clear: less than half of the regional cleft multidisciplinary units had a pediatric dental consultant [51]. Ongoing surveillance and compliance can assist in policy assertiveness and policy modification.
Coordination of care must also be rooted in integrated oral health. In example, specific mechanical and chemotherapeutic measures for oral care in children with cerebral palsy have been shown to improve oral and gingival hygiene [52]. These measures should be followed with all members of interdisciplinary teams responsible. Physical therapists can assist with mechanical brush training, medical homes and pharmacies can assist in ease of chlorhexidine gluconate (CHX) spray access and dental professionals can provide positive reinforcement for psychological or behavioral interventions. Pharmaceutical industry and policymakers can be provided additional research that better demonstrates structural, service access and interventions. As an example, as sweetener within oral medications has been identified as a potential oral health risk [53] for those with neuromuscular conditions such as cerebral palsy. Perhaps the international industry may be able to change manufacturer processes with the right research at the table.
Too, interventions may be targeted toward specific diagnoses. Despite a much lower prevalence within cerebral palsy type, some research has showed that those with mixed cerebral palsy have been found to have a higher prevalence of oral health issues [54]. Even within conditions that affect oral health care, noted disparities can be successfully targeted. These disparity movements have potential to further oral health medicine as well as accumulate insight into the intricacies of birth defects and neuromuscular conditions.
Integrating services advances oral health research agenda, promotes a solid knowledge foundation, secures specialty care and assures timely follow up on critical diagnoses. The advantages to interdisciplinary teams in oral health can be realized with policy, reimbursement practice and academia alignment. Once provided concrete data, quality metrics, reimbursement and incentives to abide by tailored guidelines can shape the future of oral health. Service and industry integration assists with overall goals, acknowledges expanded definition and provides for a united front.
Conclusion
Oral healthcare has expanded scope and science throughout the years. It is no longer acceptable nor strategic to address oral health as a fragmented, secondary aspect of medicine. Millions of individuals do not obtain needed preventative care or treatments for oral health, and significant cost effective approaches have yet to be applied to a global oral health system. Oral health must remain a priority in action, intervention and investment in both research and service delivery. Oral health statistics and data are centered on dental care. This data should guide solid dental systems for the future, and this data must be enhanced by inclusion of total oral health. Neuromuscular disorders of the throat and neck, rare genetic mutations of the mouth and neck, communication and vocal disorders, and even esophageal disorders in which swallowing or mouth care are affected are all part of the expanded oral healthcare definition. The public benefits by a strengthened, precise definition rooted in strong data. By fostering healthy behaviors, oral health education, policy, research, innovation and preventative care, a healthy public can be assured. By strengthening and aligning interdisciplinary medicine, oral health epidemiology and research, a global oral health system can provide for quality, cost-effective care. This care can dynamically transform quality of life, increase overall individual health and address identification of unknown disorders as well. Indeed, a stronger oral health system will set the foundation for discovery of previously misunderstood oral health adversity, enhance treatments and chart a path for curative medicine. The future has never been brighter.
Abbreviations
- (CDC):
-
Centers for Disease Control and Prevention
- (FDI):
-
Fédération Dentaire Internationale
- (LMIC):
-
Low and Middle Income Countries
- (REALM):
-
Rapid Estimate of ADult Literacy in Medicine
- (TOFHLA):
-
Test of Functional Health Literacy in Adults
- (TOFHLiD):
-
The Test of Functional Literacy in Dentistry
- (WHO):
-
World Health Organization
References
World Health Organization, “Oral health.” [Online]. Available: http://www.who.int/oral_health/en/. [Accessed: 15-Apr-2018].
U.S. Department of Health and Human Services, “Oral Health,” 13-Apr-2018. [Online]. Available: https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health/objectives. [Accessed: 15-Apr-2018].
Centers for Disease Control and Prevention, “Oral Health In America: Summary of the Surgeon General’s Report,” 19-Aug-2016. [Online]. Available: https://www.cdc.gov/oralhealth/publications/sgr2000_05.htm.
M. Glick, D. M. Williams, D. V. Kleinman, M. Vujicic, R. G. Watt, and R. J. Weyant, “A new definition for oral health developed by the FDI world dental federation opens the door to a universal definition of oral health,” J. Public Health Dent., vol. 77, no. 1, pp. 3–5, Dec. 2017.
J. A. Gil-Montoya, A. L. F. de Mello, R. Barrios, M. A. Gonzalez-Moles, and M. Bravo, “Oral health in the elderly patient and its impact on general well-being: A nonsystematic review,” Clin. Interv. Aging, vol. 10, pp. 461–467, Feb. 2015.
Lawrence, H. P., and Leake, J. L., The US surgeon General’s report on oral health in America: A Canadian perspective. J-Can Dent. Assoc 67(10):587–587, 2001.
S. S. Shueb, D. R. Nixdorf, M. T. John, B. F. Alonso, and J. Durham, “What is the impact of acute and chronic orofacial pain on quality of life?,” J. Dent., vol. 43, no. 10, pp. 1203–1210, Oct. 2015.
Hilgenberg-Sydney, P. B., Calles, B. M., and Conti, P. C. R., Quality of life in chronic trigeminal neuralgia patients. Rev. dor 16(3):195–197, 2015.
G. Almoznino et al., “Oral Health-Related Quality of Life in Patients with Temporomandibular Disorders,” J Oral Facial Pain Headache, vol. 29, no. 3, pp. 231–241, Summer 2015.
D. M. Saman, “A review of the epidemiology of oral and pharyngeal carcinoma: Update,” Head Neck Oncol., vol. 4, p. 1, Jan. 2012.
Global Oral cancer Form Group, “Understanding gaps in the oral cancer continuum and developing strategies to improve outcomes,” World Health Organization, 2016.
Scannapieco, F. A., and Harris, K. W., Oral Health and Pneumonia. In: Craig, R. G., Kamer, A. R. (Eds), A Clinician’s Guide to Systemic Effects of Periodontal Diseases. Berlin, Heidelberg: Springer Berlin Heidelberg, 2016, 81–92.
Klompas, M., Branson, R., Eichenwald, E. C., Greene, L. R., Howell, M. D., Lee, G., Magill, S. S., Maragakis, L. L., Priebe, G. P., Speck, K., Yokoe, D. S., Berenholtz, S. M., and Society for Healthcare Epidemiology of America (SHEA), Strategies to Prevent Ventilator-Associated Pneumonia in Acute Care Hospitals: 2014 Update. Infect. Control Hosp. Epidemiol. 35(8):915–936, 2014.
L. J. Jin, I. B. Lamster, J. S. Greenspan, N. B. Pitts, C. Scully, and S. Warnakulasuriya, “Global burden of oral diseases: Emerging concepts, management and interplay with systemic health,” Oral Dis., vol. 22, no. 7, pp. 609–619, Oct. 2016.
U. S. D. of Health, H. Services, and Others, “Integration of oral health and primary care practice,” Health Resources and Services Administration, 2014.
“Oral Health Services,” World Health Organization , 2018. [Online]. Available: http://www.who.int/oral_health/action/services/en/. [Accessed: 19-Apr-2018].
“Improving access to oral health care for vulnerable : HRSA,” National Academy of Sciences, 2011.
World Health Organization, “Density of dentistry personnel (total number per 1000 population, latest available year),” 2018. [Online]. Available: http://www.who.int/gho/health_workforce/dentistry_density_text/en/. [Accessed: 18-Apr-2018].
M. Masood, A. Sheiham, and E. Bernabé, “Household expenditure for dental care in low and middle income countries,” PLoS One, vol. 10, no. 4, p. e0123075, Apr. 2015.
E. Bernabé, M. Masood, and M. Vujicic, “The impact of out-of-pocket payments for dental care on household finances in low and middle income countries,” BMC Public Health, vol. 17, no. 1, p. 109, Jan. 2017.
S. Listl, J. Galloway, P. A. Mossey, and W. Marcenes, “Global economic impact of dental diseases,” J. Dent. Res., vol. 94, no. 10, pp. 1355–1361, Aug. 2015.
“Extent of Flouridation,” British Flouridation Society, 2012. [Online]. Available: https://docs.wixstatic.com/ugd/014a47_0776b576cf1c49308666cef7caae934e.pdf. [Accessed: 18-Apr-2018].
Petersen, P. E., and Ogawa, H., Prevention of dental caries through the use of fluoride – the WHO approach. Community Dental Health 35(1), 2016.
A. A. C. Heggie, “Oral and maxillofacial surgery: What are our credentials?,” Ann. Maxillofac. Surg., vol. 4, no. 1, p. 1, Jan. 2014.
Centers for Disease Prevention and Control, “Disparities in oral health,” 2018. [Online]. Available: https://www.cdc.gov/oralhealth/oral_health_disparities/index.htm. [Accessed: 19-Apr-2018].
M. Reza et al., “Oral health status of immigrant and refugee children in north america: a scoping review,” J. Can. Dent. Assoc., vol. 82, p. g3, Feb. 2016.
M. T. Keboa, N. Hiles, and M. E. Macdonald, “The oral health of refugees and asylum seekers: a scoping review,” Global. Health, vol. 12, no. 1, p. 59, Oct. 2016.
J. A. Shariff and B. L. Edelstein, “Medicaid meets its equal access requirement for dental care, but Oral health disparities remain,” Health Aff. , vol. 35, no. 12, pp. 2259–2267, Dec. 2016.
J. Steele et al., “The Interplay between socioeconomic inequalities and clinical oral health,” J. Dent. Res., vol. 94, no. 1, pp. 19–26, Jan. 2015.
N. Gupta et al., “Changing Trends in oral cancer - a global scenario,” Nepal J Epidemiol, vol. 6, no. 4, pp. 613–619, Dec. 2016.
K. D. Shield et al., “The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012: Lip, Oral Cavity, and Pharyngeal Cancers,” CA Cancer J. Clin., vol. 67, no. 1, pp. 51–64, Jan. 2017.
A. Taniguchi-Tabata et al., “Associations between dental knowledge, source of dental knowledge and oral health behavior in Japanese university students: A cross-sectional study,” PLoS One , vol. 12, no. 6, p. e0179298, Jun. 2017.
C.-C. Chen et al., “Immigrant-native differences in caries-related knowledge, attitude, and oral health behaviors: a cross-sectional study in Taiwan,” BMC Oral Health, vol. 14, no. 1, p. 3, Jan. 2014.
A. R. Wilson et al., “Validation and Impact of Caregivers’ Oral Health Knowledge and Behavior on Children's Oral Health Status,” Pediatr. Dent., vol. 38, no. 1, pp. 47–54, Jan. 2016.
V. Dickson-Swift, A. Kenny, J. Farmer, M. Gussy, and S. Larkins, “Measuring oral health literacy: A scoping review of existing tools,” BMC Oral Health, vol. 14, p. 148, Dec. 2014.
L. Stein, K. S. Pettersen, M. Bergdahl, and J. Bergdahl, “Development and validation of an instrument to assess oral health literacy in Norwegian adult dental patients,” Acta Odontol. Scand., vol. 73, no. 7, pp. 530–538, Feb. 2015.
I. S. Simpelaere, G. Van Nuffelen, J. Vanderwegen, K. Wouters, and M. De Bodt, “Oral health screening: Feasibility and reliability of the oral health assessment tool as used by speech pathologists,” Int. Dent. J., vol. 66, no. 3, pp. 178–189, Jun. 2016.
J. Rylands, D. Lowe, and S. N. Rogers, “Outcomes by area of residence deprivation in a cohort of oral cancer patients: Survival, health-related quality of life, and place of death,” Oral Oncol., vol. 52, pp. 30–36, Jan. 2016.
P. Speight, J. Epstein, O. Kujan, M. W. Lingen, T. Nagao, K. Ranganathan, P. Vargas “Screening for oral cancer – Who, what, why and where?,” World Health Organization, 2016.
D. R. Reissmann, A. Erler, C. Hirsch, I. Sierwald, C. Machuca, and O. Schierz, “Bias in retrospective assessment of perceived dental treatment effects when using the Oral health impact profile,” Qual. Life Res., vol. 27, no. 3, pp. 775–782, Mar. 2018.
D. J. Fischer, J. B. Epstein, Y. Yao, and D. J. Wilkie, “Oral health conditions affect functional and social activities of terminally ill cancer patients,” Support. Care Cancer, vol. 22, no. 3, pp. 803–810, Mar. 2014.
M. C. Carra, A. Schmitt, F. Thomas, N. Danchin, B. Pannier, and P. Bouchard, “Sleep disorders and oral health: A cross-sectional study,” Clin. Oral Investig., vol. 21, no. 4, pp. 975–983, May 2017.
Silvola, A.-S., Tolvanen, M., Rusanen, J., Sipilä, K., Lahti, S., and Pirttiniemi, P., Do changes in oral health-related quality-of-life, facial pain and temporomandibular disorders correlate after treatment of severe malocclusion? Acta Odontol. Scand. 74(1):44–50, 2016.
Y. Wang, D.-Y. Cao, B. Remeniuk, S. Krimmel, D. A. Seminowicz, and M. Zhang, “Altered brain structure and function associated with sensory and affective components of classic trigeminal neuralgia,” Pain, vol. 158, no. 8, pp. 1561–1570, Aug. 2017.
H. Shigeishi, M. Z. Rahman, K. Ohta, S. Ono, M. Sugiyama, and M. Takechi, “Professional oral health care reduces the duration of hospital stay in patients undergoing orthognathic surgery,” Biomed Rep, vol. 4, no. 1, pp. 55–58, Jan. 2016.
R. Sarkis-Onofre et al., “Use of guidelines to improve the quality and transparency of reporting oral health research,” J. Dent., vol. 43, no. 4, pp. 397–404, Apr. 2015.
M. C. Carra, F. Thomas, A. Schmitt, B. Pannier, N. Danchin, and P. Bouchard, “Oral health in patients treated by positive airway pressure for obstructive sleep apnea: A population-based case–control study,” Sleep and Breathing, vol. 20, no. 1, pp. 405–411, Mar. 2016.
Ajwani, S. et al., Integrated oral health care for stroke patients--a scoping review. J. Clin. Nurs. 26(7–8):891–901, 2017.
R. E. Long, M. Wilson-Genderson, B. H. Grayson, R. Flores, and H. L. Broder, “Oral health-related quality of life and self-rated speech in children with existing fistulas in mid-childhood and adolescence,” Cleft Palate Craniofac. J., 2015.
de Queiroz Herkrath, A. P. C., Herkrath, F. J., Rebelo, M. A. B., and Vettore, M. V., Measurement of health-related and oral health-related quality of life among individuals with nonsyndromic orofacial clefts: A systematic review and meta-analysis. Cleft Palate Craniofac. J. 52(2):157–172, 2015.
Smallridge, J. et al., Functional outcomes in the Cleft Care UK study--Part 3: oral health and audiology. Orthod. Craniofac. Res. 18(S2):25–35, 2015.
A. Maiya, Y. R. Shetty, K. Rai, V. Padmanabhan, and A. M. Hegde, “Use of different oral hygiene strategies in children with cerebral palsy: A comparative study,” J Int Soc Prev Community Dent, vol. 5, no. 5, pp. 389–393, Sep. 2015.
N. Sinha, B. Singh, K. G. Chhabra, and S. Patil, “Comparison of oral health status between children with cerebral palsy and normal children in India: A case-control study,” J. Indian Soc. Periodontol., vol. 19, no. 1, pp. 78–82, Jan. 2015.
Rodríguez, J. P. L. et al., Dental Decay and Oral Findings in Children and Adolescents Affected by Different Types of Cerebral Palsy: A Comparative Study. J. Clin. Pediatr. Dent. 42(1):62–66, 2018.
Availability of Data and Material
There is no original data to aggregate or report.
Funding
There are no funding contributions to declare.
Author information
Authors and Affiliations
Contributions
The author is the sole author of this manuscript.
Ethics declarations
Conflict of Interest
This author declares she has no conflict of interest This article does not contain any studies with human participants or animals performed by any of the authors There are no competing interests to declare Not applicable The author consents to publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
About this article
Cite this article
Babyar, J. Inclusive Oral Healthcare for a better Future Together. J Med Syst 44, 89 (2020). https://doi.org/10.1007/s10916-020-01560-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-020-01560-3