Abstract
The demand of healthcare systems for chronically ill patients and elderly has increased in the last few years. This demand is derived by the necessity to allow patients and elderly to be independent in their homes without the help of their relatives or caregivers. The prosperity of the information technology plays an essential role in healthcare by providing continuous monitoring and alerting mechanisms. In this paper, we survey the most recent applications in healthcare monitoring. We organize the applications into categories and present their common architecture. Moreover, we explain the standards used and challenges faced in this field. Finally, we make a comparison between the presented applications and discuss the possible future research paths.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The constant increase in elderly population caused by the innovations in healthcare and the decrease of birth rate is one of the major challenges currently facing the developing and developed countries. For example, in Japan nearly 20% of the population are aged 65 or older [1]. Figure 1 highlights the changing dynamics of elderly population distribution at various age groups in USA.
Population projections in US from 2012 to 2050 in different age group [2]
The goal is to provide this population with healthcare systems that can be installed in their homes and turn them into smart homes [3]. These healthcare systems are able to gather data about the elderly and chronically ill persons, transfer and analyze them remotely. This can increase their ability to have a relaxed, independent and safe life in their homes; which can reduce the cost of staying at the hospitals.
There are various existing systems that are developed for this purpose, which are summarized and presented in this paper. The remaining part of this paper is sectioned as follows: “Papers search and selection strategy” presents our strategy in selecting appropriate papers for this survey. Section “Healthcare initiatives” provides a list of the common healthcare initiatives in the healthcare sectors. Section “A summary of the surveyed applications” provides a summary of the surveyed applications. Sections “The common healthcare architecture” and “Overview of pervasive healthcare systems” build upon the summary presented in “A summary of the surveyed applications” and preset the common architecture and the proposed categorization of the systems respectively. Some focused studies in healthcare systems are introduced in “Focused studies in healthcare systems”. Smart sensor concept and sensor standards are briefly explained in “Standards related to healthcare monitoring”. Section “Discussion and conclusion” provides a comprehensive discussion explaining the major challenges faced in healthcare monitoring systems, a summary of the key points observed in surveyed systems, and a conclusion.
Papers search and selection strategy
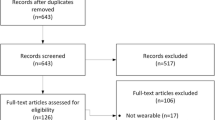
In this survey paper, we screened papers from databases such as Google Scholar, IEEE Explorer, ACM, Springer, and Elsevier covering years 2004 to December 1, 2018. We included a few older papers to explain certain algorithms or techniques such as hidden markov model. Initially, we started with the proceedings of the IEEE Healthcom’13 conference due to the abundance of papers related to remote healthcare monitoring for elderly and due to the fact that authors Y.I. and N.A. attended the conference. We screened papers according to the titles and abstracts. A full text was examined in case the abstract didn’t provide information to identify whether the paper meets our inclusion criteria or not. We focused on citing the original papers rather than the review papers. Papers that examined niche problems or algorithmic enhancement were excluded from “Overview of pervasive healthcare systems” and only included in “Focused studies in healthcare systems”. References of the selected papers were also sought to identify more related papers. Figure 2 shows a summary of the surveyed papers.
Healthcare initiatives
Over the past decade, the concern about healthcare has increased and led to the establishment of healthcare organizations and initiatives. Improving the healthcare quality and decreasing the cost were the main motives behind these initiatives. The main goals being addressed in their agenda include encouraging research in healthcare through providing funds to different research institutes in order to develop new systems, adopt information technology in healthcare, provide a standardized architecture and address the challenges and propose solutions. In this section we will shed the light on the major healthcare initiatives in the world and list their goals and scopes.
Ambient assisted living joint programme
The Ambient Assisted Living Joint Programme (AAL JP) is a very large European project funded and supported by the European Commission (EC) and twenty two countries during the period from 2008 to 2013. During this period, there was regular calls for research proposals in the field of ICT active and healthy aging. There are many objectives for the AAL, which are described as follows [4]:
-
Improve the life conditions of the elderly.
-
Qualify the elderly to depend on themselves and live independently.
-
Allow the elderly to connect with their friends and family in their social circles.
-
Reduce the costs imposed by healthcare.
The call for research proposals are quoted below [4]:
-
Call 1: ”Prevention and Management of Chronic Conditions of Elderly People.”
-
Call 2: ”Advancement of Social Interaction of Elderly People.”
-
Call 3: ”Advancement of Older Persons’ Independence and Participation in the ”Self-Serve Society.”
-
Call 4: ”Advancement of Older Persons’ Mobility.”
-
Call 5: ”Self-Management of Daily Life Activities of Older Adults at Home.”
-
Call 6: ”ICT based solutions for Supporting Occupation in Life of Older Adults.”
Over 150 projects were funded over the 6 calls. The success of the program encouraged the European Commission and 19 countries to renew it for a second phase. The new program is called Active and Assisted Living (AAL) program with an estimated budget of €700 million over the period from 2014 to 2020. The main goal is to fund projects that can improve the older population’s quality of life. Currently, there is a new proposal being submitted to the European Commission to fund projects during the period 2021 to 2027.
International telecommunication union (ITU)
International Telecommunication Union (ITU) is an international organization that is part of the United Nations (UN) organization. ITU is specialized in communication technologies and it has two study groups that are concerned with e-Health [5]:
-
ITU-D: focuses on raising the awareness of telecommunication operators, decision-makers, regulators, donors and customers about the role of telecommunication and information technologies in e-Health services.
-
ITU-T: focuses on achieving the interoperability among systems and reducing the cost of devices in e-Health.
The international federation for medical and biological engineering (IFMBE)
The International Federation for Medical and Biological Engineering (IFMBE) is a Non-Governmental Organization (NGO) for the United Nations (UN) and the World Health Organization (WHO). It was established in 1959 after a group of engineers, physicists, and clinicians met in the 2nd International Conference of Medical Engineering in France. The overarching vision of the organization is to promote collaborative clinical and engineering research. The promotion and dissemination of outcomes is done through holding conferences, world congresses, and workshops, and publishing in their journal, newsletters, and books [6].
World health organization (WHO)
World Health Organization (WHO) is the main and directing committee within the United Nations (UN) that is dedicated to health issues. The main responsibility of WHO is to provide leadership and guidance to health matters globally. The need for the standardization in health data and services has been addressed in the 66th World Health Assembly. As a result, the e-Health Technical Advisory Group (eTAG) was established in 2013 to support the work of the WHO in e-Health area. WHO’s work in e-Health includes programmes and projects in areas, such as policy and governance, research and global surveys, standardization and interoperability, eLearning and capacity building, and e-Health applications [7].
Institute of electrical and electronics engineers (IEEE) e-health technical committee (TC)
The IEEE communications society created the e-Health sub-technical committee (TC) in May 2008, which was elevated to a full-TC in December 2009, to address the challenges and opportunity of the information technology in healthcare field. e-Health TC focuses on ICT technologies and solutions to improve healthcare quality and efficiency through the following trends:
-
Enhance the quality of healthcare and decrease the expenses of healthcare by using the emerging Information and Communication Technology (ICT).
-
Ubiquitous personalized healthcare from anywhere, at anytime, by any authorized person(s) when needed.
Institute of electrical and electronics engineers (IEEE) - engineering in medicine and biology society (EMBS)
IEEE Engineering in Medicine and Biology Society (EMBS) is a huge society that brings engineers and clinicians together to develop applications that can serve and benefit a large spectrum of patients. The society consists of 12,000 members spread over 97 countries around the world. Researchers in this society develop software applications, hardware devices, and communication platforms to advance the healthcare research and outcomes. EMBS includes around 12 technical committees serving different research interest in the area of healthcare including: Biomedical and Health Informatics (BHI), Biomedical Imaging and Image Processing (BIIP), Biomedical Signal Processing (BSP), Cardiopulmonary Systems (CPS), Computational Biology and the Physiome (CBP), Wearable Biomedical Sensors and Systems (WBSS), NeuroEngineering (NE), Therapeutic Systems and Technologies (TST), BioRobotics (BR), BioNanotechnology and BioMEMS (BNM), Translational Engineering and Healthcare Innovation (TEHI), and Committee on Man and Radiation (COMAR).
Health-IT
The Office of the National Coordinator (ONC) for Health Information Technology (Health-IT) was created in 2004. ONC encourages the adoption of information and communication technologies (ICT) in the healthcare field through applying Electronic Health Records (EHRs), that can be created, managed, and viewed by authorized health providers and allow the exchange of patients’ data between several health organizations [8].
A summary of the surveyed applications
In this section, we provide a chronological and architectural overview of the healthcare monitoring systems described in this paper, summarized in Table 1. We also include other systems that have not been described in this paper due to space limitation. For each system we present the following attributes: year of issuance, type of sensors used, architecture type, local and remote devices used, the purpose of the system, whether it is used locally or remotely, security aware, power aware, the protocol used to transmit the data, and the processing location. According to the information presented in the table, we present the common architecture in “The common healthcare architecture” and then provide our proposed categorization of the surveyed applications in “Overview of pervasive healthcare systems”.
The common healthcare architecture
Several healthcare applications have been investigated in this survey. It is observed that these systems share a common architecture and a set of properties. This architecture consists of three tiers that work together to collect and analyze the patient’s sensory data. These tiers are: sensors, gateway, and remote monitoring system. The components of each tier and how they interact with each other are shown in Fig. 3. In this section, we present and describe the hierarchy of the common healthcare architecture and explain the technologies used in each layer.
Tier.1-sensors
The revolution of microelectronics industry has produced different kinds of sensors that can collect clinical or environmental data. In addition, these sensors became widely available to the industry and individuals at homes. These sensors are responsible for collecting medical signals from patients by attaching them to their bodies as a BAN (Body Area Network) or deploying them around as a PAN (Personal Area Network) or Ambient Sensors.
In a BAN, various medical sensors are usually attached to the patient, either by securing them directly to the body of the patient, on the clothes, or even implant them under the skin in case of measuring internal health status. BAN sensors continuously monitor medical signals, such as: temperature, heartbeat, physical activity, blood pressure, electroencephalography (EEG), electromyography (EMG), and electrocardiography (ECG) [51].
A PAN, also called ambient network, is composed of ambient sensors deployed on devices that belong to the patient. These sensors provide rich contextual information about the patient’s living environment and activities. Examples of these sensors are: sound, video cameras, pressure, RFID readers, luminosity, proximity, temperature, location tracking and humidity sensors [52].
The collected data are transmitted to a local device in various ways. Medical sensors can be connected to other devices through the conventional wired standards, such as: Ethernet [53] and USB [54]. Wireless connections are more dominant in transferring the collected data from sensors to the gateway. Bluetooth and Zigbee are common for short-range communication, and WiFi and LTE are common for long-range communications [55]. There are many other wireless technologies and standards used in remote healthcare monitoring systems and Internet of Things (IoT) applications, such as BLE (Bluetooth Low Energy) [56], ANT+ (for activities monitoring) [57], RFID (Radio-Frequency Identification) [58], RuBee (alternative to RFID and suitable for harsh environment) [59], 6LoWPAN (IPv6 over Low-Power Wireless Personal Area Networks) [60], DASH7 (open source) [61], Z-Wave (for home automation) [62], UWB (Ultra-Wide Band) [63], and NFC (Near Field Communication) [64].
Tier.2-gateway
A gateway is usually used for collecting data from sensors and transferring it to a remote server located at the hospital or on the cloud for analysis. However, some systems perform analysis locally, and then transfer the derived data to a remote server for further analysis or for historical recording. The later approach is more adopted recently with the emergence of fog computing, where the analysis is performed locally (called edges) for faster decision-making and better utilization of bandwidth and only partial updates are sent to the cloud. The gateway can be a dedicated device or simply a smartphone that is connected to the Internet and located in the patient’s place [52]. The communication can be uni-directional, from the sensors to the remote server through the gateway, or bi-directional as proposed in [37], where the gateway can also send information to the sensor node to modify some recording parameters. Ethernet [53], 5G, LTE, NB-IoT and SigFox could be used to transfer the collected signals from the gateway to the remote server.
Tier.3-remote monitoring system
The collected medical or environmental signals from the sensors are usually transmitted to a remote system (server) that is sophisticated and considered as the heart of the system. This system has four main functionalities:
-
1.
Run special algorithms to interpret the collected data and extract further information.
-
2.
Generate alerts in case of emergencies.
-
3.
Record each patient’s data in a database for further analysis in the future, such as applying data mining techniques to predict the existence of any undiagnosed disease.
-
4.
Provide a Graphical User Interface (GUI) to allow the real-time monitoring of the patient’s status.
The remote monitoring system is usually implemented as a server located in a hospital. However, some new researches are moving toward integrating cloud computing and fog computing into healthcare systems. As an example, Wan et al. [65] suggested a healthcare system that processes the collected data in the cloud and then transmits it to the hospital for monitoring purposes. A more recent research conducted by Vora et al. [47], proposed a fog-based remote monitoring system for patients with chronic neurological diseases. The system collects motion data and process it on the edge gateways.
Overview of pervasive healthcare systems
As stated in “The common healthcare architecture”, most of the existing healthcare systems have a common architecture that consists of sensor nodes with an embedded communication module and sometimes a processor, and a base station that is remotely connected to the caregivers PC and/or to a server through the Internet. In the literature review, we found that healthcare monitoring systems are divided into three main categories according to the type of data collected, which are: Medical Sensing, Activity & Environmental Sensing, and Integrated Medical, Activity & Environmental Sensing. These categories have two properties (or functional requirements) that describe the location where the data is collected, which are: Indoor and Outdoor. Figure 4 shows the categories and properties of the remote healthcare monitoring systems. These categories will be described in the following subsections.
Medical sensing
Systems in this category collect medical data from patients such as electrocardiography (ECG), blood pressure, electroencephalography (EEG), oxygen, and Electromyography (EMG). These sensors can form a body area network (BAN) by securing them on the body of the patient, or placed on the furniture at the patient’s house and form a personal area network (PAN). The type and the number of the medical sensors can vary based on the focus group. The purpose of these systems is to continuously monitor the physiological signals of the chronically ill patients with heart problems [23, 44], respiratory problems [27, 43], Alzheimer [22], or Parkinson [34] and take the necessary actions as soon as an incident happens. Following are some examples of such systems.
HERA [22] is a project that studied the needs of Alzheimer patients in their early stages. The proposed system architecture is composed of medical sensors (blood pressure and weight), a Set-Top-Box (STB), services platform, and health center information server. The medical sensors are directly connected to the Set-Top-Box (STB) through Bluetooth. The STB collects data from the sensors and provides an interface to the patient that is based on Text-To-Speech (TTS) and Speech Recognition (SR) techniques. Sensor data are sent to the HERA service platform where all applications reside. The HERA service platform is connected to both the health center information server located at a relative’s home and the medical center for information sharing. Security standards, such as SSL, HTTPS and Security Web Services, are adopted in all the communication interfaces.
Health @ Home (H@H) [23] targeted elderly who suffer from Chronic Heart Failure (CHF). This system is similar to the HERA system in using Bluetooth as a communication protocol, but differ in the type and number of sensors, where it collects signals from ECG, SpO2, blood pressure, and weight sensors. The collected data are then transmitted to a home gateway to process it and then send it to a remote server to be further analyzed and stored in the Hospital Information System (HIS). All sensing devices use Bluetooth as a communication protocol and follow the client/server paradigm. The interoperability of the system and the security of the transmission are guaranteed through the use of HL7 standard and the HTTPS protocol.
Smartphones are significant components in the remote healthcare systems. HELP (Home-based Empowered Living for Parkinson’s disease patients) [34] took advantage of smartphones to monitor patients suffering from Parkinson’s disease (PD). The system estimates the level of PD symptoms and adjust the dose of medication accordingly in order to reduce the symptoms. HELP architecture consists of sensors and actuators managed by a smartphone and a remote monitoring server for doctors and professionals. The authors introduced a customized MAC protocol and applied it into the network of sensors. The customized MAC protocol aims to decrease the packet loss and enhance the energy efficiency. Furthermore, the protocol reduces the sensors’ signal interactions in case of simultaneous transitions.
The systems described above used traditional databases that reside in a remote location to store patients’ medical data. Recent systems exploit cloud services to store and process the data. Fekr et al. [43] developed a wearable device that measures respiration rate and tidal volume variability. This system is different from others in which the data are transferred directly to the cloud to be saved and then accessed by the remote healthcare center. Applying cloud technology to save the collected data yields to tremendous advantages over the traditional databases, including accessibility, scalability, high availability, and fast recovery time. Bluetooth low energy (BLE) is used to send the collected data to a close PC or Smartphone, then the collected data will be transferred to the cloud using WiFi. Similarly, Yang et al. [44] used cloud services in their implementation, where they developed an IoT-based system for ECG monitoring. The system provides the ability for the heart-related elderly patients to monitor their ECG signal while at home. ECG signals are transmitted through sensor nodes, each one of these nodes has three electrodes to read the signal from the patient’s skin. The collected data is transmitted to the cloud through a WiFi access point. The cloud provides processing capabilities including cleaning, storage, analysis, and warning. Patients, caregivers and clinicians can visualize the data on their computer and mobile devices through the use of HyperText Transfer Protocol (HTTP) and Message Queuing Telemetry Transport (MQTT) servers. The HTTP server provides the data upon request. The MQTT server transmits the data from the ECG monitoring node to the web page through minimum bandwidth use.
Activity and environmental sensing
Systems in this category collect data to identify patient’s daily activities and to determine the status of their surrounding environment. Most of the applications are developed to detect fall [26, 32, 33, 38, 48, 66] and to remind patients about certain tasks such as taking medication [28, 45] or staying hydrated [67]. There is a variety of sensors that can provide information about patients’ activities and environmental changes such as cameras, microphones, proximity, accelerometer, temperature, SpO2, CO2 and humidity. Following is a description for some of the applications.
Heikkila et al. [38] developed a system that tracks the living patterns and behaviors of the elderly at home using proximity sensors and detects any abnormal event. These sensors are placed within the patient’s chair, bed, and sofa to report his/her body motions and postures. The data provide the caregivers an overview of patients’ behaviors and daily routines, especially if they are under medication or have early symptoms of memory dysfunctions. Sensors transmit the patient’s data to a gateway using Bluetooth, which then transfers the data to a server for data storage and to the caregiver’s displaying device using the Internet.
Visual sensors can also be used to identify patients’ activities. CARE [32] detects fall of the elderly at home, which uses visual sensors to detect critical situations such as falls and immobilized persons. The visual sensors are placed on a FPGA board which is capable of applying neural network functions to determine the status of the person. The board has also an integrated wireless module to send alerts to the care providers in case a fall event is detected.
The most common and effective approach to detect patients’ activities is the use of accelerometer. The availability of the accelerometer in the smartphone and smartwatch allowed researchers to start using them in monitoring applications. The system proposed by Yu et al. [33] uses the built-in accelerometer in the smartphone to detect the patient’s movements. When the system detects a fall, it sends a Multimedia Messaging Service (MMS) to everyone in the patient’s caregiver list. The message includes the time of the fall, GPS coordinates and a map for the location, so the caregivers can reach quickly the patient’s location. Mauldin et al. [48] developed an IoT-based system that leverages the data collected from the accelerometer in the smartwatch and the computational capabilities of the smartphone to detect fall using deep learning in a timely manner.
Applications to remind patients about their medications and other specific tasks are also common in the activity and environmental sensing. Mateska et al. [28] proposed a healthcare solution for elderly that is based on the Radio Frequency Identification (RFID) technology. The Sensors (temperature, humidity, CO2, and motion) are connected to a local server through a wireless sensor network base station. On the other hand, RFID system is designed using a combination of RFID tags and readers. The active RFID system is used to locate the elderly within his/her home, while, the passive system is used for elderly memory enhancement feature through items and medicament usage reminder. The server connects the wireless sensor network (WSN) and RFID gateways and executes data processing and web hosting at the same time. Furthermore, the server sends e-mails to authorized caregivers, whenever critical situations happen. Medication adherence has also been achieved through the use of sounds and vibration notifications in the smartwatch. Mondol et al. [45] developed a smartwatch application, called MedRem, to remind patients to take their medications. MedRem has a voice recognition capabilities that allows patients to communicate with the watch to inquire about the medicine for example.
Medical, activity & environmental sensing
Systems in this category combines both medical, activity and environmental sensors to provide better monitoring capabilities and better identifications of medical incidents. Following is a description for some of the applications that fall into this category.
MyHeart [15] is a wearable intelligent system developed to monitor and prevent cardiovascular disease. It is considered as one of the largest biomedical project during the period between 2004 and 2007 as it involved 33 organizations from 10 countries with an overall budget of 35 million Euros. The system starts with an initialization process to build a customized profile for the patient by collecting his/her weight, blood pressure, and cholesterol level. Based on these readings, the system starts a daily routine of collecting physiological signs, such as the rates of heart and respiration, from the on-body sensors and activity level from a fitness bike. After that, the collected data are analyzed on the User Interface (UI) device, and then displayed to the patient. The data can be further examined by forwarding it to a remote server. The system can also work as an activity coach by automatically changing the level of exercises based on the analyzed data.
Khawandi et al. [35] developed a system that uses a webcam and a heart rate sensor for fall detection purpose. Data acquired from the sensors are transmitted to a home gateway for processing using a neural network (Multi-Layer Perceptron (MLP)). The gateway places an emergency alert to the care-holders if a fall is detected. Several webcams are needed to cover the patient’s area. The system uses a face detection mechanism to switch between the webcams and keep track of the patient. Each webcam collects three details about the patient: the angle of the image, the aspect ratio of the image, and the speed of the patient’s movement. It then sends the data to the MLP for processing. Rather than just detecting fall, Horta et al. [39] proposed a smartphone application that detects and creates fall prevention strategies. The system does not only rely on the accelerometer to identify the patient’s physical activity, but also uses other medical sensors such as electrocardiogram, electromyography, blood pressure, electro dermal activity, and temperature. This combination of sensors provides better fall detection technique.
The Enhanced Sustained Usev Monitovring System (ESUMS) [42] developed a smartphone application for remote monitoring of patients with heart problems who are discharged from hospital. The monitoring system consists of a wearable device that is secured to the patient’s chest to collect skin temperature, activity level, heart rate and posture. This wearable device operates by a battery that can be charged using the regular phone charger. The collected signals are transmitted to a smartphone device through Bluetooth for live display. After that, the data are sent to the health center for monitoring through the cellular network.
Selim et al. [37] proposed a multiple hierarchical healthcare system for elderly. Each layer reports to and controlled by the higher layer. Layer 1 consists of sensors grouped into small units called Sensor Processing Units (SPUs). These Unites are responsible for collecting the patient’s vital data, processing, storing, and forwarding it to the higher layer. SPUs also allow the integration of new sensors (plug-and-play). Layer 2 consists of Low Level Processing Units (LLPUs) that combine the transmitted data from the SPUs and detect irregular events. The communication between the SPUs and LLPUs is bidirectional; which means that besides receiving data from the SPUs, LLPUs also send signals to the SPUs to execute determined tasks such as modifying the frequency of the data acquisition in the sensors. Layer 3 consists of a High Level Processing Unit (HLPU) that stores the received data sent by LLPUs. Furthermore, the HLPU process the collected data and can detect undiagnosed diseases.
The recent advancement in the smartwatch industry started to embed medical sensors that are capable of monitoring patients. For example, the newest Apple Watch 4 [68], Samsung Gear S3 [69], and BLOCKS Core [70] have sensors to track heart rate. There is still a lack of developed application that rely completely on smartwatch. The convenience of wearing a smartwatch and the ability to monitor patients in a free-living environment provide great potentials to advance the healthcare monitoring systems. Kheirkhahan et al. [49] developed a smartwatch system for Real-time and Online Assessment and Mobility Monitoring (ROAMM). The system monitors patients in a free-living environment to identify their physical activity by using the accelerometer and GPS sensors. Additionally, the system provides an ecological momentary assessments through a Likert scale displayed on the smartwatch. Data collection and processing are done on the smartwatch. A remote server is used for data storage, retrieval, reporting and monitoring.
Focused studies in healthcare systems
There are some published papers targeting specialized areas in healthcare systems. These studies include: healthcare systems testing, healthcare database issues, social media, and data science. These systems will be presented in the following subsections.
Healthcare systems testing
Testing is a very important stage in any system development process in which the system is assessed against certain functionalities based on its purpose. Testing healthcare applications is not an easy process, since it involves interaction between human and physical components. The sensing devices should be installed at patient’s house, and volunteers should be recruited to be recorded at their homes. This is difficult to achieve, therefore alternative solutions have been proposed to evaluate how typical users will react to the proposed healthcare systems.
Living labs
Living Labs are homes equipped with sensing and monitoring devices installed on standard furniture. The main purpose of these labs is to record the normal human activities. Human activities can be detected and recorded through two approaches: ubiquitous sensors, which is the typical approach, and the computer vision (cameras), which is considered somehow a new approach [71, 72]. Volunteers are recruited in these homes to do normal activities, so that behaviors and interactions can be recorded and studied. Finally, a dataset is generated containing behaviors of a set of patients which can be used by other researchers [73].
System emulation
Living labs may not be available for all researchers, therefore imitating a living lab is considered as an alternative way for testing. Gama et al. [74] created a model to emulate the basic actions of a person at home. This model contains one door, two windows, gas tube, water tube, and an electrical outlet equipped with sensors to detect their states.
Creating datasets
A healthcare monitoring dataset is a list of patients with their recorded values. Some researchers have collected medical and environmental data from volunteers in smart homes and made this dataset available to the research community to test their applications based on it. DMLSmartActions [75] is a dataset created by recording the behavior of 16 subjects using a Kinect camera. After the data was collected, it was classified into 12 different actions which represent the human’s daily life at home. This dataset consists of 932 annotated video samples that are openly available. In [76], the authors used local measurements in terms of spatio-temporal interest points [77] to represent and recognize motion patterns such as human actions. The generated dataset includes 2319 sequences for 6 human actions. However, Weinland et al. [78] used 3D motion descriptors to build models in space and time for human actions and generated 1188 sequences for 11 human actions. In AILISA [79], 1492 days of human activities were collected using presence sensors placed on walls. After that the data was recorded to generate a dataset to be available for future researchers. Table 2 lists some of the video datasets that study the human behaviors.
System simulation
Providing artificial data very similar to real data is another alternative solution to test the healthcare applications. In AILISA project [79], a mathematical model was built on a dataset, which depends on Hidden Markov Models (HMM) [80] and Pólya’s urn model [81]. The model simulates the human activities in order to be used as a benchmark by the researchers.
Standardized testing
Due to the increase of the proposed healthcare systems, a testing and certification methodology became a necessity. Faria et al. [82] define a novel testing methodology that can be applied to healthcare systems. The main goal of certifying the products and services is to affirm their acquiescence with the predefined regulations concerning safety, conservation, energy consumption, compatibility, quarantine, and impact on the environment. The Food and Drug Administration (FDA) has issued a report for the design considerations of the devices that are intended for home use. These considerations involve the design of devices, the user interface (UI), the labeling and instructions of use, and finally the user training and certification. Taking these considerations into account helps in producing devices that suit the home environment and assures the safety and effectiveness of their use [83].
Healthcare database issues
Collected data from patients are usually sent to a remote server for analysis and storing. The stored data helps in keeping a record for each patient and giving the doctor a background about any patient. Furthermore, it can be subjected to further analysis, such as data mining to extract insightful knowledge and predict the existence of new diseases [84]. The exponential increase of the generated medical data adds a huge burden to the traditional relational databases. In order to adopt the increase of data, support new IoT applications, and serve more users, migrating to cloud-based NoSQL databases becomes an urgent necessity. Tomar et al. [85] discuss the challenges and techniques to migrate to NoSQL cloud databases.
Data science in healthcare monitoring
Data science is not a completely new research area. The tremendous amount of data generated everyday allowed us to apply the known machine learning algorithms to extract insightful knowledge. Applying data science techniques has great potential in the medical field. Remote healthcare applications started recently to use these techniques for early identifications of medical incidents such as strokes and falls and for extracting hidden information. There is a need to build robust machine learning models based on the data generated from remote healthcare monitoring systems. This requires the adoption of data science in the newly developed remote healthcare applications. Forkan et al. [46] developed a personalized monitoring application by implementing decision-making algorithms using cloud services. The application runs association rules to find correlation between attributes and threshold values of the vital signals and then supervised machine learning algorithms to predict patient-specific incidents. Hassan et al. [50] also developed a cloud-based system to provide real-time healthcare monitoring dedicated for elderly with chronic conditions. The system uses the medical features of patients to predict the overall health condition by running supervised machine learning algorithms. There is still a lack of applications that take advantage of the power of data science. Wang et al. [86] discuss the capabilities of big data in the healthcare application. In their paper, they identified five data analytics capabilities in healthcare applications: “analytical capability for patterns of care, unstructured data analytical capability, decision support capability, predictive capability, and traceability”.
Healthcare social media and P2P networks
In the recent few years, social networks invaded our life and became part of our daily activities. Healthcare systems can also integrate social networks in their architecture and this is what the authors in [87] proposed. The authors propose a system called P2Care, which is based on P2P networks. The system groups the patients and doctors together according to common interests and delivers customized services in a scalable, efficient, and network-friendly manner. Through this health-social network, the searching and sharing of data are faster. Moreover, this network avoids network flooding problems and provides a fast response time.
Khorakhun and Bhatti [40] is another work inspired by social networks. The authors developed a Facebook application to send alerts to four different actors in the patient’s social network, including patient, doctor, professional carer, and a family member.
The authors in [41] developed a system that integrates social media, such as Twitter, and healthcare communications standards, such as HL7 v2.x, to followup patients who suffer from cardiovascular diseases. Patients are required to measure their cardiovascular signs and insert the values into an android application. The application encapsulate the values into HL7 v2.x messages that are tweeted to the hospital Twitter account. Once the patient’s information is tweeted, a desktop java application at the hospital side reads and parses the tweet to extract the cardiovascular information and saves them in the local patient’s Electronic Health Record (EHR).
Standards related to healthcare monitoring
Transducers (sensors and actuators) are pervasive. They are found in several real life applications, including but not limited to: industrial automation, environmental condition monitoring, transportation systems, homeland defense, and healthcare. The increased number of sensors and the diversity in design, architectures, and protocols make the integration a very challenging process. Therefore, a coherent standard is needed to overcome the differences in sensors and make them platform independent and interoperable. In this section, we explain the concept of smart sensors and the standards used for healthcare monitoring purposes [88, 89].
Smart transducer
Based on the signal transformation, it can be a sensor or an actuator. If the transducer generates an electrical signal proportional to an environmental phenomenon, such as physical, chemical, or biological, it is then called a sensor. On the other hand, if the transducer accepts an electrical signal and transforms it into motion, it is then called an actuator. Sensors are usually connected to a microcontroller that is able to do signal conditioning, data conversion, and application processing. Recently, integrating a transducer with a micro-controller, and a communication interface into one device that performs all the functions is called a smart transducer.
ISO/IEEE 11073
ISO/IEEE 11073 is a set of standards that facilitate the way that the medical sensors can communicate with the remote servers. These standards define the mechanism for capturing the patient’s data automatically and the devices’ operational configurations. There were different nomenclatures for this set of standards, which are: ISO 11073, IEEE 1073, ISO/IEEE 11073, or X73 [90, 91]. The main goals of this set of standards are to facilitate the interoperability of the different devices in the system, real-time plug-and-play, and the exchange of patients’ data with the medical experts [24]. The ISO/IEEE 11073 standard consists of three models, each one is responsible for a specific domain (information, service, and communication). These models work altogether to achieve the following tasks: data definition and representation, read and write methods definition, and agent-manager communication.
Open geospatial consortium (OGC)-sensor web enablement (SWE)
OGC is a non-profit international organization for standardization. It consists of more than 400 members, including: governmental, industrial, and academic institutions. The Sensor Web Enablement (SWE) was founded in 2003 to develop a suite of standards to enable sensor web, which means facilitating the work of the applications by making the web resources of the sensors available [89]. There is an integration between the IEEE 1451 and OGC-SWE. The goal of the IEEE 1451 set of standards is to transfer the sensor’s metadata and the collected data from the lower layer (physical layer) to the upper layer (communication layer). On the other hand, OGC-SWE is concerned with transferring the data to the application layer. Therefore, these sets of standards are complementary to each other and can be used together to bring sensor data from the physical layer into high-level sensor applications in a seamless way [92].
Health level seven (HL7)
Health Level Seven (HL7) is a messaging standard for interoperability of health information technology in over 55 countries. It allows different medical entities, such as physicians and nurses, to exchange various types of data related to the patient’s status, such as exchanging reports, images, patient’s history, and biomedical data. Exchanging these data is a burdensome task without having a standard to follow, since medical data has different formats and interfaces. HL7 solved this problem by developing a set of open standards that specify the format of the messages and ease the communication between medical entities. HL7 is designed to support both central and distributed patient care environments [93,94,95].
Universal open platform reference specification for ambient assisted living (UniversAAL)
UniversAAL is an open standardization platform that aims to build Ambient Assisted Living (AAL) solutions in a technically feasible and economically viable ways. UniversAAL contributed with standards development organizations in two different ways. First, UniversAAL proposed an encryption standard to protect privacy of elderly, which has been accepted by the Integrating Healthcare Enterprise (IHE) initiative. Second, UniversAAL committed to the expansion of AAL technologies and market. A standardized reference architecture and platform for AAL technology can support further growth of AAL market and facilitate cheaper, faster and more efficient development of AAL services. Therefore, UniversAAL is determined to contribute to the definition of AAL reference use cases, model and reference architecture, which is one of the stepping stones in this process [96].
TEDS, explained in “Standards related to healthcare monitoring”, is one of the distinguishing aspects of the IEEE 1451 standard, where specific sensor information is stored and it enables the possibility of the plug-and-play functionality. The data structure in the TEDS is not the same as the one in the HL7, which makes it hard for the two standards to inter-operate. The authors of [24] focused on this problem and proposed a solution to translate data in the TEDS into the HL7 format. The authors developed a monitoring system that collects data from patients and transmit it to the hospital. In order to allow the two standards to talk with each other, an interface is implemented in both the patient’s and hospital’s sides.
The system proposed in [14] adopted and implemented the X73 (ISO/IEEE 11073) standards on a microcontroller-based sensor hardware. The design of the system provides the plug-and-play capability for the medical devices. The monitoring functionalities are achieved through the use of sensor units, base stations, data loggers, and wireless modules that use Bluetooth protocol.
Discussion and conclusion
Following the presentation of several aspects of e-health, now we list the challenges noted during the development of the healthcare systems. These challenges, which are not necessarily listed in order of importance, include but are not limited to: power consumption, biological effects, privacy and security, mobility, portability, reliability, availability, unobtrusiveness, acceptability, interoperability, scalability, testing, cost, and cloud and fog computing. At the end of this section, we summarize these challenges and propose potential solutions in Table 3.
-
Smart Technology Acceptance Among Older Population
Remote healthcare monitoring systems rely on using cutting edge technologies in their design to achieve better results. However, these systems are usually designed to serve chronically ill patients and older population. Therefore, it is essential to understand the perception of the served population toward the use of smart devices such as smartphones, smartwatches and tablets and the barriers faced by them. There are studies in the literature that assessed the perception of the older population to use smart technology. Vaportzis et al. [97] studied the perception of 18 older adults (65-76 years old) toward using tablets. The output of the study states that older adults understand the importance of using smart technology to monitor their health status and to stay connected to the society. However, most of them experience lack of confidence to use new devices. Another study by Ding et al. [98] assessed the impressions of 98 cardiovascular patients (68 ± 10 years old) toward using smartphones and smartwatches for heart rhythm monitoring. 78% of patients reported the easiness of using smart devices for rhythm monitoring compared to the traditional monitoring devices. In order to promote acceptability and usability of smart devices, the design phase has to take into consideration the issues that affect the lack of confidence, such as lack of knowledge, lack of instructions and guidance, medical barriers such as vision, motor skills, or concentration, and the high cost of new devices. User friendly designs, use of signs rather than small text, use of large buttons, use of bezel as in Samsung Gear, and exposure therapy can mitigate the lack of confidence and help to reduce the gap between older adults and smart technology.
-
Power Consumption
Batteries are considered the main bottleneck of sensors in tier.1. Recharging the batteries can be one of the solutions, but with elderly it could be a difficult task, especially with patients who suffer from dementia; as they may forget to recharge them [52]. Reducing power consumption of sensors is considered a more sustainable solution and guarantees longterm monitoring with a minimum amount of maintenance. Yoo et al. [99] developed an ECG sensor that does not include a battery and can be powered wirelessly by a chest band. This charging band can send signals to locate the sensors and then provide the necessary power wirelessly. The authors in [100] introduce wireless sensor nodes that operates in a low power by focusing on component and system levels to optimize the power consumption for radio and signal processing core. Bhatia et al. [1] stated that wireless transmission technologies like Bluetooth and WiFi are not energy efficient. In addition, small batteries (coin size) cannot provide energy for a long time. Therefore, many researches are moving toward developing low power sensors and minimizing the processing requirements. Additionally, a better utilization of the hardware devices in any network, including the health monitoring network, can be achieved through a proper programming techniques [101].
-
Biological Effects
The biological effect (bioeffect) of the wireless biomedical sensor networks is one of the serious challenges in healthcare systems. The radiation of the radio frequency (RF) for a long period of time has negative impacts on the patients’ health. Due to the fact that sensors are fundamental components of the healthcare monitoring systems and the communication between them and other devices is irreplaceable, the bioeffect caused by the RF communication should be carefully studied. Ren and Meng [102] studied the factors that can reduce the negative health effects caused by the RF radiation. These factors are derived from the fact that by reducing the transmissions and the operating period of the sensors, radiation can be reduced consequently. Therefore, the authors suggest to design power scheduling and traffic control algorithms to reduce the radiation.
-
Privacy and Security
The ultimate purpose of any elderly healthcare system is to keep monitoring the patient’s status by collecting the medical and environmental signals and sending them to a remote subsystem for analysis. The transmission of data between the healthcare system tiers makes the system vulnerable to many threats that may break the three security principles CIA (C: confidentiality, I: integrity and A: availability). The authors in [103,104,105,106] summarize the threats and the proposed solutions by each tier. Thota et al. [107] developed a centralized fog computing remote healthcare monitoring system with a focus on building a secure platform for healthcare applications. They discussed authentication, authorization, device tracking and locating, and communication.
-
Mobility and Portability
Monitoring elderly requires placing some sensors on the patient’s body to extract certain medical signals [52]. Furthermore, there is a need for monitoring the patients outdoor (mobile healthcare-mhealth). For these two reasons, having portable and mobile healthcare systems became a necessity to monitor the patients conveniently and everywhere without restricting them to stay in a specific place. The smart shirt, proposed by [108], provides the patients with a high level of mobility and portability. This approach opens for a new research area called smart tech, that can ease the development of mhealth systems.
-
Availability and Reliable Communication
The monitoring subsystem is responsible for monitoring the patients, take proper actions, and generate alerts. These functionalities require real-time monitoring of the patient’s status, therefore, congestion and delay must be handled in the network, especially in critical situations. Moreover, the healthcare architecture must take into consideration high availability and robustness of the network. Given the fact that redundancy and cost have a positive correlation, eventually there should be a way to balance between them [52].
-
Unobtrusiveness and Acceptability
There are some concerns that need to be addressed in the process of healthcare sensors development that will help to maintain the patient’s unobtrusiveness. Healthcare sensors are placed on the person’s body or surrounding him/her. Therefore, they may be obtrusive and bring anxiety to the patient. Some of the body-worn sensors may be heavy, like the one proposed in [109], whereas some sensors are integrated into a shirt as proposed in the eCAALYX project [36] or as a watch [110] which are more easy-to-bear devices [52].
-
Interoperability
A healthcare monitoring system integrates different devices into one operational system. These devices may work on different frequencies or standards which raise interoperability challenge. According to IEEE, interoperability is the ”ability of two or more systems or components to exchange information and to use the information that has been exchanged”. Therefore, the pervasive healthcare systems must be designed to accept the differences in devices and interpret the different messaging formats of other devices [111]. The IEEE P1752 [112] is a working group sponsored by IEEE EMB/Sdts Com launched in Feb. 2017 that aims to define specifications for a mobile health data applications programming interface (API) and standardized representations for mobile health data and metadata
-
Scalability
The easy deployment of healthcare systems is also one of the challenges. Healthcare systems are intended for different profiles of users in different environments. For this reason, the healthcare system should be easily deployable and adaptable. Moreover, the system must be able to support the installation of new devices while in operation [52].
-
Testing
As described in “Focused studies in healthcare systems”, testing is very essential in order to make sure that a system is working as intended. It is considered a hard task if humans are involved, which is the case in testing healthcare monitoring systems. In order to test these systems, the devices should be installed in the patient’s home to monitor the patient for a period of time. This could be a burdensome on patients, therefore, some alternative solutions have been proposed to make the testing more convenient, such as: living labs [73], system emulation [74], creating datasets [75, 76, 78], system simulation [79], and standardized testing [82].
-
Cost and Business Models
Despite the fact that healthcare monitoring systems are intended to reduce the cost of staying at hospitals, however, we have to take into consideration the cost of building and maintaining such systems. At the end, we aim to increase the quality of the system on one hand and decrease the cost of building it on the other hand. Furthermore, payment and coverage in return for the services delivered by the healthcare providers are considered one of the biggest challenges. The American Telemedicine Association (ATA) has published a report showing the coverage and reimbursement policies of 50 states in USA. The report ranks the states based on their support and adoption of telehealth. Rank “A” is considered the highest and ”F” is the lowest. Most of the states fall in rank “B” and “C”, which indicates that most of the states still have limited and restricted policies regarding the coverage of telehealth services [113]. Therefore, there is a need for setting polices that ensure the coverage of the cost of the remote healthcare monitoring services and finding the appropriate business models.
-
Cloud and Fog Computing
Cloud computing provides high storage and processing capabilities that allow the healthcare systems to process the high amount of data generated every day. The authors in [114] discuss the challenges of using cloud computing within the healthcare systems by defining six aspects: privacy, legalization, technical, medical, organizational, and economical. These aspects inherit the same challenges mentioned above, but applied on cloud technology. As discussed earlier in this paper, hospitals and medical systems generate a huge amount of data. Sending this amount to the cloud consumes bandwidth and systems may suffer from latency issues, which becomes a critical issue in case of emergencies. For this reason, fog computing was introduced to solve this issue by deploying processing units locally with minimal requirements to process the collected data. Only updates and anomalies are sent to the cloud for further processing and reporting. Kraemer et al. [115] discuss the benefits and challenges of the fog computing with respect to the healthcare applications.
In the following, we present a summary of the key points we observed from reviewing the presented healthcare applications and future directions that researchers need to address in this area of research.
-
Most of the remote healthcare monitoring systems use a three-tier architecture that is composed of: sensors to collect vital signals, a local device and/or a gateway to transfer (and process in some cases) the data to the remote site, and a remote server for storage, processing, and alerting.
-
Most of the analysis of the patient’s data is done in a remote server located at the hospital side, and the local system is mostly used for data acquisition, integration, and transmission. Recently, applications are moving towards cloud computing and fog computing.
-
Systems that are used to monitor patients in both inside and outside environments require using portable devices, such as: tablets, smartphone or smartwatch. This highlights the significant role the portable technology plays in the advancement of healthcare systems. This includes their portability and functional capability.
-
Zigbee and Bluetooth protocols are used widely in healthcare systems. Zigbee is featured with its low power consumption compared with other protocols. However, Bluetooth is preferred when smartphones and smartwatches are used. Recently, applications tend to adopt low power wireless standards and energy saving techniques to prolong the battery life.
-
Although security is considered a crucial feature in healthcare applications, only a few systems implement strong security mechanisms. The focus in most applications is on efficient transfer of data, storage and analysis. However, maintaining the privacy of patients’ information is of the same importance.
-
Reducing power consumption is usually achieved through using low power transmission standards such as Zigbee. There are a few systems tried to achieve it in other techniques such as optimizing sleep mode or developing new interfaces. Combining both approaches would have better outcomes.
-
Cloud computing provides high processing and storage capabilities. The majority of new applications have cloud computing as an essential component of their infrastructure. New advances in cloud computing such as fog computing started to appear in some of the new applications.
-
Recent healthcare systems started to support the integration of third party “commercial-off-the-shelf” medical monitoring devices. Standards and policies are needed to provide better outcomes.
-
Data science is powerful in providing insightful outcomes especially in the medical area. There is a great potential of adopting it in the remote healthcare monitoring systems. Recent applications exploit the capabilities of machine learning techniques to provide early prediction and extract hidden patterns.
-
There is a great interest in Autonomous Vehicles lately. Developing healthcare monitoring applications in the vehicle to monitor chronically ill patients and older populations have great implications on the medical status and social involvement of patients. The ability to build a decision-making platform that uses the vital signals of patients and control the vehicle in case of medical emergencies will have great benefits.
The advancement in technology has allowed us to monitor patients at home without the need for long stay at the hospital. In this paper, we surveyed the remote healthcare applications and provided a categorization according to the sensing they provide: medical sensing, activity and environmental sensing, and integrated medical, activity and environmental sensing. Additionally, we identified the common architecture used by the current healthcare applications. Moreover, the challenges introduced in healthcare applications were studied and presented. Although there are several proposed healthcare monitoring systems, there are still some challenges to overcome. Some areas are still immature in healthcare systems, such as sensor minimization, security, power efficiency, cloud computing, data science, and sensor standardization. Addressing the challenges will allow remote healthcare monitoring systems to be more intelligent, pervasive and within the reach of ordinary elderly and chronically ill population.
References
Bhatia, D., Estevez, L., and Rao, S.: Energy efficient contextual sensing for elderly care. In: IEEE 29th Annual International Conference on Engineering in Medicine and Biology Society (EMBS), pp. 4052–4055, 2007. https://doi.org/10.1109/IEMBS.2007.4353223.
Ortman, J. M., Velkoff, V. A., and Hogan, H.: An aging nation: the older population in the United States, Washington, DC: US Census Bureau, 25–1140, 2014
Sadri, F., Ambient Intelligence: a survey. ACM Comput. Surv. 43(4):36:1–36:66, 2011. https://doi.org/10.1145/1978802.1978815.
Active Assested Living Programme (ALL), Accessed: Dec 1, 2018. http://www.aal-europe.eu
International Telecommunication Union (ITU), Accessed: Dec 1, 2018. http://www.itu.int/en/Pages/default.aspx
The International Federation for Medical and Biological Engineering (IFMBE), Accessed: Dec 1, 2018. http://ifmbe.org
World Health Organization (WHO), Accessed: Dec 1, 2018. http://www.who.int/en
Health-IT, Accessed: Dec 1, 2018. http://committees.comsoc.org/ehealth
Anliker, U., Ward, J., Lukowicz, P., Troster, G., Dolveck, F., Baer, M., Keita, F., Schenker, E., Catarsi, F., Coluccini, L., Belardinelli, A., Shklarski, D., Alon, M., Hirt, E., Schmid, R., and Vuskovic, M., AMON: a wearable multiparameter medical monitoring and alert system. IEEE Trans. Inf. Technol. Biomed. 8(4):415–427, 2004. https://doi.org/10.1109/TITB.2004.837888.
Sung, M., Marci, C., and Pentland, A., Wearable feedback systems for rehabilitation. J. Neuroeng. Rehabil. 2(1):17, 2005.
Di Rienzo, M., Rizzo, F., Parati, G., Brambilla, G., Ferratini, M., and Castiglioni, P.: MagIC system: a new textile-based wearable device for biological signal monitoring. applicability in daily life and clinical setting. In: IEEE 27th Annual International Conference on Engineering in Medicine and Biology Society (EMBS), pp. 7167–7169, 2005. https://doi.org/10.1109/IEMBS.2005.1616161.
Jih, W.-R., Hsu, J. Y.-J., Wu, C.-L., Liao, C.-F., and Cheng, S.-Y.: A multi-agent service framework for context-aware elder care. In: Proceedings of AAAMAS Workshop on Service-Oriented Computing and Agent-Based Engineering, pp. 61–75, 2006.
Wang, Q., Shin, W., Liu, X., Zeng, Z., Oh, C., AlShebli, B., Caccamo, M., Gunter, C., Gunter, E., Hou, J., Karahalios, K., and Sha, L., I-living: an open system architecture for assisted living. Systems, Man and Cybernetics 5:4268–4275, 2006. https://doi.org/10.1109/ICSMC.2006.384805.
Yao, J., and Warren, S., Applying the ISO/IEEE 11073 standards to wearable home health monitoring systems. J. Clin. Monit. Comput. 19(6):427–436, 2005. https://doi.org/10.1007/s10877-005-2033-7.
Harris, M., and Habetha, J.: The MyHeart project: a framework for personal health care applications. In: Computers in Cardiology, pp. 137–140, 2007. https://doi.org/10.1109/CIC.2007.4745440.
She, H., Lu, Z., Jantsch, A., Zheng, L.-R., and Zhou, D.: A network-based system architecture for remote medical applications. In: Network Research Workshop, Vol. 27, 2007.
Lymberis, A., and Paradiso, R.: Smart fabrics and interactive textile enabling wearable personal applications: R&D state of the art and future challenges. In: IEEE 30th Annual International Conference on Engineering in Medicine and Biology Society (EMBS), pp. 5270–5273, 2008. https://doi.org/10.1109/IEMBS.2008.4650403.
Churcher, G., Bilchev, G., Foley, J., Gedge, R., and Mizutani, T.: Experiences applying sensor web enablement to a practical telecare application. In: 3rd International Symposium on Wireless Pervasive Computing (ISWPC), pp. 138–142, 2008. https://doi.org/10.1109/ISWPC.2008.4556183.
Lorincz, K., Chen, B.-R., Challen, G. W., Chowdhury, A. R., Patel, S., Bonato, P., and Welsh, M.: Mercury: a wearable sensor network platform for high-fidelity motion analysis. In: Proceedings of the 7th Conference on Embedded Networked Sensor Systems, pp. 183–196. ACM, 2009.
Shahram Nourizadeh, Y.-Q.S., Deroussent, C., and Thomesse, J.-P.: A distributed elderly healthcare system. In: Mobihealth, 2009.
Fernández-Luque, F., Zapata, J., Ruiz, R., and Iborra, E.: A wireless sensor network for assisted living at home of elderly people, Bioinspired Applications in Artificial and Natural Computation, 65–74, 2009
Spanoudakis, N., Grabner, B., Kotsiopoulou, C., Lymperopoulou, O., Moser-Siegmeth, V., Pantelopoulos, S., Sakka, P., and Moraitis, P.: A novel architecture and process for ambient assisted living - the HERA approach. In: Information Technology and Applications in Biomedicine (ITAB), pp. 1–4, 2010. https://doi.org/10.1109/ITAB.2010.5687615.
Saponara, S., Donati, M., Bacchillone, T., Fanucci, L., Sanchez-Tato, I., Carmona, C., and Barba, P.: Remote monitoring of vital signs in patients with chronic heart failure: sensor devices and data analysis perspective. In: Sensors Applications Symposium (SAS), pp. 1–6, 2012.
Kim, W., Lim, S., Ahn, J., Nah, J., and Kim, N., Integration of IEEE 1451 and HL7 exchanging information for patients’ sensor data. J. Med. Syst. 34(6):1033–1041, 2010. https://doi.org/10.1007/s10916-009-9322-5.
Nourizadeh, S., and Deroussent, C.: Maisons vill’âge®;: smart use of home automation for healthy aging. In: International Conference on Smart Homes and Health Telematics, pp. 271–275. Springer, 2011.
Martín, P., Sánchez, M., Álvarez, L., Alonso, V., and Bajo, J.: Multi-agent system for detecting elderly people falls through mobile devices. In: Ambient Intelligence-Software and Applications, pp. 93–99. Springer, 2011.
Giokas, K., Kouris, I., and Koutsouris, D.: Autonomy, motivation and individual self-management for COPD patients, the amica project. In: Wireless Mobile Communication and Healthcare, Vol. 55 of Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering, Springer Berlin Heidelberg, pp. 49-53, 2011.
Mateska, A., Pavloski, M., and Gavrilovska, L.: RFID and sensors enabled in-home elderly care. In: Proceedings of the 34th International Convention, pp. 285–290. MIPRO, 2011.
Bekiaris, A., Mourouzis, A., and Maglaveras, N.: The REMOTE AAL project: remote health and social care for independent living of isolated elderly with chronic conditions. In: Universal Access in Human-Computer Interaction. Context Diversity, Vol. 6767 of Lecture Notes in Computer Science, Springer Berlin Heidelberg, pp. 131–140, 2011.
Wang, C., Wang, Q., and Shi, S.: A distributed wireless body area network for medical supervision. In: Instrumentation and Measurement Technology Conference (I2MTC), pp. 2612–2616, 2012. https://doi.org/10.1109/I2MTC.2012.6229260.
Tang, Y., Wang, S., Chen, Y., and Chen, Z.: PPCare: a personal and pervasive health care system for the elderly. In: Ubiquitous Intelligence and Computing, pp. 935–939, 2012.
Belbachir, A., Litzenberger, M., Schraml, S., Hofstatter, M., Bauer, D., Schon, P., Humenberger, M., Sulzbachner, C., Lunden, T., and Merne, M.: CARE: a dynamic stereo vision sensor system for fall detection. In: IEEE International Symposium on Circuits and Systems (ISCAS), pp. 731–734, 2012. https://doi.org/10.1109/ISCAS.2012.6272141.
Yi He, Y. L., and Bao, S.-D.: Fall detection by built-in tri-accelerometer of smartphone. In: IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), pp. 184–187, 2012. https://doi.org/10.1109/BHI.2012.6211540.
Ahlrichs, C., Samà, A., Simon, J., Herrlich, S., and Rodrıguez-molinero, A.: Help: optimizing treatment of Parkinson’s disease patients. In: 3Rd International Conference on the Elderly and New Technologies. Castellón, Spain, 2012.
Khawandi, S., Daya, B., and Chauvet, P.: Applying neural network architecture in a multi-sensor monitoring system for the elderly. In: The Sixth International Conference on Advanced Engineering Computing and Applications in Sciences (ADVCOMP), pp. 15–22, 2012.
Bourke, A., Prescher, S., Koehler, F., Cionca, V., Tavares, C., Gomis, S., Garcia, V., and Nelson, J.: Embedded fall and activity monitoring for a wearable ambient assisted living solution for older adults. In: Engineering in Medicine and Biology Society (EMBC), pp. 248–251, 2012. https://doi.org/10.1109/EMBC.2012.6345916.
Selim, B., Iraqi, Y., and Choi, H.-J.: A multi-sensor surveillance system for elderly care. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 502–506, 2013. https://doi.org/10.1109/HealthCom.2013.6720728.
Heikkila, T., Strommer, E., Kivikunnas, S., Jarviluoma, M., Korkalainen, M., Kyllonen, V., Sarjanoja, E., and Peltomaa, I., Low intrusive Ehealth monitoring: human posture and activity level detection with an intelligent furniture network, Wireless Communications. IEEE 20(4):57–63, 2013.
Horta, E., Lopes, I., Rodrigues, J., and Proenca, M.: A mobile health application for falls detection and biofeedback monitoring. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 36–40, 2013. https://doi.org/10.1109/HealthCom.2013.6720634.
Khorakhun, C., and Bhatti, S.: Remote health monitoring using online social media systems. In: 6th Joint IFIP Conference on Wireless and Mobile Networking (WMNC). https://doi.org/10.1109/WMNC.2013.6548953, 2013.
Trigo, J., Eguzkiza, A., Martinez-Espronceda, M., and Serrano, L.: A cardiovascular patient follow-up system using twitter and HL7. In: Computing in Cardiology Conference (CinC), pp. 33–36, 2013.
Seeberg, T., Vedum, J., Sandsund, M., Austad, H., Liverud, A., Vardoy, A., Svagard, I., and Strisland, F.: Development of a wearable multisensor device enabling continuous monitoring of vital signs and activity. In: IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), pp. 213–218, 2014. https://doi.org/10.1109/BHI.2014.6864342.
Fekr, A., Radecka, K., and Zilic, Z., Design and evaluation of an intelligent remote tidal volume variability monitoring system in e-health applications. IEEE J. Biomed. Health Inform. 19(5):1532–1548, 2015. https://doi.org/10.1109/JBHI.2015.2445783.
Yang, Z., Zhou, Q., Lei, L., Zheng, K., and Xiang, W., An IoT-cloud based wearable ecg monitoring system for smart healthcare. J. Med. Syst. 40(12):286, 2016.
Mondol, M. A. S., Emi, I. A., and Stankovic, J. A.: MedRem: an interactive medication reminder and tracking system on wrist devices. In: Wireless Health, pp. 46–53, 2016.
Forkan, A. R. M., Khalil, I., Ibaida, A., and Tari, Z., BDCAm: big data for context-aware monitoring—a personalized knowledge discovery framework for assisted healthcare. IEEE Transactions on Cloud Computing 5(4): 628–641, 2017.
Vora, J., Tanwar, S., Tyagi, S., Kumar, N., and Rodrigues, J. J. P. C.: FAAL: fog computing-based patient monitoring system for ambient assisted living. In: 2017 IEEE 19th International Conference on e-Health Networking, Applications and Services (Healthcom), pp. 1–6, 2017. https://doi.org/10.1109/HealthCom.2017.8210825.
Mauldin, T., Canby, M., Metsis, V., Ngu, A., and Rivera, C., Smartfall: a smartwatch-based fall detection system using deep learning. Sensors 18(10):3363, 2018.
Kheirkhahan, M., Nair, S., Davoudi, A., Rashidi, P., Wanigatunga, A. A., Corbett, D. B., Mendoza, T., Manini, T. M., and Ranka, S., A smartwatch-based framework for real-time and online assessment and mobility monitoring. J. Biomed. Inform. 89:29–40, 2019.
Hassan, M. K., El Desouky, A. I., Elghamrawy, S. M., and Sarhan, A. M.: Intelligent hybrid remote patient-monitoring model with cloud-based framework for knowledge discovery, Computers & Electrical Engineering
Acampora, G., Cook, D., Rashidi, P., and Vasilakos, A., A survey on ambient intelligence in healthcare. Proc. IEEE 101(12):2470–2494, 2013.
Alemdar, H., and Ersoy, C., Wireless sensor networks for healthcare: a survey. Comput. Net. 54(15): 2688–2710, 2010.
Eathernet Alliance, Accessed: Dec 1, 2018. https://ethernetalliance.org
Universal Serial Bus (USB), Accessed: Dec 1, 2018. https://www.usb.org
Ko, J., Lu, C., Srivastava, M., Stankovic, J., Terzis, A., and Welsh, M., Wireless sensor networks for healthcare. Proc. IEEE 98(11):1947–1960, 2010.
Bluetooth Low Energy (BLE), Accessed: Dec 1, 2018. https://www.bluetooth.com
ANT+, Accessed: Dec 1, 2018. https://www.thisisant.com
Rafio-Frequency Identification (RFID), Accessed: Dec 1, 2018. https://www.rfidinc.com
RuBee, Accessed: Dec 1, 2018. http://ru-bee.com
IPv6 over Low-Power Wireless Area Networks (6LoWPAN), Accessed: Dec 1, 2018. http://6lowpan.tzi.org
DASH7 Alliance, Accessed: Dec 1, 2018. http://www.dash7-alliance.org
Z-Wave, Accessed: Dec 1, 2018. https://www.z-wave.com
Ultra-Wide Band (UAB), Accessed: Dec 1, 2018. https://www.etsi.org
Near Field Communication (NFC), Accessed: Dec 1, 2018. http://nearfieldcommunication.org
Wan, J., Zou, C., Ullah, S., Lai, C.-F., Zhou, M., and Wang, X., Cloud-enabled wireless body area networks for pervasive healthcare, Network. IEEE 27(5):56–61, 2013. https://doi.org/10.1109/MNET.2013.6616116.
Haescher, M., Matthies, D. J., Srinivasan, K., and Bieber, G.: Mobile assisted living: smartwatch-based fall risk assessment for elderly people. ACM, 2018
Lutze, R., Baldauf, R., and Waldhör, K.: Dehydration prevention and effective support for the elderly by the use of smartwatches. https://doi.org/10.1109/HealthCom.2015.7454534, 2015
Apple Watch Series 4, Accessed: Dec 1, 2018. https://www.apple.com/apple-watch-series-4
Samsung Gear 3, Accessed: Dec 1, 2018. https://www.samsung.com/global/galaxy/gear-s3
BLOCKS Core, Accessed: Dec 1, 2018. https://www.chooseblocks.com
Benmansour, A., Bouchachia, A., and Feham, M., Multioccupant activity recognition in pervasive smart home environments. ACM Comput. Surv. 48(3):34:1–34:36, 2015. https://doi.org/10.1145/2835372.
Rodríguez, N. D., Cuéllar, M. P., Lilius, J., and Calvo-Flores, M. D., A survey on ontologies for human behavior recognition. ACM Comput. Surv. 46(4):43:1–43:33, 2014. https://doi.org/10.1145/2523819.
Intille, S., Larson, K., Tapia, E., Beaudin, J., Kaushik, P., Nawyn, J., and Rockinson, R.: Using a live-in laboratory for ubiquitous computing research. In: Pervasive Computing, Vol. 3968 of Lecture Notes in Computer Science, Springer Berlin Heidelberg, pp. 349–365, 2006.
Gama, O., and Simoes, R.: A platform to emulate ambient assisted living environments. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 46–50, 2013. https://doi.org/10.1109/HealthCom.2013.6720636.
Amiri, S., Pourazad, M., Nasiopoulos, P., and Leung, V.: Non-intrusive human activity monitoring in a smart home environment. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 606–610, 2013. https://doi.org/10.1109/HealthCom.2013.6720748.
Schuldt, C., Laptev, I., and Caputo, B.: Recognizing human actions: a local SVM approach. In: Proceedings of the 17th International Conference on Pattern Recognition (ICPR), Vol. 3, pp. 32–36, 2004.
Laptev, I., On space-time interest points. Int. J. Comput. Vis. 64(2-3):107–123, 2005. https://doi.org/10.1007/s11263-005-1838-7.
Weinland, D., Ronfard, R., and Boyer, E., Free viewpoint action recognition using motion history volumes. Comput. Vis. Image Underst. 104(23):249–257, 2006.
Noury, N., and Hadidi, T.: Simulation of human activity in a health smart home with HMM. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 125–129, 2013. https://doi.org/10.1109/HealthCom.2013.6720652.
Eddy, S. R., Hidden Markov models. Curr. Opin. Struct. Biol. 6(3):361–365, 1996. https://doi.org/10.1016/S0959-440X(96)80056-X.
Hoppe, F., Plya-like Urns and the Ewens’ sampling formula. J. Math. Biol. 20(1):91–94, 1984. https://doi.org/10.1007/BF00275863.
Faria, J., Lima, B., Boldt Sousa, T., and Martins, A.: A testing and certification methodology for an ambient-assisted living ecosystem. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 585–589, 2013. https://doi.org/10.1109/HealthCom.2013.6720744.
FDA Draft Guidance for Industry and FDA Staff - Design Considerations for Devices Intended for Home Use. Dec. 12, 2012. U.S. Food and Drug Administration, accessed: Dec 1, 2018. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM331681.pdf
Moor, G. D., Sundgren, M., Kalra, D., Schmidt, A., Dugas, M., Claerhout, B., Karakoyun, T., Ohmann, C., Lastic, P.-Y., Ammour, N., Kush, R., Dupont, D., Cuggia, M., Daniel, C., Thienpont, G., and Coorevits, P., Using electronic health records for clinical research: the case of the {EHR4CR} project. J. Biomed. Inform. 53:162–173, 2015. https://doi.org/10.1016/j.jbi.2014.10.006. http://www.sciencedirect.com/science/article/pii/S1532046414002263.
Tomar, D., Bhati, J. P., Tomar, P., and Kaur, G.: Migration of healthcare relational database to NoSQL cloud database for healthcare analytics and management. In: Healthcare Data Analytics and Management, pp. 59–87. Elsevier, 2019.
Wang, Y., Kung, L., and Byrd, T. A., Big data analytics: understanding its capabilities and potential benefits for healthcare organizations. Technol. Forecast. Soc. Chang. 126:3–13, 2018.
Andriopoulou, F., Birkos, K., and Lymberopoulos, D.: P2Care: a dynamic self-organized healthcare network for ubiquitous healthcare environment. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 294–298, 2013. https://doi.org/10.1109/HealthCom.2013.6720688.
Song, E., and Lee, K., Understanding IEEE 1451-networked smart transducer interface standard - What is a smart transducer?, Instrumentation Measurement Magazine. IEEE 11(2):11–17, 2008. https://doi.org/10.1109/MIM.2008.4483728.
Bröring, A., Echterhoff, J., Jirka, S., Simonis, I., Everding, T., Stasch, C., Liang, S., and Lemmens, R., New generation sensor web enablement. Sensors 11(3):2652–2699, 2011. https://doi.org/10.3390/s110302652.
Jung, M., Park, J. G., Kim, J. H., and Cho, J.: Interoperability between medical devices using near field communication. In: International Conference on Information Science and Applications (ICISA), pp. 1–4, 2013. https://doi.org/10.1109/ICISA.2013.6579328.
I. 11073, IEEE Standard for Health Informatics - Point-Of-Care Medical Device Communication - Part 20101: Application Profile - Base Standard, 2004
Song, E., and Lee, K.: Integration of IEEE smart transducers and OGC-SWE using STWS. In: Sensors Applications Symposium (SAS), pp. 298-303. IEEE, 2009. https://doi.org/10.1109/SAS.2009.4801819.
Health Level Seven (HL7), Accessed: Dec 1, 2018. http://www.hl7.org
Eichelberg, M., Aden, T., Riesmeier, J., Dogac, A., Laleci, G. B., and Survey, A, Analysis of electronic healthcare record standards. ACM Comput. Surv. 37(4):277–315, 2005. https://doi.org/10.1145/1118890.1118891. http://doi.acm.org/10.1145/1118890.1118891.
Martínez-García, A., García-García, J., Escalona, M., and Parra-Calderón, C., Working with the {HL7} metamodel in a model driven engineering context. J. Biomed. Inform. 57:415–424, 2015. https://doi.org/10.1016/j.jbi.2015.09.001. http://www.sciencedirect.com/science/article/pii/S1532046415001938.
Universal open platform reference specification for ambient living (UniversAAL), Accessed: Dec 1, 2018. http://universaal.org/index.php/en
Vaportzis, E., Giatsi Clausen, M., and Gow, A. J., Older adults perceptions of technology and barriers to interacting with tablet computers: a focus group study. Front. Psychol. 8:1687, 2017.
Ding, E., Liu, D., Soni, A., Adaramola, O., Han, D., Bashar, S. K., Noh, Y., Chon, K. H., and McManus, D. D.: Impressions of older patients with cardiovascular diseases to smart devices for heart rhythm monitoring. In: 2017 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), pp. 270-271. IEEE, 2017.
Yoo, J., Yan, L., Lee, S., Kim, Y., and Yoo, H.-J., A 5.2 mW self-configured wearable body sensor network controller and a 12 w wirelessly powered sensor for a continuous health monitoring system. IEEE J. Solid State Circuits 45(1):178–188, 2010. https://doi.org/10.1109/JSSC.2009.2034440.
Bachmann, C., Ashouei, M., Pop, V., Vidojkovic, M., Groot, H., and Gyselinckx, B., Low-power wireless sensor nodes for ubiquitous long-term biomedical signal monitoring, Communications Magazine. IEEE 50 (1):20–27, 2012. https://doi.org/10.1109/MCOM.2012.6122528.
Mottola, L., and Picco, G. P., Programming wireless sensor networks: fundamental concepts and state of the art. ACM Comput. Surv. 43(3): 19:1–19:51, 2011. https://doi.org/10.1145/1922649.1922656. http://doi.acm.org/10.1145/1922649.1922656.
Ren, H., and Meng, M.-H.: Bioeffects control in wireless biomedical sensor networks. In: IEEE 3rd Annual Communications Society on, Sensor and Ad Hoc Communications and Networks (SECON), Vol. 3, pp. 896–904, 2006. https://doi.org/10.1109/SAHCN.2006.288579.
Camara, C., Peris-Lopez, P., and Tapiador, J. E., Security and privacy issues in implantable medical devices: a comprehensive survey. J. Biomed. Inform. 55:272–289, 2015. https://doi.org/10.1016/j.jbi.2015.04.007. http://www.sciencedirect.com/science/article/pii/S153204641500074X.
Gkoulalas-Divanis, A., Loukides, G., and Sun, J., Publishing data from electronic health records while preserving privacy: a survey of algorithms. J. Biomed. Inform. 50:4–19, 2014. Special Issue on Informatics Methods in Medical Privacy. https://doi.org/10.1016/j.jbi.2014.06.002 http://www.sciencedirect.com/science/article/pii/S1532046414001403.
Ondiege, B., Clarke, M., and Mapp, G., Exploring a new security framework for remote patient monitoring devices. Computers 6(1):11, 2017.
Partala, J., Ker’́anen, N., S’́arest’́oniemi, M., H’́am’́al’́ainen, M., Iinatti, J., J’́ams’́a, T., Reponen, J., and Sepp’́anen, T.: Security threats against the transmission chain of a medical health monitoring system. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 243–248, 2013. https://doi.org/10.1109/HealthCom.2013.6720675.
Thota, C., Sundarasekar, R., Manogaran, G., Varatharajan, R., and Priyan, M.: Centralized fog computing security platform for iot and cloud in healthcare system. In: Exploring the Convergence of Big Data and the Internet of Things, IGI Global, pp. 141–154, 2018.
Lee, Y.-D., and Chung, W.-Y., Wireless sensor network based wearable smart shirt for ubiquitous health and activity monitoring. Sens. Actuators B 140(2):390–395, 2009. https://doi.org/10.1016/j.snb.2009.04.040.
Li, Z., and Zhang, G.: A physical activities healthcare system based on wireless sensing technology. In: IEEE 13th International Conference on Embedded and Real-Time Computing Systems and Applications (RTCSA), pp. 369–376, 2007. https://doi.org/10.1109/RTCSA.2007.10.
Barth, A., Hanson, M., Powell, H., and Lach, J.: TEMPO 3.1: a body area sensor network platform for continuous movement assessment. In: Sixth International Workshop on Wearable and Implantable Body Sensor Networks (BSN), pp. 71–76, 2009. https://doi.org/10.1109/BSN.2009.39.
Schmitt, L., Falck, T., Wartena, F., and Simons, D.: Novel ISO/IEEE 11073 standards for personal telehealth systems interoperability. In: Joint Workshop on High Confidence Medical Devices, Software, and Systems and Medical Device Plug-and-Play Interoperability (HCMDSS-MDPnP), pp. 146–148, 2007. https://doi.org/10.1109/HCMDSS-MDPnP.2007.9.
P1752 - Standard for Mobile Health Data, accessed: Dec 1, 2018. https://standards.ieee.org/project/1752.html
Thomas, L., and Capistrant, G.: State Telemedicine Gaps Analysis Coverage & Reimbursement, American Telemedicine Association
Liu, F. , Rijnboutt, E., Routsis, D., Venekamp, N., Fulgencio, H., Rezai, M., and van der Helm, A.: What challenges have to be faced when using the cloud for e-health services?. In: IEEE 15th International Conference on e-Health Networking, Applications Services (Healthcom), pp. 465–470, 2013. https://doi.org/10.1109/HealthCom.2013.6720721.
Kraemer, F. A., Braten, A. E., Tamkittikhun, N., and Palma, D., Fog computing in healthcare—a review and discussion. IEEE Access 5:9206–9222, 2017.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mobile & Wireless Health
This research was supported by the Khalifa University-Korea Advanced Institute of Science and Technology Program.
Rights and permissions
About this article
Cite this article
Mardini, M.T., Iraqi, Y. & Agoulmine, N. A Survey of Healthcare Monitoring Systems for Chronically Ill Patients and Elderly. J Med Syst 43, 50 (2019). https://doi.org/10.1007/s10916-019-1165-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-019-1165-0