Abstract
The Psoriasis Area and Severity Index (PASI) is the most accepted method for psoriasis severity scoring. However, a prominent level of subjectivity and a low intra- and inter-rater reproducibility was reported. Therefore, an accurate and reproducible measure of psoriasis severity is needed, especially in the setting of registration studies for systemic anti-psoriatic drugs. Herein we describe a robust, user-friendly, computer-guided technology that allows for automated PASI measurements after total body imaging and digital image analysis. For this purpose, a novel image processing software for PASI calculations was developed, which was combined with a commercially available, automated image capturing system. Our data shows, that the software was able to accurately calculate the proportion of psoriatic skin surface as well as the severity of erythema, induration, and desquamation by anatomic region. In a pilot clinical validation the time-efficient technology showed a high reproducibility and high levels of agreement to results attained by PASI-trained physicians. Therefore, automated computer-guided PASI measurements hold the promise of significantly reducing the physicians’ workload while ensuring a high level of reproducibility and standardization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Plaque type psoriasis is a chronic inflammatory skin disease affecting about 2% of the population in Western industrialized nations [1]. It is clinically characterized by sharply demarcated erythrosquamous plaques that commonly affect the scalp, extensor sides of extremities, and the sacral region [2]. For clinical trials as well as for documenting a medical indication to start systemic anti-psoriatic drugs the psoriasis severity needs to be accurately measured. For psoriasis severity assessments by physicians the Psoriasis Area and Severity Index (PASI) is widely recognized as a reference scoring system [3, 4]. Although PASI is considered a gold standard, it shows a number of limitations. The two main concerns are the high inter- and intra-observer variability and the infrequent use of PASI by dermatologists in clinical routine [5,6,7]. Moreover, as a result of the complex calculations behind the weighting of the main PASI components (i.e. severity of erythema, induration, desquamation, and percentage of affected body surface area) PASI measurements remain challenging even for experienced dermatologists [5,6,7]. The resulting demand for a technology assisting physicians in their efforts to assure reproducible, highly standardized, and objective PASI calculations with a high intra- and inter-rater consistency have prompted the development of some computer-aided image analysis systems [8,9,10]. However, due to several limitations these systems never gained widespread acceptance. Recent advances in computer technology have now paved the way towards an increasing and practically applicable level of automation in specific areas of healthcare, i.e. robotic surgery, or machine learning algorithms for making diagnoses in radiology and dermatology [11,12,13,14]. Automation in these settings is accomplished by devices that, by definition, partially or fully exert functions previously carried out by physicians [12]. In contrast to earlier attempts of computer-aided PASI measurements [8,9,10] the data reported herein investigated a robust, user-friendly, computer-guided technology that allows for automated PASI measurements after whole body imaging and digital image analysis.
Methods
Total body imaging system
For automated total body imaging (TBI) a commercially available, automated image capturing system (FotoFinder bodystudio ATBM®, FotoFinder Systems GmbH, Germany) was used. This system was licensed for the European and US market in 2013 and is mostly used for skin cancer screenings. The device offers a standardized skin surface documentation with a “mole mapping” feature, meaning the automatic detection of pigmented skin lesions and their morphological comparison over successive examinations [15,16,17]. The ATBM® system is mounted on a mobile roller and is composed of a digital reflex camera (Canon EOS 700D, Sigma 30 mm f/1.4 DC HSM lens) connected to a motorized vertical rail (linear drive system motorized by a stepper driver), a monitor (EIZO®, Flex Scan EV2336W, 58 cm), and a desktop Computer (FotoFinder Silent Medical Server: Microsoft® Windows 10 pro, Intel® Core i5 Processor, 8 GB RAM) (Fig. 1). The user has to provide the patient’s height which is used to calculate the individual camera positions for the image capturing process. This information is stored to ensure the exact same positioning at each follow up appointment. The patient needs to assume four poses (Fig. 2) and the system successively captures the i) “frontal coronal plane” with arms down at the sides and dorsum of the hands facing towards the camera, ii) “sagittal plane right” with arms stretched out in a right angle and left foot set forward, iii) “dorsal coronal plane” with arms down at the sides and palms of the hands facing towards the camera, iv) “sagittal plane left” with arms stretched out in a right angle and right foot set forward. For each pose the camera is moved along the vertical motorized rail (proportional distance in correspondence to the body height) to assume four positions for imaging fixed overlapping areas of i) head/neck, and upper trunk, ii) trunk, iii) lower trunk and thighs, and iv) distal lower extremities. Floor markings and a laser liner are used to guarantee a reproducible positioning of the patient (Fig. 3). Dark blue wallpaper provides for a standardized photograph background. The ATBM® software controls camera settings as autofocus, flash, aperture, shutter speed, ISO number, and depth of field to allow for a reproducible image quality regarding brightness and patient skin tone. Integrated polarization filters of the camera flash and lens provide cross polarized images, suppressing glare effects and light reflections of the patient’s skin surface. Of note, a TBI system for automated PASI measurements should at best allow for digital imaging of the whole cutaneous surface. However, limitations arise from skin areas frequently covered by hair (hair-bearing scalp, genital area), flexural sites (anal fold, axillary and inguinal fold), and plantar sites that constitute approximately 10% of the body surface area (BSA). In order to minimize the efforts involved, the listed body sites were excluded from TBI for automated PASI measurements. Instead, operators were offered the opportunity to manually edit the “computerized PASI” to complement for any affected body sites not adequately considered.
FotoFinder bodystudio ATBM system components: 1. Patient positioning floor-mat, 2. Electric stepper driver, 3. Linear drive belt, 4. Camera slide, 5. Flash device, 6. Camera, 7. Energy chain, 8.Linear drive axis, 9. Linear drive belt deflecting device, 10. Monitor, 11. Keyboard and mouse, 12. Compartment, 13. Laser liner positioning device, 14. FotoFinder Silent Medical Server, 15. Separating transformer, 16. Hoop Guard camera protection (Photo courtesy of FotoFinder Systems)
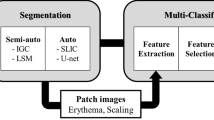
Software requirements for automated PASI measurements
In contrast to the commercially available technology for TBI with its resulting 16 standardized body images the software for the subsequent processing of images for PASI calculations had to be developed anew. The following software requirements for automated PASI measurements were identified:
- 1)
Image alignment of the 16 single digital body images into four full body views from different angles: all overlapping skin surfaces of the 16 single images were detected by a Smart Match algorithm (FotoFinder Systems GmbH, Germany) and excluded from further skin surface calculations to improve the accuracy.
- 2)
Image segmentation for identification of patients’ skin surface:skin surface detection of the patient under investigation was realized by transferring the single digital images from their original red, green, and blue (RGB) color space to an YCbCr color space (Y, luminance; Cb, blue-difference chroma component; Cr, red-difference chroma component). The YCbCr color space was more suitable for subsequent processing, operations, and storage of image data. Next, the Cr content of images was filtered out followed by the identification of the body surface by an Edge-Preserving Thresholding (EPT) algorithm, which was used for segmentation of the prominent edges in the image.
- 3)
Identification of predefined anatomical segments of the overall skin surface as defined by PASI (head/neck, trunk, upper extremities, lower extremities) was achieved by allocating every pixel of the detected skin surface to one of the anatomical segments by Automated Shape Recognition (FotoFinder Systems GmbH, Germany). The Automated Shape Recognition algorithm extracts the body edges of each image and calculates vectors inside these body edges. Vector elements are then scanned for the recognition of patterns of head/neck, trunk, upper extremities, and lower extremities.
- 4)
Image segmentation for identification of psoriatic skin lesions:as described in more detail below color adjustments and software filter methods were applied for determination of the erythema level and the scaliness level was determined by applying proprietary filters and formulas for enhancement of the roughness of skin surfaces. To visualize the segmentation for the user a blue mask was drawn over the psoriasis lesions and a green mask over healthy skin after the psoriasis regions had been identified (Fig. 4). For all calculations the algorithm considered regions covered by hair or clothes as healthy skin.
- 5)
After identification of psoriatic skin in different anatomical body regions a ratio of psoriatic skin to the overall skin surface was calculated. For these calculations the proportional skin surface was measured by the number of pixels.
- 6)
For determination of the erythema level color adjustments and software filter methods were applied. First, the software converted the original images from the RGB color model to CIELAB color space, a color space originally defined by the International Commission on Illumination (CIE) in 1931 [18] and later modified as “CIE 1976 L*a*b* space” (CIELAB, [19]). In a next step the redness of each pixel was calculated as: Redness = DoG(f(L,a,b)) where f is a filter function that maps pixel’s colors by L (lightness of color), a (position between red/magenta and green), b (position between yellow and blue) to an 8 bit value. The red, green and blue scales use 8 bits each, which have integer values from 0 to 255. This makes 256*256*256 = 16.777.216 possible colors. This processing step aimed to produce an image where the level of redness of a pixel is converted into a corresponding level of brightness. As a result of these settings deep red pixels were displayed very bright (Fig. 5). In addition, f was designed to reduce effects on redness caused by variable ambient lighting conditions. The level of redness in areas with psoriatic skin (rednesspsoriasis regions) were compared to the average color characteristics of unaffected normal skin (rednessnormal skin regions) to include the physiological skin tone of the patient and conditions of ambient light into the calculations. The level of redness was calculated as (rednesspsoriasis regions) - (rednessnormal skin regions). The final values for the level of redness were then converted and presented on a 5-point scale as defined by PASI (numerical numbers ranging from 0 to 4). The level of induration was assessed by applying proprietary gradient filter methods as a function of depth of field measurements to the edges of imaged psoriatic skin lesions. The level of scaliness of psoriatic skin was determined by applying proprietary filters and formulas for enhancement of the roughness of skin surfaces. These filters are focused on scattered roughness and fine, small edges on the skin surface. As reported earlier, surface roughness is a measurable feature that is well suited to grade the scaliness of psoriatic skin lesions [20]. To ensure that only relevant desquamation of lesional skin entered the algorithm we additionally considered information regarding the redness and thickness segmentation of perilesional skin. As already outlined above, the level of scaliness was also converted to distinct levels of brightness (Fig. 6). With these measures in place values for scaliness were transferred to a 5-point scale ranging from 0 to 4 according to PASI.
Fig. 4 Fig. 5 - 7)
To calculate the overall PASI score, the scores of each image were combined after anatomical segmentation to create the section scores according to PASI (head/neck (Area 1), upper extremities (Area 2), trunk (Area 3), and lower extremities (Area 4)). Calculations were being performed in four different body areas (head/neck (A1), upper extremities (A2), trunk (A3), lower extremities (A4). First the severity scores (numerical numbers 0–4) of erythema, thickness, and scaling were added up for each of the four anatomical regions (Score Redness + Score Thickness + Score Scaling) resulting in four subtotals (A1-A4). For weighting of the skin surface of each anatomical area subtotals were multiplied with a distinct factor resulting in the weighted subtotals B1-B4 (B1 = A1 × 0.1; B2 = A2 × 0.2; B3 = A3 × 0.3; B4 = A4 × 0.4). Next, weighted subtotals of each body area were multiplied by the score (ranging from 0 to 6) for the affected skin surface resulting in PASI area scores C1-C4 (C1 = B1 x (0 to 6); C2 = B2 x (0 to 6); C3 = B3 x (0 to 6); C4 = B4 x (0 to 6)). Finally, the total PASI is calculated based on the sum of PASI area scores (PASI = C1 + C2 + C3 + C4).
- 8)
Presentation of aligned images with the identified areas of psoriatic skin and computerized PASI results to the operator to allow for manual adjustments.
- 9)
Documentation and storage of finalized medical findings in the form of a PDF-file.
Results
Image alignment
The overlapping skin surfaces of the 16 single images were detected by a Smart Match algorithm which used the “chamfer distance function” (sum of closest point distances) for determining the overlapping body regions (Fig. 7) [21].
Skin surface detections
Digital images were transferred from their RGB to an YCbCr color space and the Cr content was filtered out. Identification of the body surface was done by an EPT algorithm for segmentation of the prominent edges in the image. As a result, all pixels corresponding to the skin surface of the individual patient could be identified.
Anatomical segmentation
By allocation of every pixel of one of the defined body regions of the detected skin surface to one of the anatomical segments by the Automated Shape Recognition algorithm PASI calculations in this setting were based on the distinct anatomical segments instead of individual images.
Identification of psoriatic skin lesions
For the differentiation of psoriatic from healthy skin the software applied different semi-transparent masks to digital images to identify erythematous and scaly psoriasis regions as well as normal skin regions.
Calculation of the percentage of skin affected by psoriasis (body surface area)
The accuracy of psoriatic skin surface calculations by pixel numbers was validated by comparing these results to the truly measured psoriatic skin surface area. To this end the psoriatic skin surface area of 10 patients was first calculated by the software as described above and then measured by expert physicians using the DuBois formula [22] and Wallace “rule of nines” [5]. A mean Intraclass-Correlation-Coefficient (ICC) of 0.84 was observed, indicating a high level of agreement between the different methods. The minor differences in the psoriatic skin surface calculations by the software versus physicians were caused by hidden body surface areas, e.g. by hair-covered scalp, genital area, or soles of the feet. In a final step, the percentage of psoriatic skin in each of the four defined anatomical areas was classified on a 7-point scale (numerical numbers 0–6) according to PASI (0 = no involvement, 1 = 1–9%, 2 = 10–29%, 3 = 30–49%, 4 = 50–69%, 5 = 70–89%, 6 = 90–100%).
Determination of erythema (redness)
The accuracy of erythema calculations was validated by comparing results to physicians’ assessments in 10 patients. A high level of agreement with a mean ICC of 0.74 was determined.
Determination of induration (thickness)
Different severities of plaque thickness could be converted to enhanced levels of brightness around psoriatic skin lesions (Fig. 8). The level of induration was then calculated by the encoded level of brightness by proprietary formulas. In a final step values for induration were translated to the 5-point scale as defined by PASI (numerical numbers ranging from 0 to 4). The agreement between the software and physicians’ determination of induration in 10 patients was high (mean ICC 0.82).
Determination of desquamation (scaliness)
When comparing the results of scaliness measurements between physicians and software in 10 patients a mean ICC of 0.78 was observed.
Calculation of the total PASI
The accuracy of total PASI calculations was validated by comparing computerized PASI scores to physicians’ assessments in 10 patients. A mean ICC of 0.83 was determined, indicating a high level of agreement. Moreover, the reproducibility of computerized PASI measurements was investigated by two successive full assessments in 10 patients yielding an excellent mean ICC of 0.98.
Option for physicians’ adjustments
An output summary of the computerized PASI was designed (Fig. 9). This output summary indicates all anatomical regions with corresponding skin area scores (0–6), severity of erythema (0–4), thickness (0–4), and scaling (0–4). Operators may modify each of the computerized items or approve computerized PASI area scores as measured by the algorithm. After approval by the operator PASI pre-scores become final PASI scores. Of note, a further feature of the designed software allows for the automated comparison of baseline and follow-up images of individual patients in order to calculate possible PASI changes over time.
Discussion
There is a medical and research need for an accurate and reproducible measure of psoriasis severity. Today, PASI is the most accepted method for severity scoring. On the one hand, PASI reduction is used as a primary outcome measure in many pharmaceutical clinical trials to substantiate the efficacy of anti-psoriatic drugs [23]. On the other hand, dermatologists need to document PASI of psoriasis patients to correctly meet the indication of many systemic anti-psoriatic drugs (“moderate to severe psoriasis” translates into a PASI score equal/greater 10). In stark contrast to the widespread acceptance and use of PASI, earlier reports gave evidence of a prominent level of subjectivity and a low intra- and interrater reproducibility [5,6,7]. To overcome these shortcomings of PASI, a few attempts to design computer-aided measurements of psoriatic lesions were reported [8,9,10]. Kreft et al. described a computer-aided strategy for measuring the skin surface affected by psoriasis [8]. However, the low-grade standardization and the requirement to print out patient images and trace the outlines of psoriatic lesions with a marker on overlaid transparency sheets made this approach unusable. The report of Lu et al. investigated features for segmentation of erythema and induration on selected single-lesion images and, therefore, did not supply a practicable solution [9]. In contrast, we describe a first comprehensive strategy for computer-aided PASI measurements by a robust method showing a high reproducibility. The proposed method relies on a commercially available, automated image capturing system providing 16 digital images of the patients’ skin surface. These images form the basis for all subsequent processing and segmentation steps which strictly follow all requirements defined by PASI. The newly created software is able to accurately calculate the proportion of psoriatic skin surface as well as the severity of erythema, thickness, and scaliness by anatomic region. Computerized measurements showed a high level of agreement to results of PASI-trained physicians in a pilot clinical study in 10 patients. Moreover, computerized PASI calculations yielded an unprecedented reproducibility of 99% when performing two successive full examinations including completely new total body images. Time requirements amounted from 7 to 10 min in patients of the pilot study and comprised the patients’ undressing and the process of total body imaging. The results of the subsequent image processing are displayed to the operator as shown in Fig. 9 within less than a minute.
In conclusion, the data presented herein describes the development and performance analysis of a first-in-class technology for computer-guided, automated PASI measurements by means of total body image analyses. The high degree of standardization and reproducibility hold the promise of significantly reducing physicians’ workload and warrant further investigations. To extent our knowledge and further optimize this technology a clinical study in 120 psoriasis patients was initiated.
References
Nast, A., Boehncke, W. H., Mrowietz, U. et al., S3 – Guidelines on the treatment of psoriasis vulgaris (English version). Update. JDDG: Journal der Deutschen Dermatologischen Gesellschaft 10:S1–s95, 2012. https://doi.org/10.1111/j.1610-0387.2012.07919.x.
Mrowietz, U., and Reich, K., Psoriasis—New insights into pathogenesis and treatment. Deutsches Ärzteblatt International. 106(1–2):11–19, 2009. https://doi.org/10.3238/arztebl.2009.0011.
Fredriksson, T., and Pettersson, U., Severe psoriasis – Oral therapy with a new retinoid. Dermatologica 157:238–244, 1978.
Naldi, L., Svensson, A., Zenoni, D., Diepgen, T., Elsner, P., Grob, J. J., Coenraads, P. J., Bouwes Bavinck, J. N., Maccagni, A., Linder, D., Williams, H., and on behalf of the European Dermato-Epidemiology Network (EDEN), Comparators, study duration, outcome measures and sponsorship in therapeutic trials of psoriasis: Update of the EDEN psoriasis survey 2001–2006. British Journal of Dermatology 162:384–389, 2010. https://doi.org/10.1111/j.1365-2133.2009.09515.x.
Ramsay, B., and Lawrence, C. M., Measurement of involved surface area in patients with psoriasis. British Journal of Dermatology 124:565–570, 1991.
Langley, R. G., and Ellis, C. N., Evaluating psoriasis with psoriasis area and severity index, psoriasis global assessment, and lattice system Physician's global assessment. Journal of the American Academy of Dermatology 51(4):563–569, 2004.
Berth-Jones, J., Grotzinger, K., Rainville, C. et al., A study examining inter- and intrarrater reliability of three scales for measuring severity of psoriasis: Psoriasis area and severity index, Physician's global assessment and lattice system Physician's global assessment. Br J Dermatol. 155:707–713, 2006.
Kreft, S., Kreft, M., Resman, A. et al., Computer-aided measurement of psoriatic lesion area in a multicenter clinical trial—Comparison to physician's estimations. In Journal of Dermatological Science 44(1):21–27, ISSN 0923-1811, 2006. https://doi.org/10.1016/j.jdermsci.2006.05.006.
Lu, J., Kazmierczak, E., Manton, J. H., and Sinclair, R., A quantitative technique for assessing the change in severity over time in psoriatic lesions using computer aided image analysis. Conf Proc IEEE Eng Med Biol Soc. 2013:2380–2383, 2013. https://doi.org/10.1109/EMBC.2013.6610017.
Yune, Y. M., Park, S. Y., Oh, H. S., Kim, D. J., Yoo, D. S., Kim, I. H., Moon, J. S., Kim, M. K., and Oh, C. H., Objective assessment of involved surface area in patients with psoriasis. Skin Research and Technology 9:339–342, 2003.
Esteva, A., Kuprel, B., Novoa, R. A. et al., Dermatologist-level classification of skin cancer with deep neural networks. Nature 542:115–118, 2017.
Argenziano, M., Katz, M., Bonatti, J., Srivastava, S., Murphy, D., Poirier, R., Loulmet, D., Siwek, L., Kreaden, U., and Ligon, D., Results of the prospective multicenter trial of robotically assisted totally endoscopic coronary artery bypass grafting. In The Annals of Thoracic Surgery 81(5):1666–1675, ISSN 0003-4975, 2006. https://doi.org/10.1016/j.athoracsur.2005.11.007.
Götz, T. I., Lahmer, G., Strnad, V. et al., A tool to automatically analyze electromagnetic tracking data from high dose rate brachytherapy of breast cancer patients. Mankin R, ed. PLoS ONE 12(9):e0183608, 2017. https://doi.org/10.1371/journal.pone.0183608.
Haenssle, H. A., Fink, C., Schneiderbauer, R., Toberer, F., Buhl, T., Blum, A., Kalloo, A., ABH, H., Thomas, L., Enk, A., Uhlmann, L., and Reader study level-I and level-II Groups, Man against machine: Diagnostic performance of a deep learning convolutional neural network for dermoscopic melanoma recognition in comparison to 58 dermatologists. Ann Oncol. 29(8):1836–1842, 2018. https://doi.org/10.1093/annonc/mdy166.
Salerni, G., Carrera, C., Lovatto, L. et al., Benefits of total body photography and digital dermoscopy (“two-step method of digital follow-up”) in the early diagnosis of melanoma in high-risk patients. Journal of the American Academy of Dermatology. 67(1):e17–e27, 2012. https://doi.org/10.1016/j.jaad.2011.04.008.
Fink, C., and Haenssle, H. A., Non-invasive tools for the diagnosis of cutaneous melanoma. Skin Res Technol 23:261, 2017.
Korotkov, K., Quintana, J., Puig, S., and Malvehy, J., Garcia R. a new total body scanning system for automatic change detection in multiple pigmented skin lesions. IEEE Trans Med Imaging. 34(1):317–338, 2015. https://doi.org/10.1109/TMI.2014.2357715 Epub 2014 Sep 12.
CIE, Commission internationale de l'Eclairage proceedings, 1931. Cambridge: Cambridge University Press; Smith, Thomas; Guild, John (1931–32). “The C.I.E. colorimetric standards and their use”. Transactions of the Optical Society 33(3):73–134, 1932.
McLaren, K., XIII—The development of the CIE 1976 (L* a* b*) uniform colour space and colour-difference formula. Journal of the Society of Dyers and Colourists 92:338–341, 1976.
Hani A (2014) Surface imaging for biomedical applications, CRC Press (Taylor & Francis Group, FL). Version Date: 20140114. ISBN 978-1-54822-1578-6.
Zhang, Q., Xu, P., Li, W., Wu, Z., Zhou, M., Efficient edge matching using improved hierarchical chamfer matching. In: IEEE International Symposium on Circuits and Systems, pp. 1645–1648 2009.
Dubois, D., and Dubois, E. F., A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med. 17:863–871, 1916.
Puzenat, E., Bronsard, V., Prey, S. et al., What are the best outcome measures for assessing plaque psoriasis severity? A systematic review of the literature. Journal of the European Academy of Dermatology and Venereology 24:10–16, 2010. https://doi.org/10.1111/j.1468-3083.2009.03562.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T.F. is an employee of FotoFinder Systems GmbH.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. A separate ethical approval was not required for this study.
Additional information
This article is part of the Topical Collection on Image & Signal Processing
Rights and permissions
About this article
Cite this article
Fink, C., Fuchs, T., Enk, A. et al. Design of an Algorithm for Automated, Computer-Guided PASI Measurements by Digital Image Analysis. J Med Syst 42, 248 (2018). https://doi.org/10.1007/s10916-018-1110-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-018-1110-7