Abstract
This study examined factors associated with psychological distress for culturally diverse family caregivers using a population-based sample. Data were analyzed from the 6634 caregivers of adults (i.e. elderly as well as non-elderly) who self-reported as non-Hispanic White, Mexican, Chinese, or Vietnamese in the 2009 California Health Interview Survey. Simple and multiple regression analyses were conducted to assess the potential influence of race/ethnicity, caregiving context, and social contextual variables on psychological distress. Analyses that included moderators showed that while more education was associated with less distress for White caregivers, it was associated with more distress for Vietnamese and Chinese caregivers. Identifying the caregiving and contextual variables associated with psychological distress is critical for tailoring interventions towards those who need the most help—in this case, possibly less educated White caregivers and more educated Asian American caregivers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Older racial/ethnic minorities (henceforth referred to as minorities) are one of the fastest growing segments of the population [1]. Among older adults, disparities vary significantly among and within various ethnic groups. Compared to Whites, some minorities have a higher prevalence of functional limitations [2], and Alzheimer’s disease [3, 4]. Consequently, the number of minorities engaged in caregiving for an older adult with impairment is also increasing rapidly [5]. Caregiving is often accompanied by challenges that place caregivers at risk for significant health problems [6, 7]. Caregivers are less likely to engage in preventive health behaviors [6]. They show evidence of decrements in immunity measures [8], greater cardiovascular reactivity, and slower wound healing [9]. Caring for an adult with a disability contributes to psychiatric morbidity in the form of higher prevalence and incidence of depressive and anxiety disorders [6, 10]. Hence, caregiving has become a public health issue and will become increasingly prominent with the aging baby boomers and ethnic diversity of the older adult population [11, 12].
Ethnic Disparities in Caregiving
It has been estimated that about 18% of the Asian American (AA) population provides care to a family member, compared to a slightly lower percentage of Latinos (16%) and to the national average (16.6%) [13]. A meta-analysis found significant ethnic differences among family caregiver populations [14]. Minority caregivers provided care for more hours per week and reported more caregiving tasks compared to White caregivers. Latino and AA caregivers also reported higher rates of depression [14, 15]. This may be because compared to Whites, both Latino and AA caregivers relied more heavily on informal support (e.g., friends, family) than on formal support (e.g., adult day centers). Relying less on formal support services may prevent caregivers from accessing needed services and lead to worse caregiver health [14]. Thus, there are clear ethnic differences in the caregiving context and potential outcomes that are important to study.
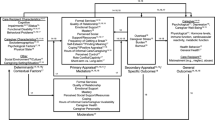
The stress-process model outlined by Pearlin et al. [16] provides a valuable framework for identifying individual differences in caregiving variables. Additionally, the revised sociocultural stress and coping model [17, 18] suggests that race/ethnicity is important in the examination of caregiver stress and provides a context for caregiving [19]. Dilworth-Anderson and Anderson combine concepts from stress and coping as well as ecological-contextual theories to suggest that ethnic differences in caregiving variables and possible resources (e.g., income, education) play a role in caregiving stressors and outcomes.
Moderators of Ethnic Differences in Psychological Distress
Although much research has examined predictors, or main effects, of psychological distress for caregivers, as well as how certain caregiving variables (e.g., social support) can protect against psychological distress [20,21,22], less is known about how the social, non-caregiving-related context of caregivers might buffer against psychological distress. Non-caregiving context variables are ones that are not specific to caregivers or the caregiving situation, but that can affect caregiver stress.
Knowledge on moderator effects of caregiver resources is valuable for understanding ethnic disparities in caregiving as well as the caregiving stress process itself. Moderators indicate which caregivers are at greater risk for distress under similar caregiving situations and which caregivers might be at decreased risk of distress, which may guide prevention and intervention efforts. Previous research as well as sociocultural stress and coping models delineate potentially important resources for minority caregivers outside the caregiving context that may protect against caregiver distress. These include education level, income, and community/neighborhood safety. Akin to the stress-buffering hypothesis [23], we propose that there are ethnic differences in psychological distress as well as caregiving context variables, and that ethnic differences in psychological distress may be moderated by non-caregiving context, or resource variables.
Education and Income
Although education among Latinos has improved over the years, Latinos continue to lag behind other groups [24]. Lower education coupled with caregiving responsibilities may lead to even greater psychological distress for Latino caregivers. In comparison, AAs as a whole have high education, but they are not a homogeneous group. For example, although Chinese and Vietnamese Americans share certain cultural values and characteristics, the circumstances of their arrival to America and subsequent adaptation led to unique experiences in the U.S. Most Chinese came to the U.S. as traditional immigrants or economic migrants; however, most Vietnamese arrived as political refugees. Vietnamese refugees lacked the usual financial resources and social networks that many Chinese immigrants had. They suffered much trauma during their escape, and their harsh experiences make them vulnerable to psychological problems [25]. Compared with Chinese Americans, Vietnamese Americans have lower English language proficiency, education levels, and median household incomes that may exacerbate psychological distress.
Caregivers who are economically and socially disadvantaged are significantly more likely to have mental health problems that are not treated timely and effectively. Continuous financial stress has a negative effect on the psychological well-being of older adults [26]. Thus, minority status coupled with lower income may lead to even greater psychological distress for caregivers.
Neighborhood Safety
Neighborhood safety may also be important in the psychological distress of family caregivers. Using the 2008 Arizona Health Survey, researchers found a positive relationship between experiencing less psychological distress and feeling safe in the neighborhood [27]. People’s perceptions of neighborhood safety affect their coping resources [28,29,30,31,32], and this may further intensify psychological distress for minority caregivers.
The Present Study
Despite the potential growth of the caregiver population, little is known regarding how Latinos and AAs, the largest and fastest growing ethnic groups in the U.S., respectively [33, 34], respond to challenges associated with the caregiving experience. Research in the U.S. that focuses on AAs tends to aggregate Asian subgroups even though these groups differ substantially (as described above). Furthermore, we know of only one other study that has examined how factors outside the caregiving context might buffer against or make caregivers more vulnerable to distress [35]; however, that study did not include AAs. The purpose of the present study was to examine ethnic group differences in psychological distress among diverse family caregivers, and to investigate how factors outside the caregiving context (education, income, and neighborhood safety) might protect against or aggravate psychological distress.
Methods
Sample and Data Collection
The 2009 California Health Interview Survey (CHIS) data were used in this study [36]. The CHIS data collection cycle has been conducted every other year since 2001 and is one of the largest population-based telephone health surveys in the nation. The survey employs a multistage sampling design, using a random-digit-dial sample of landline and cellular telephone numbers from 44 geographic sampling strata to randomly select households. Surveys were conducted in English, Spanish, Mandarin, Cantonese, Vietnamese, and Korean.
In 2009, CHIS surveyed 47,614 adults that were representative of California’s non-institutionalized population. The response rate in 2009 was 36.1%. From the full sample, we limited our study sample to include only those who reported both (a) that they had taken care of a family member (not a child) in the previous year, and (b) their own ethnicity as White, Mexican, Chinese, or Vietnamese; this brought our sample to N = 6634. IRB review was not needed due to CHIS’ availability as a public dataset.
Measures
Psychological Distress
Psychological distress was measured using the Kessler-6 (K6) scale, which measures severity of psychological distress and was designed to estimate the proportion of serious mental illness using survey data [37]. Participants were asked to recall the worst month in the past year when they had experienced serious psychological distress and were asked to report, during that time, how often they felt nervous, hopeless, restless, depressed, worthless, or that everything was an effort. Values ranged from 0 to 24, with higher values representing more distress [37,38,39].
Race/Ethnicity
Ethnicity was based on the UCLA Center for Health Policy Research Office of Management and Budget (OMB) standard. For the purposes of our study, we included only caregivers who self-identified as White (n = 5672), Mexican (n = 700), Chinese (n = 97), and Vietnamese (n = 165).
Caregiving Context Variables
Co-residence with the care recipient and use of respite care were dichotomous variables (0 = no, 1 = yes). The support variable was created from two separate CHIS variables: caregivers were asked if there was someone else who could help them if they were unable to do it; those who said yes were noted as having informal support on the support variable. Caregivers were asked if they had paid for caregivers to come; those who said yes were noted as having formal support. Those who said no to both items received a 0 on the support variable, indicating no support. Relationship to the care recipient was coded as: 0 = spouse/partner, 1 = parent/parent-in-law, and 2 = other (sibling, grandparent, other relative). Length of time caregiving was measured in years and was modified so that all values above 10 years were recoded as 11.
Non-caregiving Context Variables/Resources
Income was computed by dividing total annual household income (in dollars) by the number of adults residing in the household. Income was treated as a continuous variable in the main effects model, and dichotomized into the top and bottom half of income, with lower income as the reference category, in the interaction model. Education was a treated as a dichotomous variable (less than high school versus high school diploma or higher). Neighborhood safety fears were assessed with the question, “How often do you feel safe in your neighborhood (1 = All of the time to 4 = None of the time)? Responses were reversed coded so that higher values represented more neighborhood safety. Neighborhood safety was treated as a continuous variable in the main effects model, and dichotomized into the top and bottom half of neighborhood safety, with lower neighborhood safety as the reference category, in the interaction model.
Covariates
To facilitate interpretation of regression coefficients, caregiver age was centered at 50 in the regression analysis. Participants also self-reported their gender (male versus female) and health status (on a scale from 1—Poor to 5—Excellent). Marital status was dichotomized (married/cohabiting versus single, widowed, divorced, or separated). Individuals with missing data on any of the abovementioned variables were excluded from the study.
Analysis
Weighted chi square tests and linear regression analyses were conducted to examine ethnic group differences in psychological distress, demographics, caregiving context, and resource variables. Two regression models were conducted: Model 1 was the main effects model and did not include interactions; Model 2 included indicator variables for ethnicity and ethnicity by resource variable interaction terms (ethnicity by income, ethnicity by education, and ethnicity by neighborhood safety) to assess the differential impact of potential buffers across different ethnic groups, adjusting for caregiving context and demographic variables. Survey data analysis procedures in STATA were implemented to account for the complex sampling design of the CHIS.
Results
Ethnic Group Differences on Main Study Variables
Table 1 presents the characteristics of the 6634 caregivers in the study by ethnicity. On average, White caregivers were the oldest with Latino caregivers being the youngest. White caregivers had higher incomes and were the most educated. Vietnamese caregivers had the highest percentage of individuals who were married. Chinese and Mexican caregivers were more likely to live with their care recipient than Vietnamese, followed by White caregivers. White caregivers had the highest percentage of individuals who reported not having ever paid for support (formal support) or having someone to help if needed (informal support). AA caregivers reported taking care of their person longer than White and Mexican caregivers. White caregivers also reported the greatest perceptions of neighborhood safety. Vietnamese caregivers reported the most psychological distress and the poorest self-rated health.
Predictors of Psychological Distress in Caregivers
Table 2 presents the results of the regression analysis. Compared to Whites, both Mexican and Chinese caregivers reported significantly less psychological distress. Caregivers with informal support were less distressed than those without informal support. Caregivers taking care of a parent were less distressed than those taking care of a spouse or partner. Those with more education were less distressed than those with less education. Caregivers who reported greater neighborhood safety were less distressed, as were men, individuals who were married, older caregivers, and those with better self-rated health.
Table 3 shows results of the analysis that included moderators. All main effects that were significant in the previous model were also significant in this adjusted model. One major difference was the main effect of ethnicity: compared to Whites, Mexican, Chinese, as well as Vietnamese caregivers reported less psychological distress. However, this was qualified by some significant ethnicity by resource variable interactions. The potential moderating effect of education, income, and neighborhood safety were all tested, but the joint test of interaction effects was significant for only education F (3, 78) = 4.03, p < .05. There was a main effect of education for Whites—those with more education had significantly less distress. However, the education effect differed from Whites for Chinese (B = 3.83 [CI 1.14, 6.53], p < .01) and Vietnamese (B = 7.41 [CI 1.87, 12.95], p < .01). Among Chinese and Vietnamese caregivers, those who were more educated reported more distress than their counterparts with less education (Fig. 1). The interaction effect was not significant for income, F (3, 78) = 0.95, p = .42) or neighborhood safety, F (3, 78) = 2.41, p = .07.
Discussion
This study examined ethnic differences in psychological distress for caregivers as well as whether certain non-caregiving context resources might protect against distress. Although there were ethnic differences in psychological distress in our main effects model, these were qualified by a significant ethnicity by education interaction. Mexican caregivers had lower psychological distress than Whites across education levels, but this wasn’t the case for AA caregivers. That is, education seemed to have a protective effect against psychological distress for White caregivers, but for AA caregivers, education was associated with more distress. Although this finding seems counterintuitive, there are some potential explanations. First, it may be that more educated AA caregivers were just more willing to report psychological distress compared to their less educated counterparts. There is some research indicating that more acculturated (and thus possibly more educated) AAs have more insight into their psychological state and are more likely to self-disclose their emotional problems [40, 41]. Response styles and reporting of psychological distress can vary because of issues related to interviewer effects, acquiescence, social desirability, and cultural differences in expressing psychological distress [42]. Biases may also occur when education level is taken into account, further complicating studies that attempt to tease apart methodological biases from actual distress levels. Future research using different methodologies (e.g., self- and informant-report as well as observation) and longitudinal design should attempt to replicate findings from this study. Another potential explanation is that because education is highly valued in Chinese and Vietnamese cultures and seen as the strategy for success [43], it does not confer any added value in the sense of protecting against psychological distress. It may lead to more distress because of the pressures of professional success in addition to the familial expectations and responsibility of caregiving for AAs. However, in exploratory analyses (not shown), we did not find a significant correlation between number of hours worked and psychological distress for AA caregivers.
Using data from the National Latino and Asian American Study, Zhang and Hong [44] found that although education was not directly associated with psychological distress for AAs, it modified the effect of perceived discrimination on psychological distress, so that the effect of perceived discrimination on distress was higher for those who were more educated. The authors suggested that better educated AAs were more likely to be employed and have more social contacts with American society, which in turn, increased their chances of encountering negative interactions and discriminatory behaviors. Thus, education may be associated with other experiences (e.g., discrimination, social barriers) that make AAs, regardless of caregiving status, more vulnerable to distress in general.
Consistent with theories of social capital [45] and other studies examining neighborhood effects, more neighborhood safety was associated with less psychological distress [27, 46]. This effect did not differ by caregiver ethnicity, indicating that for all caregivers, neighborhood safety was important in protecting against psychological distress. This may be because neighborhood safety, which is related to social support and cohesion, may provide an additional source of help important in caregivers’ coping mechanisms.
The findings should be considered within the limitations of the study. First, it was unclear why caregivers were taking care of their family member and the age of the family member was unknown. Dementia caregiving is the most frequently studied type of caregiving represented in the literature and much of what was discussed in the current study; however, the CHIS does not collect data on care recipient age or type of illness. Type of care recipient illness is an important main effect as well as moderator of psychological distress [47]. Second, our data are cross-sectional and, therefore, we cannot infer causality among our variables or assume that education reduces the risk of psychological distress for Whites and increases the risk of distress for AAs, for example. Additionally, some of the cell sizes are small; however, this was because we were able to examine sub-group differences, and very few studies dis-aggregate Asian ethnic groups. Finally, findings are based on individuals from one state, and although it is demographically diverse, it is unclear how these results generalize to other individuals and settings.
New Contribution to the Literature
While important studies have contributed to our understanding of the main and mediating effects of race/ethnicity and other caregiving context variables, we have few sophisticated models that test how the effects of race/ethnicity on mental health outcomes might depend on the extent of resources available [48, 49]. Unlike many previous studies of caregivers, this sample was drawn from a relatively large population-based sample, making it more representative of the general population of culturally diverse caregivers. Additionally, the current study adds to the growing literature on caregiving and distress in ethnic minorities by examining how non-caregiving context variables might contribute to and/or buffer against psychological distress. For example, while neighborhood safety exerts effects on distress equally for all caregivers, education level does not. This is crucial to know given the growing ethnic diversity of the caregiving population.
Results of this study have implications for interventions and policy that capitalize on the strengths of diverse caregivers and could target those that might be more vulnerable to distress. Protocols for identifying caregivers at risk in primary care and other settings should be developed and tested. For example, family physicians might want to collect some background information on caregivers, such as their education level and perceptions of their neighborhood safety. Additionally, services for older adults should address the information and support needs of vulnerable caregivers. Timely and targeted interventions, tailored to the specific needs of caregivers, could improve quality of life and well-being of caregivers and their care recipients [50]. Future research should explore possible reasons for why education does not seem protective against psychological distress for AA caregivers the way it is for White, and to a lesser extent, Latino caregivers.
References
U.S. Department of Health and Human Services. A profile of older Americans. 2012.
Sinclair L, Gomez O. Ethnic and racial populations with disabilities: a public health bibilography. Atlanta, GA; 2006.
Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51(2):169–77.
Tang MX, Stern Y, Marder K, Bell K, Gurland B, Lantigua R, et al. The APOE-epsilon4 allele and the risk of Alzheimer disease among African Americans, whites, and Hispanics. J Am Med Assoc. 1998;279(10):751–5.
Fact Sheet: Selected Caregiver Statistics: Family Caregiver Alliance; 2012.
Schulz R, Newsom J, Mittelmark M, Burton L, Hirsch C, Jackson S. Health effects of caregiving: the caregiver health effects study: an ancillary study of the Cardiovascular Health Study. Ann Behav Med. 1997;19(2):110–6.
Yaffe K, Fox P, Newcomer R, Sands L, Lindquist K, Dane K, et al. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA. 2002;287(16):2090–7.
Kiecolt-Glaser JK, Dura JR, Speicher CE, Trask OJ, Glaser R. Spousal caregivers of dementia victims: longitudinal changes in immunity and health. Psychosom Med. 1991;53(4):345–62.
Kiecolt-Glaser JK, Marucha PT, Malarkey WB, Mercado AM, Glaser R. Slowing of wound healing by psychological stress. Lancet. 1995;346(8984):1194–6.
Teri L, Logsdon RG, Uomoto J, McCurry SM. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52(4):159–66.
Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12(3):240–9.
Talley RC, Crews JE. Framing the public health of caregiving. Am J Public Health. 2007;97(2):224–8.
Caregiving in the U.S. 2009. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf].
Pinquart M, Sorensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist. 2005;45(1):90–106.
Haley WE, Gitlin LN, Wisniewski SR, Mahoney DF, Coon DW, Winter L, et al. Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: findings from the REACH study. Aging Ment Health. 2004;8(4):316–29.
Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process—an overview of concepts and their measures. Gerontologist. 1990;30(5):583–94.
Aranda MP, Knight BG. The influence of ethnicity and culture on the caregiver stress and coping process: a sociocultural review and analysis. Gerontologist. 1997;37(3):342–54.
Knight BG, Sayegh P. Cultural values and caregiving: the updated sociocultural stress and coping model. J Gerontol B Psychol Sci Soc Sci. 2010;65B(1):5–13.
Dilworth-Anderson P, Anderson N. Dementia caregiving in Blacks: a contextual approach to research. In: Light E, Niederehe G, Lebowitz BD, editors. Stress effects on family Alzheimer’s patient. New York: Springer; 1994.
Chong AM, Kwan CW, Chi I, Lou VW, Leung AY. Domestic helpers as moderators of spousal caregiver distress. J Gerontol B Psychol Sci Soc Sci. 2014;69(6):966–72.
Pot AM, Deeg DJ, van Dyck R. Psychological distress of caregivers: moderator effects of caregiver resources? Patient Educ Couns. 2000;41(2):235–40.
Rabinowitz YG, Mausbach BT, Gallagher-Thompson D. Self-efficacy as a moderator of the relationship between care recipient memory and behavioral problems and caregiver depression in female dementia caregivers. Alzheimer Dis Assoc Disord. 2009;23(4):389–94.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57.
Motel S, Patten E. The 10 Largest Hispanic Origin Groups: characteristics, rankings, top counties. Pew research 2012. http://www.pewhispanic.org/2012/06/27/the-10-largest-hispanic-origin-groups-characteristics-rankings-top-counties/.
Tran TV, Phan PT. The changing Vietnamese American family. In: Wright RH Jr, Mindel CH, Tran TV, Habenstein RW, editors. Ethnic variations in America: patterns and variations. 5th ed. New York: Pearson; 2012.
Krause N. Chronic financial strain, social support, and depressive symptoms among older adults. Psychol Aging. 1987;2(2):185–92.
Booth J, Ayers SL, Marsiglia FF. Perceived neighborhood safety and psychological distress: exploring protective factors. J Sociol Soc Welf. 2012;39(4):137–56.
Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37(4):293–310.
Ellaway A, Macintyre S, Kearns A. Perceptions of place and health in socially contrasting neighbourhoods. Urban Stud. 2001;39:2299–316.
Ahern J, Galea S. Collective efficacy and major depression in urban neighborhoods. Am J Epidemiol. 2011;173(12):1453–62.
Faris RE, Dunham HW. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. Chicago: The University of Chicago Press; 1939.
Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–76.
Pew Research Center. The rise of Asian Americans. Washington, DC: Pew Research Center; 2012.
U.S. Census Bureau. Statistical Abstract of the United States: 2011, Table 11. Resident population projections by race, Hispanic-origin status, and age: 2010 and 2015. 2011. http://www.census.gov/prod/2011pubs/11statab/pop.pdf].
Rote S, Angel JL, Markides K. Health of elderly Mexican American adults and family caregiver distress. Research on Aging. 2015;37(3):306–31.
California Health Interview Survey (CHIS) Los Angeles, CA: UCLA Center for Health Policy Research. 2009.
Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76.
Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2003;33(2):357–62.
Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22.
Gim RH, Atikinson DR, Whiteley S. Asian American acculturation, severity of concerns, and willingness to see a counselor. J Couns Psychol. 1990;37:281–5.
Liem R, Lim BA, Liem JH. Acculturation and emotion among Asian Americans. Cult Divers Ethnic Minor Psychol. 2000;6:13–31.
Dohrenwend BP, Dohrenwend BS. Social status and psychological disorder: a causal inquiry. New York: Wiley-Interscience; 1966.
Kramer E, Kwong K, Lee E, Chung H. Cultural factors influencing the mental health of Asian Americans. West J Med. 2002;176:227–31.
Zhang W, Hong S. Perceived discrimination and psychological distress among Asian Americans: does education matter? J Immigr Minor Health. 2012;15:932–43.
Lin N. Social capital: a theory of social structure and action. New York: Cambridge University Press; 2002.
Nguyen D, Goel M. Social determinants and the psychological distress of Vietnamese immigrants. Int J Cult Ment Health. 2014;8(1):22–33.
Pinquart M, Sorensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2003;58(2):112–28.
Hilgeman MM, Durkin DW, Sun F, DeCoster J, Allen RS, Gallagher-Thompson D, et al. Testing a theoretical model of the stress process in Alzheimer’s caregivers with race as a moderator. Gerontologist. 2009;49(2):248–61.
Napoles AM, Chadiha L, Eversley R, Moreno-John G. Reviews: developing culturally sensitive dementia caregiver interventions: are we there yet? Am J Alzheimers Dis Other Demen. 2010;25(5):389–406.
Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, et al. Training carers of stroke patients: randomised controlled trial. BMJ. 2004;328(7448):1099.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Review by and approval from the appropriate institutional and/or national ethical review committee was not needed in this study because CHIS is a publicly available dataset (http://healthpolicy.ucla.edu/chis/data/Pages/public-use-data.aspx).
Rights and permissions
About this article
Cite this article
Meyer, O.L., Liu, X., Nguyen, TN. et al. Psychological Distress of Ethnically Diverse Adult Caregivers in the California Health Interview Survey. J Immigrant Minority Health 20, 784–791 (2018). https://doi.org/10.1007/s10903-017-0634-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-017-0634-0