Here, I am a refugee. But I don’t want refuge. I want the wings to fly.
Devi, Bhutanese refugee child.
Abstract
Bhutanese refugees resettling in the U.S. face many challenges including several related to health and health care. Limited health literacy and the relatively complicated US health care system may contribute to health disparities as well. A health assessment was conducted on adult refugees in Houston, Texas to provide healthcare providers, community organizations, and stakeholders baseline data to plan programs and interventions. A convenience sample of 100 participants had a mean age of 38.37 years, 56 % where males, and almost 80 % did not have high school level education. High blood pressure (27 %), dizziness (27 %), and arthritis (22 %) were the commonly identified chronic health conditions and trouble concentrating (34 %) and fatigue (37 %) were also reported. Sixty-two percent of the respondents reported that they consume recommended servings of fruits and vegetables and 41 %reported that they were currently getting at least 20–30 min of aerobic exercise per day. The assessment concluded with recommendations on how better provide care and services for the refugees.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bhutanese refugees who have lived in refugee camps in Nepal for many decades, have been resettling into life in the US, having recently migrated as refugees. Since 1990, over 100,000 Bhutanese of Nepali ethnic origin fled to Nepal due to coercion and fear of ethnic persecution in their home country [1–3]. However, even in UN refugee camps in Nepal, they struggled to meet their basic needs of employment, education, and health [4–8]. In 2007, the US agreed to accept at least 60,000 Bhutanese refugees and provide basic needs including housing, food stamps, health insurance, English coaching, and employment search assistance [4, 5, 9, 10]. Between calendar year 2008 through calendar year 2012 the State of Texas saw 5315 Bhutanese refugees arrive and 1534, or 29 % came to Houston, Texas’ largest city [11]. See Table 1.
In the absence of necessary knowledge and skills of daily living in the US, the now twice re-settled refugees are disproportionately disadvantaged on many fronts. Limited health literacy, knowledge of the healthcare system and the complicated application process to obtain access health care in the US, make them particularly vulnerable. Additionally, structural barriers related to language, transportation and lack of financial means to pay for health services compound the inability to access healthcare among refugees and new immigrants [13]. As a result, several forms of physical, mental and psychosocial health disparities exist among newly arrived refugees and immigrants [14].
Limited literature exists in the area of surveillance of infectious diseases among refugees and immigrants as part of the refugees’ arrival process [15]. One study focused on non-infectious diseases among Bhutanese refugees in a clinical setting [15]. Only a few studies have examined the chronic conditions among immigrants and recently settled refugees [16], mental health conditions [14], cancer screening [17], little literature exists that examines depressive symptoms, and, health-related behaviors among recently re-settled Bhutanese refugee population. Behavioral risk factors such as lack of physical activity and poor nutrition, which play a role in prevention of several chronic conditions, are issues of concern among the recent refugee population in the US. Literature does exists on immigrant populations that states their health status reflects that from their nation of origin rather than that of the general population when they arrive to the US; however, their overall health condition trends towards that of the US general population over time residing in the US [18, 19]. The Bhutanese refugees may or may not manifest this pattern owing to the deprivation experienced in the dismal conditions in the refugee camps. Lack of nutritious food in the refugee camps abroad has, in some groups, potentially led to deficiency of essential vitamins (e.g. B12) among Bhutanese refugees [20].
There is limited information about the dietary behaviors of the refugees and in particular, of the Bhutanese refugees in the US. An observational study with a very small sample size noted that most of the Bhutanese refugees still follow the dietary practices that they were practicing when they lived in the refugee camps of Nepal. The only difference noted was in terms of the need of using vehicles to get to the grocery shop here in the US as opposed to purchasing groceries in the nearby (walking distance) shops in Nepal [12]. Another qualitative study examined the knowledge, practices, and barriers related to healthy eating among refugees in the US. The study noted that three key factors (individual, structural, and societal/cultural) influence the dietary practices among refugees [21]. Findings of another study conducted among Bhutanese women, supports the finding that contextual factors may influence the dietary practices [22]. Bhatta et al. [22] al noted that meat consumption among Bhutanese women was significantly associated with excess body weight.
The adoption of an increasingly sedentary lifestyle and unhealthy dietary practices among new Bhutanese refugees escalates the risk of development of chronic health conditions. It is important to firstly, understand the practices related to dietary and physical activity behaviors, and secondly, to monitor chronic physical conditions and mental health issues among refugees over time. Thus, this study, a community-based needs assessment, aims to establish the baseline indicators for chronic conditions, mental health issues, physical activity and dietary practices among Bhutanese refugees living in Houston TX, a large urban metropolis in southern US.
Methods
We conducted a health assessment of adult (18 years or older) Bhutanese refugees resettled in Houston area. Before data collection commenced, institutional review board approval was obtained from Baylor College of Medicine. Six university students fluent in reading and writing Nepali were trained in survey data collection. Most Bhutanese refugees spoke Nepali since they had spent many years in refugee camps in Nepal. This was followed by outreaching and partnering with the refugee resettlement agencies, and two service agencies (Bhutanese American Association of Houston and Bhutanese Community of Houston), both led by Bhutanese individuals in the Houston area. With feedback from the partners, two apartment complexes where a large proportion of Bhutanese refugees were living were identified. According to resettlement agencies, the selected complexes represented more than eighty percent of the Bhutanese refugees resettled in Houston area. Managers of the identified apartment complexes were contacted and invited to participate in the study. Permission to contact the residents of the complex was obtained from the respective managers. At least two Bhutanese refugees previously identified from each complex as peer leaders were key in identifying the residences of Bhutanese refugees within the complexes. The peer leaders listed the Bhutanese householder’s last name and apartment number, which totaled to be 375 from both apartments.
The study participants were recruited using two approaches. First, we communicated about the survey through local agencies during the ‘English as a Second Language’ classes and conducted the recruitment and interviews with those who were available during those classes. Second, those interviewed identified the Bhutanese households within the apartment complex and went to knock at the doors at different times of day and on different days to access the most diverse sample. During all interviews, at least one of the peer leaders was present in the room where the interviews were conducted. A consent was received from all respondents. All respondents received a gift card of $10 redeemable at local grocery store. A resource package, which included contact numbers for culturally competent health care service providers in the Houston area, was given to all respondents. Interviews were conducted between December 15, 2011 and March 30, 2012.
A 60-item questionnaire was used for our study. The survey instrument was translated into the Nepali language and reviewed and validated by the study coordinator. The demographics, physical activity and nutrition modules of the survey are presented in this paper. The youngest adults (18+) of the households available during the survey were asked to respond to the survey as much as possible in those situations whenever the interviews were conducted at participant’s residence.
Measures
Basic socio-demographics information of the participants collected include: age (number of years), sex (male/female), country of birth (Nepal/Bhutan), number of years in USA, language spoken at home, household income (Less than $10,000 to more than $75,000/year, in an increment of $10,000), marital status (Married, Single, Widowed, Separated, Divorced, Unmarried couple), employment status (Employed for wages, Self-employed, Out of work >1 year, Out of work <1 year, Homemaker, Student, Retired, Seasonal Worker), and educational attainment (Less than high school, high school graduate, some college, college graduate). In addition, there were three questions related to insurance status. First, ‘Do you have health insurance coverage?’ with Yes/No response option. Second question is only applied to those who respond saying ‘Yes’ to first question and it asks to identify the type of insurance. The third question was geared towards capturing the continued insurance coverage for the last 12 months. The questions to capture demographic information were used from Behavioral Risk Factor Surveillance System (BRFSS) (2013) [23] questionnaire except for country of birth, number of years in USA and language spoken at home, which were borrowed from Census, 2010.
Information about chronic health conditions were assessed using one-item from the questionnaire: “has a doctor, nurse or other health professions ever told you that you had any of the following health conditions/problems?”, with 16 response options including others to identify the condition that was not in the list. Examples of included response options were heart disease, arthritis, high cholesterol, high blood pressure. If the participant was never tested or never told about the given health condition, the response was “No”.
Nutrition and physical activity behaviors related questions included: nutrition related (4 items) and physical activity related (2-items). Examples of questions asked include: ‘are you currently getting exercise at least 20–30 min of aerobic exercise per day?’, ‘do you eat 2 servings of fruits per day?’ do you eat 3 servings of vegetables per day?’ ‘Do you monitor or weight on a regular basis?’ All six items had yes/no response option. These questions were used from BRFSS (2010) questionnaire [24]. The reliability and validity of BRFSS questions have be examined and established that most of the questions are of high reliability and high validity [25].
Data Analysis
Descriptive analysis was conducted to describe the participants’ characteristics, physical activity and nutrition-related behaviors.
Results
Participant Characteristics
Table 2 presents the participant characteristics. One hundred participants agreed to participate in the study thus were recruited and interviewed. Twenty individuals declined to participate in the study because they were each heading out of the home at the time they were approached and did not have time to complete the survey. Mean age of the participants was 38.37 years, 56 % males, 44 % were female. Mean number of years in USA was 2.54. Majority (76 %) were married, 7 % were widowed and 14 % were never married. Majority participants (96 %) were born in Bhutan whereas remaining 4 % were born in Nepal. All reported Nepali as the language of choice. Almost 80 % did not have high school level education with 43 % never attended school, 6 % with high school graduation. Only 4 % had college experience. One third had an annual household income less than $15,000. Only 2 % made more than $50,000. Average number of children per household was 3.34. Only 41 % were reported having a job during the assessment period, others were either students or housewives/househusbands or unable to work. Sixty-one percent had some type of health care coverage, majority having the “Gold card” (a county indigent care program) that allowed them to use county health resources. Only two respondents had insurance from their workplace.
Chronic Health Conditions
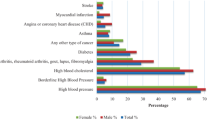
High blood pressure (27 %), dizziness (27 %), and arthritis (22 %) were the commonly identified chronic health conditions among the Bhutanese refugees. More than two-fifth (41 %) respondents reported that they are suffering from other diseases, which were not listed in the response option. The other common health problems include tuberculosis, ulcers, problems related to eyes, allergies, gynecological problems etc. It is important to mention here that most of the study participants had multiple chronic health conditions. Table 3 presents the prevalence of chronic health conditions among study participants. Although mental health services and problems were beyond the scope of this assessment, we did ask the different forms of depression the refugees experienced while living in the United States. Trouble concentrating and fatigue were found common among Bhutanese refugee (34 and 37 % respectively). Hopelessness, sleep disorder, failure, physical and speaking difficulties were also reported, which ranges between 13 and 25 %. See Fig. 1.
Physical Activity and Nutrition Related Behaviors
Sixty-two percent of the respondents reported that they consume recommended servings of fruits and vegetables. Twenty percent of the participants reported consuming soda on a daily basis, majority consumed fried foods, 60 % of the respondents did not monitor their weight on a regular basis. Only 41 % reported that they were currently getting at least 20–30 min of aerobic exercise per day. Table 4 presents the physical activity and nutrition related behaviors of the participants.
Discussion
Our results indicate that the Bhutanese refugee study participants are vulnerable on many fronts. The respondents were refugees coming from refugee camps where they lived most, if not all their lives. They had never experienced life as civilians in Nepal and were ill-equipped to manage the challenges of day to day life. All had been in the US for less than 3 years.
The most common self-reported health conditions were: abnormal blood pressure (27 %), dizziness (27 %), arthritis (22 %), and foot problems (14 %). Notable health behaviors were low rates of smoking (10 % current smokers) and alcohol consumption (4 % drinking more than few times a week), but these were both likely underreported due to social and cultural taboos. In terms of mental health, trouble concentrating and fatigue were found common (34 and 37 %, respectively), which corresponds to existing refugee literature summarized in Table 5 below. Given the low educational level of the survey participants, it is likely that their understanding of their own health and medical conditions is low. In addition, poor access to medical care in refugee camps in Nepal has likely led to inaccurate or insufficient diagnoses of chronic conditions. Since we relied on participant report, there is likely underestimation of chronic conditions among the study population.
Almost 60 % of respondents had healthcare insurance, mostly the county-based indigent care program called the “Gold Card” and Medicaid; nearly 40 % were uninsured (though likely eligible for at least the county’s Gold Card); only 2 % had private insurance. As far as seeking care, 70 % said they would go to a public clinic in Houston when in need of care, but only one third reported ever visiting one; the majority were unaware of the existence of several county and city clinics.
These findings are in line with the previously reported data from other refugee studies, specifically those examining Bhutanese refugee populations. These assessments are summarized in tabular form below in Table 5:
Turning to nutrition and exercise respondents consumed daily recommended servings of fruits and vegetables more than average Americans (62 %), but exercised less (41 %). Specifically, the Bhutanese refugees in our Houston needs assessment are consuming two or more servings of fruits a day at a much higher rate than Hispanic-Americans or all Americans (comparison data from CDC MMWR, 2005) (Fig. 2).
Fruit consumption (2 or more servings/day) [27]
The Bhutanese refugees in our Houston needs assessment are also three or more servings of vegetables a day at a much higher rate than Hispanic-Americans or all Americans (comparison data from CDC MMWR, 2005) (Fig. 3).
Vegetable consumption (3 or more servings/day) [27]
However, the Bhutanese refugees are exercising less than the national average and the Hispanic-American average (comparison data from Behavioral Risk Factor Surveillance System (BRFSS), Centers for Disease Control and Prevention (CDC), 2009) (Fig. 4).
Exercise [27]
Not only were the majority of refugee respondents not exercising regularly, but 38 % were also not monitoring their weight. Many respondents who were employed noted they did not feel the need or did not have the energy to exercise due to the standing nature of their job. Lack of regular physical activity predisposes individuals to obesity, heart disease, diabetes, depression and anxiety, weakness and fatigue, poor self-image, and early mortality.
With low educational levels and low literacy, navigating processes and institutions in their new home was particularly challenging. In terms of health status, many reported poor health due to infectious diseases prevalent in refugee camps such as tuberculosis and gastrointestinal disorders. After having migrated to the US also places them at risk of numerous chronic conditions. Greater awareness of health conditions and their respective risk factors needs to be emphasized in programming among providers serving refugees. Directing resources to this particularly vulnerable population is important. Current policies limit benefits to refugees for 8 months, at which point they are far from ready to be independent.
Limitations
The sample for this Houston-based needs assessment was selected by convenience snowball sampling since random sampling was not a feasible option in our case. Despite our sample not being a representative in the strict sense, data collected was done to maximize representativeness of age and gender.
Conclusion/Recommendations
Houston hosts one of the largest Bhutanese resettlement communities nationwide—and especially emphasizing their full range of chronic health conditions. The results from this needs assessment will allow healthcare providers, researchers, policymakers, community organizations, and other stakeholders baseline data to plan programs and interventions. In addition, the assessment provides a baseline quantitative information for the Bhutanese refugee community in Houston on the state of their community’s health. As this is a needs assessment following recommendations are offered:
The Bhutanese Refugee Community
-
Emphasize education of children to enable better future employment prospects and break the cycle of poverty
-
Improve own work-related skills (English, computers), continue to seek jobs
-
If adults or children do not currently have health insurance, check eligibility guidelines for county indigent care support or other public or private coverage oriented for refugees
-
Encourage exercise with more regularity: for example, walk to grocery stores or to pick up children from school when possible and take family trips to the park
Community-Based, Non-Governmental Organizations
-
Offer private tuitions for children who attend school and English as a Second Language (ESL) classes and computer training for adults
-
Assist in Job Employment Search Process
-
Increase awareness of healthcare insurance eligibility (County’s Gold Card, Medicaid, CHIP), and assist in applications and interviews for the same
-
Increase awareness of available public health clinics in Houston and encourage their utilization
-
Conduct public health education for common health conditions (e.g., abnormal blood pressure) and recommended health behaviors (e.g., regular exercise); determine actual levels of smoking and alcohol consumption (self-reported subject to information bias due to cultural taboo)
-
Encourage community social activities to enhance physical and mental health.
Local/State/Federal Health Authorities, Policymakers
-
Create programs assisting refugees with job skills training and employment search process (lack of adequate income continues cycle of poverty and disease, which affects the entire nation by increasing healthcare costs)
-
Expand insurance coverage access and options
-
Design and implement public health programs promoting a healthy lifestyle, mental and physical wellness, and proper management of chronic disease
-
Increase public transport options to encourage utilization of healthcare
In summary, the Bhutanese refugees who resettled in the Houston area have significant health care related needs that will require a number of substantial responses from the Bhutanese refugee community itself, as well as from the government and non-governmental agencies and organizations which seek to offer assistance around health promotion in the population.
References
Van Ommeren M, Sharma B, Sharma GK, Komproe I, Cardeña E, de Jong Joop TVM. The relationship between somatic and PTSD symptoms among bhutanese refugee torture survivors: examination of comorbidity with anxiety and depression. J Trau-matic Stress. 2002;15(5):415.
Blanck HM, Bowman BA, Serdula MK, Khan LK, Kohn W, Woodruff BA. Bhutanese refugee investigation group. Angular stomatitis and riboflavin status among adolescent Bhutanese refugees living in southeastern Nepal. Am J Clin Nutr. 2002;76:430–5.
Quigley J. Bhutanese refugees in Nepal: what role now for the European Union and the United Nations high commission for refugees? Contemp South Asia. 2004;13(2):187–200.
Kharat RS. Bhutanese refugees in Nepal: survival and prospects. Econ Political Wkly. 2003;38(4):285–9.
Banki, S. Bhutanese refugees in Nepal: anticipating the impact of resettlement. Brief-ing paper. Austcare/Griffith University. 2008. Retrieved 03 Dec 2012 from http://www.austcare.org.au/ourwork/research.aspx.
Martin AA, Moore J. Infectious disease surveillance during emergency relief to Bhutanese refugees in Nepal. J Am Med Assoc. 1994;272(5):377.
Abdalla F, Mutharia J, Rimal N, Bilukha O, Talley L, Handzel T, Bamrah S. Mal-nutrition and micronutrient deficiencies among Bhutanese refugee children—Nepal. Morb Mortal Wkly Rep. 2008;57(14):370–3.
Thapa SB, Van Ommeren M, Sharma B, de Jong JT, Hauff E. Psychiatric disability among tortured Bhutanese refugees in Nepal. Am J Psychiatry. 2014;160(11):2032–7.
Cable News Network (CNN). First of 60,000 refugees from Bhutan arrive in U.S. 2008. http://edition.cnn.com/2008/WORLD/asiapcf/03/25/bhutan.refugees/.
Sreenath SN. Helping the Bhutanese refugees. Hindu Today. 2010;32(1):9.
Houston Department of Health and Human Services & Baylor College of Medicine. Health status of Bhutanese refugees in Houston, Texas. A community needs assessment of Bhutanese refugees, 2012.
World Health Statistics. World Health Organization. Geneva, Switzerland, 2009.
Navuluri NA-RKRRRJ. Assessing barriers to healthcare access among refugees living in San Antonio, Texas. Tex Public Health J. 2014;66(3):5.
Nazzal KH, Forghany M, Geevarughese MC, Mahmoodi V, Wong J. An innovative community-oriented apporach to prevention of early intervention with refugees in the United States. Psychol Services. 2014;11(4):477–85.
Lee D, Philen R, Wang Z, et al. Disease surveillance among newly arriving refugees and immigrants—electronic disease notification system, United States, 2009. MMWR Surveill Summ. 2013;62(7):1–22.
Kumar GS, Varma S, Saenger MS, Burleson M, Kohrt BA, Cantey P. Noninfectious disease among the Bhutanese refugee population at at United States urban clinic. J Immigr Minor Health. 2014;16(5):922–5.
Yun K, Fuentes-Afflick E, Desai M. Prevalence of chronic disease and insurance coverage among refugees in the United States. J Immigr Minor Health. 2012;14(6):933–40.
Haworth RJ, Margalit R, Ross C, Nepal T, Soliman AS. Knowledge, attitudes, and practices for cervical cancer screening among the bhutanese refugee community in Omaha, Nebraska. J Community Health. 2014;39(5):872–8.
Wieland ML, Weis JA, Palmer T, et al. Physical activity and nutrition among immigrant and refugee women: a community-based participatory research approach. Women’s Health Issues. 2012;22(2):e225–32.
Walker PF, O’Fallon A, Nelson K, Mamo B, Dicker S, Chute S, Swoboda P, Householder S, Painter J, ZhouW, PfeifferCM. Vitamin B12 deficiency in resettled Bhutanese refugees. U. S. centers for disease control and prevention. Morb Mortal Wkly Rep. 2011;60(11):343–6. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6011a4.htm.
Kiptinness C, Dharod JM. Bhutanese refugee in the United States: their dietary habits and food shopping practices upon resettlement. J Hunger Environ Nutr. 2011;6:75–85.
Bhatta MP, Shakya S, Assad L, Zullo, MD. Chronic disease burden among Bhutanese refugee women aged 18–65 years resettled in Northeast Ohio, United States, 2008–2011. J Immigr Minor Health. 2014; May 22. http://springerlink.bibliotecabuap.elogim.com/article/10.1007%2Fs10903-014-0040-9.
Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA. U.S. Department of Health and Human Services. 2013. http://www.cdc.gov/brfss/questionnaires/index.htm.
Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Questionnaire, 2010. U.S. Department of Health and Human Services. February, 2009 http://www.cdc.gov/brfss/questionnaires/pdf-ques/2010brfss.pdf.
Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13(1):49.
Vonnahme LA, Lankau EW, Ao T, Shetty S, Cardozo BL. Factors associated with symptoms of depression among Bhutanese Refugees in the United States. J Immigr Minor Health. 2014. doi:10.1007/s10903-014-0120-x.
Centers for Disease Control and Prevention (CDC). Morbidity and mortality weekly report. Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity—United States, 2005. 2007;56(13);301–4.
Acknowledgments
A special thanks to Sewa International, USA Houston Chapter for its generous monetary donation to each of the participating refugees in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Misra, S.M., Nepal, V.P., Banerjee, D. et al. Chronic Health Conditions, Physical Activity and Dietary Behaviors of Bhutanese Refugees: A Houston-Based Needs Assessment. J Immigrant Minority Health 18, 1423–1431 (2016). https://doi.org/10.1007/s10903-015-0282-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-015-0282-1