Abstract
Factors associated with CES-D depression among Mexican Americans living on and off the U.S.–Mexico border are examined. Data are from two studies of Mexican American adults. The Border Survey conducted face-to-face interviews in urban U.S.–Mexico border counties of California, Arizona, New Mexico, and Texas (N = 1307). The non-border HABLAS survey conducted face-to-face interviews in Houston, Los Angeles, New York, Philadelphia, and Miami (N = 1288). Both surveys used a multistage cluster sample design with response rates of 67 and 76 %, respectively. The multivariate analysis showed that border residence and higher perceived neighborhood collective efficacy were protective for depression among men. Among men, lower education, unemployment, increased weekly drinking, and poor health status were associated with depression. Among women, alcohol-related problems and poorer health status were also associated with depression. Further examinations of how neighborhood perceptions vary by gender and how these perceptions influence the likelihood of depression are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The U.S. Census Bureau estimated that in 2013, the 24 counties of California, Arizona, New Mexico, and Texas that share common borders with Mexico were home to approximately 7.5 million people [1]. The border population is predominantly Hispanic (approximately 68 %), the majority of which are of Mexican origin [1, 2]. There are several unique characteristics of the border that impact the well-being of its residents. These include high rates of poverty, under-education, and unemployment [2]. The border is also characterized by poor indices of health and many lack health insurance coverage [2]. In addition, the border is a designated “medically underserved area” due to the paucity of health care professionals there relative to non-border areas [2–5].
The extent to which living on the border, with its socioeconomic and health disadvantages, puts its residents at risk for mental health problems, such as depression, is important to assess as this condition is a major cause of disability that impairs psychosocial functioning and quality of life [6]. Data from the 2005–2009 state Behavioral Risk Factor Surveillance System (BRFSS) surveys for Arizona, California, New Mexico, and Texas show approximately equal lifetime prevalence rates of depressive disorder on and off the border (17.4 and 18.3 %, for border and non-border residents respectively) [7]. Border residents, however, were significantly less likely than non-border residents to report one or more days of poor mental health in the previous month (i.e., stress, depression, and problems with emotions) (34.5 vs. 39.2 % for border and non-border residents, respectively: p value = 0.001) [7]. The actual number of poor mental health days in the previous month, however, is comparable between border and non-border locations [8]. For example, BRFSS data from the border and non-border areas in which our current study collected data indicate that on the border, the approximate average number of poor mental health days was 3.54 (range of 2.4 days in Santa Cruz County, Arizona to 5.1 days in Imperial County, California) versus 3.62 days in non-border areas (range of 2.9 days in Harris County, where the city of Houston, Texas is located to 4.4 days in Philadelphia County, where the city of Philadelphia, Pennsylvania is located); [8]. Unfortunately, BRFSS response rates across states are low and vary widely. For example, in 2009, overall response rates in Arizona, California, New Mexico, and Texas were 23.17, 27.75, 50.90, and 29.40 %, respectively [9]. Another limitation of BRFSS data is its land-line data collection methodology. The BRFSS did not pilot a cell phone survey until 2008 [10]. Because of the increasing number of homes with wireless only telephones, the potential for survey under-coverage is great. For example, from 2007 to 2009, the prevalence of wireless only telephone technology within households ranged from approximately 17 to 27 % in Arizona, 9 to 16 % in California, 17 to 26 % in New Mexico, and 20 to 30 % in Texas [11]. The potential for bias is even greater among Hispanic households since Hispanic adults are more likely to be wireless only compared to adults of other ethnicities [12].
Several studies have linked perceptions of neighborhood disorganization and instability to depression [13–18]. Adverse neighborhood conditions are thought to lead to depression because social disorder exposes residents to greater daily stress [16]. Residents of disadvantaged neighborhoods are also more vulnerable to depression following negative life events because such neighborhoods lack appropriate resources for coping [16]. Finally, the social disorder of neighborhoods with adverse conditions makes it difficult to form and maintain meaningful social ties [16].
Utilizing the concept of collective efficacy, this paper examines the association between neighborhood disorder and depression among Mexican Americans living in U.S.–Mexico border and non-border regions. Developed by Sampson [19, 20], collective efficacy reflects the perceptions of neighborhood residents that their neighborhood acts in socially cohesive ways and implements informal social controls that maintain public order. We hypothesize that because of the socioeconomic and health disparities on the border relative to non-border areas, border residents will perceive their neighborhoods to be lower in collective efficacy and will be more likely to experience depression. We will control for several sociodemographic factors in our analyses because of their documented association with depression. These include: age, gender, socioeconomic status [21–24], level of acculturation, birthplace [24, 25], alcohol consumption [21, 24, 26, 27], and physical health status [28–30]. Because our data were collected via face-to-face household interviews, we avoid the limitations raised by telephone surveys (as per BRFSS discussed earlier).
Methods
Sample and Data Collection
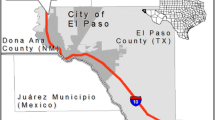
The data used for these analyses are from two separate studies of Mexican American adults: one from those living in U.S.–Mexico border areas (Border Survey) and the other, from those living in non-border areas (Hispanic Americans Baseline Alcohol Survey (HABLAS)). For the Border Survey, interviews were conducted among 1307 self-identified Mexican Americans in the U.S.–Mexico border counties of California (Imperial County: N = 365), Arizona (Cochise, Santa Cruz, and Yuma Counties: N = 173), New Mexico (Dona Ana County: N = 65), and Texas (Cameron, El Paso, Hidalgo and Webb Counties: N = 704) between March 2009 and July 2010. Data for the Border Survey were collected in urban areas for increased comparability with the non-border sample. The non-border self-identified Mexican American respondents were interviewed in 2006 as part of HABLAS (N = 1288). The majority of HABLAS respondents were interviewed in non-border cities of California and Texas (Los Angeles: N = 609 and Houston: N = 513). Additional interviews were conducted in New York (N = 86), Philadelphia (N = 59), and Miami (N = 21). Both surveys employed identical multistage cluster sampling methodologies; weighted response rates were 67 and 76 %, for the Border Survey and HABLAS, respectively.
Both surveys (Border Survey and HABLAS) utilized identical questionnaires with the exception of questions regarding drinking across the border in Mexico, which were asked only in the Border Survey given the close proximity to Mexico. The questionnaire that was initially developed for the non-border HABLAS survey (and that was also used in the Border Survey), was pre-tested in English, translated into Spanish, and then back-translated to English. The added questions for the Border Survey on drinking in Mexico were similarly pre-tested in English, translated into Spanish, and then back-translated to English. In both surveys, trained bilingual interviewers conducted approximately hour-long Computer Assisted Personal Interviews (CAPI) in respondents’ homes in either Spanish or English. With the CAPI, questions and appropriate skip patterns were programed into laptop computers and our interviewers entered the responses. In the Border Survey, 55 % of the interviews were conducted mostly or completely in Spanish whereas in the HABLAS survey, this proportion was higher, at 71 %. The interviewers for both surveys underwent the same supervised training procedure in order to ensure the uniformity of data collection and interviewing approaches.
Respondents in both samples received a $25 incentive for their participation in the study. All respondents signed a written informed consent and the Committee for the Protection of Human Subjects of the University of the Texas Health Science Center at Houston approved both the Border Survey and HABLAS.
Measures
Depression
Self-reported depression was assessed using the 20-item Center for Epidemiological Studies Depression Scale (CES-D) [31]. This valid and reliable scale is often used as a measure of depression in epidemiologic research [32]. Items were rated on a 4-point Likert-type scale ranging from 0 to 3 (total scale range: 0–60). A cumulative score of 16 or greater is considered an indicator of depression [32]. This dichotomous variable was coded “0” for “no depression” and “1” for “depression.” The scale’s intra-group reliability for these data was good (Cronbach’s α: 0.84 and 0.88; Guttman’s split-half coefficient: 0.81 and 0.87 for men and women, respectively).
Perceived Neighborhood Collective Efficacy
Collective efficacy is a valid and reliable cumulative measure of the respondents’ perceived social control and social cohesion within their neighborhood environment [19, 20]. Perceived social control was measured using a 5-item Likert-type scale on the likelihood of the following: that neighbors would intervene if children skipped school, children spray-painted graffiti, children were disrespectful toward adults, fights broke out in front of their house, and the fire station was closed due to budget cuts. Perceived social cohesion was measured using a 5-item Likert-type scale of agreement on the following statements: people around here are willing to help their neighbors, this is a close-knit neighborhood, people in this neighborhood can be trusted, people in this neighborhood generally don’t get along with each other, and people in this neighborhood do not share the same values. Because social cohesion and informal social control were closely associated (r = 0.80), Sampson et al. concluded that the two measures were assessing aspects of the same latent construct and therefore combined them into the collective efficacy summary measure [19]. Although not as strong as the correlation reported by Sampson et al., we similarly observed a relatively strong correlation between the two subscales in our data (r = 0.54). This cumulative collective efficacy measure had an acceptable level of intra-group reliability for our data (Cronbach’s α: 0.79 and 0.81 for men and women, respectively).
Because of the well documented strong association between alcohol consumption and depression [21, 24, 26, 27], these analyses controlled for the number of drinks consumed per week, binge drinking, and alcohol-related problems. The number of drinks consumed per week, a continuous measure which is widely used in epidemiological studies of alcohol use and related problems [33–35], was assessed by combining self-reported frequency and quantity of drinking wine, beer, liquor, and mixed drinks with liquor in the previous 12 months (for methodological discussions also see Room [36] and Greenfield and Kerr [37]). Binge drinking was defined as per the National Institute of Alcohol Abuse and Alcoholism: that is, drinking 4 or more (women) or 5 or more (men) standard drinks per occasion within a 2-hour period in the past 12 months (standard drink: 12 oz of beer, 5 oz of wine, 1½ ounces of liquor) [38]. Respondents were categorized as abstainers, current drinkers who did not binge in the past year (reference), and current drinkers who binged 1 or more times in the previous year. The presence of alcohol-related problems was assessed with the following items: salience of drinking (defined as when drinking becomes a higher priority than one’s health, social relationships, hobbies/interests, and obligations; [39]), need to drink, increased tolerance, impaired control, withdrawal symptoms, prolonged intoxication, financial problems, belligerence, police problems, accidents, health problems, problems with spouse, problems with others, and job problems [39, 40]. Based on the positive responses to these items, an additive scale was built. In the analyses, this variable was represented as dichotomous: zero (reference) versus 1 or more problem as is frequent in studies of alcohol epidemiology [41–43].
Sociodemographic Covariates
These analyses also controlled for several sociodemograpic factors because of their documented association with depression [7, 21–24]. The main sociodemographic independent variable for these analyses was border versus non-border (reference) location. Additional sociodemographic covariates were also controlled for these in these analyses and included: age (18–29, 30–39, 40–49, and 50+ years); level of education (some college/vocational school/beyond (reference), high school diploma/GED, and no high school diploma); income (continuous); marital status (married/cohabitating (reference), separated/divorced/widowed, and never married/never lived with anyone); employment status (working full- or part-time (reference), unemployed/temporary illness/student, homemaker, retired/disabled/never worked); religious preference (Protestant (reference), Catholic, other religion, and no preference). Place of birth (U.S. vs. foreign-born as the reference) and level of acculturation (low as the reference versus medium and high) were also controlled for in the analyses because prior research has linked these factors to depression among Hispanics [24, 25]. Developed by Caetano [44], the acculturation scale has demonstrated validity and reliability and consists of 12 questions covering the following information: daily use of and ability to speak, read, and write English and Spanish; preference for media in English or Spanish; ethnicity of people with whom respondents interact at church, at parties, the current neighborhood and the neighborhood where they were raised; and a series of questions about values thought to be characteristic of the Hispanic lifestyle. With the exception of the items used to assess language use, all other items were coded in a 4-point Likert scale (strongly agree to strongly disagree). The scales intra-group reliability for these data was good (Cronbach’s α: 0.90 and 0.91 for men and women, respectively). A continuous score of acculturation was computed, then subjects were grouped into three categories using tertiles to form low, medium, and high acculturation levels [44].
Self-rated health status was also controlled for in the analysis because of the strong and well documented association between physical and mental health [28–30]. Self-rated health status was assessed by asking respondents to indicate whether their general health status ranged from poor to excellent. In the analyses, this variable was categorized as excellent/very good/good (reference), fair, and poor.
Statistical Analysis
To account for the multistage cluster sample design used in both surveys, analyses were conducted with Stata 13 [45]. Data were weighted to correct for unequal probabilities of selection into the sample. A post-stratification weight was also applied, which corrects for nonresponse and adjusts the sample to known Hispanic population distributions on demographic variables. Bivariate associations between categorical variables were assessed with Chi square statistics. The tables depict weighted percentages with unweighted Ns. Multivariate logistic regression was used to assess predictors of depression. Due to non-response on the income item (15.2 %), log-transformed income was multiply imputed and used in the analyses (see Caetano and Mills; [46]). Preliminary models were fit using the average of the 10 imputed income values and final model estimates were obtained by combining estimates from analyses on each of the 10 imputed datasets using Rubin’s rules [47, 48]. Because the prevalence and predictors of depression vary by gender [20, 21, 23], gender-specific models were run. Also, because previous analyses of this sample detected interactions involving border proximity, gender, and age [34, 49], age by location interactions were initially tested in both male and female depression models.
Results
Sample Description
The sample was composed of 2595 Mexican Americans: 1307 residing in U.S.–Mexico border areas and 1288 residing in non-border areas. The gender distribution in the sample was almost equally split, with women representing 51 % of the sample (border: 53 %; non-border: 48 %). The percentage of respondents married or cohabitating was also comparable across locations (border: 58 %; non-border: 60 %), as was the percentage of respondents with less than a high school education (border: 49 %; non-border: 48 %). The mean annual income was 28.5 K ± 2.0 for those on the border compared to 26.0 K ± 1.2 for non-border residents. Fifty-five percent of respondents of the Border Survey and 71 % of respondents of HABLAS were born outside of the U.S. Also, although not a control variable in our analyses, it is interesting to note that 55 % of the border sample and 71 % of the non-border sample was interviewed completely or mostly in Spanish. The mean age of the border sample was higher (41.3 ± 1.0 vs. 37.8 ± 0.6 years non-border sample) and those in non-border areas were more likely to be employed part- or full-time (61 vs. 45 % among border residents).
Perceived Neighborhood Collective Efficacy on and off the Border
Perceived neighborhood collective efficacy was significantly higher among border than non-border residents (37.39 ± 0.35 vs. 36.21 ± 0.44, p = 0.04, for border and non-border residents, respectively). Differences in the mean scores for collective efficacy among men were not statistically significant (37.24 ± 0.64 vs. 36.56 ± 0.51, for border and non-border men, respectively). However, among women, those on the border had significantly higher perceived collective efficacy than those off the border (37.24 ± 0.64 vs. 35.84 ± 0.46, p = 0.01).
Bivariate Results
The weighted prevalence of depression was slightly lower among both men and women on the border compared to those off the border (Table 1). These differences, however, were not statistically significant. The bivariate analysis also showed that the proportion of men and women with depression was greater among those without a high school diploma and those who were retired, disabled, or who had never worked. While depressed individuals reported lower annual family incomes than non-depressed individuals, this association was statistically significant only among women. In particular, depressed women reported a mean income of 20.03 K (±2.03) compared to 27.10 K (±1.39) reported by non-depressed women, p = 0.003 (data not shown). While there was no association between binge drinking and depression, men and women with 1 or more alcohol-related problem were more likely to be depressed, although this association was only marginally significant among men. Depressed men also drank a statistically significantly higher number of drinks per week than non-depressed men (13.13 ± 2.11 vs. 7.50 ± 0.61 for depressed and non-depressed men respectively, p = 0.01; data not shown). Among women, however, there was no statistically significant difference in the volume of alcohol consumption in relation to depression. Self-rated health was also associated with depression. For men and women, the proportion of depressed individuals increased in a step-wise manner as health status decreased.
Multivariate Results
Interactions between border residence and age in predicting depression were not statistically significant and therefore are not reported further. The multivariate logistic regression for men showed that border residence, as well as higher perceived neighborhood collective efficacy, were protective for depression (Table 2). Among the sociodemographic variables, men with no high school diploma, compared to those with at least some college or technical/vocational education were at an increased risk for depression. Unemployed men were also more likely to be depressed compared to their employed counterparts. A higher volume of alcohol consumed per week was also associated with depression. Finally, those with poor self-rated health were more than five times more likely to suffer from depression compared to men who rated their health as good, very good, or excellent.
Among women, neither border location nor perceived collective efficacy was associated with depression (Table 2). In addition, neither measure of alcohol consumption was associated with depression; however, women with 1 or more alcohol-related problem were almost three times more likely to be depressed compared to women with no problems. Self-rated health status was also associated with depression. Women in fair health had a more than 3-fold increased likelihood of depression and those in poor health were almost seven times more likely to be depressed compared to women of good to excellent health.
Discussion
We hypothesized that the prevalence of CES-D depression would be higher on the border than off the border. In contrast, we found that on the border, the prevalence of depression was slightly lower than the prevalence off the border; however, these differences were not statistically significant (i.e., 15 % of border men and 23 % of border women were depressed vs. 19 % of non-border men and 25 % of non-border women). In the multivariate analyses, after controlling for the effects of covariates, residing on the border, compared to off the border, was protective for depression among men, but not women. These were surprising findings given the socioeconomic and health disparities on the border relative to non-border areas. However, in spite of its socioeconomic hardships, border regions are unique because of the level of symbiosis, or cross-border interdependence between Mexico and the U.S. [50, 51]. Border culture has been shaped by a history of interactions between Mexico and the U.S., including the geographical mobility between the two countries and the associated international and ethnic conflicts and compromises that have arisen over time. All this has resulted in a sense of uniqueness, great resiliency, and a growing social and political awareness among residents on both sides of the border [50, 51]. This uniqueness is evident in the blending of both Mexican and Anglo traditions, language, religion, values, and customs.
The rich and unique qualities of border culture may also provide some explanation as to why, contrary to our hypothesis, border residents perceived their neighborhoods to be more socially cohesive and better able to implement informal social controls (i.e., collective efficacy) than did non-border residents. The analyses also showed that higher perceived neighborhood collective efficacy was associated with a lesser likelihood of depression. This finding is in accordance with previous findings in this area [14, 15]. It is possible that stronger collective efficacy buffers the effects of daily stressors that lead to depression [15]. These findings, however, were only significant for men, a finding previously seen in the literature [52]. For example, Vaeth et al. [52] found that among men, but not women, the likelihood of depression decreased as the sense of collective efficacy increased and this association was independent of other risk factors for depression such as heavy drinking, alcohol-related problems, and intimate partner violence. Higher perceived collective efficacy was not protective for depression among women, in spite of the fact that the mean levels for women were essentially equal to those of men. This could be due to the differences in the nature and size of social support systems between men and women [53, 54]. For example men’s social networks have been reported to consist more of co-workers and friends whereas women’s consist mostly of kin [53, 54]. Uchino et al. [55] have described how familial sources of support are important factors in protecting one’s health and well-being. Indeed, Márquez and Romo [56] emphasize how the border region is grounded in strong family values and family unity. Unfortunately, we did not have a measure of family unity or family cohesion to examine in these analyses.
Among women, in the multivariate logistic regression model, the likelihood of depression did not vary by location. Ryan-Ibarra et al. similarly found that the prevalence of depression did not vary in relation to border residence status among California women [57]. In this study, binge drinking predicted depression in both border and non-border areas of California [57]. In our study, binge drinking was not associated with women’s depression; however, the presence of alcohol-related problems was. Women with 1 or more problem were almost three times more likely to be depressed compared to women with no problems. This association has been well documented by previous research [21, 22, 24, 25]. The only other variable that was associated with depression among women was self-rated health status. Women who reported their health as fair had a more than 3-fold increased likelihood of depression and those in poor health were at nearly a 7-fold increased risk. Poor self-rated health was also associated with a 5-fold increased likelihood of depression among men. These findings were not surprising given the strong association between physical and mental health status [27–29].
Among men, those with less than a high school education were approximately two times more likely to be depressed. This is in contrast to findings from the Collaborative Psychiatric Epidemiology Studies (CPES) and the National Latino and Asian American Study (NLAAS) that showed no association between level of education and major depressive disorder in CPES and any depressive disorder in NLAAS among Hispanics [58, 59]. Unemployed men were also at increased risk for depression, although this was not the case among women, a finding that is also supported in the literature [22]. Finally, among men, the likelihood of depression increased as the weekly consumption of drinks increased. It is possible that drinking contributes to the development of depression and/or that depressed men are drinking more in a chronic manner as a coping mechanism. It is surprising, however, that neither binge drinking nor the presence of alcohol-related problems was associated with depression among men. Regarding binge drinking, this behavior is prevalent among Mexican American men and often occurs at social events [34, 35, 60]. In fact there is some evidence that binge drinking may have a protective effect on depression among men [52].
This study has some important strengths. Using the same selection and interviewing methodology, data were collected from representative samples of Mexican Americans living in both border and non-border areas of the U.S., thus allowing for comparisons across locations. In addition, this study collected comprehensive data on a variety of topics, including depression, health status, collective efficacy, and alcohol use during face-to-face interviews. Importantly, interviews were conducted by bilingual interviewers so that both English and Spanish speakers were included and in fact, 55 % of the border sample and 71 % of the non-border sample was interviewed completely or mostly in Spanish. In spite of the larger proportion of non-border residents who were interviewed in Spanish, there were no differences in level of acculturation between border and non-border groups [61]. Further, in this study, level of acculturation was not associated with depression for either men or women.
This study also has some limitations. In spite of relatively good response rates for both the border and non-border samples, the border response rate was only 67 % (compared to 76 % off the border). Because the two surveys were restricted to urban areas, our findings may not be generalizable to the rural Mexican American population. In addition, the Border Survey and HABLAS were not conducted concurrently; however, the epidemiology of alcohol in large populations is relatively stable [62, 63], as is the prevalence of depression given the chronic nature of this condition [6, 64]. Another limitation of this study is that the identification of depression with the CES-D is not based on clinical criteria. However, research has shown a good level of agreement between the CES-D’s use of a cut-off point of 16 or more depressive symptoms and a clinical diagnosis of depression [32, 65]. Also, this is a cross-sectional analysis and a temporal order in the relationships between our independent variables and depression cannot be established. Finally, this paper focuses on a special U.S. population and the generalizability of these findings to other populations in the world may be limited. However, in the U.S., Mexican Americans have a strong and growing presence, representing 64 % of the total Hispanic population in 2012 [66]. Given the significant impact of depression on functional status and quality of life [6], further examinations of how neighborhood perceptions vary by gender and how these perceptions influence the likelihood of depression are warranted.
References
United States Census Bureau. American Fact Finder. Annual Estimates of the Resident Population: April 2010 to July 1 2013. 2014. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed 10 Oct 2014.
Bhavsar GP, Martin AB, Probst JC, Torres ME, Iyer M, Hardin J. Rural border health chartbook II. Columbia: South Carolina Rural Health Research Center, Rural Health Research & Policy Centers; 2014.
Soden DL. At the cross roads: U.S./Mexico border counties in transition. U.S./Mexico border County Coalition. 2006.
Gerber J. Developing the U.S.–Mexico border region for a prosperous and secure relationship: human and physical infrastructure along the U.S. border with Mexico. 2009.
Pan American Health Organization. United States–Mexico border area. Health in the Americas Volume II-Countries. 2007. http://www.paho.org/hia/archivosvol2/paisesing/United%20States%20Mexico%20Border%20Area%20English.pdf. Accessed 10 Oct 2014.
Hellerstein DJ, Agosti V, Bosi M, Black SR. Impairment in psychosocial functioning associated with dysthymic disorder in the NESARC study. J Affect Disord. 2010;127(1–3):84–8.
Martin AB, Torres M, Vyavaharkar M, Chen Z, Towne S, Probst JC. Rural border health chartbook. Columbia: South Carolina Rural Health Research Center, Rural Health Research & Policy Centers; 2013.
University of Wisconsin Population Health Institute School of Public Health. 2015. County Health Rankings & Roadmaps. Poor mental health days, 2010. http://www.countyhealthrankings.org/. Accessed 21 May 2015.
Centers for Disease Control. Behavioral risk factor surveillance system 2009 summary data quality report. Version #1. 2011. http://www.cdc.gov/brfss/annual_data/2009/pdf/2009_Summary_Data_Quality_Report.pdf. Accessed 24 Feb 2015.
Centers for Disease Control. Behavioral risk factor surveillance system cell phone pilot operational protocol. 2008. http://www.ndhealth.gov/brfss/publications/2008%20BRFSS%20Cell%20Phone%20Pilot%20Opeartional%20Protocol-Final.pdf. Accessed 24 Feb 2015.
Blumberg SJ, Luke JV, Ganesh N, Davern ME, Boudreaux MH, Soderberg K. Wireless substitution: state-level estimates from the National Health Interview Survey, January 2007–June 2010. National health statistics reports; no 39. Hyattsville, MD: National Center for Health Statistics. 2011.
Blumberg SJ, Luke JV. Wireless substitution: early release of estimates from the National Health Interview Survey, January–June 2012. National Center for Health Statistics. July 2014. http://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless201407.pdf. Accessed 3 Mar 2015.
Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37(4):293–310.
Ross CE. Neighborhood disadvantage and adult depression. J Health Soc Behav. 2000;41:177–87.
Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003;44(1):34–44.
Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. J Abnorm Psychol. 2005;114(1):3–15.
Gary TL, Stark SA, LaVeist TA. Neighborhood characteristics and mental health among African Americans and Whites living in a racially integrated urban community. Health Place. 2007;13(2):569–75.
Echeverria S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Association of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health Place. 2008;14(4):853–65.
Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–24.
Sampson RJ. The neighborhood context of well-being. Perspect Biol Med. 2003;46(3):S53–64.
Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder. Results from the National Epidemiologic Survey on alcoholism and related conditions. Arch Gen Psychiat. 2005;62(10):1097–106.
Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13.
Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav. 2009;74:264–82.
Golding JM, Burnam MA, Benjamin B, Wells KB. Risk factors for secondary depression among Mexican Americans and non-Hispanic Whites. J Nerv Ment Dis. 1993;181(3):166–75.
Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou P, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic Whites in the United States. Results from the National Epidemiologic Survey on alcohol and related conditions. Arc Gen Psychiat. 2004;61:1226–33.
Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiat. 2004;61(8):807–16.
Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118(4):330–41.
Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates, and association with health resource utilization, lost productivity, and functional disability. Gen Hosp Psychiatry. 2007;29(5):409–16.
Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiat. 2007;29(2):147–55.
Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–8.
Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401.
Radloff L, Locke BZ. The community mental health survey and the CES-D scale. In: Weissman MM, Myers JK, Ross CE, editors. Community surveys of psychiatric disorders. New Brunswick: Rutgers University Press; 1986. p. 177–89.
Moore AA, Gould R, Reuben DB, Greendale GA, Carter K, Karlamangla ZK. Longitudinal pattern and predictors of alcohol consumption in the United States. Am J Public Health. 2005;95:458–65.
Caetano R, Mills BA. Vaeth PAC. Alcohol consumption and binge drinking among U.S.–Mexico border and non-border Mexican Americans. Alcohol Clin Exp Res. 2012;36(4):667–85.
Ramisetty-Mikler S, Caetano R, Rodriguez LA. The 2006 Hispanic Americans Baseline Alcohol Survey (HABLAS): alcohol consumption patterns and sociodemographic predictors among Hispanic national groups in the United States. J Subst Use. 2010;15(6):402–16.
Room R. Measuring alcohol consumption in the U.S.: methods and rationales. In: Clark WB, Hilton ME, editors. Alcohol in America. Drinking practices and problems. Albany: State University of New York Press; 1991.
Greenfield TK, Kerr WC. Alcohol measurement methodology in epidemiology: recent advances and opportunities [Review]. Addiction. 2008;103(7):1082–99.
National Institute on Alcohol Abuse and Alcoholism. NIAAA council approved definition of binge drinking. No. 3. Publications Distribution Center; Rockville, MD. NIAAA Newsletter; p.3. http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf. Accessed 25 June 2014.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Brit Med J. 1976;1:1058–61.
Hilton ME. Demographic characteristics and the frequency of heavy drinking as predictors of self-reported problems. In: Clark WB, Hilton ME, editors. Alcohol in America. Drinking practices and problems. Albany: State University of New York Press; 1991.
Vaeth PAC, Caetano R, Ramisetty-Mikler S, Rodriguez LA. Hispanic Americans Baseline Alcohol Survey (HABLAS): alcohol-related problems across Hispanic National Groups. J Stud Alcohol Drugs. 2009;70:991–9.
Caetano R, McGrath C, Ramisetty-Mikler S, Field CA. Drinking, alcohol problems and five-year recurrence and incidence of male to female and female to male partner violence. Alcohol Clin Exp Res. 2005;29(1):98–106.
Caetano R, Kaskutas LA. Changes in drinking problems among Whites, Blacks, and Hispanics, 1984–1992. Subst Use Misuse. 1996;31:1547–71.
Caetano R. Acculturation and drinking patterns among US Hispanics. Brit J Addict. 1987;82:789–99.
StataCorp. Stata statistical software: release 13. College Station: StataCorp LP; 2013.
Caetano R, Mills BA. The Hispanic Americans Baseline Alcohol Survey (HABAS): is the “Prevention Paradox” applicable to alcohol problems across Hispanic national groups? Alcohol Clin Exp Res. 2011;35(7):1256–64.
Carlin JB, Galati JC, Royston P. A new framework for managing and analyzing multiply imputed data in Stata. Stata J. 2008;8(1):49–67.
Rubin DB. The calculation of posterior distributions by data augmentation: comment: a noniterative sampling/importance resampling alternative to the data augmentation algorithm for creating a few imputations when fractions of missing information are modest: The SIR algorithm. J Am Stat Assoc. 1987;82(398):543–6.
Caetano R, Vaeth PAC, Mills BA, Rodriguez LA. Alcohol abuse and dependence among U.S.–Mexico border and non-border Mexican Americans. Alcohol Clin Exp Res. 2013;37(5):847–53.
Ganster P, Lorey D. The U.S.–Mexican Border into the Twenty-first Century. Plymouth: Rowman & Littlefield Publishers, Inc.; 2008.
Martinez OJ, Lorey D. Border people: life and society in the U.S.–Mexico borderlands, vol. 2. Tucson: The University of Arizona Press; 1994.
Vaeth PAC, Ramisetty-Mikler S, Caetano R. Depression among couples in the United States in the context of intimate partner violence. J Interpers Violence. 2010;25(5):771–90.
Moore G. Structural determinants of men’s and women’s personal networks. Am Soc Rev. 1990;55(5):726–35.
Munch A, McPherson JM, Smith-Lovin L. Gender, children, and social contact: the effects of childrearing for men and women. Am Soc Rev. 1997;62(4):509–20.
Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488–531.
Márquez RR, Romo HD. Transformations of La Familia on the U.S.–Mexico border. Notre Dame: University of Notre Dame Press; 2008.
Ryan-Ibarra S, Epstein JF, Induni M, Wright MA. Current depression among women in California according to residence in the California–Mexico border region. Rev Panam Salud Pública. 2012;31(5):417–26.
Gavin AR, Walton E, Chae DH, Alegría M, Jackson JS, Takeuchi D. The associations between socioeconomic status and major depressive disorder among Blacks, Latinos, Asians, and non-Hispanic Whites. Psychol Med. 2010;40(1):51–61.
Cook B, Alegría M, Lin JY, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99(12):2247–54.
Treno AJ, Alaniz ML, Gruenewald PJ. The use of drinking places by gender, age and ethnic groups: an analysis of routine drinking activities. Addiction. 2000;95(4):537–51.
Mills BA, Caetano R. Decomposing associations between acculturation and drinking in Mexican Americans. Alcohol Clin Exp Res. 2012;36:1205–11.
Caetano R, Baruah J, Ramisetty-Mikler S, Ebama MS. Sociodemographic predictors of pattern and volume of alcohol consumption across Hispanics, Blacks, and Whites: 10-year trend (1992–2002). Alcohol Clin Exp Res. 2010;34(10):1782–92.
Caetano R, Clark CL. Trends in alcohol consumption patterns among Whites, Blacks and Hispanics: 1984 and 1995. J Stud Alcohol. 1998;59(6):659–68.
Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, Hirschfeld RM, Shea T. Time to recovery, chronicity, and levels of psychopathology in major depression. A 5-year prospective follow-up of 431 subjects. Arch Gen Psychiat. 1992;49(10):809–16.
Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–14.
U.S. Census. Hispanic Americans by the numbers: from the U.S. Census Bureau. 2014. http://www.infoplease.com/spot/hhmcensus1.html. Accessed 26 May 2015.
Acknowledgments
Preparation of this article was supported by grants (RO1-AA013642 and RO1-AA016827) from the National Institute on Alcohol Abuse and Alcoholism to the Prevention Research Center, Pacific Institute for Research and Evaluation, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vaeth, P.A.C., Caetano, R. & Mills, B.A. Factors Associated with Depression Among Mexican Americans Living in U.S.–Mexico Border and Non-Border Areas. J Immigrant Minority Health 18, 718–727 (2016). https://doi.org/10.1007/s10903-015-0236-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-015-0236-7