Abstract
We examined associations between intimate partner forced sex (IPFS) and HIV sexual risk behaviors among physically abused Black women. Women aged 18–55 in intimate relationships were interviewed in health clinics in Baltimore, MD and St. Thomas and St. Croix, US Virgin Islands (USVI). Of 426 physically abused women, 38 % experienced IPFS; (Baltimore = 44 and USVI = 116). USVI women experiencing IPFS were more likely to have 3+ past-year sex partners (AOR 2.06, 95 % CI 1.03–4.14), casual sex partners (AOR 2.71, 95 % CI 1.42–5.17), and concurrent sex partners (AOR 1.94, 95 % CI 1.01–3.73) compared to their counterparts. Baltimore women reporting IPFS were more likely to have exchanged sex (AOR 3.57, 95 % CI 1.19–10.75). Women experiencing IPFS were more likely to report their abuser having other sexual partners in Baltimore (AOR 3.30, 95 % CI 1.22–8.88) and USVI (AOR 2.03, 95 % CI 1.20–3.44). Clinicians should consider the influence of IPFS on individual and partnership HIV sexual risk behaviors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Women of color are disproportionately affected by both intimate partner violence (IPV) and HIV [1–4]. Despite increased attention to HIV acquisition risk among women experiencing IPV, very little research examines intimate partner forced sex (IPFS) as a related but independent risk factor [5]. Reported prevalence of IPFS varies globally. In Sub-Saharan Africa, lifetime prevalence of IPFS ranges from 10 to 59 % [6, 7]. US population-based studies estimate approximately one in ten women experience forced sex during their lifetime, with 30–50 % perpetrated by a current or former intimate partner [8, 9]. Among African American adult women and adolescents, studies have reported the prevalence of forced sex by partners or others to be between 14 and 42 % [10–12].
Few studies document the association between IPFS and HIV risk while accounting for the heterogeneous nature of Black women. Within the social environment, cultural norms related to IPFS may differ within different groups of Black women (i.e., African American, African Caribbean, African born) [13, 14]. With this in mind, we examined the association between IPFS and HIV sexual risk among Black women in Baltimore, Maryland and in the US Virgin Islands (USVI) (St. Thomas and St. Croix), both areas with high HIV prevalence among Black women [15, 16].
Conceptual Framework
As the HIV epidemic shifts towards women of color exposed primarily through heterosexual contact [16–18], the intersection of gender-based violence and HIV sexual risk deserves further scrutiny. Sexual violence can increase women’s risk for HIV directly through forced/coerced sex by an infected partner and indirectly through individual and partnership sexual risk behaviors (e.g., sex-partner concurrency, inconsistent condom use, substance abuse) [5, 19–22]. Although sexual violence takes many forms, physically forced sexual intercourse is the most direct route for HIV transmission [23]. In this study, we hypothesized that an experience of IPFS would result in increased HIV sexual risk behaviors. We therefore examined HIV sexual risk behaviors as outcomes of an experience of IPFS.
Forced sex has been associated with increased sexual risk behaviors and serious gynecologic sequelae [10, 12, 24–26]. The growing body of studies focusing on Black women found similar associations. Specifically, in a recent longitudinal study [12] and a previous cross-sectional study [10] among US African American adolescent females, those with rape victimization histories reported less condom-protected sex, less condom use at last sex, and more sex partners at follow-up compared to their counterparts. South African female students who experienced threats of violence or physically forced sex were less likely to use condoms consistently [27]. Wingood and colleagues [28] also found among African American women aged 18–24, a history of IPFS was associated with increased HPV incidence. Among a sample of African American women living in low-income housing, 42 % experienced coerced sex, either by threats or physical force and were more likely to be physically abused, and fearful of asking their partner to use a condom [11]. Josephs and Mazur Abel [29] found coerced sex mediated the relationship between IPV and HIV risk through decreased efficacy in sexual decision-making in a sample of adult African American women in intimate relationships. If women with a history of IPFS (IPFS+) are more likely to engage in HIV sexual risk behaviors than women who experience physical IPV without forced sex (IPFS−) it behooves researchers and healthcare providers to examine IPFS as a distinct risk factor.
Methods
Participants
Data were collected as part of a multi-site case–control study examining the impact of intimate partner abuse (IPA: physical, sexual and/or psychological abuse) on health outcomes among Black women, which has been described elsewhere [30–32]. Study team members recruited participants from primary care, prenatal or family planning clinics in Baltimore, MD and St. Thomas and St. Croix, USVI between 2009 and 2011. Eligible women were aged 18–55, had an intimate relationship in the past 2 years and identified as being of racial or ethnic heritage including African descent.
Data Collection
Consented women completed surveys via audio computer-assisted self-interviews (ACASI) in private clinic offices. Each participant received $20 remuneration and a list of local social service and violence-related resources. The Institutional Review Boards at Johns Hopkins University and the University of the Virgin Islands approved the study.
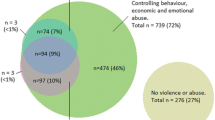
Women screening positive for a history of IPA were enrolled as cases. To obtain comparable group sizes in a population where non-abuse is more prevalent than abuse, never-abused women were randomly selected by the ACASI system as controls. “Non-selected controls” were those never-abused women who were eligible but not enrolled. Of the 1,579 women screened, 1,315 were eligible. Eleven did not finish the survey, 403 were non-selected controls, and 901 women participated in the study (543 cases; 358 controls). This analysis uses data from 426 women who reported physical IPV and compares women with a history of both IPFS and physical IPV (physical violence with or without psychological abuse; IPFS+) to those who experienced physical IPV only (IPFS−). Women reporting psychological abuse in the absence of physical or sexual abuse were excluded.
Measures
Dependent Variables
STI History
Women reporting past year STIs, including Chlamydia, gonorrhea, syphilis, and HIV were classified as positive for STI history.
Number and Type of Sexual Partners
Women were asked their number of male sexual partners in the past year, dichotomized to three or more or less than three, a common cut point in HIV risk literature [33, 34]. Women were also asked if they ever had exchange sex partners (i.e., sex in exchange for food, money, shelter, or drugs) and casual sex partners (i.e. men you hook up with from time to time to have sex).
Concurrent Sex Partners
We use the terms concurrent sex partners and sex-partner concurrency to denote one person engaging in sexual activities with more than one sex partner during the same time frame. Women were asked whether they and whether their current partners had ever engaged in sexual activity outside their relationships. Those answering “I don’t know” were recoded as “no”. Women without a current partner skipped these questions. Participants were also asked about concurrent sex partners in their most recent abusive relationship, whether they and separately, whether their abuser—which may have been different from their “current” partner—had engaged in sexual activity outside the relationship.
Condom Use and Negotiation
Women were asked how often condoms were used at the last five vaginal and last five anal sex acts. Participants could indicate not having experienced anal sex; these women were excluded from analysis specific to anal intercourse (61 % of Baltimore sample, 64 % of USVI sample). Those responding “always” were coded as “always using condoms”. All other answers were coded as “inconsistent condom use.”
Women were asked if they had ever asked their partner to use a condom and if they had ever refused sex when their partner did not want to use a condom. Women who responded “yes” to refusing sex over condom use were asked about violent responses, including (a) how often the partner threatened to hit her and (b) how often the partner actually hit her when asked to use a condom. Responses were dichotomized as “never” versus “at least once”.
Independent Variables
Sociodemographics
Demographic characteristics included age, race/ethnicity, proxies for socioeconomic status (i.e., education, monthly income, employment status, health insurance status, public aid), partnership status, pregnancy at time of survey, and children less than 18 years old living in the household.
Intimate Partner Forced Sex (IPFS)
Women were asked: (a) if in the past 2 years an intimate partner had forced her to have sexual activities, (b) if in the past 12 months they were physically forced (like hitting, holding down or using a weapon) to have oral, vaginal or anal sex by a partner with frequency (never, once, a few times, many times, not in past 12 months, but it did happen before), and (c) as part of the Danger Assessment, if a current or most recent abuser had ever forced her to have sex when she did not want to [26]. We present a frequency of past year forced sex experiences (vaginal, oral, and anal) based on their responses to “b” above. Because these questions were not cumulative nor mutually exclusive, the decision was made to code a positive response to any of the above questions as IPFS+.
Analysis
We calculated percentages of women who reported IPFS (IPFS+). Descriptive statistics characterized the sample. All further analysis was stratified by recruitment site. Differences in HIV sexual risk behaviors between IPFS+ women and IPFS− women were analyzed using Pearson’s Chi square or Fischer’s exact tests for binary variables. Bivariate relationships between IPFS and a total of 15 HIV sexual risk behaviors were examined. A series of generalized linear models were carried out for the dependent variables, including individual and partnership HIV sexual risk factors. HIV sexual risk behaviors related to IPFS with p values of <0.20 were examined further for relationships with sociodemographic variables. The multivariate models were adjusted for those sociodemographic variables with p values of <0.20 in bivariate analyses or those which were theoretically relevant. Analyses were conducted using STATA version 11.0.
Results
The majority of the 426 women who experienced physical IPV self-identified as Black, African American, or African Caribbean without Hispanic and/or Latino ethnicity (91 %). Over three quarters (79 %) were under age 35. Seventy-six percent reported having a current partner, and 81 % had at least a high school diploma or GED. Half (50 %) were unemployed, although 64 % reported having health insurance. Only 22 % reported no children under age 18 in the household and 26 % were pregnant at the time of survey. Most (88 %) reported individual monthly income below $1,200, and 76 % reported receiving aid (i.e., housing assistance, Medicaid, WIC, food stamps, public assistance) (see Table 1). Only one woman self-reported having HIV. Over 20 % reported having an STI in the past year.
Over one-third (38 %) reported an experience of IPFS, 44 women in Baltimore and 116 in the USVI. Thirty-nine percent of IPFS acts were vaginal, 26 % oral, 21 % anal, and 14 % were unspecified. Of 39 women reporting past-year forced vaginal sex, 10 (26 %) reported it happening many times. Of 23 women reporting past-year forced oral sex, 9 (39 %) reported that it occurred at least a few times, while 4 (17 %) reported it happening many times. Finally, of 22 women reporting past-year forced anal sex, 4 (18 %) reported it occurring at least a few times and 3 (14 %) reported it occurring many times. There were no differences between Baltimore and USVI on types and rates of forced sex. Additionally, 11 (23 %) of the 47 women reporting forced vaginal, oral or anal sex in the past year experienced at least two types while 13 (28 %) experienced all three types.
In Baltimore, three of the 15 sexual risk factor outcomes examined in bivariate analysis were associated with IPFS at p value <0.20: lifetime exchange sex, sex-partner concurrency by most recent abuser, and inconsistent condom use for anal sex (see Table 2). In the USVI, nine of the 15 sexual risk factors were associated with IPFS at p value <0.20: 3+ male sex partners in the past year, lifetime exchange sex, lifetime casual sex, sex-partner concurrency by most recent abuser, participant sex-partner concurrency during current and/or most recent abusive relationship, inconsistent condom use for anal sex, never asking most recent abuser to use a condom, and never having refused sex if a partner did not want to use a condom (see Table 3).
IPFS and Number and Type of Sexual Partners
Accounting for socio-demographics, IPFS+ women in Baltimore were over three times (AOR 3.57; 95 % CI 1.19–10.75) more likely to report ever having exchange sex partners than IPFS− women. IPFS+ USVI women were over two times (AOR 2.06; 95 % CI 1.03–4.14) more likely to report 3+ male sexual partners in the past year than IPFS− women. IPFS+ women in the USVI were also almost three times as likely to report ever having casual sex partners (AOR 2.71, 95 % CI 1.42–5.17) than IPFS− women (see Table 4).
IPFS and Concurrent Sex Partners
Experiencing IPFS was independently associated with women reporting their most recent abusive partner having concurrent sexual partners during the relationship in both Baltimore (AOR 3.30; 95 % CI 1.22–8.88) and the USVI (AOR 2.03; 95 % CI 1.20–3.44). In addition, IPFS+ USVI women were almost twice as likely (AOR 1.94; 95 % CI 1.01–3.73) to report concurrent sexual partners during a current relationship (see Table 5).
IPFS and Condom Use and Negotiation
Ever experiencing anal intercourse was reported by 174 (40 %) women; 57 in Baltimore and 117 in the USVI. Although in bivariate analysis at both sites IPFS was associated with inconsistent condom use during anal intercourse (p value = 0.13) this relationship did not attain statistical significance at either site when adjusting for sociodemographic variables (results not shown). No relationship existed between IPFS and condom use at last intercourse or inconsistent condom use during last five vaginal sex acts. IPFS was not significantly associated with any of the condom negotiation variables (results not shown).
Discussion
In our sample of Black women with experiences of physical IPV, one in three also reported a history of IPFS. This is considerably higher than national estimates of less than one in ten women experiencing both IPFS and physical abuse among women exposed to any type of IPV[8]. However, it is comparable to the prevalence of forced sex in convenience samples of physically abused African American adult women and adolescents [10–12, 24]. There were differences in the sexual risk behaviors associated with IPFS in Baltimore and USVI. IPFS+ Baltimore women were more likely to report ever having engaged in exchange sex than IPFS- Baltimore women. IPFS+ USVI women were more likely to report having three or more sex partners in the past 12 months, were more likely to report ever having engaged in casual sex and were more likely to report sex-partner concurrency than IPFS− USVI women. IPFS+ women in both Baltimore and the USVI were more likely to report having an abuser with concurrent sex partners than their IPFS− counterparts.
Our study extends prior findings on forced sex suggesting physically abused women with histories of IPFS are more likely to report multiple, casual, and exchange sex partners than those without a history of IPFS [12, 25]. Our findings also echo previous studies from multiple settings including the US [35], Tanzania [36], and South Africa [37], which indicate that abusers are more likely to engage in sexual risk behaviors thus increasing the risk of HIV transmission to their partners. Far less research has examined women’s sex-partner concurrency, although recent research has shown an association between IPV and partner concurrency in young adults [38]. Our finding that IPFS+ USVI women are more likely to have concurrent sex partners than IPFS− USVI women is similar to a recent study showing that women who experienced forced sex as an adult were almost two times more likely to report concurrent sexual partnerships [39]. With our data, we are unable to assess whether these concurrent sexual partners were casual or exchange sex partners.
The lack of a relationship between IPFS and condom use during vaginal and/or anal sex is not entirely surprising. Similar to previous findings, we found that a history of IPFS was not independently predictive of consistent condom use for vaginal sex with any partner [40, 41]. The lack of relationship between IPFS and condom use for anal sex may be a result of reduced statistical power due to analyzing site data separately as well as the smaller proportion of women at both sites reporting engaging in anal sex. The lack of relationship may also be due to increased difficulty negotiating safe sex associated with any kind of violence (whether physical and sexual or physical only) [42]. Condom negotiation difficulty was further illustrated in our data with over 20 % of IPFS+ women being hit over condom negotiation and 14 % of IPFS− reporting the same. Because our data is cross-sectional, we cannot determine whether refusing sex over condom use preceded forced sex perpetration or vice versa, or even whether the reported inconsistent condom use represented a forced sex event. Nearly three quarters (74 %) of physically abused women, irrespective of IPFS, requested condom use during the relationship.
Similarly, there was no significant difference in reported past year STI between IPFS+ and IPFS− women at either site. Again, the lack of association may be related to condom negotiation difficulty in the presence of any violence. In a previous analysis from the same parent study comparing IPA cases to never abused controls, USVI IPA cases reported higher rates of STIs, but not Baltimore IPA cases [32]. It is important to note that common STIs are often asymptomatic in women, therefore rates of STIs in this sample may be higher than reported [43]. Finally, the rates of STIs (including chlamydia, gonorrhea and syphilis as well as herpes and HIV/AIDS) in our sample are much higher than general population rates in both Baltimore (approximately 1.5 %) [44] and USVI (<1 %) [45] for chlamydia, gonorrhea and syphilis.
Limitations to this post hoc analysis include the cross-sectional design, which limited our ability to establish causal relationships between IPFS and HIV sexual risk factors. Furthermore, no biologic measures were collected as part of the parent study so we relied on self-report for past year STI history. Although we assessed whether women and/or their partners were engaging in sexual activity with concurrent partners, we did not assess whether women were currently in a monogamous relationship which may have impacted the results of our condom use analysis. There was also potential for recall bias in regards to condom use; however, we limited the assessment to last five vaginal/anal acts to reduce this possibility. Our use of a dichotomous measure of lifetime casual and exchange sex partners limited the ability to identify true HIV sexual risk given lack of continuous data. Despite this limitation there was still an association with exchange sex and IPFS in Baltimore, and casual sex IPFS in the USVI. Findings from the study may not be generalizable to Black women outside Baltimore, MD and St. Thomas and St. Croix, USVI. Additionally, our study focused on women of reproductive age; results are not generalizable to early adolescents or elderly women. Nonetheless, our study has a number of strengths including its focus on IPFS and Black women, a population experiencing high rates of HIV/STIs and sexual violence.
Our findings provide directions for future research. Longitudinal studies are needed to examine the temporal relationship between IPFS and sexual risk behaviors. Other studies need to examine how characteristics such as mental health and substance abuse influence the context of IPFS increasing women’s vulnerability to forced sex. Sex-partner concurrency among women warrants further examination in the causal pathways between vulnerability to IPFS, mental health, and HIV/STI risks. Intervention studies could provide evidence for the best methods of assessing for IPFS and best practices for improving women’s self-efficacy and decreasing HIV risk behaviors, specifically in an abusive relationship. All studies should include culturally appropriate strategies and recognize diversity within a racially and ethnically diverse group of women.
New Contribution to the Literature
The findings from this study demonstrate that even in the context of physical abuse, IPFS is associated with greater likelihood of engaging in sexual risk behaviors. Sexual violence and physical violence are qualitatively different. Furthermore, our findings support the need for cultural sensitivity to the differential ways Black women may engage in sexual risk behaviors depending on location, cultural norms, and cultural background. In Baltimore there may be a need to focus on factors predisposing Black women to engage in exchange sex, such as substance use and unmet subsistence needs. In the USVI it may be appropriate to focus on reducing the number of past year sex partners and/or sex-partner concurrency.
The high prevalence of IPFS is noteworthy among these two groups of women. IPFS was associated with exchange sex in Baltimore as well as increased number of past year sex partners, casual sex, and sex-partner concurrency in the USVI. All of these behaviors are known sexual risk factors for HIV transmission. Therefore we encourage existing HIV prevention programs (whether community- or clinic-based) to incorporate routine assessment for forced sex in addition to IPV as it may indicate a need to tailor programmatic HIV prevention efforts.
References
Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. The national intimate partner and sexual violence survey (NISVS): 2010 summary report. Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2011.
Taft CT, Bryant-Davis T, Woodward HE, Tillman S, Torres SE. Intimate partner violence against African American women: An examination of the socio-cultural context. Aggression and Violent Behavior. 2009;14(1):50–8.
Centers for Disease Control and Prevention. Disparities in diagnoses of HIV infection between blacks/African Americans and other racial/ethnic populations—37 states, 2005–2008. Morb Mortal Wkly Rep. 2011;60(4):93–8.
Le Franc E, Samms-Vaughan M, Hambleton I, Fox K, Brown D. Interpersonal violence in three Caribbean countries: Barbados, Jamaica and Trinidad and Tobago. Revista Panamericana de Salud Pública. 2008;24(6):409–21.
Stockman JK, Lucea MB, Campbell JC. Forced sexual initiation, sexual intimate partner violence, and HIV risk in women: a global review of the literature. AIDS Behav. 2013;17(3):832–47.
Garcia-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368:1260–9.
Koenig MA, Lutalo T, Zhao F, Nalugoda F, Kiwanuka N, Wabwire-Mangen F, et al. Coercive sex in rural Uganda: Prevalence and associated risk factors. Soc Sci Med. 2004;58(4):787–98.
Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. The national intimate partner and sexual violence survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2011.
Basile K, Arias I, Desai S, Thompson MP. The differential association of intimate partner physical, sexual, psychological, and stalking violence and posttraumatic stress symptoms in a nationally representative sample of women. J Trauma Stress. 2004;17(5):413–21.
Wingood GM, DiClemente RJ. Rape among African American women: Sexual, psychological, and social correlates predisposing survivors to risk of STD/HIV. J Womens Health. 1998;7(1):77–84.
Kalichman SC, Williams EA, Cherry C, Belcher L, Nachimson D. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. J Womens Health. 1998;7(3):371–8.
Lang DL, Sales JM, Salazar LF, Hardin JW, DiClemente RJ, Wingood GM, et al. Rape victimization and high risk sexual behaviors: longitudinal study of African-American adolescent females. West J Emerg Med. 2011;12(3):333–42.
Downer G, Callwood G. Developing an effective HIV/AIDS response for women and girls in the US virgin islands. Womens Health Issues. 2011;21(6s):s283–6.
Hampton R, Oliver W, Magarian L. Domestic violence in the African American community: an analysis of social and structural factors. Violecnce Against Women. 2003;9(5):533–57.
Center for HIV Surveillance and Epidemiology. Baltimore city HIV/AIDS epidemiological profile, fourth quarter 2010. Infectious Disease and Environmental Health Administration, Maryland Department of Health and Mental Hygiene. 2010.
HIV surveillance report, communicable disease division STD/HIV/TB program, HIV surveillance unit, 2010 [Internet]; 2010. http://www.healthvi.com/assets/documents/2010/2010-hiv-surveillance%20report.pdf.
Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012;17(4):1–26. http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental.
HIV among African Americans [Internet].; 2012. http://www.cdc.gov/hiv/topics/aa/index.htm.
Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health (Larchmt). 2011;20(7):991–1006.
Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: A review. Int J Inj Contr Saf Promot 2008 12/01; 2012/03;15(4):221–31.
Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: Directions for future research and interventions. Soc Sci Med. 2000;50(4):459–78.
Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence. Trauma Violence Abus. 2007;8(2):178–98.
Campbell JC, Lucea MB, Stockman JK, Draughon JE. Forced sex and HIV risk in violent relationships. Am J Reprod Immunol. 2012;69(Suppl. 1):41–4.
Campbell JC, Soeken K. Women’s responses to battering over time: an analysis of change. J Interpers Violence. 1999;14:21–40.
Go V, Srikrishnan A, Parker C, Salter M, Green A, Sivaram S, et al. High prevalence of forced sex among non-brothel based, wine shop centered sex workers in Chennai India. AIDS Behav. 2011;15(1):163–71.
Campbell JC, Webster D, Glass N. The danger assessment: validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence. 2008;24:4653–74.
Hoffman S, O’Sullivan LF, Harrison A, Dolezal C, Monroe-Wise A. HIV risk behaviors and the context of sexual coercion in young adults’ sexual interactions: results from a diary study in rural South Africa. Sex Transm Dis. 2006;33(1):52–8.
Wingood GM, Seth P, DiClemente RJ, Robinson LS. Association of sexual abuse with incident high-risk human papillomavirus infection among young African-American women. Sex Transm Dis. 2009;36(12):784–6.
Josephs LL, Mazur Abel E. Investigating the relationship between intimate partner violence and HIV risk-propensity in Black/African-American women. J Fam Violence. 2009;24(4):221–9.
Sabri B, Bolyard R, Stockman JK, Lucea MB, Callwood GB, Coverston CR, et al. Intimate partner violence, depression, PTSD, and use of mental health resources among ethnically diverse black women. Soc Work Health Care. 2013;52(4):351–69.
Lucea MB, Stockman JK, Mana-Ay M, Bertrand D, Callwood GB, Coverston CR, et al. Factors influencing resource use by African American and African Caribbean women disclosing intimate partner violence. J Interpers Violence. 2013;28(8):1617–41.
Stockman JK, Lucea MB, Draughon JE, Sabri B, Anderson JC, Bertrand D, et al. Intimate partner violence and HIV risk factors among African-American and African-Caribbean women in clinic-based settings. AIDS Care. Sep 25 2012.
Neaigus A, Jenness SM, Hagan H, Murrill CS, Wendel T. Reciprocal sex partner concurrency and STDs among heterosexuals at high-risk of HIV infection. J Urban Health. 2013;90(5):902–14.
Noor SW, Ross MW, Lai D, Risser JM. Drug and sexual HIV risk behaviours related to knowledge of HIV serostatus among injection drug users in Houston. Texas Int J STD AIDS. 2014;25(2):89–95.
Raj A, Silverman J, Amaro H. Abused women report greater male partner risk and gender-based risk for HIV: findings from a community-based study with Hispanic women. AIDS Care. 2004;16(4):519–29.
Lary H, Maman S, Katebalila M, McCauley A, Mbwambo J. Exploring the association between HIV and violence: young people’s experiences with infidelity, violence and forced sex in Dar es Salaam Tanzania. Int Fam Plan Perspect. 2011;30(4):200–6.
Dunkle K, Jewkes R, Nduna M, Levin J, Jama N, Khuzwayo N, et al. Perpetration of partner violence and HIV risk behavior among young men in the rural eastern cape South Africa. AIDS. 2006;20(16):2107–14.
Hess K, Javanbakht M, Brown J, Weiss RE, Hsu P, Gorbach PM. Intimate partner violence and sexually transmitted infections among young adult women. Sex Transm Dis. 2012;39(5):366–71.
Grieb S, Davey-Rothwell M, Latkin C. Concurrent sexual partnerships among urban african american high-risk women with main sex partners. AIDS Behav. 2012;16(2):323–33.
Chan RL, Martin SL. Physical and sexual violence and subsequent contraception use among reproductive aged women. Contraception. 2009;80(3):276–81.
Littleton H, Breitkopf CR, Berenson A. Sexual and physical abuse history and adult sexual risk behaviors: Relationships among women and potential mediators. Child Abuse Negl. 2007;31(7):757–68.
Fuentes C. Pathways from interpersonal violence to sexually transmitted infections: a mixed-method study of diverse women. J Womens Health. 2008;17(10):1591–603.
Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. Morbidity and Mortality Weekly Report. 2010;59(RR-12):inclusive.
Maryland department of health and mental hygiene center for sexually transmitted infection prevention [Internet]. Baltimore, MD: Maryland Department of Health and Mental Hygiene; 2014 [updated 9 May 2014; cited 1 July 2014]. http://phpa.dhmh.maryland.gov/OIDPCS/CSTIP/SitePages/sti-data-statistics.aspx.
Sexually transmitted diseases surveillance [Internet]; 2010. http://www.cdc.gov/std/stats10/default.htm.
Acknowledgments
J.E.D. is now with the Department of Community Health Systems, University of California, San Francisco School of Nursing, San Francisco, CA.
Funding
This study was supported by the National Institutes of Health (NIMHD P20MD002286, Caribbean Exploratory Research Center, University of the Virgin Islands). J.E.D. was supported by NIMH (F31MH088850) and NINR (T32NR007081). M.B.L. is supported by NICHD (T32HD064428 and R01HD077891) and NIMHD (L60MD006272). J.K.S. is supported by NICHD (R01HD077891) NIDA (K01DA031593 and R25DA025571), NIMHD (L60MD003701) and NIMH (R25MH080664 and R25MH080665). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Draughon, J.E., Lucea, M.B., Campbell, J.C. et al. Impact of Intimate Partner Forced Sex on HIV Risk Factors in Physically Abused African American and African Caribbean Women. J Immigrant Minority Health 17, 1313–1321 (2015). https://doi.org/10.1007/s10903-014-0112-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-014-0112-x