Abstract
As policies legalizing adult cannabis use increase in the United States, understanding and characterizing the proportion of individuals consuming cannabis for medical and nonmedical purposes is important to inform targeted health education efforts. Data came from 7672 adults (> = 18 years) with past month cannabis use who responded to questions about reason for cannabis use on the 2018 Behavioral Risk Factor Surveillance System survey in 14 states. State and aggregated data were analyzed using weighted frequencies for descriptive analyses, and prevalence ratios were computed to identify demographic and substance use characteristics associated with medical only use or use for both medical and nonmedical reasons (vs. nonmedical use). Overall, 28.6% (95% CI: 26.7, 30.4) of adults who use cannabis reported using cannabis medically, 34.2% (95% CI: 32.3, 36.2) nonmedically, and 37.2% (95% CI: 35.2, 39.2) both medically and nonmedically. Characteristics associated with medical only use (compared with nonmedical only use) included being female; aged > 45 years; out of work, a homemaker, or unable to work; having daily or near daily cannabis use; having past month cigarette use; having no past month alcohol use; self-reporting poor health; and ever having been diagnosed with certain chronic diseases. Medical only use of cannabis is the least prevalent reason for use; use for both medical and nonmedical reasons is the most prevalent. Monitoring reasons for cannabis use can aid states in understanding differences between medical and nonmedical cannabis users, providing context to use patterns, and targeting health education messages to appropriate audiences.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As of April 2021, 36 U.S. states and the District of Columbia (DC) have approved comprehensive, publicly available medical cannabis (sometimes referred to as marijuana) programsFootnote 1; 17 of these states (Alaska, Arizona, California, Colorado, Illinois, Maine, Massachusetts, Michigan, Montana, Nevada, New Jersey, New Mexico, New York, Oregon, Vermont, Virginia, and Washington) have also approved the use and sale of cannabis to adults for nonmedical purposes (sometimes referred to as recreational use) [1].
Despite recent policy changes, the science is still emerging around the health effects of cannabis and cannabinoids. The cannabis plant has more than 100 individual cannabinoids or compounds [2]. Some of these compounds have been found to be effective in treating some medical conditions or symptoms, including certain types of chronic pain, chemotherapy-induced nausea and vomiting, rare seizure disorders like Dravet’s syndrome, and patient-reported spasticity from multiple sclerosis [3]. However, cannabis can also have potential negative health effects, including short-term impairment in learning, memory, and attention,impaired driving and risk for motor vehicle crashes; chronic bronchitis and increased respiratory symptoms (primarily due to smoked or inhaled cannabis); lower birth weight among babies born to individuals who used cannabis; and increased risk for the development of schizophrenia and other psychoses, cannabis use disorder, and other substance use disorders [3,4,5,6,7].
As policies legalizing adult cannabis use expand in states, gaining an understanding of the proportion of individuals consuming cannabis for medical and nonmedical purposes is particularly important, as public education efforts and messages about cannabis may need to differ between adult medical and nonmedical consumers. However, evolving state cannabis policies can make classifying medical cannabis use more challenging. National data collection systems like the National Survey on Drug Use and Health (NSDUH), an annual, nationally representative household survey funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), do not collect information on medical and nonmedical cannabis use, but have collected information on whether any or all past year marijuana use was recommended by a doctor [8]. A study used 2013–2014 data from this particular NSDUH survey question as a proxy for medical cannabis use and found that 0.8% of adults reported use only for medical reasons (i.e., reported that all use was recommended by a doctor), 11.6% reported use only for nonmedical reasons (i.e., reported that no use was recommended by a health care professional), and 0.5% reported use for both medical and nonmedical reasons (i.e., reported at least some use was recommended by a health care professional) [9]. A subsequent study using the same NSDUH question about use recommended by a health care professional found that reported cannabis use for medical reasons increased significantly in adults from 1.2% in 2013 to 1.6% in 2015 [10]. However, as states legalize broader use of and access to cannabis, medical and nonmedical reasons for use may be less tied to a medical recommendation and more tied to self-treatment, making indicators about receipt of a clinical recommendation for medical cannabis use an imprecise proxy.
State medical cannabis programs may authorize a broad range of medical uses, [11] and typically require at least one initial in-person visit with a clinician and/or a bona fide clinician/patient relationship to certify a medical need for cannabis [11]. In some states, clinicians are required to certify the dose, mode or method of use, and other details about the types of products approved for patient use [12,13,14]. As states legalize adult nonmedical cannabis use, medical programs continue to exist. However, medical and nonmedical cannabis marketplaces may be combined (as in the case of Alaska, California, and Washington, where there is a single marketplace) [15]. For adults seeking cannabis for medical purposes, purchasing through a state medical program instead of through the adult use marketplace may mean paying lower or no taxes (most states have no state-added ad valorem excise tax on medical cannabis products), and may allow for the purchase of greater quantities of product than can be obtained in the adult use marketplace [16]. However, there may be time and cost barriers associated with obtaining clinician certification to become a medical cannabis patient, and some adults may choose to forgo the process of becoming a patient in favor of accessing cannabis with fewer barriers through the adult use marketplace. Conversely, for states that do not have legal adult nonmedical use, some adults may access the medical cannabis program solely or primarily to gain access to cannabis products for nonmedical use.
This policy landscape complicates the validity of using questions about clinician recommendations for cannabis as a proxy for medical use on state or federal surveys. Assessing medical cannabis use based only on having a clinician recommendation for cannabis use may result in an inaccurate reporting of actual medical use versus nonmedical use. A more subjective, self-reported measure may be needed when collecting data from adults who use cannabis to understand their self-described reason for use. Such a measure was piloted in a 2014 consumer panel survey (Summer Styles) that was weighted to reflect the national population [17]. Data from that sample of adults aged 18 years and older suggested that in 2014, 10.5% of past month cannabis users reported use for only medical reasons, 53.4% reported use for nonmedical (recreational) reasons, and 36.1% reported using for both medical and nonmedical reasons [17]. More recent data on self-reported medical and nonmedical reasons for cannabis use have not been published in the scientific literature.
Accordingly, this study assessed data from a multi-state sample of adults who responded to a question about reason for cannabis use (i.e., medical only, nonmedical only, or both medical and nonmedical) on the Behavioral Risk Factor Surveillance System (BRFSS) optional marijuana module [18]. Characteristics associated with self-described medical only, nonmedical only, or combined medical and nonmedical cannabis use are also assessed to better characterize populations ascribing to each reason for use. These characterizations can aid in better targeting public health messaging, which may need to differ based on reasons for use.
Methods
Data Source and Sample
Data for this study came from a total of 109,075 participants aged 18 years and older in 14 states who responded to the questions on the optional cannabis module on the 2018 BRFSS; 7672 participants indicated past month cannabis use [18]. The BRFSS is a cross-sectional telephone (landline and cell phone) survey conducted annually by state health departments in all 50 U.S. states, the District of Columbia (DC), and U.S. territories, in collaboration with the Centers for Disease Control and Prevention [19]. The survey is administered to a disproportionate stratified sample of adults aged ≥ 18 years living in households [19]. The BRFSS survey consists of core questions (administered by all states, DC, and territories), optional modules (which states can elect to use), and state-added questions [18]. We analyzed questions included in an optional marijuana use module used by the following 14 states: California (CA), Florida (FL), Idaho (ID), Maryland (MD), Minnesota (MN), Montana (MT), New Hampshire (NH), North Dakota (ND), Ohio (OH), Oklahoma (OK), South Carolina (SC), Tennessee (TN), West Virginia (WV), and Wyoming (WY).
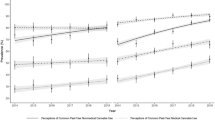
States varied in terms of the proportion of the overall weighted sample that they contributed to the multi-state sample (Fig. 1). All participants with complete data on the relevant measures were included in the sample. Response rates for BRFSS were calculated using the American Association of Public Health Opinion Research response rate formula (AAPOR 4) [20]. The median survey response rate for all states and DC was 53.3% for the landline sample and 43.4% for the cell phone sample [20]. Cooperation rates (the percentage of persons who completed interviews among all eligible persons who were contacted) in the 14 states ranged from 51.6% to 73.4% (median: 65.1%) for landline samples and 70.6% to 91.1% (median: 83.2%) for cell phone samples [20]. Additional information about the BRFSS survey design, data collection, and full-text questionnaires can be found at http://www.cdc.gov/brfss.
Prevalence of medical only use, nonmedical only use, and both medical and nonmedical use of cannabis among adults who use cannabis in 14 states, Behavioral Risk Factor Surveillance System, 2018. The 14 states included in this sample are: California (CA), Florida (FL), Idaho (ID), Maryland (MD), Minnesota (MN), Montana (MT), New Hampshire (NH), North Dakota (ND), Ohio (OH), Oklahoma (OK), South Carolina (SC), Tennessee (TN), West Virginia (WV), and Wyoming (WY)
Note that the 14 states included in this sample had a range of policies in place regarding the legalization of cannabis at the time of sampling (Table 1), with CA having both legal nonmedical adult cannabis use and medical use policies in place; FL, MD, MN, MT, NH, ND, and OH having policies in place legalizing medical cannabis use; and ID, SC, TN, WV and WY having either no policies in place legalizing cannabis, or policies legalizing only cannabidiol (CBD) or low-tetrahydrocannabinol (THC) products (Table 1). Voters in OK legalized medical cannabis in June 2018, during data collection [21]. Even in cases where states have the same macro-level policy (e.g., legalization of medical use), important regulatory differences exist from state to state (e.g., in terms of the number of retail licensees and distance between retailers, the types of available legal products, and the types of clinicians engaged in recommending and in some dispensing products), making comparisons across policies challenging [22].
Measures
Participants were asked about past 30-day cannabis use: During the past 30 days, on how many days did you use marijuana or cannabis? Those indicating use on 1–30 of the past 30 days were asked about their reason for use: “When you used marijuana or cannabis during the past 30 days, was it usually: (1) for medical reasons (like to treat or decrease symptoms of a health condition), (2) for nonmedical reasons (like to have fun), or (3) for both medical and nonmedical reasons,” and their mode or method of use: “During the past 30 days, which one of the following ways did you use marijuana the most often? Did you….smoke it, eat it, drink it, vaporize it, dab it, or use it in some other way?”[18].
Participants were also asked about past 30-day cigarette smoking, alcohol use and frequency, and whether they were ever told they had a number of different chronic diseases or medical conditions (e.g., diabetes, cancer, asthma, etc.). Sociodemographic variables were also asked, including: sex, age (18–24 years, 25–44 years, 45–64 years, 65 or more years), race (white, non-Hispanic [NH]; black, NH; Hispanic; other/multiracial, NH), education (less than high school graduate, high school graduate or GED, at least some college, college or more), employment (employed for wages, self-employed, out of work/homemaker, student, retired, unable to work), and health status (poor, fair to good, and very good to excellent).
Data Analysis
We extracted data from the landline and cell phone combined data samples. Data were weighted for the complex sampling design. One state, OK, used the optional module on one of two versions of their BRFSS survey; data were weighted for that version. Datasets were concatenated with one final weighting variable. To account for the complex data sampling design, analyses were conducted using SAS-callable SUDAAN, version 9.2 (RTI International, Research Triangle Park, N.C.)
We estimated weighted percentages and 95% confidence intervals (CIs) of cannabis use and the reported reasons for cannabis use (medical only, nonmedical only, and both medical and nonmedical) overall and by state. We also estimated weighted percentages and 95% CIs of the reasons for cannabis use across demographic, other substance use, and chronic disease characteristics. To compare reason for use categories by covariables, we used predicted marginals from bivariable logistic regression to generate prevalence ratios (PRs) and associated 95% CIs for (1) medical only use vs. nonmedical cannabis use and (2) both medical and nonmedical use v. nonmedical cannabis use. Multivariable models were not developed as our goal was to describe how prevalence of reasons for use vary by other characteristics in the population rather than to isolate an association between reason for use and a particular characteristic.
Results
Multi-state and Individual State Prevalence for Reported Reasons for Cannabis Use
Among the 14-state sample, the prevalence of all respondents reporting past month cannabis use was 11.0% (95% CI: 10.6, 11.5) (data not shown in table); prevalence varied by state from 6.9% (95% CI: 6.0, 8.0) (WV) to 14.9% (95% CI: 14.0, 15.9) (CA) (Table 1). Overall, 28.6% (95% CI: 26.7, 30.4) of respondents with past month cannabis use reported using cannabis for medical only reasons, 34.2% (95% CI: 32.3, 36.2) for nonmedical only reasons, and 37.2% (95% CI: 35.2, 39.2) for both medical and nonmedical reasons (Fig. 1). The prevalence of medical and/or nonmedical cannabis use varied across states. For medical only use, prevalence ranged from 19.4% (95% CI: 14.5, 25.6) in WY to 41.5% (95% CI: 36.1, 47.1) in MT; for nonmedical only use, prevalence ranged from 20.5% (95% CI: 13.8, 29.4) in OK to 44.3% (95% CI: 40.8, 47.8) in MN; and for both medical and nonmedical use, prevalence ranged from 29.6% (95% CI: 24.4, 35.4) in SC to 43.2% (95% CI: 35.9, 50.8) in WY (Table 1).
Among states in the sample with policies in place at the time of data collection legalizing medical use, use for medical only reasons ranged from 20.4% (95% CI: 17.8, 23.3) (MN) to 41.5% (95% CI: 36.1, 47.1) (MT); use for nonmedical only reasons ranged from 28.4% (95% CI: 23.5, 33.8) (MT) to 44.3% (95% CI: 40.8, 47.8) (MN); and use for both medical and nonmedical reasons ranged from 30.2% (95% CI: 25.2,35.7) (MT) to 41.6% (95% CI: 32.5, 51.3) (ND) (Table 1). Among states in the sample with no policies in place at the time of data collection legalizing medical or nonmedical use, use for medical only reasons ranged from 19.4% (95% CI: 14.5, 25.6) (WY) to 39.4% (95% CI: 32.3, 46.9) (WV); use for nonmedical only reasons ranged from 24.1% (95% CI: 18.2, 31.2) (WV) to 43.5% (37.7, 49.5) (SC); and use for both medical and nonmedical reasons ranged from 29.6% (95% CI: 24.4, 35.4) (SC) to 38.7% (95% CI: 30.9, 47.2) (TN). California was the only state in the sample with a policy in place at the time of data collection legalizing adult nonmedical use; among adults using cannabis, the prevalence of medical only use in CA was 28.5% (95% CI: 25.5, 31.7); nonmedical only use was 31.9% (95% CI: 28.8, 35.2), and use for both medical and nonmedical reasons was 39.6% (95% CI: 36.4, 43.0).
Characteristics Associated with Different Reasons for Cannabis Use
Characteristics more prevalent among adults who reported medical only cannabis use compared to those who reported nonmedical only use included older age (PR for 45–64 years: 1.2, 95% CI: 1.1, 1.4; PR for 65 years and older: 2.3, 95% CI: 1.7, 3.1); having less than a high school education (PR 1.4, 95% CI: 1.1, 1.9); being out of work or a homemaker (PR 1.9, 95% CI: 1.4, 2.6), retired (PR 1.9, 95% CI: 1.3, 2.6), or unable to work (PR 6.2, 95% CI: 4.3, 9.0); reporting 20 or more days of cannabis use in the past month (PR 1.9, 95% CI: 1.7, 2.2); eating cannabis (PR 1.4, 95% CI: 1.1, 1.9) or drinking or reporting another form of cannabis use (PR: 11.2, 95% CI: 5.3, 23.8); past month cigarette use (PR 1.3, 95% CI: 1.1, 1.5); no past month alcohol use (PR 2.0, 95% CI: 1.7, 2.4); and self-reported poor health (PR 1.3, 95% CI 1.2, 1.5) or fair to good health (PR 5.1, 95% CI: 3.0, 8.8) (Table 2). All health conditions assessed were more common among those who reported medical only use compared to those who reported nonmedical only use. Those who reported medical only use were less likely to be male compared to those who reported nonmedical only use.
Characteristics more prevalent among adults who reported both medical and nonmedical cannabis use compared to those who reported nonmedical only use included being out of work or a homemaker (PR 1.6, 95% CI: 1.2, 2.1) or unable to work (PR 3.0, 95% CI: 2.0, 4.5); using cannabis on 20 or more of the past 30 days (PR 2.1, 95% CI: 1.8, 2.4); dabbing cannabis (PR 2.3, 95% CI: 1.1, 5.0); and self-reporting fair to good health (PR 1.3, 95% CI: 1.2, 1.4). Health conditions more likely among those who reported both medical and nonmedical cannabis use compared to those who reported medical only use included asthma (PR 1.3, 95% CI: 1.1, 1.6), Chronic Obstructive Pulmonary Disease (COPD) (PR 2.1, 95% CI: 1.5, 3.0), heart attack (PR 1.8, 95% CI: 1.1, 2.8), stroke (PR 2.0, 95% CI: 1.1, 3.5), arthritis (PR 2.1, 95% CI: 1.6, 2.6), and depressive disorder (PR 1.7, 95% CI 1.4, 2.0).
Discussion
This is among the first studies to assess self-reported medical and nonmedical use of cannabis in a multi-state adult sample. Important findings include that just under one-third of adults with past month cannabis use reported using cannabis for medical only reasons, while just over one-third reported using for nonmedical only reasons, and the largest proportion – nearly 4 in ten adult cannabis users – reported using for both medical and nonmedical reasons. The prevalence of medical only use is markedly different from a 2014 consumer panel survey of U.S. adults that found just over 10% reported using for medical only reasons [17]. This may be due in part major differences in the two data sources – though this was a 14-state sample, BRFSS is nationally representative, while the consumer panel survey was weighted to the national population (but not nationally representative). Differences could also be due to policy changes that have occurred between 2014 and 2018. For example, six states included in the sample for this study legalized comprehensive medical use between 2014 and 2018. However, research has consistently found that nonmedical use is prevalent among people with medical cannabis use [17, 23, 24]. This phenomenon may be a result of individuals either using cannabis nonmedically and experiencing later medical benefits, or the converse. Furthermore, it is possible that a number of specific reasons for use (e.g., to fit in, to reduce stress, to have fun) may be classified by individuals as both medical and nonmedical reasons for use. More research is warranted to understand how cannabis users conceptualize their use in different situations and settings.
Socio-demographic, substance use, and chronic disease-related characteristics of medical only cannabis use differ from nonmedical only use. This study found that those who reported cannabis use for medical only reasons were less likely to be male compared to those who reported cannabis use for nonmedical only reasons, and no differences existed based on race/ethnicity between individuals using cannabis for medical and nonmedical reasons. Lin et al. [25] had similar findings in their analysis of 2013 NSDUH data, using clinician recommendation for cannabis as a proxy for medical use [25]. The finding that those using cannabis for medical only reasons were more likely to be out of work, retired, or unable to work compared with those using for only nonmedical reasons may be related to having a medical condition that prevents people who use cannabis for medical purposes from work, or that makes it difficult for them to find or keep work.
Findings from this study indicate that medical only users are more likely to consume cannabis daily or almost daily. Other studies have documented similar findings – both here in the U.S. and in Canada [24, 25]. More frequent use patterns among medical only versus nonmedical only users may be related to treatment and/or tolerance [24]. The finding that medical only users are more likely than nonmedical only users to consume cannabis in edibles, drinks, or other forms (e.g., pills, tinctures, capsules, etc.) is expected, given that medical cannabis users may try to avoid smoked or combusted forms due to the known health harms of smoking in general. Interestingly, the prevalence of vaping cannabis is similar across groups. This may be due to preference, or it could be related to aspects of some policies that prohibit smokable or edible cannabis and ultimately leave vaping as the primary legal mode of medical cannabis consumption. For example, a number of state medical cannabis programs ban either smokable or edible cannabis. In some cases – such as in MN – both smokable and edible products are banned [26], leaving vaping as a primary legal mode of medical cannabis consumption.
In this study, those consuming cannabis for medical only reasons were more likely than nonmedical only users to report past month use of cigarettes. Other studies have found higher levels of nicotine dependence in medical cannabis consumers [25]. More research is needed to better understand why individuals seeking to use cannabis for medical reasons were more likely to use cigarettes. It may be that cannabis is an appealing “medical” treatment for those who smoke cigarettes, due to a similar mode of consumption (e.g., smoked or vaped) and a general overlap in populations using both substances [17, 27,28,29,30]. Individuals who report using cannabis medically may also be self-treating with nicotine, a theory that has been hypothesized in the scientific literature – particularly related to behavioral health conditions [31,32,33]. Or, individuals may be using cannabis medically for conditions that are smoking-related (e.g., cancer). Nicotine is highly addictive and can be challenging to quit successfully [34, 35]. Importantly, while the health effects of cannabis are still emerging, the health harms of tobacco use and of smoking in general are well established [36] making it concerning that some individuals seeking a “medicine” are also smoking cigarettes.
Perhaps predictably, all health conditions assessed as part of BRFSS were more common among respondents using cannabis medically compared to those who reported nonmedical only use. Some of the reported chronic conditions have scientific evidence supporting the potential use of cannabis as treatment (e.g., for symptoms from chemotherapy used in cancer) [3]. However, other reported chronic conditions may be worsened by cannabis use, including COPD and cardiovascular disease [3, 6, 37]. Participants may also have been using cannabis to treat another co-morbidity not assessed as part of the BRFSS survey instrument. More research is warranted to better understand how individuals with chronic conditions make choices about using cannabis as a possible treatment, whether they are using cannabis to treat other conditions, and whether they understand potential risks that can come with cannabis use, given their particular medical conditions.
State variation exists in the prevalence of reasons for use among past month cannabis consumers but on qualitative review, does not appear to necessarily align with state cannabis policy. For example, MN has had a restrictive medical cannabis program that limits the types of available products and the points of access in the marketplace [26]. Still, in 2018, nearly 80% of adults sampled from MN who reported past month cannabis use reported consuming cannabis in part or entirely for nonmedical reasons. In WV, no medical cannabis program existed at the time of survey, yet more than 75% of adults who reported past month cannabis use reported consuming cannabis in part or entirely for medical reasons.
The following limitations should be considered when interpreting data from this study. First, data are self-reported and may be subject to social desirability bias and recall error. Second, households without telephones (landline or mobile) are not contacted for the survey, and the survey is only conducted in English and Spanish, which can lead to selection bias. However, these sources of bias do not change from year to year, making BRFSS a valuable surveillance system to assess future trends in mode of cannabis use. Third, data were collected from 14 states, since the marijuana module on BRFSS remains an optional module that states have to elect to offer. Finally, as noted, assessing how state cannabis policy affects cannabis mode of use was out of the scope of this study, and would require detailed policy databases to merge with BRFSS data.
Despite these limitations, these data suggest that about three in ten adults who report past month cannabis use report using cannabis for medical only reasons, and that these individuals differ from those using cannabis for nonmedical only reasons across a number of social demographics, substance use, and health-related variables. Public health promotion messages targeting those who use cannabis medically may need to differ from those focused on primarily nonmedical consumers – both because of the apparent differences in these populations, as well as nuances related to medical use of a substance that – like a number of other medicines – can also pose potential harms [38]. More research is also warranted to better understand whether individuals using cannabis medically are using it in place of or in addition to FDA-approved medications and impacts that decisions to use cannabis in place of FDA-approved medications may have on medical outcomes. Ongoing data monitoring assessing reasons for cannabis use can assist states and communities in better understanding medical and nonmedical populations of cannabis users to improve message targeting and to provide context to certain patterns of cannabis use.
Data Availability
Data used in this study are available from: https://www.cdc.gov/brfss/annual_data/annual_data.htm.
Notes
A number of additional states have medical cannabis programs that allow for use only of CBD or low-THC products, but not a broader range of cannabis products.
References
National Conference of State Legislatures. (2020). State Marijuana Laws. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx
Caulkins, J. P., Hawken, A., Kilmer, B., & Kleinman, M. A. (2012). Marijuana legalization: What everyone needs to know. Oxford University Press.
National Academies of Sciences Engineering and Medicine. (2017). The health effects of cannabis and cannabinoids: Current state of evidence and recommendations for research.
Colorado Department of Public Health & Environment. (2016). Monitoring health concerns related to Marijuana in Colorado: 2016.
Colorado Department of Public Health and Environment. (2018). Monitoring health concerns related to Marijuana in Colorado: 2018. https://drive.google.com/drive/u/0/folders/1HEDVleZsVFml12FI7Om95QZ3t4c2RrlA
Colorado Department of Public Health and Environment. (2021). Monitoring health concerns related to Marijuana in Colorado: 2020. https://drive.google.com/drive/folders/1H9g7iwIIW-NMdDCgmtdgk8zvjwWcQGqd
Volkow, N. D., Baler, R. D., Compton, W. M., & Weiss, S. R. (2014). Adverse health effects of marijuana use. New England Journal of Medicine, 370(23), 2219–2227. https://doi.org/10.1056/NEJMra1402309
Substance Abuse and Mental Health Services Administration. (2020, September). National Survey on Drug Use and Health: 2019 NSDUH Detailed Tables. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables
Compton, W. M., Han, B., Hughes, A., Jones, C. M., & Blanco, C. (2017). Use of Marijuana for medical purposes among adults in the United States. JAMA. https://doi.org/10.1001/jama.2016.18900
Han, B., Compton, W. M., Blanco, C., & Jones, C. M. (2018). Trends in and correlates of medical marijuana use among adults in the United States. Drug and Alcohol Dependence. https://doi.org/10.1016/j.drugalcdep.2018.01.022
Philpot, L. M., Ebbert, J. O., & Hurt, R. T. (2019). A survey of the attitudes, beliefs and knowledge about medical cannabis among primary care providers. BMC Family Practice, 20(1), 17. https://doi.org/10.1186/s12875-019-0906-y
Public Act 12–55: An Act Concerning the Palliative Use of Marijuana, (2013). https://portal.ct.gov/DCP/Medical-Marijuana-Program/Law-and-Regulations
Section 1004.2 - Practitioner issuance of certification, (2020). https://regs.health.ny.gov/content/section-10042-practitioner-issuance-certification
Office of Medical Marijuana Use Florida Department of Health. (2020). Creating a Certification and Orders. https://s27415.pcdn.co/wp-content/uploads/_documents/Instructional_Guides/QP/Create-Certification-Orders_v4.pdf
Washington State Liquor Control Board. (2014). Washington State Register 14-10-044 Amendatory Section, filed 4.30.14, effective 5.31.14. https://lcb.wa.gov/publications/rules/OTS-6471_1Final.pdf
Leafly. (2021). Medical marijuna laws in the United States. https://www.leafly.com/learn/legalization/medical-states
Schauer, G. L., King, B. A., Bunnell, R. E., Promoff, G., & McAfee, T. A. (2016). Toking, vaping, and eating for health or fun: Marijuana use patterns in adults, US, 2014. American Journal of Preventive Medicine. https://doi.org/10.1016/j.amepre.2015.05.027
Centers for Disease Control and Prevention. (2018). 2018 BRFSS Questionnaire. https://www.cdc.gov/brfss/questionnaires/pdf-ques/2018_BRFSS_English_Questionnaire-508.pdf
Centers for Disease Control and Prevention. (2019b, July 26). The behavioral risk factor surveillance system (BRFSS) overview: 2018. https://www.cdc.gov/brfss/annual_data/2018/pdf/overview-2018-508.pdf
Centers for Disease Control and Prevention. (2019a). Behavioral risk factor surveillance system: 2018 summary data quality report. https://www.cdc.gov/brfss/annual_data/2018/pdf/2018-sdqr-508.pdf
Ballotpedia. (2018, June). Oklahoma State Question 788, Medical Marijuana Legalization Intitiative. https://ballotpedia.org/Oklahoma_State_Question_788,_Medical_Marijuana_Legalization_Initiative_(June_2018)
Pacula, R. L., Powell, D., Heaton, P., & Sevigny, E. L. (2015). Assessing the effects of medical marijuana laws on marijuana use: The devil is in the details. Journal of Policy Analysis and Management, 34(1), 7–31.
Morean, M. E., & Lederman, I. R. (2019). Prevalence and correlates of medical cannabis patients’ use of cannabis for recreational purposes. Addictive Behaviors. https://doi.org/10.1016/j.addbeh.2019.02.003
Turna, J., Balodis, I., Munn, C., van Ameringen, M., Busse, J., & MacKillop, J. (2020). Overlapping patterns of recreational and medical cannabis use in a large community sample of cannabis users. Comprehensive Psychiatry. https://doi.org/10.1016/j.comppsych.2020.152188
Lin, L. A., Ilgen, M. A., Jannausch, M., & Bohnert, K. M. (2016). Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addictive Behaviors. https://doi.org/10.1016/j.addbeh.2016.05.015
Chapter 311 - S.F. No.2470, (2014). https://www.revisor.mn.gov/laws/2014/0/311/ss
Schauer, G. L., Berg, C. J., Kegler, M. C., Donovan, D. M., & Windle, M. (2016). Differences in tobacco product use among past month adult marijuana users and nonusers: findings from the 2003–2012 national survey on drug use and health. Nicotine & Tobacco Research, 18(3), 281–288. https://doi.org/10.1093/ntr/ntv093
Schauer, G. L., Hall, C. D., Berg, C. J., Donovan, D. M., Windle, M., & Kegler, M. C. (2016). Differences in the relationship of marijuana and tobacco by frequency of use: A qualitative study with adults aged 18–34 years. Psychology of Addictive Behaviors. https://doi.org/10.1037/adb0000172
Singh, T., Kennedy, S. M., Sharapova, S. S., Schauer, G. L., & Rolle, I. V. (2016). Modes of ever marijuana use among adult tobacco users and non-tobacco users—Styles 2014. Journal of Substance Use. https://doi.org/10.3109/14659891.2015.1122100
Trivers, K. F., Gentzke, A. S., Phillips, E., Tynan, M., Marynak, K. L., & Schauer, G. L. (2019). Substances used in electronic vapor products among adults in the United States, 2017. Addictive Behaviors Reports. https://doi.org/10.1016/j.abrep.2019.100222
Baker, T. B., Piper, M. E., McCarthy, D. E., Majeskie, M. R., & Fiore, M. C. (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. https://doi.org/10.1037/0033-295X.111.1.33
Leonard, S., Mexal, S., & Freedman, R. (2007). Genetics of Smoking and Schizophrenia. Journal of Dual Diagnosis, 3(3–4). https://doi.org/10.1300/J374v03n03_05
Prochaska, J. J., Das, S., & Young-Wolff, K. C. (2017). Smoking, mental illness, and public health. Annual Review of Public Health. https://doi.org/10.1146/annurev-publhealth-031816-044618
U.S. Department of Health and Human Services. (1988). The Health Consequences of Smoking: Nicotine Addiction. A Report of the Surgeon General (C. for D. C. and Prevention, Ed.). U.S. Department of Health and Human Services.
U.S. Department of Health and Human Services Office of the Surgeon General. (2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health.
U.S. Department of Health and Human Services. (2014). The health consequences of smoking -- 50 years of progress. A report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf
Wang, X., Derakhshandeh, R., Liu, J., Narayan, S., Nabavizadeh, P., Le, S., Danforth, O., Pinnamaneni, K., Rodriguez, H., Luu, E., Sievers, R., Schick, S., Glantz, S., & Springer, M. (2016). One minute of Marijuana secondhand smoke exposure substantially impairs vascular endothelial function. Journal of the American Heart Association. https://doi.org/10.1161/JAHA.116.003858
Dowell, D., Haegerich, T. M., & Chou, R. (2016). CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. https://doi.org/10.1001/jama.2016.1464
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
GLS conceptualized the study, conducted the data analyses, and drafted the manuscript. BH and DRR reviewed the data analyses, discussed the data findings and implications, and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The Authors report no conflict of interest.
Ethical Approval
This study used deidentified publicly available data and did not require any ethics approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schauer, G.L., Roehler, D.R. & Hoots, B.E. Self-Reported Medical and Nonmedical Cannabis Use: Results from the 2018 Behavioral Risk Factor Surveillance System in 14 States. J Community Health 47, 641–649 (2022). https://doi.org/10.1007/s10900-021-01049-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-021-01049-1