Abstract
Among rural and underserved areas, existing disparities are very well studied, but current perceptions of HPV vaccination among parents are unknown. This study was designed using a survey administered to parents of children eligible for the HPV vaccine at community events throughout Central and Northern Michigan. These data suggest that the most important factor leading to successful vaccination is a conversation with a PCP. However, when the geographic location of these parents is considered, non-metropolitan parents were more concerned with the underlying safety and efficacy with the vaccine. This underscores the importance of tailoring a conversation with parents to meet their needs and concerns to lead to highest vaccination rates, and ultimately prevent HPV-related cervical cancers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nearly all cases of cervical, penile, and anal cancer are the result of Human Papillomavirus (HPV) infection [1]. Despite this fact, fewer than 33% of girls and 20% of boys in Michigan have completed the vaccine series [2]. As of 2016, all National Cancer Institute (NCI) designated cancer centers are encouraging parents and health care practitioners to improve vaccination rates to decrease incidence of preventable HPV-related cancers. Two vaccines (Gardasil 9 and Gardasil) in a two-dose series given 6 months apart during middle school may ensure that “our nation’s children don’t grow up to become cancer patients” [1].
These vaccines have very high efficacy rates, and the FDA recently announced approval one of the HPV vaccines up to 45 years of age [3]. Certain strains of HPV are responsible for up to 80% of all cases of cervical, penile, anal, and increasingly responsible for oropharyngeal and laryngeal cancers [4]. Non-oncogenic strains of HPV lead to genital warts (condyloma acuminata) and warts of the hands (verrucae vulgaris) and vocal cords (laryngeal papillomatosis). An estimated one in four people will become infected with HPV at some point in their lives [5], and up to 90% of HPV infections are asymptomatic [6], which facilitates spread of the infection and can allow undetected infection to persist once exposed. Over 38,000 new cases of cancer are diagnosed annually in areas of the body that can be infected with HPV.
While cervical cancer can be detected by preventative screenings (Pap smear), not all women have access to these screenings. Additionally, screening methods do not exist for other cancers that can be caused by HPV, including those that affect men who are vaccinated at a far lower rate than women. HPV is the leading cause of penile and anal cancer in addition to cervical cancer, causes more than half a million cases of cancer each year [7], is spread by multiple methods of sexual contact, cannot be prevented by condom use, does not have a cure, and often does not show symptoms [8]. This presents a serious risk of cancer to all individuals regardless of sex or sexual orientation. In addition to cancer, HPV infection sequelae, including infertility and condyloma accuminata [9], can yield severely life-altering reproductive health effects.
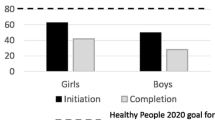
HPV vaccination was first introduced in 2006, but uptake has been slow in Michigan. While the rate of HPV vaccination initiation (≥ 1 dose) in Michigan (66%) is above to the national average (57%), completion of the vaccine series in Michigan teens lags behind national averages, and vaccination rates for both Michigan and the nation are significantly below the CDC Healthy People 2020 campaign targets [10]. Of note, vaccination initiation rates in our study population were 50% which is below both the reported Michigan and national averages. Limitations regarding the representativeness of our study population are discussed later. Correlations have been observed between vaccine uptake and cervical cancer incidence and mortality. In a recent study comparing HPV vaccination rates with cervical cancer mortality, Michigan ranked in the bottom half of the nation in vaccinations and was above average for cervical cancer mortality [11]. Despite this, there is data to suggest a reduction in cervical cancer since the advent of the HPV vaccine. In the 12 years since the first HPV vaccination became available, the incidence of precancerous Pap smear findings consistent with the development of cervical cancer has declined by 56% [12, 13]. The data clearly shows that HPV vaccination is a highly effective form of cancer prevention, but a vaccine’s efficacy is only as strong as the size of the cohort receiving it.
Methods
Participants and Survey Setting
This cross-sectional study utilized community events such as health fairs, craft fairs, and sporting events which allowed a targeted sample of the Michigan population to be surveyed regarding their perceptions towards HPV vaccination. Inclusion criteria were being the parent or primary guardian of at least one child aged 11–18. All survey participants were provided and signed an informed consent prior to the surveys. No underage minors (< 18 years of age) were surveyed and participated in the study. Surveys and educational material were provided by CITI trained students of CMU College of Medicine Community Health Research Initiative. Metropolitan and non-metropolitan areas are defined using counties of residence. “Metropolitan” refers to counties in areas of 250,000 to 1 million residents. “Non-metropolitan” refers to urban populations of 20,000 or more and that are adjacent to metro areas [14].
Surveys and Education
An anonymous nine questions survey was designed from prior studies from this research group to capture current perceptions of the caregiver’s knowledge and understanding of HPV and potential barriers in receiving the vaccine. Additional demographic data was also captured in the survey. The surveys were conducted in English, and a CITI trained team member was present to address any questions which arose. A consent form was included as the cover page and was removed from the survey to protect anonymity. All participants participated voluntarily and were then provided brief education regarding the HPV issues addressed in the survey.
Data Analysis
Statistical analysis was done using the SPSS Statistics version 25.0 (IBM, Armonk, New York). Descriptive statistics were provided including mean (standard deviation) for continuous variables, and count (%) for categorical variables. Logistic regressions were computed to examine the association of demographic variables and two outcome variables: vaccination uptake and dichotomous items indicating knowledge of HPV. All of the analytical results were considered to be significant when p-values were ≤ 0.05.
Ethical Approval
The Central Michigan University and Central Michigan University College of Medicine Institutional Review Board provided ethical guidance, approval, and oversight in the design and data gathering of this project to ensure participant anonymity. Approval was gathered in writing from each regional site where surveys were administered.
Results
Sample
A total of 112 primary caregivers were surveyed throughout the Central Michigan and Saginaw Valley region, with an average age of 45.9 years. A majority (77%) of those surveyed were female. Further descriptions of the sample surveyed can be found in Table 1. The sample was nearly split equally with 49% of those surveyed having at least one child who had received at least one dose of the HPV vaccine. The sample overall represented a highly educated and affluent population; 57.8% of the study participants reported receiving a bachelor’s degree or higher, and 51% identified being in the highest income bracket on the survey scale. According to most recent Census data, Michigan’s population is 78.9% white, 50.9% female, and the average household earns $52,668 annually; 28.9% of Michigan residents have attained a bachelor’s degree or higher [15].
Conversation with PCP Regarding HPV Vaccination
The most significant influencing factors on vaccine uptake and parental knowledge of HPV differed among parents based on their metropolitan versus non-metropolitan residential status as listed in Table 2. In metropolitan subjects, having a conversation with their PCP regarding HPV vaccination yielded an odds ratio (OR) of 8.33 that their child would be vaccinated, meaning parents who had this conversation were 8.33 times more likely vaccinate. Among the entire sample, the OR was 7.37. Among the non-metropolitan parents, their knowledge of HPV being a sexually transmitted disease yielded an OR of 19.0, almost three-fold increase in the overall sample OR of 6.64.
Parents Beliefs Regarding HPV Vaccination
Table 3 indicated that in non-metropolitan area parents were 6.46 times more likely to have vaccinated their child against HPV if they reported a belief that vaccines are safe and effective at reducing disease, when compared to parents who doubted the safety and efficacy of vaccination.
Racial Disparities and HPV Vaccination
While the survey sample was 86% white, among the metropolitan parents, white parents had an OR of 4.61 as compared to non-white parents with regard to knowing HPV is transmitted sexually as listed in Table 4.
Parental Education Level Impact on HPV Vaccination
Education of the survey respondents ranged from high school graduates to doctoral degrees. The largest subset of the sample (31.2%) were college graduates. Parents with higher levels of education had greater knowledge of the HPV vaccine as indicated in Table 5. Amongst all parents, at each incremental increase in degrees obtained, there was a 50% increase in the odds of knowing HPV is sexually transmitted. This relationship was even more notable when comparing geographic residences of the respondents. Among metropolitan area parents, at each incremental increase in education there was a 61% increase in the odds of knowing how HPV is transmitted. For non-metropolitan area parents the impact of education is even more dramatic; each incremental increase in education will have an expected 908% increase in the odds of knowing that HPV infection can resolve without treatment.
Views on the HPV Vaccine
Discussion
This study was designed to better understand the motivations and factors that lead to successful initiation of the HPV vaccine among parents of eligible children throughout Central and Northern Michigan. This study revealed that within this sample, multiple subgroups are influenced by unique factors that drive vaccine uptake and basic knowledge of HPV. Providing effective parental education in different regions of Michigan demands specific considerations from the medical community.
All Parents
The most significant factor driving vaccine uptake in all surveyed parents was having a conversation with their primary care provider (PCP) regarding the HPV vaccine. Parents reporting a conversation about the HPV vaccine with their PCP exhibited a 7.37 OR that their child had initiated the HPV vaccine series. When analyzing parental knowledge of HPV, parents who had a conversation with their PCP were 2.57 times more likely to know that HPV can cause cervical cancer, and 6.64 times more likely to know HPV can be transmitted sexually. This suggests that such a conversation yields both improved knowledge of HPV and increased vaccination rates.
Metropolitan Area Parents
Consistent with the overall sample, responses from parents residing in metropolitan areas demonstrated a positive association between HPV vaccination rates and knowledge of the virus were with a conversation with their PCP regarding the vaccine. However, among these metropolitan parents, there was an even high OR at 8.33, as compared to the overall sample, suggesting this conversation bears even greater significance on vaccine uptake in this community.
Ethnicity and education level were also related to HPV knowledge. White participants were 4.61 times more likely to know HPV can be transmitted sexually when compared to non-white participants in the metropolitan area parents specifically. Parents reporting higher education levels are more likely to know that HPV can be transmitted sexually; each additional level of education on the survey scale is correlated with a 61% increase in the odds of knowing the route of HPV transmission.
Non-Metropolitan Area Parents
When examining responses from individuals living in non-metropolitan areas, a conversation with the PCP was no longer the most significant factor affecting HPV vaccination; in these communities it was outpaced by the impact of parental belief that vaccines are safe and effective. Parents were 6.46 times more likely to have vaccinated their child against HPV if they reported a belief that vaccines are safe and effective at reducing disease, when compared to parents who doubted the safety and efficacy of vaccination. This leads to the baseline level of confidence and understanding of the medical system. A conversation regarding HPV is useless, unless there is a basic confidence in the vaccine safety and ability to prevent disease.
No other variables, including whether or not a PCP had a conversation with them about HPV vaccination, were found to have a significant effect on HPV vaccination status for children in non-metropolitan areas.
Although a conversation with their child’s doctor was no longer a main determinant of vaccine uptake in non-metropolitan areas, this conversation continued to impact basic knowledge of HPV, an even higher OR than in the metropolitan area communities. This conversation leads to these parents being 19 times more likely to know that HPV can be transmitted sexually.
Finally, education level still carried a significant influence on baseline HPV knowledge. Parents with a higher education level were more likely to know that HPV infection can resolve on its own without treatment; each additional level of education on the survey scale is correlated with a 908% increase in the odds of knowing that many HPV infections are self-resolving.
Strengths and Limitations
The impact of this study is strengthened by this project’s commitment to not only collect data but provide education in the process. This required surveys to be administered in-person, which limited the settings in which the study took place. Study participants were therefore limited to parents who chose to attend these community events, restricting the population to those who are financially stable and active within their community. Further, these data may be influenced by the relatively self-selecting nature of subject participants. It cannot be avoided that parents who had already vaccinated their children may be more likely to engage study administrators in conversations about HPV and would therefore be more willing to fill out surveys on the topic. Overall, this sample reflected a largely white, female, affluent, and educated population. Future studies could validate how representative our conclusions are of the general Michigan population by comparing results from in-person and remote access surveys as well as a more representative sample of the areas of interest.
Conclusions
Widening disparities in access to healthcare between urban and rural communities in the context of a continually evolving healthcare landscape have been subject to much investigation in recent years [16] While these disparities are becoming more clear, little research has investigated the influence of patient perception on their access and utilization of care. This study was designed to investigate perceptions among parents of eligible children with regards to HPV vaccination throughout Central and Northern Michigan. While increasing access to preventative healthcare is vital for HPV vaccination, our study revealed that a conversation with a PCP regarding the HPV vaccine is one of the strongest factors that leads to initiation of the series of vaccinations in addition to improved knowledge regarding HPV. The impact of this conversation is further nuanced by parents’ ethnicity, education level, and belief that vaccines are safe and effective. While a conversation regarding HPV vaccination and basic education about HPV infection is required for vaccine literacy and uptake, these data suggest this conversation must be tailored to the context of each individual family. Parents from non-metropolitan areas were more concerned with the vaccine safety and efficacy, suggesting addressing these concerns as opposed to a flat recommendation is a key in successful vaccination. However, vaccine uptake from parents in metropolitan areas was more significantly affected by education level and ethnicity. Regardless of sub-population, a conversation with the PCP led to positive outcomes in all participants with regard to vaccine literacy or uptake. Understanding these motivations can lead to more efficient and effective office visits among PCP throughout underserved areas and lead to improved health outcomes and can help reduce the incidence of preventable HPV-related cancers.
References
National Cancer Institutes. (2017). NCI-designated Cancer Centers Endorse Updated HPV Vaccination Recommendations. Bethesda, MD. National Institutes of Health. Retrived January 24, 2017 from https://cancer.osu.edu/~/media/files/shared/press-releases/cancer/2017/hpvconsensusstatement-jan2017.pdf?la=en.
Michigan Department of Health and Human Services (2017). Michigan HPV vaccination snapshot: Pharmacies. [Internet] Lansing, MI. Retrived January 24, 2017 from http://www.michigan.gov/documents/mdhhs/HPV_Snapshot_Pharmacy_512272_7.pdf.
US Food & Drug Administration. US department of Health and Human Services (2018). FDA news release: FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old. [Internet] Silver Spring, MD. Retrieved December 12, 2018 from https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm622715.htm.
Centers for Disease Control and Prevention. (2017). HPV and cancer. [Internet] Atlanta, GA. Retrieved January 24, 2017 from https://www.cdc.gov/cancer/hpv/statistics/cases.htm.
Centers for Disease Control and Prevention. (2017). Human papillomavirus (HPV): The link between HPV and cancer. Atlanta, GA. December 16, 2016. Retrieved January 24, 2017 from https://www.cdc.gov/hpv/parents/cancer.html.
Bosch, et al. (2002). The causal relation between human papillomavirus and cervical cancer. Journal of Clinical Pathology, 55, 244–265.
Hariri, et al. (2017). Chapter 5: Human papillomavirus (HPV). Manual for the surveillance of vaccine-preventable diseases. [Internet] Atlanta, GA. Centers for disease control and prevention. Retrieved January 24, 2017 from https://www.cdc.gov/vaccines/pubs/surv-manual/chpt05-hpv.html#f11.
Centers for Disease Control and Prevention. (2017) Human Papillomavirus (HPV) Genital HPV Infection—Fact Sheet. [Internet] Atlanta, GA. Retrieved January 24, 2017 from https://www.cdc.gov/std/hpv/stdfact-hpv.htm.
Souho, T., Benlemlih, M., & Bennani, B. (2015). Human papillomavirus infection and fertility alteration: A systematic review. PLoS ONE, 10(5), e0126936.
Michigan Department of Health and Human Services. (2014) Human Papillomavirus (HPV) Vaccination Report: Michigan. [Internet] Lansing, MI. Retrieved January 24, 2017 from https://www.michigan.gov/documents/mdch/MichiganHPVReport_479144_7.pdf.
Moss, J. L., Reiter, P. L., & Brewer, N. T. (2015). Correlates of human papillomavirus (HPV) vaccine coverage: A state-level analysis. Sexually Transmitted Diseases, 42(2), 71–75.
Markowitz, L. E., Hariri, S., Lin, C., Dunne, E. F., Steinau, M., McQuillan, G., Unger, E. R. (2013). Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. Journal of Infectious Diseases, 208(3), 385–393.
Chaturvedi. (2010) Beyond cervical cancer: Burden of other HPV-related cancers among men and women Journal of Adolescent Health, 46, (4 Suppl), S20–S26.
United States Department of Agriculture; Economic Research Service. Rural-Urban Continuum, Codes. (2013). Retrieved March 22, 2018 from https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.
United States Census Bureau/American FactFinder. “Community Facts: Michigan”. 2017 American Community Survey. U.S. Census Bureau’s American Community Survey Office, 2017. Retrived from http://factfinder2.census.gov.
James (2014). All rural places are not created equal: Revisiting the rural mortality penalty in the United States. American Journal of Public Health, 104(11), 2122–2129.
Acknowledgements
The authors want to extend a special thank-you to all those involved in this research, especially all of the medical students who were involved in survey distribution.
Funding
The funding was provided by Central Michigan University
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gamber, A., Nowatzke, J., Cheng, CI. et al. Disparities in HPV Screening and Prevention in Metropolitan and Nonmetropolitan Regions of Michigan. J Community Health 44, 473–478 (2019). https://doi.org/10.1007/s10900-019-00644-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-019-00644-7