Abstract
Despite ambitious goals to eliminate hepatitis C virus (HCV) in the United States by 2030, the majority of those infected are not aware of their diagnosis, and only a small minority have been cured. A lack of knowledge regarding risk factors and treatment may contribute to low cure rates. We aimed to evaluate HCV knowledge and the association of risk factor knowledge with HCV incidence. In fall 2017, a survey regarding HCV knowledge was disseminated through social media, web link, and in person throughout the state of Virginia. The survey was completed by 613 individuals. Residents of high-incidence counties identified fewer risk factors (5.6 vs 6.1 of 9, p = 0.04), a difference that remained significant when controlling for education and age (p = 0.03). Fewer participants in the high-incidence group recognized snorting drugs to be a risk factor (25% vs 36%, p = 0.01). Only 38% of all respondents correctly identified HCV to be curable. Knowledge of HCV risk factors is lower in high incidence regions. These results identify a critical knowledge gap in the general population at a time of ongoing HCV transmission. Public health interventions must target these gaps in high-incidence regions as part of comprehensive disease prevention programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, only 50% of the estimated 3.5 million people infected with hepatitis C virus (HCV) know of their diagnosis [4]. Those who are unaware of their status cannot seek out hepatitis C care or curative treatment and remain at risk for complications such as cirrhosis, liver cancer, and need for liver transplantation. Whereas the majority of those infected are “baby boomers” born between 1945 and 1965, the opioid epidemic has led to a rise in hepatitis C associated with intravenous drug use, particularly among young non-urban people in regions such as Appalachia [14, 20].
Knowledge of hepatitis C has been shown to be limited among the general population and in high risk populations [3, 9, 10, 15, 16], though knowledge is greater in those with more education [5, 11, 13, 15, 16], those who are white [4, 7], and women [15, 16]. Given the concerning rise in hepatitis C infections associated with the opioid epidemic, and the limited progress in diagnosing and treating those infected, we aimed to determine whether living in a region with high hepatitis C incidence impacted knowledge of hepatitis C risk factors and treatment among the general population.
Methods
Study Design
We undertook a convenience sampling of adults in the state of Virginia between August and December 2017. This research study was reviewed and determined to be non-human subjects research by the University of Virginia Social and Behavioral Sciences institutional review board. In order to reach Virginians from across the state, multiple methods of survey dissemination were used including through social media, a web link, and in person at community events. Basic demographic information, including residence location, age group, and education level was collected. Participants completed knowledge questions regarding hepatitis C risk factors and treatment.
Those participants who provided a city or county residence location within the state of Virginia were assigned to high and low incidence groups. The high incidence group was defined to have an incidence of 150 cases per 100,000 population or greater based on 2016 data from the Virginia Department of Health [17].
Statistical Analysis
For statistical analysis, the proportion of participants correctly identifying each risk factor was compared using chi square with Fisher’s exact, based on the number of responses. The number of risks identified, a continuous variable, was analyzed using Mann–Whitney test given non-normality. Multivariate logistic regression was performed to adjust risk factor identification by age group and education level. Statistical analyses were performed with Stata 15.0 (StataCorp LLC, College Station, TX).
Results
The survey was completed by 613 participants, of whom, 407 (66%) accessed the survey through social media, 134 (22%) through the web link, and 72 (12%) in person. Participants varied in age and education (Table 1). Ninety-nine percent of participants had heard of hepatitis C, most commonly through television (57%). Hepatitis C was correctly identified to be curable by 229 (37%) participants.
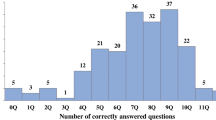
Among the 499 participants for whom county level residence was provided, 225 (45%) live in an area with high hepatitis C incidence. The high incidence group identified a mean of 5.6 risk factors, significantly lower than the 6.1 risk factors identified in the low incidence group (p = 0.03). The most commonly identified risk factor was injection drug use and the least commonly identified risk factor was snorting drugs (Fig. 1). The proportion of participants correctly identifying a risk factor was lower in the high incidence group for all nine risk factors included in the study. The difference was significantly lower in the identification of tattoos or piercings and snorting drugs as risk factors (77% vs 87%, p = 0.004 and 25% vs 36%, p = 0.01). In a multivariate logistic regression model adjusted for age and education level, living in a high incidence region was associated with lower odds of identifying at least 6 of 9 risk factors (OR 0.66, 95% CI 0.46–0.96, p = 0.03).
In the high incidence group, 102 of 225 people (45%) identified hepatitis C to be curable, significantly higher than the 88 of 274 (32%) in the low incidence group (p = 0.002). Those in the high incidence group were also more likely to correctly identify treatment to consist of 12 weeks of pills (75 of 225, 33% vs 62 of 274, 23%, p = 0.008).
Discussion
Overall knowledge of hepatitis C among the general population surveyed is limited. Those living in high incidence regions identified fewer hepatitis C risk factors than those in low incidence regions. As injection drug use is the primary risk factor for new cases of hepatitis C in this region [18], it is encouraging that most participants identified this to be a risk factor in accordance with prior studies [9, 16]. Unfortunately, only a few participants were able to identify that snorting drugs, a form of non-injection drug use, places individuals at risk for intranasal transmission of hepatitis C [1]. “Baby boomers” born between 1945 and 1965 have been targeted for diagnosis with one-time screening recommended for all people in this age group. Despite the recommendation for widespread screening, only 51–58% of our participants identified this group to be at risk. While those in high incidence regions were more likely to know hepatitis C can be cured, only a minority in each group answered this question correctly. Our findings are similar to the 22–35% of people in earlier studies who knew that hepatitis C is curable [8, 9].
Among people living with hepatitis C, knowledge impacts their care. Those with higher knowledge are more likely to discuss hepatitis C management with their medical provider [8] and more likely to be willing to accept treatment [2, 7, 19]. Hepatitis C education campaigns can improve knowledge [9, 13], and a formal hepatitis C education program can shorten time to treatment and improve virologic response [6]. In a screening program focused on people who use drugs in rural Appalachia, a portion of which includes Virginia, only 8% received treatment after testing positive for hepatitis C [12], demonstrating a significant need for improvement in linkage to care and treatment. Given the limited knowledge within our cohort, there is room for improvement through educational campaigns.
The use of convenience sampling is a limitation of the survey. Lack of county-level residence information restricted the number of participants included in our primary analysis. To maintain brevity and ensure completion of the survey, survey questions regarding an individual’s hepatitis C risk were not included, and therefore participants have been grouped by their population-level risk rather than their individual-level risk.
In the midst of an ongoing opioid and hepatitis C epidemic, public health efforts must address the limited knowledge of risk factors for hepatitis C, as this may impact prevention of new cases. To encourage treatment of those already infected, there is a role for educational campaigns promoting knowledge of risk factors and possibility of cure, especially in high incidence regions.
References
Aaron, S., McMahon, J. M., Milano, D., Torres, L., Clatts, M., Tortu, S., et al. (2008). Intranasal transmission of hepatitis C virus: Virological and clinical evidence. Clinical Infectious Diseases, 47(7), 931–934. https://doi.org/10.1086/591699.
Alam-Mehrjerdi, Z., Moradi, A., Xu, F., Zarghami, M., Salehi-Fadardi, J., & Dolan, K. (2016). Willingness to receive treatment for hepatitis C among injecting drug users on methadone program: Implications for education and treatment. Addiction & Health, 8(2), 90–97.
Chen, E. Y., North, C. S., Fatunde, O., Bernstein, I., Salari, S., Day, B., & Jain, M. K. (2013). Knowledge and attitudes about hepatitis C virus (HCV) infection and its treatment in HCV mono-infected and HCV/HIV co-infected adults. Journal of Viral Hepatitis, 20(10), 708–714. https://doi.org/10.1111/jvh.12095.
Denniston, M. M., Klevens, R. M., McQuillan, G. M., & Jiles, R. B. (2012). Awareness of infection, knowledge of hepatitis C, and medical follow-up among individuals testing positive for hepatitis C: National Health and Nutrition Examination Survey 2001–2008. Hepatology (Baltimore. Md.), 55(6), 1652–1661. https://doi.org/10.1002/hep.25556.
Lea, T., Hopwood, M., & Aggleton, P. (2016). Hepatitis C knowledge among gay and other homosexually active men in Australia. Drug and Alcohol Review, 35(4), 477–483. https://doi.org/10.1111/dar.12333.
Lubega, S., Agbim, U., Surjadi, M., Mahoney, M., & Khalili, M. (2013). Formal hepatitis C education enhances HCV care coordination, expedites HCV treatment and improves antiviral response. Liver International, 33(7), 999–1007. https://doi.org/10.1111/liv.12150.
Mah, A., Hull, M. W., DeBeck, K., Milloy, M. J., Dobrer, S., Nosova, E., et al. (2017). Knowledge of hepatitis C and treatment willingness amongst people who inject drugs in an era of direct acting antivirals. The International Journal on Drug Policy, 47, 137–143.
Mehta, S. H., Genberg, B. L., Astemborski, J., Kavasery, R., Kirk, G. D., Vlahov, D., et al. (2008). Limited uptake of hepatitis C treatment among injection drug users. Journal of Community Health, 33(3), 126–133. https://doi.org/10.1007/s10900-007-9083-3.
Norton, B. L., Voils, C. I., Timberlake, S. H., Hecker, E. J., Goswami, N. D., Huffman, K. M., et al. (2014). Community-based HCV screening: Knowledge and attitudes in a high risk urban population. BMC Infectious Diseases. https://doi.org/10.1186/1471-2334-14-74.
Pieper, B., & Sickon, K. (2017). Hepatitis C virus: Patients’ risk factors and knowledge in an urban clinic providing wound care. Wounds: A Compendium of Clinical Research and Practice, 30(3), 62–67.
Proeschold-Bell, R. J., Blouin, R., Reif, S., Amana, A., Rowland, B. J., Lombard, F., et al. (2010). Hepatitis C transmission, prevention, and treatment knowledge among patients with HIV. Southern Medical Journal, 103(7), 635–641. https://doi.org/10.1097/SMJ.0b013e3181e1dde1.
Stephens, D. B., Young, A. M., & Havens, J. R. (2017). Healthcare contact and treatment uptake following hepatitis C virus screening and counseling among rural appalachian people who use drugs. The International Journal on Drug Policy, 47, 86–94.
Surjadi, M., Torruellas, C., Ayala, C., Yee, H. F., Jr, & Khalili, M. (2011). Formal patient education improves patient knowledge of hepatitis C in vulnerable populations. Digestive Diseases and Sciences, 56(1), 213–219. https://doi.org/10.1007/s10620-010-1455-3.
Suryaprasad, A. G., White, J. Z., Xu, F., Eichler, B. A., Hamilton, J., Patel, A., et al. (2014). Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006–2012. Clinical Infectious Diseases, 59(10), 1411–1419. https://doi.org/10.1093/cid/ciu643.
Treloar, C., Hull, P., Dore, G. J., & Grebely, J. (2012). Knowledge and barriers associated with assessment and treatment for hepatitis C virus infection among people who inject drugs. Drug and Alcohol Review, 31(7), 918–924. https://doi.org/10.1111/j.1465-3362.2012.00468.x.
Vermunt, J., Fraser, M., Herbison, P., Wiles, A., Schlup, M., & Schultz, M. (2015). Prevalence and knowledge of hepatitis C in a middle-aged population, Dunedin, New Zealand. World Journal of Gastroenterology, 21(35), 10224–10233. https://doi.org/10.3748/wjg.v21.i35.10224.
Virginia Department of Health. (2016). Communicable disease data. http://www.vdh.virginia.gov/data/communicable-diseases/. Accessed Mar 2018.
Virginia Department of Health. (2016). Virginia hepatitis C epidemiologic report 2016. http://www.vdh.virginia.gov/content/uploads/sites/10/2016/06/Virginia-Hepatitis-C-Epidemiologic-Profile-2016.pdf. Accessed Mar 2018.
Zeremski, M., Dimova, R. B., Zavala, R., Kritz, S., Lin, M., Smith, B. D., et al. (2014). Hepatitis C virus-related knowledge and willingness to receive treatment among patients on methadone maintenance. Journal of Addiction Medicine, 8(4), 249–257. https://doi.org/10.1097/ADM.0000000000000041.
Zibbell, J. E., Iqbal, K., Patel, R. C., Suryaprasad, A., Sanders, K. J., Moore-Moravian, L., et al. (2015). Increases in hepatitis C virus infection related to injection drug use among persons aged. MMWR. Morbidity and Mortality Weekly Report, 64(17), 453–458.
Funding
This work was support by the National Institute of Allergy and Infectious Diseases [Grant Number T32 AI007046-41].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Knick, T., Sherbuk, J.E. & Dillingham, R. Knowledge of Hepatitis C Risk Factors is Lower in High Incidence Regions. J Community Health 44, 12–15 (2019). https://doi.org/10.1007/s10900-018-0545-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-018-0545-6