Abstract
There has been a marked increase in use of herbal products and dietary supplements (HP/DS) in many developed and developing countries. However, data about consumption patterns and awareness about these products in the Lebanese population is scarce. The present study aimed to examine the determinants of HP/DS use in Lebanese adults, identify potential interactions and safety concerns and assess the knowledge and attitudes of consumers towards the efficacy and safety of these products. A face-to-face, 28-item survey was administered to Lebanese adults (n = 726) in community pharmacies across the country. Thirty-five percent of participants reported to be currently consuming at least one HP/DS including 23 % who were consuming vitamins and/or mineral supplements and 18 % consuming herbal products. Significant safety concerns were identified among consumers in the form of disease–supplement, drug–supplement as well as supplement–supplement interactions. Logistic multivariate regression analysis indicated that use of supplements was positively associated with the female gender and increasing age. The majority of respondents falsely believed that HP/DS pose no risk to the general population and that they must be safe to be sold in Lebanon. Moreover, most participants were consuming these products based on recommendations from friends or relatives rather than from healthcare professionals. Substantial misconceptions about HP/DS exist among Lebanese adults, indicating a need for consumers’ education from professional and reliable sources on the efficacy and safety of such products.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Complementary and alternative medicine (CAM), a non-conventional health-care practice, used in the prevention, diagnosis, improvement or treatment of various physical and mental illnesses has expanded globally and gained popularity worldwide According to the World Health Organization’s global survey on traditional and herbal medicines, there has been a marked increase in consumption of herbal products and dietary supplements (HP/DS) in many developed and developing countries [1].
As defined by the Food and Drug Administration (FDA), a dietary supplement is a non-drug product intended to supplement the diet with one or more of the following: vitamins, minerals, herbs, and amino acids; yet not be represented for use as a conventional food or sole item of a meal, or as a medicinal alternative [2]. It has been estimated that 40 % of the US population uses dietary supplements often and that almost twice as many have used at least one of the estimated 29,000 dietary supplements on the market [3]. Out-of-pocket expenditures on HP/DS totaled an estimated $36.7 billion in 2014 [4].
Although dietary supplement manufacturers must register their facilities with the FDA, they are not required to get FDA approval before producing or selling HP/DS [2]. Moreover, claims and information on product labels can sometimes be misleading to consumers [2]. While some dietary supplements have proven benefits in treating or preventing diseases; such as the use of Ginkgo biloba for managing cognitive impairments, the use of calcium and vitamin D to preserve healthy bones, or the use of folic acid to decrease the risk of certain birth defects [5]; well-designed clinical studies often times fail to support the use of other dietary supplements for multiple indications. Consequently, the American Society of Health-System Pharmacists (ASHP) believes that the widespread, indiscriminate use of dietary supplements presents substantial risks to public health. In fact, dietary supplements contain active ingredients that might interact significantly with certain prescription or over-the-counter medications, making them less effective and/or causing severe (sometimes life-threatening) clinical consequences. Herbal products that are reported to interact with medication include garlic, ginger, G. biloba, ginseng, and St. John’s wort [6]. Moreover, drugs that have a high potential to interact with herbal medicines usually have a narrow therapeutic index, like warfarin, digoxin, cyclosporine, tacrolimus, amitriptyline, midazolam, indinavir, and irinotecan [6]. Case reports have demonstrated that G. biloba may increase bleeding when combined with warfarin or aspirin, elevates blood pressure when combined with thiazide diuretics, and has even led to coma when combined with trazodone, a medication used to treat depression [6]. Other examples of drug–supplement interactions include chelation and inactivation of quinolone-type antibiotics by calcium and magnesium supplements [7] and diminished absorption and efficacy of bisphosphonates with concomitant calcium and vitamin D supplementation [8]. Another safety concern is the risk of toxicity when exceeding the RDA of vitamins and minerals. For instance, data suggests a possible increase in mortality with long-term use of vitamin E (400 IU or more), especially in patients with chronic diseases [9].
Studies conducted in the United States and Europe established high prevalence rates for the consumption of HP/DS and reported a widespread general belief that these products are harmless [10–12]. Similarly, high prevalence of CAM use was reported in Arab countries including Saudi Arabia and Kuwait [13, 14]. In Lebanon, the use of CAM therapies was evaluated in specific populations, such as diabetic individuals residing in the capital [15] as well as osteoarthritis patients [16]. Only one study was conducted among the general Lebanese adult population, revealing a 30 % prevalence of CAM use that was significantly associated with higher income, chronic disease and lack of access to needed healthcare [17]. However, no study has assessed Lebanese consumers’ knowledge and attitudes toward HP/DS. Understanding the outlook of the Lebanese community towards these products is an essential first step towards reducing their misuse and associated risks.
Methods
A quantitative research design was developed to study the use of HP/DS among a sample of Lebanese adults as well as the attitudes, and knowledge towards these products. The study was approved by the Lebanese American University’s Institutional Review Board. The purpose of the study was elucidated and participant consent was obtained prior to administering the surveys.
Sample
The targeted population were ambulating Lebanese subjects aged 18 years or above, recruited in various community pharmacies across different regions of Lebanon. To ensure a representative sample of adults, the pharmacies were randomly selected across the six Lebanese governorates: North of Lebanon, Mount Lebanon, Beirut, South of Lebanon, Beqaa and Nabatieh. Subjects were interviewed face-to-face by one of four interviewers (two registered dietitians and two pharmacy students) and were asked about their consumption of any HP/DS. Their knowledge and attitudes towards HP/DS were assessed through a questionnaire.
Instrument
The 28-item questionnaire was modified from the 35-item instrument used by Marinac et al. [10], to measure usage patterns for, attitudes about, and knowledge of herbal products and nutritional supplements among older adults in the US.
The instrument included five parts: socio-demographics (gender, age, region, educational level, smoking and alcohol consumption status, and physical activity status), medical history and status (medical visits, medical conditions, medicinal drugs and indications), consumption patterns (use of vitamins, minerals, dietary supplements, herbal products, information source and purchase location, side effects), attitude, and knowledge towards HP/DS use.
To assess inter-observer reliability and to evaluate the clarity of the survey queries, a pilot study was carried out on 18 volunteers. Accordingly, minor modifications were made to question wording and layout based on feedback from the respondents and interviewers.
Data Analysis
Data were prospectively stratified by gender, age and education level. Each demographic inquiry and assessment question was tabulated and then recorded as the percentage of the total survey. We used descriptive statistics to assess basic knowledge, as well as perceptions—especially with regard to safety and usage. Multivariate logistic regression was used to assess univariate associations with the Odds Ratios (OR) of HP/DS use among the interviewees. Sociodemographic factors, current health status, and participants’ attitudes towards use were the independent predictors. Adjusted OR and 95 % confidence intervals (CI) for the probability of using at least one HP/DS were calculated for each predictor to explain the strength of the association after controlling for age, gender and education level.
All quantitative data were analyzed with the statistical package SPSS, version 22. Descriptive data were presented as mean ± standard error of the mean (SEM). p values < 0.05 were considered statistically significant.
Results
Demographic Data and Health Status
Sociodemographic characteristics and health status of participants are summarized in Table 1. A total of 726 surveys were collected. The survey response rate was 93 %. Among respondents, 59.8 % were females while 40.2 % were filled by males. Age distribution was as follows; 35.8 % of participants were 18–29 years old, 22.0 % were 30–39 years old, 19.6 % were 40–49 and 22.6 % were 50 or above (50–59 years, 14 %; 60–69, 5.1 %; and 70+, 3.4 %). Most participants (69.1 %) had a university degree and were residing in Beirut governorate (44.0 %). Regarding physical activity, more than half of the participants reported exercising 1–3 times a week (57.5 %). The most prevalent medical conditions reported were gastrointestinal diseases (12.4 %), followed by hypertension (12.0 %), diabetes mellitus (7.4 %), and dyslipidemia (6.7 %). Patients on chronic medications constituted 41.2 % of the studied population.
Patterns of Use of Dietary Supplements and Herbal Products
Thirty-five percent of participants reported to be currently consuming at least one HP/DS.
Around 23 % of the respondents reported taking at least one vitamin and/or mineral supplements. Among these, one-a-day multivitamin supplements were most commonly used (13.1 %) followed by calcium (9 %) and vitamin C (5.4 %), (Fig. 1).
Eighteen percent of participants reported taking at least one herbal product or non-vitamin/mineral supplement. A total of 16 different herbs or non-vitamin/mineral supplements were identified (Fig. 1). Fish oil and L-carnitine were the most commonly used products, followed by G. biloba, protein shakes and glucosamine. Probiotics, ginseng, valerian, aloe vera, garlic and St. John’s wort were less frequently used.
More than half of the individuals (64 %) who reported taking HP/DS purchased them in pharmacies, 32 % at nutrition/supplement stores, 3 % ordered them online and 1 % purchased them in local market (not as pre-packaged products). Regarding sources of information, 39.5 % of respondents reported consuming supplements based on the recommendation of a family member, friend or relative, 21 % based on the advice of a pharmacist, 19.7 % based on their physician’s recommendation, 19 % based on information from the media (magazines, internet, newspaper, TV…), and 2.3 % based on one or more of the mentioned information sources.
Predicting Factors Associated with the Use of HP/DS
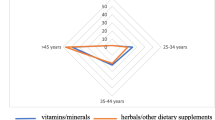
Table 2 summarizes the predictors for HP/DS use in our study population. Based on the logistic regression model, results showed that participants consuming HP/DS (compared with participants not using any) were associated with the female gender (OR 2.35, 95 % CI 1.99–2.51, p = 0.031) and older age (OR 1.22, 95 % CI 0.97–1.54, p = 0.04). The age group consuming the most HP/DS was 50–59 years (of which 45.7 % consumed at least 1 supplement);
On the other hand, participants who reported exercising 2–3 times a week (OR 0.24, 95 % CI 0.12–0.48, p ≤ 0.001) or more than 3 times a week (OR 0.3, 95 % CI 0.15–0.61, p = 0.001) were less likely to use HP/DS. Also, having heart disease, gastrointestinal or musculoskeletal disorders was associated with a decreased probability of HP/DS use (respective OR 0.15, 95 % CI 0.05–0.28, p < 0.05) There were no significant associations between HP/DS use and place of residence, education, smoking or alcohol consumption (Table 3).
Safety
A total of 71 significant disease–supplement, drug–supplement and supplement–supplement interactions were identified. Among patients taking herbals or non-vitamin/mineral supplements, 16 % were found to have a potential disease–supplement interaction (like worsening of glycemia control in diabetics, worsening of cholesterol levels in dyslipidemia patients), 20 % had documented drug–supplement interactions (such as being on two blood thinners, aspirin and omega-3 fish oil) and 13 % of consumers were identified having a least one supplement–supplement interaction (such as duplication of therapy, two supplements containing omega-3 fish oil).
Knowledge, Awareness and Attitudes Towards HP/DS
Results from the survey items relating to the perceptions and knowledge of respondents towards dietary supplements are presented in Table 2. Fifteen percent of males and 29.2 % of females believed that “vitamin and mineral supplements do not pose risk to the general population”. The majority of participants knew that the herbal products sold in Lebanon were not regulated by the government and that herbal products sold in Lebanon may not be pure. The majority of respondents (80.2 %) acknowledged the fact that different brand names do not contain the same amount of herbal products and considered that it was important to inform one’s physician about any supplements being consumed (93.3 %).
When asked about whether insurance should pay for the dietary supplements and vitamins, 34.9 % of participants believed that insurance should cover supplements. In addition, the majority (85.9 %) expressed an interest in getting more information on whether dietary supplements or herbal products are helpful.
When asked about motives for consuming HP/DS, 21.8 % of participants responded that they were likely to consume them “only if needed”, 25.2 % if they thought “it will help them”, 24.8 % upon physician’s recommendation and 28.2 % said that they would not consume HP/DS.
Discussion
Patterns of Use of HP/DS
Around 35 % of our study participants were using at least one HP/DS. The high prevalence of use may be explained by multiple factors such as consumers’ increased awareness toward health and well-being, and perceived benefits of the supplements. It was demonstrated that individuals expect such products to prevent and treat diseases, improve quality of life, boost the immune system and promote emotional support [8, 17, 18]. An additional factor might be linked to patients’ usual dissatisfaction with conventional medicine and their recourse to alternative medicine that they believe to be natural and harmless [19].
The present results revealed that multivitamin-type supplements were predominantly used in the Lebanese community. Similar findings in published reports showed the frequent tendency of multivitamins’ use in the US adult population [20–23]. A possible explanation may be that participants feel reassured against nutrition deficiencies by using a multivitamin-type supplement. Moreover, individuals may prefer this practice over augmenting specific nutrients in their diet [21]. Even if multivitamins are relatively safe, caution is warranted due to the high prevalence of use, the abundance of high-dose supplements on the market as well as the risk of multiple supplements use [24].
Among the non-vitamins/minerals supplements, omega-3 fatty acids (eicosapentaenoic acid, EPA and docosahexaenoic acid, DHA) were the most commonly used. As indicated by the American Heart Association, the role of these supplements is limited to the secondary prevention of coronary artery disease (CAD) and/or the medical management of hypertriglyceridemia at specific target doses of EPA and DHA equivalent to 1 g and 2–4 g/day respectively. For individuals without documented CAD, no definitive role of omega-3 supplementation exists and a diet-based approach was shown to be preferable [25]. Consumers therefore need to be aware of the limited documented benefits of these supplements. Moreover, the most common omega-3 preparations on the market usually provide only 180 mg of EPA and 120 mg DHA per capsule, therefore healthcare providers and consumers should be advised to carefully read nutrition labels to determine the therapeutic doses per indication. Additional areas of concern are the reported side effects and potential drug interactions of omega-3 fatty acid supplementation: gastrointestinal upset, bleeding risks especially when combined with blood thinning agents, non-steroidal anti-inflammatory drugs, worsening of glycemia and increase in LDL cholesterol [23, 24].
Predicting Factors of HP/DS Use
It is important for health-care providers (HCP) to recognize individuals most likely to use HP/DS since some patients might be reluctant to discuss their CAM therapies. While some investigators found no correlation between HP/DS use and sociodemographic factors [26, 27]; the present survey revealed that the woman gender, as well as middle-age (especially the 50–59 years age group) were positive predictors. This finding is consistent with other surveys conducted in the US population reporting highest HP/DS use in women aged 50–59 years [11, 15, 28, 29]. Special attention is required in this population since older adults tend to develop more chronic diseases, and become more prone to be on complex drug regimens. Supplement-disease exacerbations and interactions with polypharmacy are therefore a more frequent concern.
On the other hand, participants who tended to be more physically active (exercising at least 2–3 times a week) were less likely to use HP/DS compared to sedentary participants. This observation may be explained by the fact that physically active individuals rely on the general health benefits offered by physical activity and do not see a need for HP/DS to improve their health.
We also found that patients with chronic conditions (particularly heart, musculoskeletal and gastrointestinal disorders) were less likely to ingest HP/DS. Probable reasons may be more frequent HCP-patient interactions and closer medical follow-up as well as a pre-existing complex drug regimen among patients with chronic diseases, and its associated pill burden.
Safety Concerns
Significant safety concerns were identified among consumers in the form of disease–supplement, drug–supplement as well as supplement–supplement interactions. The most common drug–supplement interaction was the increased risk of bleeding with anticoagulants and antiplatelet agents when taken concomitantly with fish oil, G. biloba, glucosamine and/or garlic [30, 31]. Another serious drug–supplement interaction was potentiation of CNS depression in patients on benzodiazepines concomitantly taking St. John’s wart [6]. Regarding disease–supplement interactions, a large number of participants treated for gastrointestinal (GI) diseases were exacerbating their conditions by ingesting supplements like garlic or fish oil known for their GI disturbances side effects [6]. Also some diabetes patients were consuming fish oil and/or glucosamine supplements which might affect their glycemic control [8, 32]. Important supplement–supplement interactions recorded on participants taking multiple supplements were omega-3 fatty acids duplication therapy with fish oil and cod liver oil or flaxeed oil, as well as additive blood thinning effects of combined omega-3 supplements, G. biloba, garlic and/or glucosamine [6].
Knowledge, Awareness and Attitudes Towards HP/DS
The present study revealed misperceptions and misconceptions regarding the safety of HP/DS among the Lebanese community. More than half of the respondents falsely believed that supplements pose no risk to the general population and that they must be safe to be sold in Lebanon. Similar work conducted in the US population and in Serbia, revealed similar widespread beliefs that HP/DS available on the market are inoffensive [10–12]. Moreover, the present results revealed that most respondents were consuming supplements based on non-professional friends and the advice of relatives, marginalizing the role of HCP in regards to CAM use. This attitude was also observed in Lebanese diabetic patients since two-thirds of surveyed patients were referred or encouraged to use CAM by a friend [15]. Explanation for this observation might be linked to the nature and characteristics of the Lebanese community where family and friends have a big influence on individuals. Indeed, it has been shown that the Arab culture generally encourages individuals to discuss and solve problems within the context of the informal social systems of family and community [33]. Interestingly, the large majority of the Lebanese population represented in our study expressed a desire to know more about efficacy and safety of the supplements. These findings underscore a compelling need to raise public awareness regarding HP/DS use. Unfortunately, a survey evaluated Lebanese physicians’ perceptions and practices regarding herbal medicine and showed an alarmingly poor knowledge of supplements’ mechanisms of action, possible interactions and overall safety [14]. Therefore, physicians, pharmacists, dietitians, among other HCP are invited to educate themselves and consequently the public regarding the safety and efficacy of DS/HP in specific chronic conditions as well as their potential interactions with pharmacologic treatments.
Limitations
The present study does have potential limitations. Similarly to all pharmacy-based patient surveys [34], there might have been a selection bias, which could partly explain the somewhat higher prevalence rate in comparison with the study by Naja et al. [17]. When recruiting participants at pharmacies, it is more likely that they consume medications and supplements. Collected data may not be extrapolated to institutionalized or homebound subjects, or those individuals less likely to visit the pharmacy. Additionally, under-or inaccurate reporting might have occurred since we relied on participants’ self-reporting of their consumption of DS/HP without performing thorough medication reviews which might have introduced an unknown degree of measurement error and or recall bias. Despite the mentioned limitations, the major strength of our study resides in the fact that it was the first to examine the perceptions and attitudes of a large number of individuals on HP/DS use, and to identify potential interactions and safety concerns.
Conclusion/Recommendations
The present study reported the prevalence of HP/DS use in a select Lebanese general population. Results showed that the use of these supplements is prevalent, and that it was highest among females aged between 50 and 59 years. Moreover, significant drug or disease interactions with HP/DS and misconceptions about the appropriate use of these products were identified.
The current results therefore emphasize the compelling need for spreading public awareness in Lebanon regarding DS/HP products. Patients should be advised that the use of the DS/HP products may not always be beneficial and can cause serious side effects therefore consulting with HCP is essential before initiation of any supplement. Additionally all members of the multidisciplinary healthcare team should fully understand the potential hazards and benefits of HP/DS therapies and should encourage patients’ disclosure on alternative medicine as part of the visit histories. A collaborative effort of governmental bodies, health-major educational institutions is recommended to educate, regulate and promote the appropriate and safe use of HP/DS.
References
World Health Organization. (2005). National policy on traditional medicine and regulation of herbal medicines: Report of a WHO global survey.
US Food and Drug Administration. Dietary supplement health and education act of 1994.
Department of Health and Human Services (DHHS), Office of the Inspector General. (2003). Dietary supplement labels: key elements. Report OEI-01-01-00120.
Nutrition Business Journal. NBJ’s Supplement Business Report 2015. Penton Media, Inc., 2015.
Dietary Supplements: What you need to know. (2011). US Department of Health and Human Services, Office of Dietary Supplements. National Institutes of Health.
Chen, X. W., S Serag, E., B Sneed, K., et al. (2011). Clinical herbal interactions with conventional drugs: From molecules to maladies. Current Medicinal Chemistry, 18(31), 4836–4850.
Hartshorn, E. A., Lomaestro, B. M., & Bailie, G. R. (1991). Quinolone-cation interactions: A review. Annals of Pharmacotherapy, 25(11), 1249–1258.
Altundag, O., Altundag, K., Silay, Y. S., Gunduz, M., Demircan, K., & Gullu, I. (2004). Calcium and vitamin D supplementation during bisphosphonate administration may increase osteoclastic activity in patients with bone metastasis. Medical Hypotheses, 63(6), 1010–1013.
Bjelakovic, G., Nikolova, D., Gluud, L. L., Simonetti, R. G., & Gluud, C. (2012). Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane: The Cochrane Library.
Marinac, J. S., Buchinger, C. L., Godfrey, L. A., Wooten, J. M., Sun, C., & Willsie, S. K. (2007). Herbal products and dietary supplements: A survey of use, attitudes, and knowledge among older adults. The Journal of the American Osteopathic Association, 107(1), 13–23.
Kennedy, J. (2005). Herb and supplement use in the US adult population. Clinical Therapeutics, 27(11), 1847–1858.
Samojlik, I., Mijatović, V., Gavarić, N., Krstin, S., & Božin, B. (2013). Consumers’ attitude towards the use and safety of herbal medicines and herbal dietary supplements in Serbia. International Journal of Clinical Pharmacy, 35(5), 835–840.
AlBedah, A. M., Khalil, M., Elolemy, A. T., et al. (2013). The use of and out-of-pocket spending on complementary and alternative medicine in Qassim province, Saudi Arabia. Annals of Saudi Medicine, 33(3), 282–289.
Awad, A., & Al-Shaye, D. (2014). Public awareness, patterns of use and attitudes toward natural health products in Kuwait: A cross-sectional survey. BMC Complementary and Alternative Medicine, 14(1), 105.
Naja, F., Mousa, D., Alameddine, M., Shoaib, H., Itani, L., & Mourad, Y. (2014). Prevalence and correlates of complementary and alternative medicine use among diabetic patients in Beirut, Lebanon: A cross-sectional study. BMC Complementary and Alternative Medicine, 14(1), 185.
Alaaeddine, N., Okais, J., Ballane, L., & Baddoura, R. M. (2012). Use of complementary and alternative therapy among patients with rheumatoid arthritis and osteoarthritis. Journal of Clinical Nursing, 21(21–22), 3198–3204.
Naja, F., Alameddine, M., Itani, L., Shoaib, H., Hariri, D., & Talhouk, S. (2015). The use of complementary and alternative medicine among lebanese adults: Results from a National Survey. Evidence-Based Complementary and Alternative Medicine.
Ernst, E., & Hung, S. K. (2011). Great expectations. The Patient: Patient-Centered Outcomes Research, 4(2), 89–101.
Stickel, F., & Shouval, D. (2015). Hepatotoxicity of herbal and dietary supplements: An update. Archives of Toxicology, 89(6), 851–865.
Foote, J. A., Murphy, S. P., Wilkens, L. R., Hankin, J. H., Henderson, B. E., & Kolonel, L. N. (2003). Factors associated with dietary supplement use among healthy adults of five ethnicities the Multiethnic Cohort Study. American Journal of Epidemiology, 157(10), 888–897.
Block, G., Sinha, R., & Gridley, G. (1994). Collection of dietary-supplement data and implications for analysis. The American Journal of Clinical Nutrition, 59(1), 232S–239S.
Slesinski, M. J., SUBAR, A., & Kahle, L. L. (1995). Trends in use of vitamin and mineral supplements in the United States: The 1987 and 1992 National Health Interview Surveys. Journal of the American Dietetic Association, 95(8), 921–923.
Slesinski, M. J., Subar, A. F., & Kahle, L. L. (1996). Dietary intake of fat, fiber and other nutrients is related to the use of vitamin and mineral supplements in the United States: the 1992 National Health Interview Survey. The Journal of Nutrition, 126(12), 3001.
Guallar, E., Stranges, S., Mulrow, C., Appel, L. J., & Miller, E. R. (2013). Enough is enough: Stop wasting money on vitamin and mineral supplements. Annals of Internal Medicine, 159(12), 850–851.
Krauss, R. M., Eckel, R. H., Howard, B., et al. (2000). AHA dietary guidelines revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation, 102(18), 2284–2299.
Planta, M., Gundersen, B., & Petitt, J. C. (2000). Prevalence of the use of herbal products in a low-income population. Family Medicine, 32(4), 252–257.
Johnson, E. M., Wootton, J. C., Kimzey, R., et al. (2000). Use of herbal therapies by adults seen in an ambulatory care research setting: An exploratory survey. The Journal of Alternative and Complementary Medicine, 6(5), 429–435.
Eisenberg, D. M., Davis, R. B., Ettner, S. L., et al. (1998). Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA, 280(18), 1569–1575.
Kaufman, D. W., Kelly, J. P., Rosenberg, L., Anderson, T. E., & Mitchell, A. A. (2002). Recent patterns of medication use in the ambulatory adult population of the United States: The Slone survey. JAMA, 287(3), 337–344.
Knudsen, J. F., & Sokol, G. H. (2008). Potential Glucosamine‐Warfarin Interaction Resulting in Increased International Normalized Ratio: Case Report and Review of the Literature and MedWatch Database. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 28(4), 540–548.
Izzo, A. A., & Ernst, E. (2001). Interactions between herbal medicines and prescribed drugs. Drugs, 61(15), 2163–2175.
Smith, J. D., & Clinard, V. B. (2014). Natural products for the management of type 2 diabetes mellitus and comorbid conditions. Journal of the American Pharmacists Association, 54(5), e304–e321.
Pines, A. M., & Zaidman, N. (2003). Israeli Jews and Arabs similarities and differences in the utilization of social support. Journal of Cross-Cultural Psychology, 34(4), 465–480.
Frisk, P., Kälvemark-Sporrong, S., & Wettermark, B. (2014). Selection bias in pharmacy-based patient surveys. Pharmacoepidemiology and Drug Safety, 23(2), 128–139.
Acknowledgments
We acknowledge Ms. Marya Hanna and Ms. Maria-Elena hakim for their contribution in interviewing participants.
Authors’ Contributions
G.K. and N.Z. conceived the study, and participated in its design and coordination. N.Z., G.K. and W.R. carried out the data collection. N.Z. performed the statistical analysis. The manuscript was drafted by G.K. and N.Z. and reviewed by W.R.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare of no conflicts of interest.
Rights and permissions
About this article
Cite this article
El Khoury, G., Ramadan, W. & Zeeni, N. Herbal Products and Dietary Supplements: A Cross-Sectional Survey of Use, Attitudes, and Knowledge Among the Lebanese Population. J Community Health 41, 566–573 (2016). https://doi.org/10.1007/s10900-015-0131-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-015-0131-0