Abstract
This study examined the intersection of rurality and community area deprivation using a nine-state sample of inpatient hospitalizations among children (<18 years of age) from 2011. One state from each of the nine US census regions with substantial rural representation and varying degrees of community vulnerability was selected. An area deprivation index was constructed and used in conjunction with rurality to examine differences in the rate of ACSC hospitalizations among children in the sample states. A mixed model with both fixed and random effects was used to test influence of rurality and area deprivation on the odds of a pediatric hospitalization due to an ACSC within the sample. Of primary interest was the interaction of rurality and area deprivation. The study found rural counties are disproportionality represented among the most deprived. Within the least deprived counties, the likelihood of an ACSC hospitalization was significantly lower in rural than among their urban counterparts. However, this rural advantage declines as the level of deprivation increases, suggesting the effect of rurality becomes more important as social and economic advantage deteriorates. We also found ACSC hospitalization to be much higher among racial/ethnic minority children and those with Medicaid or self-pay as an anticipated source of payment. These findings further contribute to the existing body of evidence documenting racial/ethnic disparities in important health related outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As Affordable Care Act (ACA) implementation in the United States continues to reduce the proportion of the population without health insurance coverage, the impact of expanding insurance and health system reforms on effective primary care delivery for children remains largely unknown. There is, however, a need to understand existing community vulnerabilities and have metrics to monitor changes in the primary care system for children over time. Hospitalizations from ambulatory care sensitive (ACS) conditions, or those deemed by medical professionals as potentially preventable, are an increasingly common measure of access to primary care of reasonable quality [1].
Previous research has noted that hospitalization for ACSC diagnoses are more common among rural communities than among urban [2–8], suggesting gaps in service availability or quality for rural populations. Among children, however, these findings are mixed. Some research suggests that hospitalizations from ACSC are higher among rural children [2–4], while other studies have found no associations between rural residence and ACSC hospitalizations for this population [5]. The majority of studies, however, tend to be limited in scope, single state focused or oriented to a small number of ambulatory care sensitive conditions [9].
One potential reasons for these mixed findings is the extent to which area-level vulnerabilities more common in rural communities, but not exclusive to such communities, may influence observed outcomes. Higher rates of poverty and unemployment, lower rates of educational attainment, and the lack of access to affordable health care represent just some of the social determinants of health more prevalent in rural US communities which may contribute to observed health disparities [10]. Research suggests these underlying vulnerabilities also play a role in hospitalizations from ACSC and should be considered when examining this outcome [11].
Area deprivation, as a way of conceptualizing the intersection of these underlying community vulnerabilities, is an approach that has been used in United Kingdom, Europe and Asia when examining health care utilization [11, 12]. The core notion is that an index comprised of multiple indicators of the environment will be more accurate in pinpointing high-risk areas than examining each of the indicators alone, as is more commonly done in ACSC studies [13]. Use of an index reduces inter-correlation among multiple factors that generally vary together, such as employment and education, which are a threat to the validity of multivariable analysis.
The present study examines the intersection of rurality and area deprivation using hospitalizations for ACS diagnoses as an indicator of potentially inadequate access to care. A nine-state sample of inpatient hospitalizations among children (<18 years of age) from 2011 was used in the study. One state from each of the nine US census regions with substantial rural representation and varying degrees of community vulnerability was selected. An area deprivation index was constructed and used in conjunction with rurality to examine differences in the rate of ACSC hospitalizations among children in the sample states. The interaction of rurality and area deprivation was of primary interest for this study. We examined the extent to which observed effects of rurality vary within comparable levels of area deprivation. We anticipated some level of disparity between rural and urban children, and also expected differences among varying levels of area deprivation. However, the interplay of these two factors remains largely unknown.
Materials and Methods
Design and Data Source
We conducted a cross-sectional analysis of hospital discharge data from the 2011 AHRQ State Inpatient Databases (SID). Although 44 states participate in the SID, only 24 provide the patients’ county of residence. From this 24, nine states were chosen, using a selection algorithm that provided: (1) one state from each of the nine US Census regions; (2) adequate numbers of discharges; (3) adequate numbers of rural counties; (4) adequate representation of minority children; and (5) cost-effective data purchase. The selected states included 552 counties, about 18 % of all counties in the US
In total, 464,671 hospital discharges to children (<18 years of age) occurred in 2011 among the sample states. Approximately 64 % of the all discharges in the sample occurred Florida (147,994) and New York (149,460). Michigan accounted for nearly 10 % of discharges (45,198), while the remainder came from Washington (31,258), Colorado (29,525), Mississippi (27,806), Arkansas (25,306), South Dakota (6635) and Vermont (1759).
Study Variables
Hospitalization for an ACSC, the outcome of interest, was defined using the diagnosis list developed by Lu and Kuo [14]. We then created an area deprivation index to provide a practical measure of county-level vulnerability using public and readily available data. After a review of the literature for existing indices of area deprivation, we identified three area-level indices similar in concept to the present study, but not directly transferrable. The most closely related index came from Eibner and Sturm [15], which was heavily influenced by parallel indices constructed in the United Kingdom [12].
The Eibner and Sturm index uses unweighted Census-tract data from 16 variables reflecting various social determinants to measure deprivation. Relevant socio-demographic measures included income, poverty, unemployment, high school graduation rate, car ownership, household overcrowding, home ownership, percent married, percent non-white, percent non-English speakers, access to grocery stores and parks. Our index development process paralleled Eibner and Sturm, but used county of residence as the level of analysis. We began with the socio-demographic variables noted above. Car ownership was removed for conceptual reasons, as not owning a car in densely populated urban areas is not uncommon in the United States. Household overcrowding was dropped, as a reliable data source was not available. Finally, percent minority population was also dropped, recognizing the inappropriateness of labeling “non-white” a less than desirable status [16].
Using the remaining nine variables, we conducted a principal components analysis (PCA) to determine which of these variables were highly correlated with the concept of deprivation. The results of our PCA determined that these nine variables were measuring four discrete constructs, represented by four components. Five of our study variables loaded on the first component: income, poverty, unemployment, high school graduate rate, and single parent homes. These five variables were retained for construction of our deprivation index. We standardized the variables using z-scores, with the direction of positive or negative change across each variable in a consistent direction, summed the scores across the retained variables, and divided the results into quartiles to derive the actual index used in the analysis. Derivation of the index included all US counties, with quartile values assigned to each county in the sample. Child residence was measured at the county level. Rurality was defined using 2013 Urban Influence Codes (UIC), UIC codes 1 and 2 classified as urban and UIC codes (3–12) were considered rural [17].
In addition to rurality and area deprivation, additional individual characteristics and health system capacity measures were also included in the analysis. Individual factors were derived from the State Inpatient Database and include the child’s age, race/ethnicity, gender, and expected source of payment. Health system capacity was measured at the county level and includes the presence of a Federally Qualified Health Center (FQHC), Rural Health Clinic (RHC), and the quartile distributions of physicians and hospital beds per capita (10,000). The quartile distribution of physicians and hospital beds were derived from the 2012 Area Health Resource File (AHRF) and reflect the position of each studied county among all counties in the United States, not just the nine-state sample.
Statistical Analysis
A mixed model with both fixed and random effects was used to test influence of rurality and area deprivation on the odds of a pediatric hospitalization due to an ACSC within the sample. Of primary interest was the interaction of rurality and area deprivation. We specifically examined the effect of rurality within comparable levels of area deprivation. Fixed effects for rural, area deprivation, the interaction of rural and area deprivation, race/ethnicity, age, gender, pay source, transfer status, presence of a Federally Qualified Health Center or Rural Health Clinic, and the per capita number of physicians and hospital beds (10,000) were included in the model. Random effects for state were included in the model to account for unobserved heterogeneity at the state level. Predicted probabilities or marginal means were derived from the model incorporating both fixed and random effects in the estimates. All analysis was conducted using Stata version 12.
Results
Characteristics of the Study Population
Approximately 14 % of hospital discharges studied involved children who lived rural counties, while 86 % of discharges occurred among urban children (Table 1). Nearly one-third of child discharges in the sample took place in communities that are among the most deprived (34.88 %). Sample discharges most commonly involved children between 0 and 4 years of age (42.51 %) and white race/ethnicity (48.12 %). Black and Hispanic children accounted for 22.81 and 18.90 % of discharges, respectively. Slightly over one in three discharges had private insurance as a payment source (35.87 %), while Medicaid was the source of payment for over half of the all discharges (56.23 %).
When examining measures of health system capacity (Table 1), the majority of discharges involved children (91.14 %) who resided in a county with at least one Federally Qualified Health Center (FQHC), while 28.69 % resided in a county with a Rural Health Clinic (RHC). Most discharges among children occurred in counties with the per capita physician ratio and number of hospital beds available were in the top third and fourth quartiles.
Discharges among children in rural counties were disproportionately in the most deprived counties (41.18 %), compared to 33.85 % among urban county residents (p < 0.05; Table 1). Conversely, 15.13 % of child discharges occurring in urban counties were among the least deprived, compared to 6.55 % among rural. The age distribution of discharges among urban and rural children was comparable, with 42.12 % of urban discharges involving children ages 0–4 years, compared to 44.96 % of discharges among rural. Significant variation in the racial/ethnic composition of child discharges in the sample was noted, with 44.92 % of urban discharges occurring among white children compared to 67.83 % among rural discharges (p < 0.05). Approximately 20.75 % of discharges among Hispanic children in the sample occurred in urban areas compared to only 7.54 % in rural. Differences in anticipated source of payment were also noted, with 36.76 % of discharges among urban children being paid through private insurance compared to 30.40 % of rural discharges. Conversely, 66.50 % of discharges among rural children had Medicaid as a source of payment compared to 55.21 % of among their urban counterparts (p < 0.05).
The presence of an FQHC in the county was more common in urban counties, with 94.87 % of urban child discharges occurring in communities with an FQHC compared to 68.21 % among rural child discharges (p < 0.05, Table 1). As expected, more rural child discharges occurred in communities with an RHC than among urban child discharges (69.8 vs. 22.0 %). The distribution of physicians per capita was much different for urban and rural child discharges in the sample. Approximately 1.8 % of discharges to urban children occurred among communities with the lowest quartile for physicians per capita, compared to 20.03 % of rural children (p < 0.05). Conversely, only 20.05 % of rural child discharges occurred in counties among the top quartile of physicians per capita, versus 43.42 % of urban child discharges (p < 0.05).
Bivariate Analysis Results
As shown in Table 2, unadjusted bivariate analysis found no differences in the likelihood that a hospitalization would be due to ACSC among children by rurality alone. Across all discharges, approximately 25.35 % were due to ACSC among urban children compared to 24.08 % among rural children (unadjusted odds ratio 0.93; 95 % CI 0.73–1.19). Examining characteristics of the children themselves (Table 2), ACSC hospitalization rates were higher among those ages 5–9 (37.28 %) than among those 0 to 4 years of age (32.75 %; unadjusted odds ratio 1.22; 95 % CI 1.09–1.37). Significant differences by race/ethnicity were also noted with 22.34 % of hospitalizations due to ACSC among white children compared to 28.54 % among black children (unadjusted odds ratio 1.39; 95 % CI 1.30–1.49) and 28.57 % among Hispanic children (unadjusted odds ratio 1.37; 95 % CI 1.20–1.57). ACSC hospitalization rates were also significantly higher among child discharges with Medicaid as payment source (26.80 %) compared to those with private insurance (23.10 %; unadjusted odds ratio 1.21; 95 % CI 1.12–1.32).
Considering measures of health system capacity, child discharges occuring counties with a FQHC had a slightly higher proportion of ACSC hospitalizations (25.39 %) compared to 22.97 % among those with no FQHC (unadjusted odds ratio 1.14; 95 % CI 1.05–1.24). No differences in ACSC hospitalizations were noted by quartiles of physicians per capita.
Adjusted Analysis Results
Results from the adjusted analysis are shown in Table 3. After adjusting for individual measures, heath system capacity, and potentially unobserved heterogeneity at the state level, a slightly different pattern emerges. Although rurality alone was not a significant predictor of ACSC hospitalization, our findings suggest a differential impact of rurality within comparable levels of area deprivation. The interaction of rurality with level of area deprivation was significant; therefore dummy variables for the interaction were added to the models and differences in the likelihood of ACSC admissions between rural and urban were examined within each level of area deprivation.
Within the least deprived counties, the odds ACSC hospitalization were significantly lower in rural counties compared to urban counties (adjusted odds ratio 0.805, 95 % CI 0.741–0.876). Among not very deprived counties, the odds of hospitalization remained lower in rural counties compared to urban counties (adjusted odds ratio 0.937, 95 % CI 0.891–0.984). Among somewhat deprived counties however, the likelihood of ACSC hospitalization in rural counties is higher than that observed among urban counties (adjusted odds ratio 1.037, 95 % CI 0.997–1.080), but not statistically significant at alpha 0.05 level (p value = 0.074). Similar findings were noted among the most deprived counties (adjusted odds ratio 1.038, 95 % CI 0.998–1.081, p value = 0.065).
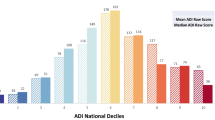
We interpret these findings to suggest that the effect of rurality becomes more important relative to what is observed among urban counties as area deprivation worsens. Figure 1 shows the predicted probability (marginal means) from the model for ACSC hospitalizations that includes both fixed and random effects, further illustrating the observed effect. In essence, the likelihood of ACSC hospitalization among discharged children in urban communities is largely unchanged across levels of area deprivation when adjusting for previously mentioned factors—but that is not the case for rural communities.
Predicted probability of ACSC hospitalization among children (<18 years of age) by Residence and Level of Deprivation (2011). Probabilities derived from a mixed model with fixed effects for rural, area deprivation, race/ethnicity, age, gender, pay source, transfer status, presence of a Federally Qualified Health Center or Rural Health Clinic, and the per capita number of physicians and hospital beds (10,000). Random effects for State were included in the model. Predicted probabilities were derived from the model using both fixed and random effects
Additional differences in ACSC hospitalization by individual characteristics and health system capacity are also shown in Table 3. The likelihood of ACSC hospitalization was significantly higher among discharges to black children (adjusted odds ratio 1.27, 95 % CI 1.24–1.29) and Hispanic children (adjusted odds ratio 1.18, 95 % CI 1.16–1.21). Compared to child discharges with private insurance, the risk of ACSC hospitalization was higher among children with Medicaid (OR 1.04, 95 % CI 1.02–1.05) and those who were private pay (adjusted odds ratio 1.17, 95 % CI 1.12–1.22). Notable reductions to ACSC hospitalization were noted among counties with physicians per capita in the top quartile (adjusted odds ratio 0.087, 95 % CI 0.83–0.91) compared to the lowest quartile. An increasing number of hospital beds per capita appears to be positively correlated with increases in ACSC hospitalization, but is likely due to higher concentrations of population volume in communities with hospital capacity.
Conclusions
Our study found that rurality alone was not significantly associated with increased likelihood of hospitalization from ACSCs among children. Although direct comparison is difficult given the methodological approach taken this study, our findings are consistent with previous research that also found no significant associations between rurality and ACSC hospitalization for children after adjusting for other important factors [5, 9]. Conversely, our findings differ from other studies that have found significant associations between rurality and ACSC hospitalizations [3, 4].
Although our study did not find that rurality alone is a strong predictor of ACSC hospitalization, we did find evidence of a differential effect for rural counties when accounting for the underlying level of vulnerability in the county using our area deprivation index. Within the least deprived counties, the likelihood of an ACSC hospitalization was significantly lower in rural counties than that observed among their urban counterparts. This rural advantage declined as the level of deprivation increased, principally because the likelihood of an ACSC hospitalization increased in parallel with area deprivation in rural counties, while declining in urban counties. Increases in ACSC hospitalizations for both rural and urban counties were noted at the highest level of deprivation. This pattern suggests the effect of rurality becomes more important as social and economic advantage deteriorates.
These findings suggest that examining rurality alone may under-represent the potential relationships between residence and selected outcomes when underlying levels of vulnerability are not well defined. Consolidating these determinants into a single measure that can be interacted with rural residence allows for examining the effects of rural within comparable levels of county deprivation that could otherwise be missed when examining residence alone or in conjunction with multiple control variables of interest.
These findings are consistent with other important research examining rural populations and factors contributing to observed differences in outcomes [18, 19]. Examining trends in rural–urban mortality differences between 1969 and 2009, Singh and Siahpush noted the substantial rural–urban differences in life expectancy over time. These investigators also found poverty to have a significant impact on mortality within rural areas, noting a 6.2 years difference in the life expectancy between those residing in affluent rural areas compared to high poverty rural areas [18]. Findings from our study also suggest a gradient in selected outcomes as social and economic disadvantage progresses within rural communities.
We also found ACSC hospitalization to be much higher among racial/ethnic minority children and those with Medicaid or self-pay as an anticipated source of payment. These findings further contribute to the existing body of evidence documenting racial/ethnic disparities in important health related outcomes. Fortunately, ACSC hospitalizations remain a rare outcome event among children. When they do occur however, they can be serious and costly. The disproportionate burden among non-white children and those with Medicaid or self-pay has important cost implications for families, state Medicaid agencies, and providers. Previous estimates suggests that decreasing the hospitalization rate from ACSC by 5 % would result in a cost saving of more than $1.3 billion [1].
The study is not without weakness. The use of secondary data that is limited to a nine-state sample restricts the range of potential findings, because important factors associated with child health, such as parental education and socioeconomic status, are not available in discharge data. In addition, given the population estimates of the sample states, the relative contribution of individual states to observe outcomes may vary significantly. Although controlling for state level effects should address state influence, overall findings may more strongly reflect findings from the more populous states, while masking potentially important differences among the smaller states in the sample. Furthermore, given the geographic distribution of the states in the sample, the cultural underpinnings of rural communities, potentially related to available care and hospitalization decisions, across the states in the sample can be quite different.
Our study also has specific strengths. We were able to examine rural/urban disparities in ACSC hospitalizations among a large, representative sample of children 18 years of age. Although the relative contribution of each state to the total study population varies, the ability to examine this issue across a more broadly defined population is important for garnering a better understanding the current vulnerabilities at the macro level. In addition, the ability to characterize the intersection of multiple social determinants of health into a single index, as was done in this study, can be quite useful for rural health research in the future. Currently, no standard index for capturing area deprivation is widely used in practice; however, the measures used to comprise the index used in this study are among the most common [20]. Moreover, the index was derived from readily available, public data sources and is easily duplicated. The index proved to be quite useful for examining the effects of rurality in a way that could potentially be masked by incorporating important factors individually.
Policy Implications
The eventual impact of the ACA on effective primary care delivery for children remains unknown. The ability to characterize existing vulnerabilities of the primary care system for children and measure these changes over time is important. While our finding that ACSC hospitalizations among rural and urban children are comparable is encouraging, we did find evidence of a differential impact of rurality as area deprivation worsens. These findings suggest that vulnerabilities in the existing primary care system remain a salient theme among rural communities, particularly primarily high need communities. Observers have suggested that expanding insurance and decreasing financial barriers for receipt of health services will increase the demand for healthcare; simultaneously, the existing supply of providers remains constrained, as they struggle to accommodate new patients [21, 22]. Prior to the ACA, constrained supply was an existing hurdle for ensuring access to quality primary care services in rural and underserved communities. There is real concern that increasing demand for healthcare services stemming from the ACA could further exacerbate existing challenges in obtaining primary care in rural and underserved communities—particularly for children.
More recently, existing coverage of children though Medicaid and Child Health Insurance Programs (CHIP) has translated to comparable levels of insurance coverage for rural and urban children [10], but differences in the duration, entry, and exit of coverage may remain [23]. It is unlikely the demand for healthcare services from newly insured children will increase substantially with ACA implementation. However, the American Academy of Pediatrics (AAP) has noted that current pediatrician workforce is inadequate for rural and other underserved communities [24]. In the absence of pediatricians, children will now be competing with previously uninsured adults also seeking healthcare services from a limited provider base. It is plausible that access to care for children could be adversely affected by these changes, particularly in rural and underserved communities.
This research draws attention to this important issue and provides a methodological tool for monitoring the impact of these policies and ACA implementation continues. Future research that incorporates more states in the sample and examines the potential differences in ACSC among children in Medicaid expansion and non-expansion states is warranted.
References
Kruzikas D. T., Jiang, H. J., Remus, D., Barrett, M. L., Coffey, R. M., & Andrews, R. (2004). Preventable hospitalizations: A window into primary and preventive care 2000. Rockville, MD. Retrieved from http://archive.ahrq.gov/data/hcup/factbk5/factbk5.pdf.
Casey, M. (2007). Ambulatory care sensitive condition hospitalizations among rural children: UMRHRC Policy Brief. Minneapolis, MN. Retrieved from http://rhrc.umn.edu/wp-content/files_mf/caseyruralchildren.pdf.
Chevarley, F. M., Owens, P. L., Zodet, M. W., Simpson, L. A., McCormick, M. C., & Dougherty, D. (2006). Health care for children and youth in the United States: Annual report on patterns of coverage, utilization, quality, and expenditures by a county level of urban influence. Ambulatory Pediatrics, 6(5), 241–264. doi:10.1016/j.ambp.2006.06.004.
Garg, A., Probst, J. C., Sease, T., & Samuels, M. (2003). Potentially preventable care: Ambulatory care-sensitive pediatric hospitalizations in South Carolina in 2003. Southern Medical Journal, 96(9), 850–858.
Laditka, J. N., Laditka, S. B., & Probst, J. C. (2009). Health care access in rural areas: Evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health and Place, 15(3), 731–740. doi:10.1016/j.healthplace.2008.12.007.
Nayar, P., Nguyen, A. T., Apenteng, B., & Yu, F. (2012). Preventable hospitalizations: Does rurality or non-physician clinician supply matter? Journal of Community Health, 37(2), 487–494. doi:10.1007/s10900-011-9468-1.
Chen, L. W., Zhang, W., Sun, J., & Mueller, K. J. (2007). Regional variation in rural hospital charges due to ambulatory care sensitive conditions. Rural Policy Brief, (PB2007-5), 1–4.
Zhang, W., Mueller, K. J., & Chen, L. W. (2008). Uninsured hospitalizations: Rural and urban differences. Journal of Rural Health, 24(2), 194–202. doi:10.1111/j.1748-0361.2008.00158.x.
Knudson, A., Casey, M., Burlew, M., & Davidson, G. (2009). Disparities in pediatric asthma hospitalizations. Journal of Public Health Management and Practice, 15(3), 232–237.
Crosby, R., Monica, M. L., Vanderpool, R. C., & Casey, B. (2012). Rural populations and health: Determinants, disparities, and solutions. Hoboken: Wiley.
Rosano, A., Loha, C. A., Falvo, R., Van Der Zee, J., Ricciardi, W., Guasticchi, G., & De Belvis, A. G. (2013). The relationship between avoidable hospitalization and accessibility to primary care: A systematic review. European Journal of Public Health, 23(3), 356–360. doi:10.1093/eurpub/cks053.
Mclennan, D., Barnes, H., Noble, M., Davies, J., & Garratt, E. (2011). The English Indices of Deprivation 2010—Technical report. Social Policy. http://www.communities.gov.uk/publications/corporate/statistics/indices2010technicalreport.
Coevoet, V., Fresson, J., Vieux, R., & Jay, N. (2013). Socioeconomic deprivation and hospital length of stay: A new approach using area-based socioeconomic indicators in multilevel models. Medical Care. doi:10.1097/MLR.0b013e3182928f84.
Lu, S., & Kuo, D. Z. (2012). Hospital charges of potentially preventable pediatric hospitalizations. Academic Pediatrics, 12(5), 436–444. doi:10.1016/j.acap.2012.06.006.
Eibner, C., & Sturm, R. (2006). US-based indices of area-level deprivation: Results from healthcare for communities. Social Science and Medicine, 62(2), 348–359. doi:10.1016/j.socscimed.2005.06.017.
Fu, M., Exeter, D. J., & Anderson, A. (2015). “So, is that your ‘relative’ or mine?” A political-ecological critique of census-based area deprivation indices. Social Science and Medicine, 1(142), 27–36.
Baer, L. D., Johnson-Webb, K. D., & Gesler, W. M. (1997). What is rural? A focus on urban influence codes. The Journal of Rural Health, 13(4), 329–333.
Singh, G. K., & Siahpush, M. (2014). Widening rural-urban disparities in life expectancy, US, 1969–2009. American Journal of Preventive Medicine. doi:10.1016/j.amepre.2013.10.017.
Singh, G. K., & Siahpush, M. (2013). Widening rural–urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. Journal of Urban Health, 91(2), 272–292. doi:10.1007/s11524-013-9847-2.
Van Vuuren, C. L., Reijneveld, S. A., van der Wal, M. F., & Verhoeff, A. P. (2014). Neighborhood socioeconomic deprivation characteristics in child (0–18 years) health studies: A review. Health and Place. doi:10.1016/j.healthplace.2014.05.010.
Kirch, D. G., Henderson, M. K., & Dill, M. J. (2012). Physician workforce projections in an era of health care reform. Annual Review of Medicine. doi:10.1146/annurev-med-050310-134634.
Schwartz, M. D. (2012). Health care reform and the primary care workforce bottleneck. Journal of General Internal Medicine. doi:10.1007/s11606-011-1921-4.
Coburn, A. F., McBride, T. D., & Ziller, E. C. (2002). Patterns of health insurance coverage among rural and urban children. Medical Care Research and Review: MCRR, 59(3), 272–292. doi:10.1177/1077558702059003003.
Basco, W. T., & Rimsza, M. E. (2013). Pediatrician workforce policy statement. Pediatrics, 132(2), 390–397. doi:10.1542/peds.2013-1517.
Acknowledgments
Funding for this study was provided in part from the Federal Office of Rural Health Policy under a Cooperative Agreement with the South Carolina Rural Health Research Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hale, N., Probst, J. & Robertson, A. Rural Area Deprivation and Hospitalizations Among Children for Ambulatory Care Sensitive Conditions. J Community Health 41, 451–460 (2016). https://doi.org/10.1007/s10900-015-0113-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-015-0113-2