Abstract
Participation in gambling is rising in older adults. Indeed, in the coming years, engagement in gambling as a social activity is expected to increase more sharply in the elderly than in any other age group. Due to their exposure to powerful age-specific risk factors such as isolation, inactivity and failing health, older people are highly vulnerable to gambling-related problems. This study aimed to explore the existence of empirical clusters related to gambling habits in a sample of elderly participants from the general population. The sample included n = 361 participants, age range 50–90 years (mean 73.8, SD 8.4). Empirical clusters were identified through a two-step clustering analysis based on a broad set of indicators, including sociodemographic features, psychopathological state, substance use, life events, gambling preferences and scores on screening measures of gambling severity. The prevalence of GD in the study was 1.4%. Two clusters were identified: (a) cluster 1 (labeled as “low risk of gambling problems”, n = 265, 73.4%), which included the higher proportion of non-gamblers or individuals who engage only in non-strategic gambling, women, widowed, and lower levels of education (no individual into this group met criteria for GD); and (b) cluster 2 (labeled as “higher risk of gambling problems”, n = 96, 26.6%), which included the higher proportion of men, who reported both non-strategic and strategic gambling preferences (all participants diagnosed of GD were grouped into this cluster), older age, longer history of gambling, higher gambling severity, higher use of substances and worse psychopathological state. The elderly constitute a heterogeneous group with regard to gambling phenotypes. The results of this study may prove particularly useful for developing reliable screening tools able to identify older patients at a high risk of gambling problems, and for designing effective prevention and intervention programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gambling is a frequent recreational and social activity among older adults. In recent years its prevalence in this sector of the population has risen, establishing the elderly as a high-risk group for the development of gambling-related problems (Tse et al. 2012). A variety of motivations for initiating and/or maintaining gambling habits have been identified in older adults, including retirement, social isolation (especially distancing from family and friends, or reduced social contact), physical-mental diseases, or the loss of the partner (Clarke 2008; Kerber et al. 2008; Pattinson and Parke 2017). The combination of these elements often leads older adults to seek refuge in gambling activities as a form of entertainment and distraction which helps them to some extent to disconnect from their environment. In the elderly, monetary reward is rarely the motivation for gambling (Martin et al. 2011), and many older recreational gamblers present no negative impairment in their daily functioning. However, some elderly present gambling-related problems, and may even display clinical criteria for behavioral addictions such as gambling disorder (GD).
The definition of GD suggests a persistent and recurrent urge to gamble that causes clinical distress or impairment in family, professional or personal areas. The last edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (American Psychiatric Association 2013) classified GD under the heading of addictive disorders (in fact, GD is the only behavioral addiction in this group), since gambling has been shown to activate neurobiological systems similar to the ones affected in substance use disorders such as alcohol or drug abuse (Rash et al. 2016).
Studies in adult populations show that between 0.1 and 5.8% of the general population present gambling problems at the time of assessment, and that lifetime prevalence ranges between 1.1 and 10.6% (Calado and Griffiths 2016). However, epidemiological studies estimating the frequency of GD in the elderly population are scarce. Recent data indicate that its prevalence may be twice as high in young adults as in older adults (Abbott et al. 2018), but other studies obtained rates in older populations quite similar to those obtained in younger groups: specifically, around 50% of adults aged over 60 have a history of lifetime gambling, around 70% have gambled in the last 12 months, and around 2% are problem gamblers (Subramaniam et al. 2015; Tse et al. 2013). It has also been claimed that aging adults with severe gambling problems only perceive and recognize these difficulties when the more adverse consequences have already occurred—a situation that may result in an underestimation of the real prevalence of GD at these ages (Bischof et al. 2014) and, as a result, an under-prescription of professional treatment. The probability of high-risk behaviors related to gambling is likely to change over time, with increased rates among older adults expected due to their growing internet use and the ease of access to multiple platforms offering different forms of gambling activity (Abbott et al. 2018; Alberghetti and Collins 2015; Ioannidis et al. 2018; Sauvaget et al. 2015).
Regarding gambling preferences, there appear to be multiple reasons that lead particular individuals to select a preferred style of gambling (e.g., accessibility, availability, sex, age, academic level, or socio-economic status) (Lorains et al. 2014; Moragas et al. 2015). One of the primary factors is age. It is usual to group gambling activities into two broad categories: non-strategic (i.e., games which involve little or no decision-making or skill, and in which gamblers cannot influence the outcome, such as slot-machines, bingo and lotteries) versus strategic (games in which gamblers attempt to use their knowledge to influence or predict the outcome, such as poker, sports/animal betting or craps). In general, non-strategic gambling is associated with significantly older individuals, who tend to select low-skill, high-change gambling activities (Assanangkornchai et al. 2016; Grant et al. 2009; Nower and Blaszczynski 2008); however, other studies have obtained different profiles, identifying an association between older gamblers and higher rates of betting on horseracing (Subramaniam et al. 2015). These conflicting results highlight the need for additional empirical research in this area.
From an etiological perspective, GD is considered a multicausal behavioral addiction in which environmental, psychological and biological factors intervene and interact (Calado and Griffiths 2016). Centering on the older adult group, in addition to social and individual motivational factors preceding the behaviors (for example, social isolation or the desire to avoid unpleasant emotions), neurobiological agents have also been identified as potentially powerful age-specific risks for gambling-related problems and GD (Quintero 2016). The brain is known to become more vulnerable with age, in particular the frontal structures; this may lead to deficits in cognitive functioning, such as reasoning slowness. This age-related decline has been observed in the study of the neural correlates of cognitive processing during risky decision-making tasks, suggesting that older adults seem to be less able to shift attention from positive to negative information, a reluctance that may cause impaired neuropsychological performance (Boggio et al. 2010; Di Rosa et al. 2017). It has also been suggested that the decrease in cognitive performance during older age may be related both to a limited ability to gain explicit insight into the rules of ambiguous decision tasks and to the difficulty of choosing the less risky events after the rules have been fully understood (Schiebener and Brand 2017). The neuroanatomical and neurochemical changes in aging adults may also interact with dysfunctions in executive control; this possible interaction has been proposed as an additional risk factor for the emergence of gambling-related problems during old age in lifetime gamblers who had no such difficulties during early adulthood (McCarrey et al. 2012). In fact, some studies have found a relationship between lower scores on measures of executive functioning and higher levels of problem gambling in older adult samples, and correlates between gambling severity and higher levels of impulsivity only in individuals with cognitive deficits identified by screening tools (von Hippel et al. 2009). Cognitive distortions related to the illusion of control, probability control, and interpretive control have also been reported among older adult gamblers, and it has been suggested that these biases play a key role in both maintaining and increasing the severity of gambling behaviors (especially the self-perceived concept of luck, chasing wins/losses, miscalculating the win/loss ratio, superstitious beliefs and the perception that gambling is a skill) (Subramaniam et al. 2017).
Regarding the phenotype related to gambling habits in older adults, studies have suggested the existence of a range of profiles. From a longitudinal perspective, three primary groups can be identified (Welte et al. 2011): (a) a first group of individuals without a history of gambling or who gamble only irregularly and occasionally as a recreational activity, without any related impairment; (b) a second group who may have gambled sporadically, but due to age-related factors may be moderate-to-high risk for the development of GD due to their increased gambling in later life; and finally (c) a group of people with long-standing gambling behaviors (some of whom have had gambling-related problems at some point in their lives), who continue to gamble and present a chronic GD course. Three main pathways to late-life problematic gambling have also been identified (Tira et al. 2014): a grief pathway associated with unresolved losses, a habit pathway related to habituation to gambling, and a dormant pathway defined by high levels of impulsivity. In the area of the studies of the phenotypes, an age-by-gender interaction effect has also been found, suggesting that GD women do not begin gambling regularly until a mean age of 55 years, whereas older male gamblers usually report a lifetime history of gambling (Petry 2002). Other cross-cultural comparison studies have highlighted important differences in gambling progression, sociodemographic features, gambling-related behaviors and personal antecedents (Medeiros et al. 2015), lending support to the hypothesis of heterogeneity in the phenotype of gambling in aging adults. However, few studies have used statistical classification techniques to explore the existence of a gambling phenotype grouping in aging adults through statistical classification techniques. A pioneering clinical analysis using latent class techniques found that a two-class solution was the best for differentiating between lifetime and current problem gamblers (with the latter group recording worse self-rated health) (Hong et al. 2009). To our knowledge, no studies have been carried out to replicate this classification; nor have studies been performed with samples recruited from the general population.
Objectives
Aging adults are highly vulnerable to gambling problems, but little is known about the phenotype of gambling habits in this age group. The aim of this study was to explore the existence of empirical clusters which suggest heterogeneity in gambling activity profiles in a sample recruited from the general population aged between 50 and 90. Based on the available empirical evidence, we hypothesized that older people constitute a heterogeneous group in which subgroups of participants with different risk levels for gambling problems can be identified. Establishing the variables related to these empirical subcategories would facilitate the development of assessment tools with high discriminative capacity (including early detection measures) and the planning of effective prevention and treatment programs.
Methods
Participants
The study sample of this study pertained to a project aimed to compare gambling habits in older age between clinical and population-based individuals. In order to guarantee that participants were from the same geographical area, the clinical cohort was recruited from the Pathological Gambling Unit sited at the Bellvitge University Hospital, and the control cohort from the Podiatry and Dentistry Clinics on the same Bellvitge University Hospital campus, between November 2016 and February 2018. Previously, a collaboration agreement had been signed with the Podiatry and Dentistry Clinics to authorize patient recruitment. Inclusion criteria were age of 50 or over and sufficient cognitive capacity to complete the study’s self-report measures. Exclusion criteria were the presence of an organic mental disorder, intellectual disability, neurodegenerative disorder (such as Parkinson’s disease) or active psychotic disorder.
This study was carried out with the data recruited at the population based sample of the previous project, including n = 361 participants in the 50–90 year age range (mean age = 73.8 years, SD 8.4), 226 women (62.6%) and 135 men (37.4%). Age 50 was selected as the lower bound for classifying older adults based on the substantially variations in literature (usually from age 50+ to 70+ years).
Measures
Diagnostic Questionnaire for Pathological Gambling (According to DSM Criteria) (Stinchfield 2003)
This self-report identifies the presence of GD through 19 items which measure the DSM criteria [for the DSM-IV-TR (American Psychiatric Association 2010) and the DSM-5 versions (American Psychiatric Association 2013)]. The Spanish adaptation of this questionnaire has achieved good psychometric properties (Cronbach’s alpha α = 0.81 for the general population and α = 0.77 for clinical samples) (Jiménez-Murcia et al. 2009). This study assessed the total number of DSM-5 criteria for GD, as well as the classification of GD severity [(absent (0 criteria), problematic gambling (1–3 criteria), low (4–5 criteria), moderate (6–7 criteria) and severe (8–9 criteria)]. The internal consistency for this scale in the study sample was in the adequate range (α = 0.710).
South Oaks Gambling Severity Screen (SOGS) (Lesieur and Blume 1987)
This self-report questionnaire screens gambling-related problems through 20 items and provides a total score which is used as a measure of gambling severity. The Spanish validation of the scale’s questionnaire showed very good psychometric properties (test–retest reliability R = 0.98, internal consistency α = 0.94 and convergent validity R = 0.92) (Echeburúa et al. 1994). The internal consistency in the study sample was in the good range (α = 0.843).
Symptom Checklist-Revised (SCL-90-R) (Derogatis 1997)
This self-report tool measures the global psychological state through 90 items structured in nine primary (first order) dimensions (somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism) and three global indices (global severity index, GSI, total positive symptoms, PST, and positive symptoms discomfort index, PSDI). The Spanish version of this questionnaire has obtained good to adequate indices (mean α = 0.75) (Gonzalez De Rivera et al. 1989). The internal consistency in our sample was also in the good (α = 0.720 for the hostility scale) to excellent range (α = 0.954 for the global indices).
Life Events
A self-report questionnaire was developed for this study, with the aim of identifying lifetime exposure to traumatic events (including separation-divorce, death of close relatives, major financial problems, life-threatening accidents, physical-sexual abuse, physical assault, serious illness, etc.). Respondents were asked to report whether each event occurred (yes–no), the number of times it occurred, their age at the time of the event and the degree to which it affected them. The total number of cumulative life events was used. Internal consistency in the study sample was good (α = 0.740).
Other Variables
Additional data were registered through a semi-structured interview, including sociodemographic features (sex, education, and marital and employment status), the socioeconomic position according to Hollingshead’s index (which provides a global measurement based on the participants’ profession and level of education) (Hollingshead 2011), and other gambling problem-related variables (age of onset of the gambling behaviors, duration of gambling activity, bets per gambling/episode and debts accumulated due to gambling).
Procedure
The study was approved by the Ethics Committee of University Hospital of Bellvitge (Barcelona). Psychologists with extensive experience in GD collected the information of the semi-structured clinical interview, and they also helped the participants to complete the self-report tools in order to ensure that all the items were answered and that no data were missing due to lack of understanding. The evaluation process took place in a single session lasting about 45 min. The psychologists visited the waiting rooms of the Podiatry and Dentistry clinics (located inside the hospital) and asked patients if they were willing to participate in the study on a voluntary basis. Patients who accepted were given information sheets and were asked to provide signed informed consent before beginning the protocol. There was no financial or other compensation for being part of the sample of the study.
Statistical Analysis
Statistical analysis was carried out with SPSS24 for windows (IBM-Corp 2016). Empirical clustering was based on two-step cluster analysis, a method which allows exploration of the existence of natural groupings within a dataset of categorical and continuous variables, using an agglomerative hierarchical clustering method which allows automatic determination of the optimal number of groups [the log-likelihood distance and the Schwarz Bayesian Information Criterion (BIC) are used to determine the optimal number of clusters, choosing a solution with a reasonably large ratio of Schwarz Bayesian Information Criterion and a large ratio of distance measures]. The indicator variables in the clustering included sociodemographic features and other psychological and gambling-related variables: sex, age, education level, marital status, income, psychopathological state (SCL-90R GSI), substance use (tobacco, alcohol and other drugs), life events, gambling preference (non-gambling, only non-strategic, strategic and both) and gambling severity (number of DSM-5 criteria and SOGS total). The global consistency of the clustering was valued with the Silhouette index, in which values (in the range from −1 to +1) are interpreted as a measure of cohesion/separation (i.e., how similar individuals are to their own cluster compared to other clusters) (Rousseeuw 1987). High values in this index are indicative of adequate matching in one’s own cluster and of poor matching in other clusters (values lower than 0.30 are interpreted as poor fits, between 0.30 and 0.50 as fair, and higher than 0.50 as good).
The comparison between the empirical clusters for categorical variables was performed with Chi square tests (χ2) and the comparison between the quantitative variables with T TEST procedures. Effect sizes for the proportion and mean differences were based on the standardized Cohen’s-d coefficient, considering poor-low effect size for |d| > 0.20, moderate-medium for |d| > 0.5 and large-high for |d| > 0.80 (Kelley and Preacher 2012). In addition, Type-I errors due to the multiple statistical tests were controlled with Finner’s method (a stepwise familywise error rate procedure which offers a more powerful test than the classical Bonferroni correction) (Finner 1993).
Results
Characteristics of the Sample
Many participants in the study had lower than primary (n = 180, 49.9%) or primary (n = 129, 35.7%) levels of schooling; most were married (n = 223, 61.8%) or widowed (n = 110, 30.5%), retired (n = 354, 98.1%) and did not require social assistance (n = 339, 93.9%).
Regarding gambling problems, 356 participants (98.6%) did not present DSM-5 criteria for GD, while five participants (1.4%) were diagnosed with GD. Considering the gambling severity group based on the number of DSM-5 criteria for GD, 327 participants (90.6%) reported zero DSM-5 criteria, 29 participants (8.0%) presented 1–3 (indicative of problem gambling), one participant (0.3%) presented 4–5 (mild GD), and four (1.1%) presented 6–7 (moderate GD).
Clustering Procedure
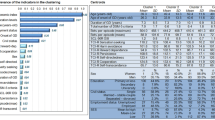
Table 1 includes the results of the auto-clustering, with the fitting coefficients used by the system to automatically select the most favorable model. The optimal number of clusters chosen by the system was two, since it achieved the largest ratio of distances measures (1.703) and the highest measure of cohesion/separation (Silhouette = 0.35). Since this solution also reported adequate clinical relevance, it was selected as the best for the data analysed in this study. Other solutions with a higher number of clusters were rejected since they achieved poorer fitting indexes, and they did not allowed better clinical interpretation.
Figure 1 displays the ordered bar-chart with the relative relevance weight of each indicator in the clustering process (with values in the range 0–1), which provides a measure of the discriminative capacity of each variable (the greater the relevance of the indicator, the less likely it is that changes between clusters for said variable are attributable to chance). In this study, the variable with greatest discriminative relevance (represented with darkest bar) was alcohol use. Participants’ sex, gambling subtype, gambling severity and income presented lower relevance; the variables with the lowest capacity for clustering were participants’ age, overall psychopathological state, use of illegal drugs, level of education, total number of life events and tobacco use.
Comparison Between Empirical Clusters
Table 2 displays the comparison between clusters for the sociodemographic and psychological measures of the study, while Table 3 shows the comparison for the gambling activity and gambling severity measures. These data provide a numerical summary of the phenotypes associated with each empirical cluster.
Cluster 1 comprised approximately three quarters of the sample (n = 265, 73.4%), and included the highest proportion of female participants, widowed, and individuals with lower levels of education. Participants in this cluster were also older, had lower income, reported fewer total number of life events, better psychopathological state and lower prevalence of substance use. Regarding the gambling profile, cluster 1 included mainly participants with no gambling activity or only non-strategic preference (predominantly lotteries), older age of onset, and shorter duration of gambling behavior, and lower gambling severity. None of these participants presented DSM-5 criteria for GD (96.2% reported zero criteria and 3.8% between one and three).
Cluster 2 (n = 96, 26.6%) included the highest proportion of men; subjects tended to be married, younger, with higher levels of education and higher incomes, higher mean number of cumulative life events, worse psychopathological states and higher prevalence of substance use. Regarding the gambling profile, this cluster included the highest proportion of participants engaging in both non-strategic and strategic gambling (lotteries and pools being the two preferred forms of gambling), younger age of onset, longer duration of the gambling activity and higher gambling severity. All the participants who met clinical criteria for GD were in cluster 2 (five in all, representing 5.2% of the individuals in the group).
Figure 2 displays the radar-plot with the main variables that showed differences between the empirical clusters, and thus represents a visual summary of the composition of the clusters obtained. Proportions for the categorical variables and z-standardized means for the quantitative variables are plotted (z-standardized values are shown, since the original scale differs for each variable and makes interpretation difficult). Based on the set of results in this study, cluster 1 is labeled “low risk of gambling problems” and cluster 2 “higher risk of gambling problems”.
Discussion
Through cluster analysis, this study explored the differences in the phenotype related to gambling habits in a sample of older adults recruited from the general population. The two-cluster solution was chosen as the best from a set of indicators which included sociodemographic variables, substance use, psychopathological state and scores on gambling assessment measures. Cluster 1 included 73.4% of the sample and grouped participants with a phenotype related to a low risk of gambling problems/severity. Cluster 2 contained the remaining 26.6% of the participants and comprised individuals with a phenotype more closely related to higher risk of gambling problems/severity.
In this study, 1.4% of participants met DSM-5 criteria for GD (4 or more criteria) while 8.0% were in the problem gambling group (between 1 and 3 criteria). These prevalences were within the range of worldwide cross-sectional estimates obtained in recent systematic reviews (from 0.12 to 5.8% for GD, and 0.7 to 7% for problem gambling) (Calado and Griffiths 2016). Centering on older adults (aged 50+), the lifetime prevalence of problem gambling ranges from 0.2 to 13%, and the prevalence during the past year between 0.3 and 10.4% (Tse et al. 2012). The high variation across studies (mostly related to methodological procedures, locations, samples, measurement instruments and time frames) highlights the need to examine the potential interrelations of many individual and sociocultural variables and their influences on gambling patterns in different age groups.
The variable with the highest impact on the clustering was alcohol use. In our study, the prevalence of alcohol use was 76.0% in cluster 2 (compared to 3.8% in cluster 1), suggesting that this variable is a powerful risk factor for the onset and/or progression of gambling-related problems in aging adults. Although less relevant for the clustering process, the prevalence of tobacco and illegal drug use were also significantly higher in cluster 2, and global psychopathological state (measured with the SCL-90R GSI) was worse in this class. Most empirical research in both clinical and community settings had obtained similar results, i.e., a strong association between gambling severity and the presence of poorer health status. In the study by Pietrzak et al. (2005) older adults with gambling disorder reported worse state of mental health than non-gamblers and infrequent gamblers, including higher levels of substance use, depression, anxiety and paranoid ideation. The epidemiological study by Assanangkornchai et al. (2016) in a sample of aging adults recruited from the general population obtained a prevalence of 57.4% for alcohol abuse, 49.5% for nicotine dependence and 16.2% for drug use in the subgroup of pathological gamblers, as well as a strong association between pathological gambling and a history of major depressive episodes. Other longitudinal research in older adults aged between 55 and 90 also found substance use disorder and anxiety disorders to be more frequent in high risk problem/pathological gamblers than in non-gamblers or low frequency gamblers (Pilver et al. 2013). In a sample of older adults with a history of lifetime pathological gambling, Kerber et al. (2008) found high levels of psychiatric comorbidity, including alcohol dependence, depression, and anxiety disorders. However, the role of mental disorders in problem gambling (that is, establishing the extent to which the presence of these comorbidities may act as predictors, moderators or mediators of gambling problems or be the result of these problems) is not clear. Studies based on pathway analysis had concluded that late-life problem gambling may be a way of escaping from anxiety and depression caused by impaired physical well-being and social isolation (Parke et al. 2018). Reports of higher levels of comorbid disorders related to GD in older adults than in younger populations had also been regarded as evidence of the potential role of psychological and physical state as early signs of the onset and/or evolution of the gambling problems (van der Maas et al. 2017). In any case, the higher relevance weight of alcohol use for the clustering found in our study (even higher than for gambling severity) indicates the importance of this variable as a powerful risk factor in the elderly, and suggests that education plans for the prevention of unhealthy habits in this sector of the population should include both alcohol use and gambling habits simultaneously.
As far as gambling preferences are concerned, high proportions of participants in our study reported non-gambling (35.5%) or only non-strategic gambling (46.0%) as their main gambling activity. This result was consistent with those of other studies evaluating preferences in aging adults, which have identified non-strategic gambling as the preferred form (Ariyabuddhiphongs 2012; Nower and Blaszczynski 2008; Subramaniam et al. 2015). Lotteries represented the most popular form of gambling in our study (60.4%), a point prevalence similar to the value obtained for lotteries among older adults (69.5%) in the study by Assanangkornchai et al. (2016). Also consistent with our results, the clinical study by Odlaug et al. (2011) found significantly higher proportions of women and of older people among non-strategic gamblers. In our sample, strategic games were less prevalent, with betting on sports (specifically football pools, in common with many other countries in Europe) being most popular form of this subtype in cluster 2 (32.3% compared to 7.2% in cluster 1). The association between the higher preference for strategic games in cluster 2 suggests that this gambling subtype may be a signal of higher risk of gambling- related problems, and this finding is consistent with those of other studies that have found significantly higher prevalences of GD among strategic gamblers and in both strategic plus non-strategic gamblers compared to non-strategic gamblers alone [7.3% vs. 2.1% in the study by Subramaniam (Subramaniam et al. 2016)].
Cluster 2 was of special interest because it included those individuals with higher risk of gambling problems (compared to cluster 1). But this cluster should not be interpreted as a disordered gambling group of moderate-to-high gambling severity, since the number of participants who really met clinical criteria for GD was very low. The clinical relevance of this cluster is the grouping of all GD individuals (as well as those with higher gambling level) and the linkage to the highest functional impairment. In fact, other variables defining the phenotype for cluster 2 were male sex, married status, higher level of education, younger age, higher income and higher number of cumulative life events. These variables had been related to a higher risk of gambling problems during aging in studies such as Subramaniam who found that older gamblers were more likely to be male, married, and with only primary or secondary education (Subramaniam et al. 2015). As regards the role of life events, findings in many studies stressed their importance as motivators and/or contributing features for gambling severity and gambling changes over time (Godinho et al. 2018). For example, problem gambling behaviors during adulthood was strongly associated with the presence of trauma in childhood (e.g., domestic violence or divorce) and with reporting life stressors in adulthood (e.g., intimate partner violence or severe economic hardship) (Roberts et al. 2017). Compared with healthy controls, patients who met clinical criteria for GD showed higher levels of post-traumatic stress symptoms (including higher physiological arousal sub-scores), and greater gambling severity was associated with stress-like emotional states in GD subsamples (Green et al. 2017). Cross-lagged analyses had also shown that the number of cumulative life events was related to increases in the severity of current problem gambling for at least the following 12 months, and that the concurrence of life events in several domains was also likely to be related over time to increases in the chronicity of risky gambling habits (Luce et al. 2016). Examining the contribution of specific life events to problem gambling and the related clinical implications, differences according to sex had also been highlighted (Bonnaire et al. 2016). Future research should aim to identify the different ways in which life events contribute to gambling habits during aging, including the possible sex-related differences.
Limitations
The first limitation of this study was that the analysis of cross-sectional data restricts the temporal analysis of causative associations. Future research should assess which risk factors lifespan increase the likelihood that elderly individuals belong to high-risk groups for GD, and how these higher-risk groups evolve during old age. Secondly, the low prevalence of GD involved that we could only explore variables related to clustering and therefore to the higher risk of gambling-related problems, and we could not generalize the results to the clinical settings of gamblers or to identify risk factors related to the onset and/or the chronicity of the GD. The low frequency of GD in the study (although being consistent with the point prevalence estimates in population-based samples) did not allow obtaining a cluster of patients with moderate to high affectation due to the gambling activity. Finally, the lack of data regarding physical aspects of the aging process (such as the use of medical services or medication, the assessment of overall health status and/or chronic conditions) prevents us from establishing their distribution in the empirical clusters and from estimating their potential relation to gambling problems/severity.
Conclusion and Implications
For many older adults, gambling is a recreational behavior perceived as an entertaining occupation, an exciting/stimulating activity for relieving boredom and escaping from social isolation, and a way for coping with stress or emotional difficulties. These older adults are able to enjoy gambling without problems. However, prevalence studies warn that gambling may entail clinically significant problems among some older adults due their exposure to age-specific risk factors for GD, which make them an especially vulnerable population. The prevalence of GD is expected to rise in the coming years, mainly due to the proliferation of new gambling platforms on the Internet, the ease of access to these new systems and the increasing familiarity of aging adults with the use of new technologies. One of the biggest difficulties in detecting/diagnosing gambling-related problems is that behavioral addictions such as GD can go unnoticed in older people, who may be less likely to recognize gambling as a potential problem. Our study highlighted some potential risks related to gambling habits in aging adults, and our findings may be of help in the development of valid and reliable screening tools and effective programs for preventing the onset/evolution of GD and potential comorbid secondary disorders.
This study identified a phenotype characterized by elderly individuals who, in addition to alcohol and tobacco consumption, emotional distress problems and stressful life-events, presented a greater risk of gambling problems. Given that these are often people in situations of relative loneliness and isolation, primary care physicians and/or geriatricians and nurses should routinely explore this issue. Ideally, health campaigns aimed at older people regarding issues such as diet, physical exercise, sleep and so on should also include recommendations on gambling in order to minimize the risk of developing gambling-related problems.
References
Abbott, M., Hodgins, D. C., Bellringer, M., Vandal, A. C., Palmer Du Preez, K., Landon, J., et al. (2018). Brief telephone interventions for problem gambling: A randomized controlled trial. Addiction,113(5), 883–895. https://doi.org/10.1111/add.14149.
Alberghetti, A., & Collins, P. A. (2015). A passion for gambling: A generation-specific conceptual analysis and review of gambling among older adults in Canada. Journal of Gambling Studies,31(2), 343–358. https://doi.org/10.1007/s10899-013-9425-2.
American Psychiatric Association. (2010). Diagnostic and statistical manual of mental disorders (4th Rev). Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington DC: Author.
Ariyabuddhiphongs, V. (2012). Older adults and gambling: A review. International Journal of Mental Health and Addiction,10(2), 297–308. https://doi.org/10.1007/s11469-011-9325-6.
Assanangkornchai, S., McNeil, E. B., Tantirangsee, N., Kittirattanapaiboon, P., & Thai National Mental Health Survey Team. (2016). Gambling disorders, gambling type preferences, and psychiatric comorbidity among the Thai general population: Results of the 2013 National Mental Health Survey. Journal of Behavioral Addictions,5(3), 410–418. https://doi.org/10.1556/2006.5.2016.066.
Bischof, A., Meyer, C., Bischof, G., Guertler, D., Kastirke, N., John, U., et al. (2014). Association of sociodemographic, psychopathological and gambling-related factors with treatment utilization for pathological gambling. European Addiction Research,20(4), 167–173. https://doi.org/10.1159/000356904.
Boggio, P. S., Campanhã, C., Valasek, C. A., Fecteau, S., Pascual-Leone, A., & Fregni, F. (2010). Modulation of decision-making in a gambling task in older adults with transcranial direct current stimulation. European Journal of Neuroscience,31(3), 593–597. https://doi.org/10.1111/j.1460-9568.2010.07080.x.
Bonnaire, C. L., Kovess, V., Guignard, R., Richard, J.-B., Du-Roscoat, E., & Beck, F. O. (2016). Life events, substance use, psychological distress, and quality of life in male and female French gamblers. Annals of Clinical Psychiatry: Official Journal of the American Academy of Clinical Psychiatrists,28(4), 263–279.
Calado, F., & Griffiths, M. D. (2016). Problem gambling worldwide: An update and systematic review of empirical research (2000–2015). Journal of Behavioral Addictions,5(4), 592–613. https://doi.org/10.1556/2006.5.2016.073.
Clarke, D. (2008). Older adults’ gambling motivation and problem gambling: A comparative study. Journal of Gambling Studies,24(2), 175–192. https://doi.org/10.1007/s10899-008-9090-z.
Derogatis, L. R. (1997). SCL-90-R. Cuestionario de 90 síntomas. Madrid: TEA Ediciones.
Di Rosa, E., Mapelli, D., Arcara, G., Amodio, P., Tamburin, S., & Schiff, S. (2017). Aging and risky decision-making: New ERP evidence from the Iowa Gambling Task. Neuroscience Letters,640, 93–98. https://doi.org/10.1016/j.neulet.2017.01.021.
Echeburúa, E., Báez, C., Fernández, J., & Páez, D. (1994). Cuestionario de juego patológico de South Oaks (SOGS): Validación española (South Oaks Gambling Screen (SOGS): Spanish validation). Análisis de Modificación de Conducta,20, 769–791.
Finner, H. (1993). On a monotonicity problem in step-down multiple test procedures. Journal of the American Statistical Association,88, 920–923. https://doi.org/10.1080/01621459.1993.10476358.
Godinho, A., Kushnir, V., Hodgins, D. C., Hendershot, C. S., & Cunningham, J. A. (2018). Betting on life: Associations between significant life events and gambling trajectories among gamblers with the intent to quit. Journal of Gambling Studies,34(4), 1391–1406. https://doi.org/10.1007/s10899-018-9767-x.
Gonzalez De Rivera, J. L., Derogatis, L. R., De las Cuevas, C., Gracia Marco, R., Rodríguez-Pulido, F., Henry-Benitez, M., et al. (1989). The Spanish version of the SCL-90-R. Normative data in the general population. Towson: Clinical Psychometric Research.
Grant, J. E., Kim, S. W., Odlaug, B. L., Buchanan, S. N., & Potenza, M. N. (2009). Late-onset pathological gambling: Clinical correlates and gender differences. Journal of Psychiatric Research,43(4), 380–387. https://doi.org/10.1016/j.jpsychires.2008.04.005.
Green, C. L., Nahhas, R. W., Scoglio, A. A., & Elman, I. (2017). Post-traumatic stress symptoms in pathological gambling: Potential evidence of anti-reward processes. Journal of Behavioral Addictions,6(1), 98–101. https://doi.org/10.1556/2006.6.2017.006.
Hollingshead, A. B. (2011). Four factor index of social status. Yale Journal of Sociology,8, 21–51.
Hong, S.-I., Sacco, P., & Cunningham-Williams, R. M. (2009). An empirical typology of lifetime and current gambling behaviors: Association with health status of older adults. Aging & Mental Health,13(2), 265–273. https://doi.org/10.1080/13607860802459849.
IBM-Corp. (2016). IBM SPSS statistics for windows, version 24.0. Arkmonk, NY: IBM Corp.
Ioannidis, K., Treder, M. S., Chamberlain, S. R., Kiraly, F., Redden, S. A., Stein, D. J., et al. (2018). Problematic internet use as an age-related multifaceted problem: Evidence from a two-site survey. Addictive Behaviors,81, 157–166. https://doi.org/10.1016/j.addbeh.2018.02.017.
Jiménez-Murcia, S., Stinchfield, R., Alvarez-Moya, E., Jaurrieta, N., Bueno, B., Granero, R., et al. (2009). Reliability, validity, and classification accuracy of a Spanish translation of a measure of DSM-IV diagnostic criteria for pathological gambling. Journal of Gambling Studies,25(1), 93–104. https://doi.org/10.1007/s10899-008-9104-x.
Kelley, K., & Preacher, K. J. (2012). On effect size. Psychological Methods,17(2), 137–152. https://doi.org/10.1037/a0028086.
Kerber, C. S., Black, D. W., & Buckwalter, K. (2008). Comorbid psychiatric disorders among older adult recovering pathological gamblers. Issues in Mental Health Nursing,29(9), 1018–1028. https://doi.org/10.1080/01612840802274933.
Lesieur, H. R., & Blume, S. B. (1987). The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry,144(9), 1184–1188. https://doi.org/10.1176/ajp.144.9.1184.
Lorains, F. K., Dowling, N. A., Enticott, P. G., Bradshaw, J. L., Trueblood, J. S., & Stout, J. C. (2014). Strategic and non-strategic problem gamblers differ on decision-making under risk and ambiguity. Addiction,109(7), 1128–1137. https://doi.org/10.1111/add.12494.
Luce, C., Kairouz, S., Nadeau, L., & Monson, E. (2016). Life events and problem gambling severity: A prospective study of adult gamblers. Psychology of Addictive Behaviors,30(8), 922–930. https://doi.org/10.1037/adb0000227.
Martin, F., Lichtenberg, P. A., & Templin, T. N. (2011). A longitudinal study: Casino gambling attitudes, motivations, and gambling patterns among urban elders. Journal of Gambling Studies,27(2), 287–297. https://doi.org/10.1007/s10899-010-9202-4.
McCarrey, A. C., Henry, J. D., von Hippel, W., Weidemann, G., Sachdev, P. S., Wohl, M. J. A., et al. (2012). Age differences in neural activity during slot machine gambling: An fMRI study. PLoS ONE,7(11), e49787. https://doi.org/10.1371/journal.pone.0049787.
Medeiros, G. C., Leppink, E., Yaemi, A., Mariani, M., Tavares, H., & Grant, J. (2015). Gambling disorder in older adults: A cross-cultural perspective. Comprehensive Psychiatry,58, 116–121. https://doi.org/10.1016/j.comppsych.2014.12.021.
Moragas, L., Granero, R., Stinchfield, R., Fernández-Aranda, F., Fröberg, F., Aymamí, N., et al. (2015). Comparative analysis of distinct phenotypes in gambling disorder based on gambling preferences. BMC Psychiatry,15(1), 86. https://doi.org/10.1186/s12888-015-0459-0.
Nower, L., & Blaszczynski, A. (2008). Characteristics of problem gamblers 56 years of age or older: A statewide study of casino self-excluders. Psychology and Aging,23(3), 577–584. https://doi.org/10.1037/a0013233.
Odlaug, B. L., Marsh, P. J., Kim, S. W., & Grant, J. E. (2011). Strategic vs nonstrategic gambling: Characteristics of pathological gamblers based on gambling preference. Annals of Clinical Psychiatry,23(2), 105–112.
Parke, A., Griffiths, M., Pattinson, J., & Keatley, D. (2018). Age-related physical and psychological vulnerability as pathways to problem gambling in older adults. Journal of Behavioral Addictions,7(1), 137–145. https://doi.org/10.1556/2006.7.2018.18.
Pattinson, J., & Parke, A. (2017). The experience of high-frequency gambling behavior of older adult females in the United Kingdom: An interpretative phenomenological analysis. Journal of Women & Aging,29(3), 243–253. https://doi.org/10.1080/08952841.2015.1138047.
Petry, N. M. (2002). A comparison of young, middle-aged, and older adult treatment-seeking pathological gamblers. The Gerontologist,42(1), 92–99.
Pietrzak, R. H., Molina, C. A., Ladd, G. T., Kerins, G. J., & Petry, N. M. (2005). Health and psychosocial correlates of disordered gambling in older adults. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry,13(6), 510–519. https://doi.org/10.1176/appi.ajgp.13.6.510.
Pilver, C. E., Libby, D. J., Hoff, R. A., & Potenza, M. N. (2013). Problem gambling severity and the incidence of Axis I psychopathology among older adults in the general population. Journal of Psychiatric Research,47(4), 534–541. https://doi.org/10.1016/j.jpsychires.2012.12.013.
Quintero, G. (2016). A biopsychological review of gambling disorder. Neuropsychiatric Disease and Treatment,13, 51–60. https://doi.org/10.2147/NDT.S118818.
Rash, C., Weinstock, J., & Van Patten, R. (2016). A review of gambling disorder and substance use disorders. Substance Abuse and Rehabilitation,7, 3–13. https://doi.org/10.2147/SAR.S83460.
Roberts, A., Sharman, S., Coid, J., Murphy, R., Bowden-Jones, H., Cowlishaw, S., et al. (2017). Gambling and negative life events in a nationally representative sample of UK men. Addictive Behaviors,75, 95–102. https://doi.org/10.1016/j.addbeh.2017.07.002.
Rousseeuw, P. J. (1987). Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. Journal of Computational and Applied Mathematics,20, 53–65. https://doi.org/10.1016/0377-0427(87)90125-7.
Sauvaget, A., Jiménez-Murcia, S., Fernández-Aranda, F., Fagundo, A. B., Moragas, L., Wolz, I., et al. (2015). Unexpected online gambling disorder in late-life: A case report. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2015.00655.
Schiebener, J., & Brand, M. (2017). Age-related variance in decisions under ambiguity is explained by changes in reasoning, executive functions, and decision-making under risk. Cognition and Emotion,31(4), 816–824. https://doi.org/10.1080/02699931.2016.1159944.
Stinchfield, R. (2003). Reliability, validity, and classification accuracy of a measure of DSM-IV diagnostic criteria for pathological gambling. American Journal of Psychiatry,160(1), 180–182. https://doi.org/10.1176/appi.ajp.160.1.180.
Subramaniam, M., Abdin, E., Vaingankar, J. A., Shahwan, S., Picco, L., & Chong, S. A. (2016). Strategic versus nonstrategic gambling: Results from a community survey. Journal of Addiction Medicine,10(3), 174–181. https://doi.org/10.1097/ADM.0000000000000211.
Subramaniam, M., Chong, S. A., Browning, C., & Thomas, S. (2017). Cognitive distortions among older adult gamblers in an Asian context. PLoS ONE,12(5), e0178036. https://doi.org/10.1371/journal.pone.0178036.
Subramaniam, M., Wang, P., Soh, P., Vaingankar, J. A., Chong, S. A., Browning, C. J., et al. (2015). Prevalence and determinants of gambling disorder among older adults: A systematic review. Addictive Behaviors,41, 199–209. https://doi.org/10.1016/j.addbeh.2014.10.007.
Tira, C., Jackson, A. C., & Tomnay, J. E. (2014). Pathways to late-life problematic gambling in seniors: A grounded theory approach. The Gerontologist,54(6), 1035–1048. https://doi.org/10.1093/geront/gnt107.
Tse, S., Hong, S.-I., & Ng, K.-L. (2013). Estimating the prevalence of problem gambling among older adults in Singapore. Psychiatry Research,210(2), 607–611. https://doi.org/10.1016/j.psychres.2013.06.017.
Tse, S., Hong, S.-I., Wang, C.-W., & Cunningham-Williams, R. M. (2012). Gambling behavior and problems among older adults: A systematic review of empirical studies. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences,67(5), 639–652. https://doi.org/10.1093/geronb/gbs068.
van der Maas, M., Mann, R. E., McCready, J., Matheson, F. I., Turner, N. E., Hamilton, H. A., et al. (2017). Problem gambling in a sample of older adult casino gamblers. Journal of Geriatric Psychiatry and Neurology,30(1), 3–10. https://doi.org/10.1177/0891988716673468.
von Hippel, W., Ng, L., Abbot, L., Caldwell, S., Gill, G., & Powell, K. (2009). Executive functioning and gambling: Performance on the trail making test is associated with gambling problems in older adult gamblers. Neuropsychology, Development, and Cognition,16(6), 654–670. https://doi.org/10.1080/13825580902871018.
Welte, J. W., Barnes, G. M., Tidwell, M.-C. O., & Hoffman, J. H. (2011). Gambling and problem gambling across the lifespan. Journal of Gambling Studies,27(1), 49–61. https://doi.org/10.1007/s10899-010-9195-z.
Acknowledgments
This manuscript and research were supported by grants from the Ministerio de Economía y Competitividad (PSI2015-68701-R). The research was funded by the Delegación del Gobierno para el Plan Nacional sobre Drogas (2017I067), Instituto de Salud Carlos III (ISCIII) (FIS PI14/00290 and PI17/01167) and co-funded by FEDER funds/European Regional Development Fund (ERDF), a way to build Europe. CIBERobn and CIBERSAM are both initiatives of ISCIII. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Support was received from the Secretariat for Universities and Research of the Ministry of Business and Knowledge of the Government of Catalonia. TMM, CVA and MLM are supported by a predoctoral grant awarded by the Ministerio de Educación, Cultura y Deporte (FPU16/02087; FPU16/01453; FPU15/02911). We thank the CERCA Programme/Generalitat de Catalunya for institutional support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Ethical Approval
All procedures were carried in accordance with the Declaration of Helsinki. This research was approved by the Ethics Committee of the Bellvitge University Hospital (Ref: PR286/14).
Informed Consent
All subjects were informed about the study and all provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.