Abstract
We developed and pilot-tested the first online psycho-educational intervention that specifically targets people with a family history of depression (‘LINKS’). LINKS provides genetic risk information and evidence-rated information on preventive strategies for depression and incorporates a risk assessment tool and several videos using professional actors. LINKS was pilot-tested in the general practitioner (GP) setting. The patient sample included people with a family history of at least one first-degree relative (FDR) with major depressive disorder (MDD) or bipolar disorder (BD). Patients attending participating GP practices were invited to enroll in the study by letter from their GP. Patients who self-identified as having at least one first-degree relative (FDR) with MDD or BD were eligible. Patients completed questionnaires, pre-post viewing LINKS, with measures assessing satisfaction, relevance, emotional impact and perceived improvement of understanding. Six GP practices participated, and 24 patients completed both questionnaires. Of these, all reported that they were satisfied or very satisfied with LINKS, and 74 % reported that LINKS met their expectations, and 21 % that it exceeded their expectations. LINKS was judged highly acceptable by this sample of GP attendees, and results indicate that an assessment of its effectiveness in a larger controlled trial is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Having a family history of depression is the strongest documented risk factor for onset of depression (Sullivan et al. 2000). Family, twin, and adoption studies strongly suggest that both major depressive disorder (MDD) and bipolar disorder (BD) have heritable components, with heritability estimates of about 40 % for MDD (Sullivan et al. 2000) and 80 % to 90 % for BD (Kieseppa et al. 2004). A recent meta-analysis of cohort and case-control studies showed that having one first-degree relative (FDR) with MDD increases the risk of having MDD, with an odds ratio (OR) = 2.1, compared to healthy controls. This risk estimate increases to OR = 3.2 if the proband has two FDRs with MDD (Wilde et al. 2014). The same meta-analysis found that having one FDR with BD increased the risk of having BD with an OR = 7.9 compared to healthy controls (Wilde et al. 2014).
Many individuals with a family history of depression are concerned about their risks of developing MDD and/or BD and the risks to their offspring. They report a range of unmet educational and psychological support needs in relation to their familial risk. In a study of the unmet psycho-educational needs of adults and siblings of adults with BD, the relevance of education on how BD can be prevented, recognition of early symptoms, and risk modification, particularly in young relatives, was highlighted (Peay et al. 2009). Similarly, in a recent study of the information needs and preferences of people at increased familial risk for MDD (Quinn et al. 2014), individuals reported a need for information about MDD’s etiology and development, reproductive decision-making, early detection of symptoms and risk-reducing strategies. Nearly all participants expressed an interest in risk assessment. The most preferred way to access depression information was via the Internet (87 % of participants) (Quinn et al. 2014).
The Internet is perhaps the most efficient method of reaching a large and growing number of individuals living in both urban and rural settings, and it allows for the automated delivery of tailored information, such as personalized risk estimates. Several high-quality websites delivering therapy for, and education about, depression have been developed both in Australia and internationally, e.g. www.beyondblue.org.au, www.bluepages.anu.edu.au. The effectiveness of websites that deliver therapy for depression has been demonstrated (Donker et al. 2009). Evidence is also available that online interventions focused on ‘depression literacy’ (Jorm et al. 2006) are as effective as those delivering online cognitive behavioral therapy in reducing the symptoms of depression (Mackinnon et al. 2008). Although a small number of studies of face-to-face preventative psychological interventions for those with a family history of MDD have been published, e.g. Beardslee et al. (2013), to the best of our knowledge, no online interventions are available that specifically target people with a family history of depression, despite the well-documented unmet psycho-educational needs of this at-risk group (Peay et al. 2009; Quinn et al. 2014).
Studies on unmet psycho-educational needs demonstrate that people at familial risk prioritize information on strategies which they or their offspring might use to reduce risk of depression onset (Peay et al. 2009; Quinn et al. 2014). There have been calls for more widespread promotion and implementation of evidence–based depression prevention approaches in the general population (Cuijpers et al. 2012; Munoz et al. 2010; Barrera et al. 2007; Barrera et al. 2012), also referred to as ‘universal interventions’ (Barrera et al. 2007). The benefits of implementation of risk-reducing strategies are perhaps an even greater priority for individuals at familial risk. Such individuals are at the highest level of disease burden where the potential benefits of risk-reducing strategies are greatest; thus they are likely to benefit from ‘targeted interventions’ (Barrera et al. 2007).
There is strong evidence from meta-analyses synthesizing the results from randomized controlled trials (RCTs) that prevention trials can be highly effective in reducing the occurrence of new cases of depression (Barrera et al. 2007; Cuijpers et al. 2012). Several trials involved the Internet and demonstrated the effectiveness of Internet-based approaches (Ebert et al. 2015; Andersson and Hedman 2013). Studies show that cognitive behavioral and other psychological therapies are particularly effective in people with a family history of depression (Cuijpers et al. 2008; Marry et al. 2004; Barrera et al. 2007; Beardslee et al. 2013; Cuijpers et al. 2011). Such therapies have been shown to reduce the risk of depression, and in groups with a higher risk of developing MDD, therapy can almost halve the chance of it developing (Cuijpers et al. 2008; Marry et al. 2004; Barrera et al. 2007; Garber et al. 2009; Clarke et al. 2001).
Aside from cognitive behavioral and other psychological therapies, a range of lifestyle factors may influence depression risk and thus have preventative potential. These include regular physical activity, e.g. Larun et al. (2006); minimizing alcohol (in heavy drinkers) and avoiding street drugs, e.g. Davis et al. (2008); ensuring adequate amounts of sleep, e.g. Perlman et al. (2006); eating a Mediterranean diet, e.g. Skarupski et al. (2013); and ensuring adequate levels of Vitamin D, e.g. Berk et al. (2007). A number of psychosocial characteristics have also been identified as being linked to decreased risk of depression, in particular having good social support, e.g. Stice et al. (2004), and being optimistic, e.g. Seligman et al. (2005). Prospective studies are also available that show the risk of developing depression is lower in those who are religious and/or spiritual when compared to those who are not; this includes studies specifically performed in people with a family history of depression (Jacobs et al. 2012; Kasen et al. 2012). In summary, there is substantial evidence that supports the value of a range of strategies, including psychological therapies, life style factors and psychosocial strategies, in reducing the risk of depression onset. These strategies may be used to reduce risk of depression; however those at-risk need to be informed about such strategies.
Study Objectives
This study aimed to pilot-test the first online tailored psycho-educational intervention targeted to individuals with a family history of depression to provide such individuals in a general practice setting with education about familial risk for depression. The intervention offered ‘depression literacy’, including education on evidence-based prevention and treatment strategies; it was not designed to provide therapy to prevent or treat depression. The intervention also incorporated a risk assessment tool to provide tailored risk estimates, delivery of education targeted to people with a family history of depression and feedback to general practitioners (GPs) of individuals’ risk status. The pilot study will be followed by a cluster RCT, the methodology of which has been described in detail (Meiser et al. 2013).
Methods
Development of Website Content
A psycho-educational website, LINKS, targeting people with a family history of depression was developed, using our study of the information needs and preferences of people at increased familial risk as the basis for the development of website content (Quinn et al. 2014). Accordingly, information was included on: the likelihood of depression occurring, early signs and symptoms of depression, and the environmental and genetic risk factors such as stress and lifestyle factors, amongst other topics. The early prototypes were developed with a multidisciplinary committee, including researchers and clinicians with expertise in psychiatry, psychiatric genetics, psychology, general practice, e-medicine in the psychiatry setting, genetic counseling, and genetics education; the team also included a consumer representative. The website is available for viewing at the following URL: http://www.links.neura.edu.au.
The intervention consists of 50 screens and eight embedded videos. Information is provided on MDD and BD symptoms; family history of depression; multi-generational family history of MDD and/or BD; the role of individual and shared environmental factors and genetic factors in depression development; differences in genetic information and depression risk; risk factors for recurrence of depression; the effects of stressful life events in people with a family history of depression; prevention strategies; family history of depression and suicide; childbearing decisions; depression and stigma; family history of depression and stigma; as well as early detection and early intervention strategies.
Unique Features of Website
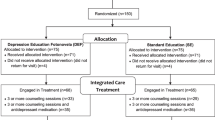
Visual Illustrations
As much as possible, visual illustrations were used to convey key concepts; for example, the jar model of genetic susceptibility, adapted from Austin and Peay (Peay and Austin 2011), as shown in Fig. 1, and the one hundred people diagrams used for the risk assessment tool (Fig. 2). In Australia, the recommended reading level is 8th grade (National Health and Medical Research Council 1999). Despite the team’s best efforts in trying to further reduce the readability level, the final version of the intervention was 9th grade reading level.
Mental illness jar model illustration adapted from Peay and Austin (2011)
Section on Rating of Evidence-Based Prevention Strategies
In our earlier research (Quinn et al. 2014), we found that many at-risk individuals felt that educational resources should provide information as to how to reduce the likelihood of depression occurring both for themselves and their family. Accordingly, literature searches were undertaken to identify strategies shown to prevent depression specifically in people at increased familial risk as well as the general population. The aim was to identify risk-reducing strategies supported both by a strong evidence basis such as RCTs as well as those supported by weaker evidence, e.g. cross-sectional epidemiological studies. Sufficient details were extracted from identified studies to allow the evidence base to be rated according to the methodological rigor of the evidence supporting each strategy. Each risk prevention strategy was evidence-rated by MP and ratings were reviewed by the whole team, with an increasing number of ticks (√) indicating greater methodological rigor. Any discrepancies in ratings were resolved through discussion. Four ticks indicate a large number of RCTs and associated meta-analyses, which show reductions of depression symptoms; three ticks indicate some RCT evidence and/or availability of prospective studies, which correlate changes in an intervention with depression prevention or between strategies and depression development; two ticks, cross-sectional and epidemiological studies; and one tick, evidence-based treatments for depression with unknown efficacy in prevention. Accordingly ‘Psychological strategies’ were rated four ticks, regular physical activity three ticks, getting adequate amount of sleep two ticks; and the following strategies received one tick each: Mediterranean-style diet, minimizing alcohol (in heavy drinkers), avoiding drug use, good social support, optimism/having a positive attitudes, and being religious or spiritual.
Risk Assessment Tool
To provide the basis for the tailored risk estimates provided by the website, we conducted a meta-analysis to estimate the incidence of MDD and BD in FDRs of probands affected by MDD or BD (Wilde et al. 2014). The meta-analysis provides estimates of the risk for MDD or BD for relatives associated with having: (i) one FDR with MDD or BD (two analyses); (ii) two FDRs with MDD or BD (two analyses); and (iii) pooled data for FDRs and probands with either MDD or BD. Unfortunately, too few papers reported effect sizes for second-degree relatives and thus the risk estimates provided by LINKS do not take into account second-degree relatives with MDD or BD.
The risk assessment tool allows the user to enter input to visualize lifetime risks and risks over the next year of MDD or BD relative to the general population, for a person with either one parent or sibling with MDD or two FDRs with MDD; the risk of developing BD for person with either one parent or sibling or two FDRs with BD; and the risk of developing BD for person with one parent or sibling with MMD and vice versa. In total 12 different risks scenarios can be visualised (see Fig. 2 for an example).
Video Vignettes
Vignettes of four hypothetical people with a family history of MDD or BD were developed and professional actors and a professional film producer engaged to produce eight embedded videos, ranging from 4 to 7 min in length, which were arranged thematically throughout LINKS, as well as two videos featuring well known experts. Four actors portrayed two people with a personal diagnosis of either MDD or BD, and two without a personal diagnosis but with a family history of depression.
Participants
Recruitment of GP practices: GP practices were located across Greater Sydney and GPs were identified using an existing GP database. GPs were sent letters of invitation and were offered a AUD$1500 reimbursement per practice and 40 individual Continuing Medical Education points as an acknowledgement of the time commitments required to participate in the study. Those returning an expression of interest form were contacted to arrange a meeting to discuss the study. The research team provided personalized academic detailing, which included an explanation of the study materials and obtaining GPs’ written consent to participate.
Recruitment of patients: Patients were eligible to participate if they: (i) had a family history of at least one FDR with MDD or BD; (ii) were able to give informed consent; (iii) were proficient readers in English; (iii) were aged between 18 and 75 years; and, (iv) were deemed fit by their GP to participate. Patients attending participating GP practices who met the eligibility criteria were invited to the study by their GP. As many GPs do not elicit and systematically record a family history of depression, patients were asked to self-identify as having a FDR with MDD or BD. Individuals who have had an episode of MDD or BD, and those who have not, were eligible to participate.
Procedures
The pilot study received ethics approval from the institutional review board of the University of New South Wales. Researchers worked with staff at GP practices to generate random lists of up to 500 patients per practice who met eligibility criteria (i) to (iv) above. The expectation was that about 20 % of attendees would have at least one first-degree relative with either MDD or BD (Department of Health and Ageing 2013), and, based on similar work involving the testing of a cancer family history assessment tool, it was estimated that approximately 15 % of patients would opt-in to an online trial following an invitation letter from their GP (Trevena et al. 2006). By contacting up to 500 patients for each GP practice, a recruitment rate of up to 15 participants per practice was anticipated.
GPs were asked to screen these randomly selected patients and exclude those who would not be suitable (e.g. cognitive impairment, severe illness, patients with a psychiatric disorder that is currently not well controlled); those deemed suitable were sent a letter of invitation by their GP. The letter invited those who self-identified as having at least one FDR with depression to enter the LINKS website.
Instrumentation
Baseline measures: Each patient entering the website was asked to complete the Family History Screen (FHS) (Weissman et al. 2000) to confirm eligibility (in particular whether they had a FDR with MDD or BD) and provide the basis for feedback to the participants, and optionally their GP, regarding their family history details, including whether they have had an episode of MDD or BD and brief details regarding their family history. The FHS is a valid and reliable measure of psychiatric family history and has been shown to have high sensitivity and specificity for depression (Weissman et al. 2000). It identifies the status of the FDRs for assessment (pedigree collection) and screens lifetime history of MDD and/or BD of the participant and the biological relatives identified in the pedigree. The FHS begins with a broadly sensitive introductory question about the participant and any FDR to stimulate memory. If the status of any family members is provided in response to the first question, an additional five narrower ‘symptom definition’ questions are asked.
Participants proceeded to complete the Personal Health Questionnaire (PHQ9), a 10-item self-administered validated instrument, which scores each of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria for MDD (Kroenke et al. 2001). It can be used both as a diagnostic measure as well as a symptom severity measure and assesses depression symptoms over the past two weeks. It has 4-point Likert type response options ranging from “Not at all” to “Every day”; scores range from 0 to 27, with higher scores indicating higher levels of depression. Depression levels can be categorized as mild (5 to 9 scores), moderate (10 to 14 scores), moderately severe (15 to 19 scores) or severe depression (20 to 27). Results from the FHS and PHQ9 populated a one-page report, which participants were able to print out. The report included a brief summary of the participant’s family history, as well as the participant’s PHQ9 score and recommendations specific to the participant’s PHQ score; for example for participants with PHQ9 scores indicating moderately severe depression, the report recommended treatment for depression, including referral to a mental health professional.
Patients then completed measures assessing Socio-demographic data (sex, age, education level, marital status and country of birth). On completion of the baseline questionnaire, participants were given access to the website. A link to the follow-up questionnaire was e-mailed to participants once they had accessed the website.
Follow-up measures: Twenty-seven Likert-type items and 17 open-ended items assessed acceptability, satisfaction with length and level of detail, perceived relevance, emotional impact and perceived improvement of understanding as well as usability and functionality of the online tool, using items adapted from a previously developed measure (Wakefield et al. 2007). A full copy of the questionnaire is available from the authors on request. Descriptive statistics were performed using the Statistical Program for the Social Sciences, Version 22.
Results
Six GP practices participated in this pilot study, and 54 patients opted into the study and completed the baseline questionnaire. Of these, two patients reported no FDRs with MDD and/or BD and were excluded from the analysis (N = 52). Twenty-four of these 52 participants also completed the follow-up questionnaire and comprised the final sample. There were no statistically significant differences between patients who completed the follow-up questionnaire and those who did not in terms of age, educational level, marital status and PHQ9 score. However, patients who were lost to follow up were more likely to have a family history of BD (p < 0.001) and not to have children (p = 0.002). Table 1 shows the sociodemographic and family history characteristics of the participants. Of note, nine (35 %) had a university degree and in addition seven (27 %) had a post-graduate degree and all were born in an English-speaking country.
Eleven (49 %) participants reported having read everything on the website, 5 (22 %) reported having read the website quite thoroughly, 3 (13 %) just the parts that were relevant, and 4 (17 %) briefly. The time taken to read the website ranged from less than 5 min to less than 30 min for 13 participants (57 %), 30 to less than 60 min for 9 (39 %) participants and more than 60 min for one participant (4 %).
Table 2 summarizes participant responses to the items that assessed acceptability. Briefly the majority of participants felt that the website contained about the right amount of information (n = 21, 91 %) and was the right length (n = 18, 78 %). Most participants reported that they found the website “somewhat” or “very useful” (n = 22, 96 %). All were “somewhat satisfied” or “very satisfied” with the information on the website (n = 23, 100 %). One (4 %) and 4 (17 %) reported that the website greatly exceeded or exceeded their expectations, respectively, while 17 (74 %) reported it met their expectations, and one (4 %) that they were a bit disappointed by it. The latter participant expressed frustration in several open-ended questions about survey items that required respondents to provide a response before being able to progress to the next item. The majority of participants (n = 18, 86 %) reported they would recommend the website to other people with a family history of depression.
By contrast two (10 %) were not sure and one (4 %) individual reported they would not recommend it; these particular individuals had also experienced technical problems, such as being unable to play the videos and software bugs. The latter individual was of the opinion that the FHS had incorrectly classified family members and herself as having experienced an episode of MDD and/or BD.
The perceived emotional impact of the website was generally positive, with the majority of participants reporting that it caused them to feel “worried or concerned” either “not at all” (n = 16, 76 %) or only “a little” (n = 5, 24 %). In response to an open-ended question about what made them feel worried, answers included: “Genetically I could be at higher risk of depression – that’s depressing!! (Hahaha)” and “My parents are both still living. When one dies, I could suffer depression.” Three (14 %) participants reported feeling “not at all” reassured after reading the information on the website, 2 (10 %) reported feeling “a little” reassured, and 7 (33 %) “somewhat”, 7 (33 %) “quite a bit” and 2 (10 %) “very much so” reassured. Answering an open-ended question about what made them feel reassured, responses included: “I remember my chance of depression is 13%, which is very low”; “That there were fairly simple things that I could do help with depression” and “All the information… on your website, it gives you somewhere to turn to…”.
Participants were also asked to rate their perceived improvements in understanding of a range of topics using Likert-type items ranging from “not at all” (1) to “a lot” (5). The highest ranked topics were “Importance of early detection” (mean = 4.0, SD = 0.9) and “The role of environmental and genetic factors” (mean = 4.0, SD = 1.0), followed by “Strategies to reduce your chances of depression and prevent the development of depression” (mean = 3.9, SD = 1.1), “Your chances of developing depression” (mean = 3.8, SD = 1.0), “Your family history of depression” (mean = 3.7, SD = 1.0) and “Other lifestyle issues around depression, such as stigma’ (mean = 3.7, SD = 1.2).
In response to an open-ended question about what participants liked best about the website, comments included: “Clear, upbeat, friendly”; “It presented the information clearly, in quite a lot of depth”; “It was all evidence-based”; “The structure was pretty good”; “Well organized. Not too technical”; “The diagrams of the jars…it just made sense”.
Discussion
In this study we pilot-tested the first online psycho-educational intervention that is specifically targeted to people with a family history of depression and provides genetic risk information and ratings of evidence-based information on preventive strategies for depression. The website was well received by participants. Individuals reported feeling satisfied with the website, rating both the amount of information provided and the length of the website favorably. The website was deemed to be relevant to their situation, with most participants reporting that they would recommend it to other people with a family history of depression. Most participants felt that the website had improved their understanding of familial aspects of depression, evaluated the online website positively and found it easy to use. All participants reported that the site was easy to navigate, and that the information was well organized and easy to read. Eighty-six percent reported they would recommend the website to other people with a family history of depression.
In response to open-ended questions assessing perceived emotional impact, a small number of participants reported feelings of worry that were generated by the realization that they were at increased risk of developing depression. Similarly about a quarter of participants reported feeling “not at all” or “a little” reassured. These findings are perhaps not surprising given the intent of the website, which was to provide accurate genetic risk information and provide users with estimates of their own risk. For individuals who were unaware that they were at increased risk, the website content may have led to a more accurate estimation of their risk, thus prompting worry, which in turn may facilitate or inhibit preventative behaviors. In our ongoing RCT we will assess the relationship between worry and preventative behaviors (Meiser et al. 2013).
While other websites are available which provide evidence-based information on treatments for depression, e.g. http://bluepages.anu.edu.au, to our knowledge, this novel website is the first to provide up-to-date evidence-based information on strategies to prevent depression onset in people at increased familial risk as well as the general population more widely. The literature searches undertaken to identify strategies with preventative potential update and extend previous literature reviews in this area (Cuijpers et al. 2008; Cuijpers et al. 2012; Munoz et al. 2010; Barrera et al. 2007). The website offers users an overview of the evidence of the value of a range of strategies, including psychological therapies, lifestyle factors and psychosocial strategies, in reducing the risk of depression onset as well as ratings of the methodological rigor of the evidence.
Study Limitations
The follow-up response rate achieved in this pilot study was disappointing. Due to the opt-in nature of the pilot-study, it is unknown how many patients at each practice met the eligibility criteria of having at least one FDR with MDD and/or BD and had internet access. It is possible that people may be more reluctant to participate in research studies that focus on depression and/or genetics. We are currently conducting a cluster RCT to test the hypotheses that LINKS will lead to better knowledge about risk factors for depression and risk-reducing strategies, greater intention to adopt such strategies, and less depression and perceived stigma (Meiser et al. 2013). Given patients were randomly selected and GP practices were sampled broadly across different regions of Sydney, it is likely that a significant proportion of those invited would have been from ethnic minorities. However, disappointingly, all participants were from English-speaking backgrounds. The sample was also highly educated with >60 % reporting a university degree. The acceptability in a more culturally and linguistically diverse and less educated sample is unknown. Also, patients who were lost to follow up were more likely to have a family history of BD and not to have children, and thus the views of participants from these subgroups may be underrepresented.
Practice Implications
While the website was tested with patients of GPs, it would be equally suitable for patients consulting genetic counsellors and other genetics practitioners, psychiatrists and psychologists about their familial risk of depression. LINKS would be suitable both to supplement the consultation as well as a stand-alone tool to refer patients to in order to work through LINKS according to their preference. However, it was beyond the scope of this study to trial LINKS with other health professional groups and test it as a stand-alone tool. Furthermore, LINKS could also be evaluated as a teaching tool for healthcare professionals, who come in contact with people with a family history of depression, including genetic counsellors, psychologists, psychiatrists and GPs.
Research Recommendations
This pilot study highlights the importance of pilot-testing online educational resources prior to testing them in a larger trial. In particular, pilot-testing identified several software bugs and technical problems that needed addressing. Also, it showed that the percentage of participants who completed the follow up questionnaire was low; as a result we decided to offer an incentive to participants in the RCT ($50 voucher for a supermarket chain), given the success demonstrated by monetary incentives in increasing questionnaire response and minimizing loss to follow up (Brueton et al. 2014; Gates et al. 2009).
Results from this pilot study evaluation demonstrate that the website is highly acceptable in this community group. However, to demonstrate the efficacy of the intervention, more rigorous evidence is needed, in the form of our ongoing cluster RCT (Meiser et al. 2013). Future studies evaluating similar interventions should aim to recruit a more linguistically and culturally diverse sample, for example by translating website content and the survey instrument used for evaluation. Another important priority for future research is an exploration of the ethical, legal and social implications of offering psycho-education to people at increased familial risk of depression, including how to best offer information that maintains personal choice and minimises adverse consequences (Biesecker and Peay 2003) and how to communicate about genetic risk without increasing perceived stigma. While our pilot data indicate that the LINKS website achieved these aims, our subsequent cluster RCT will allow the impact on important patient outcomes such as stigma to be determined more precisely (Meiser et al. 2013).
References
Andersson, G., & Hedman, E. (2013). Effectiveness of guided internet-based cognitive behavior therapy in regular clinical settings. Verhaltenstherapie, 23, 140–148.
Barrera, A., Torres, L., & Munoz, R. (2007). Prevention of depression: the state of the science at the beginning of the twenty-first century. International Review of Psychiatry, 19, 655–670.
Barrera, A., Beekman, A. T., & Reynolds, C. (2012). Prevention of depression: a global priority. JAMA, 307, 2259.
Beardslee, W., Brent, D., Weersing, V., et al. (2013). Prevention of depression in at-risk adolescents: longer-term effects. JAMA Psychiatry, 70, 1161–1170.
Berk, M., Sanders, K., Pasco, J., et al. (2007). Vitamin D deficiency may play a role in depression. Medical Hypotheses, 69, 1316–1319.
Biesecker, B., & Peay, H. (2003). Ethical issues in psychiatric genetics research: points to consider. Psychopharmacology, 171, 27–35.
Brueton, V., Tierney, J., Stenning, S., et al. (2014). Strategies to improve retention in randomised trials: a Cochrane systematic review and meta-analysis. BMJ Open, 4, e003821. doi:10.1136/bmjopen-002013-003821.
Clarke, G., Hornbrook, M., Lynch, F., et al. (2001). A randomised trial of a group cognitive intervention for depression in adolsecent offspring of depressed patients. Archives of General Psychiatry, 58, 1127–1134.
Cuijpers, P., van Straten, A., Smit, F., et al. (2008). Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. American Journal of Psychiatry, 165, 1272–1280.
Cuijpers, P., Donker, T., Johansson, R., et al. (2011). Self-Guided Psychological Treatment for Depressive Symptoms: A Meta-Analysis PLOS ONE, 6, e21274.
Cuijpers, P., Beekman, A., & Reynolds, C. (2012). Preventing depression: a global priority. JAMA, 307, 1033–1034.
Davis, L., Uezato, A., Newell, J., et al. (2008). Major depression and comorbid substance use disorders. Current Opinion in Psychiatry, 21, 14–18.
Department of Health and Ageing (2013). National Mental Health Report 2013: Tracking progress of mental health reform in Australia, 1993–2011. Canberra: Commonwealth of Australia.
Donker, T., Griffiths, K., Cuijper, P., et al. (2009). Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Medicine, 2009(7), 79.
Ebert, D., Zarski, A., Christensen, H., et al. (2015). Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PloS One, 10, e0119895.
Garber, J., Clarke, G., & Weersing, R. (2009). Prevention of depression in at-risk adolescents: a randomised controlled trial. Journal of the American Medical Association, 301, 2215–2224.
Gates, S., Williams, M., Withers, E., et al. (2009). Does a monetary incentive improve the response to a postal questionnaire in a randomised controlled trial? The MINT incentive study. Trials, 10. doi:10.1186/1745-6215-1110-1144.
Jacobs, M., Miller, L., Wickramaratne, P., et al. (2012). Family religion and psychopathology in children of depressed mothers: ten-year follow-up. Journal of Affective Disorders, 136, 320–327.
Jorm, A. F., Barney, L. J., Christensen, H., et al. (2006). Research on mental health literacy: what we know and what we still need to know. Australian and New Zealand Journal of Psychiatry, 40, 3–5.
Kasen, S., Wickramaratne, P., Gameroff, M., et al. (2012). Religiosity and resilience in persons at high risk for major depression. Psychological Medicine, 42, 509–519.
Kieseppa, T., Partonen, T., Haukka, J., et al. (2004). High concordance of bipolar I disorder in a nationwide sample of twins. American Journal of Psychiatry, 161, 1814–1821.
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–613.
Larun L, Nordheim L, Ekeland E, et al. (2006) Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database of Systematic Reviews.
Mackinnon, A., Griffiths, K., & Christensen, H. (2008). Comparative randomised trial of online cognitive–behavioural therapy and an information website for depression: 12-month outcomes. British Journal of Psychiatry, 192, 130–134.
Marry S, McDowell H, Hetrick S, et al. (2004) Psychological and/or educational interventions for the prevention of depression in children and adolescents. Cochrane Database of Systematic Reviews.
Meiser, B., Schofield, P., Trevena, L., et al. (2013). Cluster randomized controlled trial of a psycho-educational intervention for people with a family history of depression for use in general practice. BMC Psychiatry, 13.
Munoz, R., Cuijpers, P., Smit, F., et al. (2010). Prevention of major depression. Annual Review of Clinical Psychology, 6, 181–212.
National Health & Medical Research Council. (1999). How to present the evidence for consumers. Canberra: Commonwealth of Australia.
Peay, H., & Austin, J. (2011). How to talk with families about genetics and psychiatric illness. New York: W.W. Norton Company Inc..
Peay, H., Hooker, G., Kassem, L., et al. (2009). Family risk and related education and counseling needs: perceptions of adults with bipolar disorder and siblings of adults with bipolar disorder. American Journal of Medical Genetics Part A., 149 A, 364–371.
Perlman, C., Johnson, S., & Mellmand, T. (2006). The prospective impact of sleep duration on depression and mania. Bipolar Disorders, 8, 271–274.
Quinn, V., Wilde, A., Meiser, B., et al. (2014). Preferences regarding targeted education and risk assessment in people with a family history of major depressive disorder. Journal of Genetic Counseling, 23, 785–795.
Seligman, M., Steen, T., Park, N., et al. (2005). Positive psychology progress: empirical validation of interventions. American Psychologist, 60, 410–421.
Skarupski K, Tangney C, Li H, et al. (2013) Mediterranean diet and depressive symptoms over time. Journal of Nutrition, Health and Aging 17.
Stice, E., Ragan, J., & Randall, P. (2004). Prospective relations between social support and depression: differential direction of effects for parent and peer support? Journal of Abnormal Psychology, 113, 155–159.
Sullivan, P., Neale, M., & Kendler, K. (2000). Genetic epidemiology of major depression: review and meta-analysis. American Journal of Psychiatry, 157, 1552–1562.
Trevena, L., Irwig, L., & Barratt, A. (2006). Impact of privacy legislation on the number and characteristics of people who are recruited for research: a randomised controlled trial. Journal of Medical Ethics, 32, 473–477.
Wakefield, C., Meiser, B., Homewood, J., et al. (2007). Development and pilot testing of two decision aids for individuals considering genetic testing for cancer risk. Journal of Genetic Counseling, 16, 325–339.
Weissman, M., Wickramaratne, P., Adams, P., et al. (2000). Brief screening for family psychiatric history: the family history screen. Archives of General Psychiatry, 57, 675–682.
Wilde, A., Chan, H., Rahman, B., et al. (2014). A meta-analysis of the risk of major affective disorder in relatives of individuals affected by major depressive disorder or bipolar disorder. Journal of Affective Disorders, 158, 37–47.
Acknowledgments
We would like to thank the participants in this study. We also thank Raghib Ahmad for assistance with manuscript submission. We are very grateful to Associate Professor Jehannine Austin and Dr. Holly Peay for reviewing the content of the website and providing valuable feedback and suggestions for improvements. This study was funded by an Australian Research Council Linkage Grant (LP120200075), with additional funding from NSW Health and the Centre for Genetics Education. Bettina Meiser is supported by a National Health and Medical Research Council of Australia (NHMRC) Senior Research Fellowship (1078523). Philip Mitchell and Peter Schofield are supported by an NHMRC Program Grant (1037196). Helen Christensen is supported by a John Cade Fellowship (1056964), and Michelle Peate by a National Breast Cancer Foundation Early Career Fellowship (ECF-15-005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Animal Studies
No animal studies were carried out by the authors for this article.
Conflict of Interest
None of the authors have a conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Meiser, B., Peate, M., Levitan, C. et al. A Psycho-Educational Intervention for People with a Family History of Depression: Pilot Results. J Genet Counsel 26, 312–321 (2017). https://doi.org/10.1007/s10897-016-0011-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-016-0011-5