Abstract
As the impact of breast cancer (BC) risk assessment in asymptomatic women with a family history of BC had never been explored in Italy, we performed a study on a retrospective series of women who had undergone BC risk assessment. To this aim, a semi-structured telephone interview was administered to 82 women. Most participants considered the information received as clear (96.2 %) and helpful (76.8 %). Thirty-eight (46.3 %) stated that their perceived risk of BC had changed after the counseling: for 40.2 % it had decreased, for 6.1 % increased; however, women highly overestimating their risk at the baseline (≥4-fold) failed to show improvements in risk perception accuracy. Sixty-six women (80.5 %) stated they had followed the recommended surveillance, while 19.5 % had not, mainly due to difficulties in arranging examinations. Most women (89.0 %) had shared the information with their relatives, with 57.3 % reporting other family members had undertaken the recommended surveillance. BC risk assessment was associated with high rates of satisfaction and had a favorable impact on risk perception in a subgroup of women. The impact on surveillance adhesion extended to relatives. Organized programs for identification and surveillance may help identify a larger fraction of at-risk women and overcome the reported difficulties in arranging surveillance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most common women’s cancer, occurring in one woman in eight in Western countries, including Italy (AIRTUM 2014). Family history of BC is a major risk factor, with about 5 % of all cases being caused by mutations in the genes associated with BC and Ovarian cancer: BRCA1/2 (Hilgart et al. 2012).
Overall, 5 to 10 % of women have a mother or sister with breast cancer, and about twice as many have either a first-degree relative (FDR) or a second-degree relative with breast cancer (Hilgart et al. 2012). Although the relative risk (RR) conferred by any family history of BC is estimated to be 2.1 (Pharoah et al. 1997), it is well known that risk increases with the number of affected relatives, age at diagnosis, and the presence of affected male relatives; for instance, the RR of a woman having one FDR affected (sibling or parent) is 1.74–2.57, with the risk increasing more when a brother, if compared to a sister, is affected (RR = 2.48 versus 1.87), while the RR of women having two FDR affected is 2.81–4.71 (Bevier et al. 2012).
BC family history is therefore a reason for referring women to genetic counseling aimed at BC risk assessment, in order to tailor BC surveillance according to individual risk. Nevertheless, whereas consistent guidelines exist for high-risk women (lifetime risk >20–30 %, including BRCA carriers), management of intermediate risk women is more variable; in Italy, in the last two decades, high-risk women had the opportunity to be enrolled into a multicenter trial coordinated by a national health institution (Istituto Superiore di Sanità, Rome, Italy) (Sardanelli et al. 2011), with those not entering the trial being managed according to EUSOMA guidelines (Sardanelli et al. 2010). Conversely, surveillance of women at moderate familial risk varied across different institutions. From 2012, in the Regione Emilia-Romagna (RER), Italy, a systematic assessment of familial BC risk has been undertaken in order to identify and properly manage women with familial BC. To this aim, a regional network has been established with a “Hub and Spoke” organization: the multi-step process starts with a basic questionnaire to be filled for every woman undergoing screening mammography and for women seeking advice about their BC family history from general practitioners or other health professionals. Every woman who fulfils the criteria for accessing second-level assessment is referred to the Spoke, where individual BC risk is evaluated. If a hereditary predisposition is suspected on the basis of specific criteria, the woman is referred to the Hub center: a cancer genetic clinic where genetic counseling is performed, including genetic testing whenever appropriate (“DGR n. 220/2011;” Protocollo assistenziale nelle donne a rischio ereditario di tumore della mammella e/o ovaio 2014).
During the preparation of the Regional program, a common concern among the clinicians involved was that assessment and communication of BC risk may have an unfavorable psychological impact. Available literature evidence (Hilgart et al. 2012) suggests that BC risk assessment helps to reduce distress, to improve the accuracy of perceived risk, and to increase knowledge. Improvements in psychological well-being and decrease in the levels of cancer worry have been also reported (Hilgart et al. 2012). Nevertheless, the majority of the studies on this issue have been carried out in North America or Northern Europe, with little or no data existing for the Italian population. Therefore, we undertook a study aimed at assessing the impact of genetic counseling in a retrospective series of asymptomatic women undergoing genetic counseling because of a family history of BC in the main town of Regione Emilia-Romagna, Bologna, before the start of the organized program.
Methods
Study Design
In 2011 we undertook a cross-sectional survey on women with family history of BC who had undergone genetic counseling for BC risk assessment in Bologna, Italy.
Study Population
From 2003 to 2010, 102 asymptomatic women with family history of BC underwent genetic counseling for BC risk assessment in three hospitals of Bologna (Policlinico S.Orsola-Malpighi; Ospedale Maggiore; Ospedale Bellaria). All the counseling sessions were held by the same team, consisting of a clinical cancer geneticist (DT) and a psychologist with experience in clinical genetics (ER). Although general criteria for referral had been proposed to physicians, these were not precluding the access to counseling, therefore no restrictive selection was made before counseling. Women belonging to families eligible for BRCA1/2 testing (“genetic” risk assessment) were not considered for the present study, which focused on familial risk assessed through probabilistic methods (“empiric” risk assessment). At the time of counseling, all the clients gave their consent to be re-contacted and were therefore eligible for this study, which was approved by the Ethical Board of Hospital S.Orsola-Malpighi, Bologna, Italy.
Eighty-two women (80.4 %) were contacted by telephone and all gave their informed consent to the interview, while 20 (19.6 %) were not reachable.
Interviews
A semi-structured telephone interview was designed including both multiple choice questions and free-text boxes, which allowed us to collect data on specific questions, but also enabled respondents to provide further information about their views. The interview included 16 items (Table 1), grouped in three sections. The first section (1–5) explored perceived clarity of understanding and helpfulness of the information received during counseling; the second section (6–10) assessed the compliance to the recommended surveillance; the last section of the interview included five questions about information-sharing within the family.
Telephone interviews were performed between July 2011 and March 2012 by a psychologist with experience in clinical genetics (MB) and a genetic nurse (LG).
Risk Assessment
Individual BC risk was calculated using the model by Tyrer-Cuzick (IBIS Breast Cancer Risk Evaluation Tool, RiskFileCalc version 1.0, copyright 2004), which has been adopted by RER to define risk-based surveillance programs. Relative risk (RR) has been defined as the ratio between lifetime individual risk and lifetime population risk. According to RER guidelines, women were assigned three different BC risk levels: level 1 (RR < 2): risk similar to the general population, level 2 (RR 2–2.99): moderately increased risk, and level 3 (RR ≥3): significantly increased risk.
For 27 women, who had also participated in another study, the baseline perceived risk was available, based on the question “In your opinion, what is your risk of getting cancer in the future (0–100 %)”. For these women, risk perception accuracy (RPA) was defined as the ratio between the perceived and the objective lifetime risk as estimated by the IBIS model.
Statistical Analysis
All available data were entered anonymously into a dedicated database and were analyzed by using the statistical package IBM-SPSS Statistics (Ver. 21 for Windows, IBM Co., Armonk, NY, USA). Means, standard deviation (SD), ranges and frequencies were used as descriptive statistics. The Kruskal-Wallis one-way analysis of variance by ranks and chi-squared for nominal variables, the Fisher’s exact test for dichotomous variables; ANOVA one-way was used to analyze differences between group means. Two-tailed P values lower than 0.05 were considered statistically significant.
Results
Participant Characteristics
As shown in Table 1, at the time of counseling participants had a mean age of 41.8 ± 11 years (range: 22–80) and the 65.9 % of them had children. Among those having children, 64.8 % had daughters, while 35.2 % had only sons. The mean time elapsed between counseling session and telephone interview was 37.2 ± 23 months (range: 7–103 months; median: 31 months); more in detail, 35 women (42.7 %) were interviewed within 2 years from the counseling session, 31 (37.8 %) between 3 and 5 years and 16 (19.5 %) 6 to 8 years after counseling. After risk assessment, 20 women (24.4 %) were assigned to risk level 1; 51 (62.2 %) to risk level 2, and 11 (13.4 %) to risk level 3, according to RER protocol. Women belonging to risk level 3 tended to be younger (36.86 years on average) when compared to those of levels 1 (42.47 years) and 2 (42.53 years), but this difference did not reach statistical significance.
Perceived Clarity and Helpfulness of the Information Received
As shown in Table 1, the large majority of participants judged the information received during counseling as clear and helpful: overall, 74 (90.2 %) considered the information as quite, very or extremely clear, and 63 (76.8 %) as quite, very or extremely helpful.
No significant correlations were observed with baseline variables and risk levels; nevertheless, in the lowest risk group, the proportion of women extremely unsatisfied about clarity (15 %) and, especially, helpfulness (25 %) was higher than in the other groups.
Perceived clarity and helpfulness seemed to influence other outcomes, as described in the respective paragraphs.
Twelve women (14.6 %) stated they had doubts remaining after counseling; as expected, this answer was significantly more frequent among participants reporting information as quite/little/not clear (25.7 %) than among those quoting it as very/extremely clear (6.4 %) (χ2 = 6.8, P = 0.009). Similarly, it was more common among women reporting information as quite/little/not helpful (21.7 %) than among those quoting it as very/extremely helpful (5.5 %) (χ2 = 6.6, P = 0.010).
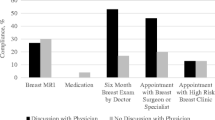
Compliance to Surveillance
Sixty-six women (80.5 %) stated they had followed the surveillance recommended by the counselor (Table 1). Among those, 62 (93.9 %) defined themselves as very/extremely confident and satisfied with the surveillance.
When asked about any difficulties in organizing surveillance examinations, 49 (74.2 %) reported no difficulties, ten (12.2 %) complained about waiting times, two (2.4 %) found it difficult to reconcile examinations with work, one (1.2 %) complained about the lack of health professionals coordinating/arranging the examinations and one (1.2 %) reported problems in reaching the medical center.
On the other hand, 16 women (19.5 %) declared they did not follow recommended surveillance; all of them provided at least one reason for that and six gave two reasons, for a total of 22: the most common was the difficulties in arranging the examinations (6 participants; 27.3 % of responses), lack of health professionals coordinating/arranging the examinations was reported by four women (18.2 % of responses), family problems were invoked by four women (18.2 % of responses), three women stated they were unsatisfied with the recommendations received during counseling (13.6 % of responses), two were tired or non-confident about surveillance (9.1 % of responses), one was too scared to find something wrong (4.5 % of responses), one reported problems to reach the medical center (4.5 % of responses), while one reported that the reassurance received at counseling led her to reduce surveillance (4.5 % of responses).
Compliance to surveillance was not influenced by perceived clarity/helpfulness. A trend was observed between increasing risk and increasing adherence to surveillance (Table 1).
Impact of Counseling on Health Behaviors
The majority of women (67; 81.7 %) stated they had not made any important decisions regarding their health after counseling. Conversely, 13 (15.9 %) declared to have more regularly followed or intensified the surveillance as a consequence of counseling, and two (2.4 %) had adopted a healthier lifestyle (with one stopping smoking after the counseling session). Women stating they had made decisions were significantly more likely to have regarded information as very/extremely clear and very/extremely helpful (86.7 and 66.7 %, respectively) than women reporting no important decisions (50.7 and 38.8 %, respectively), (χ2 = 9, P = 0.003 and χ2 = 7.3, P = 0.007, respectively).
Information-Sharing Within the Family
Seventy-three participants (89 %) stated they had shared the information received with their relatives. The most frequently reported reason for doing it, was the desire to provide other family members with information helpful for their health (45 women; 61.6 %). Six women (8.2 %) recommended their relatives to intensify surveillance, five (6.8 %) were seeking reassurance, and two tried to involve the index case for genetic testing, while 15 women (20.5 %) did not explain why they decided to share the information.
On the other hand, nine women (11 %) decided not to share information with other family members: three reported poor relationship with their relatives, two wanted to avoid worrying their relatives, two had no living close relatives, while two did not explain the reason.
Forty-seven women (57.3 %) declared that other family members had undertaken the recommended surveillance after they shared information received at counseling, specifically: parents (for 23 women), siblings (for 22), children (for eight), more distant relatives (for 12).
Women perceiving information as very/extremely helpful were more likely to share (94.4 %) in comparison to women perceiving it as quite/little/not helpful (84.8 %) (χ2 = 7.5 P = 0.006). Albeit without statistical significance, the higher the risk, the higher the chance to share with relatives (100 % for risk level 3).
Reported Impact on Perceived Risk
As shown in Tables 1 and 2, 38 women (46.3 %) stated that their perceived risk of BC had changed after genetic counseling: for 33 (40.2 % of the total sample) it had decreased, for five (6.1 %) increased. The change did not significantly correlate with risk level, although all the women reporting an increased perceived risk belonged to level 2.
As shown in Table 2, women with increased perceived risk tended to be older than those with reduced/unchanged perception, although this difference did not reach the statistical significance (P = 0.08). Because a difference, although non-significant, was observed in mean time elapsed since counseling (Table 2), the influence of time on risk perception changes was further explored by comparing the three categories subdivided on the basis of the time elapsed between counseling and interview; results are summarized in Fig. 1: notably, perceived risk was reported as changed (increased or reduced) by 62.9 % of women interviewed within 2 years after counseling, as compared to 29 % of women interviewed 2–5 years and 43.8 % interviewed >5 years after counseling (χ2 = 4.8, P = 0.029).
A significant difference was also observed in relation to perceived helpfulness: 21 out of 36 (58.3 %) women who had defined the information as very/extremely helpful stated their perceived risk had changed (for 19 reduced), in comparison to 17 out of the 46 (37 %) defining the information as quite/little/not helpful (χ2 = 4,4, P = 0.037). Moreover, 25 of 47 (53.2 %) women considering the information as very/extremely clear reported changes in perceived risk (reduction in 21), if compared to 13 of 35 (37.1 %) of those defining the information as quite/little/not clear (P = 0.77).
For the 27 women for whom the baseline perceived risk had been recorded, subjective risk ranged from 15 to 100 % and RPA from 0.2 to 6.4. More detailed, 6 women (22.2 %) had a RPA between 0.2 and 2; 15 (55.6 %) between 2 and 3.99; 6 (22.2 %) 4 or higher.
Baseline perceived risk was significantly more accurate in women perceiving the information received as quite/very extremely clear than in those dissatisfied about clarity (mean RPA 2.65 versus 4.2; F = 7.3, P = 0.012). Mean RPA was 2.4 ± 1 for women reporting decreased perceived risk, compared to 5.1 ± 0.3 for those reporting increased perceived risk (P = 0.06). Consistently, out of the six women with RPA 4 or higher, two reported their perceived risk as increased and four as unchanged.
Discussion
In the 7-years period considered, 102 asymptomatic women underwent empiric BC risk assessment and 82 participated into the study. About one-quarter of the latter belongs to the BC risk level 1 (general population risk), while only 13.4 % were classified as high risk (level 3). After the launch of the regional program, the number of the women counseled, as well as the proportion of women at increased risk, have raised significantly; in 2013, 204 asymptomatic women underwent empiric BC risk assessment in Bologna: 48 (23.5 %) were assigned to level 1; 79 (38.7 %) to level 2 and 77 (37.7 %) to level 3 (unpublished data). These data demonstrate that such a systematic assessment, beyond leading to an enormous increase in referrals, also enables the identification of a higher proportion of high-risk women (37.7 % compared to 13.4 %).
Satisfaction about genetic counseling was generally high among participants, with 90 % of women considering information received as clear and 77 % as helpful. Although the impact on life-style seems limited (81.7 % of women failed to make any relevant decisions), reported compliance to surveillance is high (80 %). Complaints about difficulties in arranging surveillance were registered among both women following and women not following surveillance, for a total of 21 women (25 % of the total sample) reporting problems (such as the lack of health professionals coordinating the examinations) that should be currently overcome by the Hub and Spoke organization.
Moreover, the information received at the time of counseling session was frequently shared with other family members (89 %) without apparent psychological adverse outcomes. As an effect, the 57.3 % reported that other family members had undertaken the recommended surveillance after their counseling session. We can therefore state that oncogenetic counseling provides useful information not only for counseled women but also for other family members. The way women explain family BC to their family members, and the value they gave to the information received could also influence family members’ decision to undertake surveillance program. The availability of Spoke centers that organize surveillance program for these women could also be a facilitator factor for their compliance and adherence.
Counseling led to a reported decrease in perceived risk in 40 % of participants, which is in agreement with previous studies reporting an overall decrease in participants’ perceived risk of BC, and, subsequently, in anxiety and worry (Bowenet al. 2006; Bowen et al. 2004; Matloff et al. 2006).
Although through indirect evidence, our findings support previous data showing that improvement in risk perception accuracy is generally limited to the short-term (Dieng et al. 2014): accordingly, in our study, the fraction of women reporting an effect on risk perception was significantly higher in the group counseled more recently than in the groups with longer time elapsed from counseling. Notably, women highly overestimating their cancer risk (RPA ≥ 4) did not report any reassurance after counseling, which suggests that benefits may be limited in women with particularly high cancer worry/distress. The reasons underlying such overestimation should be explored in more depth through qualitative studies, in order to identify factors potentially limiting the effectiveness of counseling, which could be preliminarily assessed to plan tailored counseling for specific clients.
In conclusion, no adverse effects have been found to be associated with BC risk assessment, which, conversely, showed a favorable impact on both risk perception and adherence to surveillance. This latter effect extends to the family members of the counseled women.
Study Limitations
A limitation of our study is that changes in perceived risks are reported by participants, instead of being evaluated through repeated assessments. Moreover, perceived risk measures were available only for a fraction of participants (27) and only at baseline, which hampers significant conclusions on the impact of counseling on perceived risk. In addition, the statistical approach adopted, based on the use of multiple univariate tests, increases the family wise error rate.
Practice Implications
Our study suggests that establishing an organized program through which women with increased BC risk are identified and taken in care to perform surveillance would improve comprehensive adherence into these programs and avoid important drop out, without causing adverse emotional outcomes. Nevertheless, particular attention should be devoted to identify women with abnormally high perceived risk, who would benefit from a tailored counseling intervention, since standard risk assessment and counseling seem to have no effect in improving risk perception accuracy.
References
AIRTUM. (2014). I numeri del cancro in Italia 2014. Retrieved from https://doi.org/www.registri-tumori.it/PDF/AIOM2014/I_numeri_del_cancro_2014.pdf.
Bevier, M., Sundquist, K., & Hemminki, K. (2012). Risk of breast cancer in families of multiple affected women and men. Breast Cancer Research and Treatment, 132(2), 723–8. doi:https://doi.org/10.1007/s10549-011-1915-2.
Bowen, D. J., Burke, W., McTiernan, A., Yasui, Y., & Andersen, M. R. (2004). Breast cancer risk counseling improves women’s functioning. Patient Education and Counseling, 53(1), 79–86. doi:https://doi.org/10.1016/S0738-3991(03)00122-8.
Bowen, D. J., Burke, W., Culver, J. O., Press, N., & Crystal, S. (2006). Effects of counseling Ashkenazi Jewish women about breast cancer risk. Cultural Diversity & Ethnic Minority Psychology, 12(1), 45–56. doi:https://doi.org/10.1037/1099-9809.12.1.45.
DGR 21 Febbraio 2011, n. 220/2011, in materia di “Rischio eredo-familiare per il carcinoma della mammella”. (2011). Retrieved from https://doi.org/www.consultoriemiliaromagna.it/file/user/dgr.pdf.
Dieng, M., Watts, C. G., Kasparian, N. A., Morton, R. L., Mann, G. J., & Cust, A. E. (2014). Improving subjective perception of personal cancer risk: systematic review and meta-analysis of educational interventions for people with cancer or at high risk of cancer. Psycho-Oncology, 23(6), 613–25. doi:https://doi.org/10.1002/pon.3476.
Hilgart, J. S., Coles, B., & Iredale, R. (2012). Cancer genetic risk assessment for individuals at risk of familial breast cancer. The Cochrane Database of Systematic Reviews, 2, CD003721. doi:https://doi.org/10.1002/14651858.CD003721.pub3.
Matloff, E. T., Moyer, A., Shannon, K. M., Niendorf, K. B., & Col, N. F. (2006). Healthy women with a family history of breast cancer: impact of a tailored genetic counseling intervention on risk perception, knowledge, and menopausal therapy decision making. Journal of Women’s Health (2002), 15(7), 843–56. doi:https://doi.org/10.1089/jwh.2006.15.843.
Pharoah, P. D., Day, N. E., Duffy, S., Easton, D. F., & Ponder, B. A. (1997). Family history and the risk of breast cancer: a systematic review and meta-analysis. International Journal of Cancer. Journal International Du Cancer, 71(5), 800–9. Retrieved from https://doi.org/www.ncbi.nlm.nih.gov/pubmed/9180149.
Protocollo assistenziale nelle donne a rischio ereditario di tumore della mammella e/o ovaio — Screening — E-R Salute. (2014). Retrieved from https://doi.org/salute.regione.emilia-romagna.it/screening/tumori-femminili/notizie/2014/copy_of_PDTAOTTOBRE.pdf.
Sardanelli, F., Boetes, C., Borisch, B., Decker, T., Federico, M., Gilbert, F. J., & Wilson, R. (2010). Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. European Journal of Cancer, 46, 1296–1316.
Sardanelli, F., Podo, F., Santoro, F., Manoukian, S., Bergonzi, S., Trecate, G., & Del Maschio, A. (2011). Multicenter surveillance of women at high genetic breast cancer risk using mammography, ultrasonography, and contrast-enhanced magnetic resonance imaging (the high breast cancer risk italian 1 study): final results. Investigative Radiology, 46(2), 94–105. doi:https://doi.org/10.1097/RLI.0b013e3181f3fcdf.
Acknowledgments
We are grateful to all participants for giving consent to the study and responding to the interview. LG is supported by the Grant from Regione Emilia-Romagna “Diagnostics advances in hereditary breast cancer (DIANE)” (PRUa1GR-2012-001).
Conflict of Interest
The authors Lea Godino, Elisabetta Razzaboni, Margherita Bianconi and Daniela Turchetti declare that they have no conflicts of interest.
Human Studies and Informed Consent
The study protocol conforms to the ethical guidelines of the WMA Declaration of Helsinki and was approved by the Ethical Board of Hospital S.Orsola-Malpighi, Bologna, Italy (Prot. 154/2010/O).
Animal Studies
No animal studies were carried out by the authors for this article
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 37 kb)
Rights and permissions
About this article
Cite this article
Godino, L., Razzaboni, E., Bianconi, M. et al. Impact of Genetic Counseling in Women with a Family History of Breast Cancer in Italy. J Genet Counsel 25, 405–411 (2016). https://doi.org/10.1007/s10897-015-9884-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-015-9884-y