Abstract
The aim of this study is to investigate the effect of diabetes genetic counseling on attitudes toward diabetes and its heredity in relatives of type 2 diabetes patients. This study was an unmasked, randomized controlled trial at a medical check-up center in Japan. Subjects in this study are healthy adults between 30 and 60 years of age who have a family history of type 2 diabetes in their first degree relatives. Participants in the intervention group received a brief genetic counseling session for approximately 10 min. Genetic counseling was structured based on the Health Belief Model. Both intervention and control groups received a booklet for general diabetes prevention. Risk perception and recognition of diabetes, and attitude towards its prevention were measured at baseline, 1 week and 1 year after genetic counseling. Participants who received genetic counseling showed significantly higher recognition about their sense of control over diabetes onset than control group both at 1 week and 1 year after the session. On the other hand, anxiety about diabetes did not change significantly. The findings show that genetic counseling for diabetes at a medical check center helped adults with diabetes family history understand they are able to exert control over the onset of their disease through lifestyle modification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As the number of patients with diabetes continues to grow (Whiting et al. 2011), creating a global burden, the development of an effective preventive strategy is urgently needed. In most of the research done in this area, obesity has been used as a marker for high risk of diabetes. However, a recent international risk prediction study also suggests that Asian populations show a high-risk of diabetes even with a nearly normal Body Mass Index (BMI) (Chiu et al. 2011). Obesity is therefore a less specific indicator to detect risk in some populations, especially in Asian countries. In order to screen high-risk individuals, therefore, other risk factors must be discovered.
Type 2 diabetes occurs because of a complicated combination of genetic and environmental factors. Considerable progression in the genomic approach has led to a vast amount of literature identifying disease susceptible variants for type 2 diabetes (Grant et al. 2009). However, it is difficult to use genotype as a predictor of diabetes risk (Anand et al. 2013; Bao et al. 2013; Dagogo-Jack 2012; Muhlenbruch et al. 2013; Vassy and Meigs 2012; Vorderstrasse et al. 2013). In addition, even if people obtain genomic profiling and interventions based on their genotype, their lifestyle or attitude towards prevention is unlikely to be modified unless they also perceive themselves to be at risk for the disease (Arkadianos et al. 2007; Bloss et al. 2011). Therefore, it would be premature to use individual genotype alone as a public health tool without also incorporating patient education targeted at realistic risk perception.
Furthermore, genotype is not the only indicator of genetic predisposition. Family history is a well-known risk indicator from both the genetic and environmental perspective, because individuals with a family history of diabetes can be regarded as having similar genetic predispositions as well as similar lifestyle habits as do their relatives (Kuzuya and Matsuda 1982; Vassy et al. 2011). Individuals with an affected first-degree relative display a 2.3- to 5.5-fold higher risk of type 2 diabetes, independent of sex, age, race/ethnicity, BMI, and other demographic characteristics(Valdez et al. 2007). Therefore, family history can still be used even in this post-genomic era, as a simple and effective screening tool for a high risk population (Hariri et al. 2006a, b; Harrison et al. 2003; Khoury et al. 2008; Stolerman and Florez 2009).
For those who have known risk factors including family history, perception of disease susceptibility is one of the most crucial issues in terms of motivation for preventive behavior (Leventhal et al. 2008; Rosenstock 1966). Perceived susceptibility is an element of the Health Belief Model (Rosenstock 1966), which is a common theoretical model that attempts to provide a comprehensive view of health behavior engagement. The Health Belief Model consists of 6 elements: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy (Rosenstock et al. 1988). A previous study investigating preventive behavior using this model in adult offspring of type 2 diabetic patients in Japan showed that they usually accurately perceived their high-risk status of diabetes onset (Nishigaki et al. 2007). However, they tended to make light of environmental factors and blame disease onset on heredity to avoid personal responsibility for changing their lifestyle. The nature of their perceived susceptibility seemed to cause poor perceived controllability of diabetes (Nishigaki et al. 2007), which is a primary component of self-efficacy. Thus adequate risk education is beneficial to individuals who misconceptualize diabetes susceptibility and have a poor sense of control over diabetes.
This potential benefit, however, must be balanced by the risk that information regarding disease heredity could pose a stigmatizing burden. Thus risk-increased information should be provided with information about adequate coping strategy against that risk (Baum et al. 1997). Additionally, a recent study showed that genetic information about diabetes would not have a favorable effect if the individual already had low-motivation or inappropriate risk perception (Markowitz et al. 2011). Therefore, genetic risk education should be combined with genetic counseling to enable subjects to understand their diabetes risk appropriately and use it as a motivating factor for positive behavior, without provoking unnecessary psychological burden. The present study aimed to investigate the effect of diabetes genetic counseling on attitudes toward diabetes and its heredity among healthy adults with a family history of type 2 diabetes in their first degree relatives.
Methods
This study is part of a three-armed, unmasked, randomized longitudinal trial in a single medical check-up center in the Tokyo metropolitan area. In this article, we report the effect of genetic counseling on subjects’ attitudes towards diabetes prevention. Details of the protocol and the participants’ baseline characteristics have been described previously (Nishigaki et al. 2012).
Subjects
All subjects were recruited at a medical check-up institution for employees in the Tokyo metropolitan area. Subjects were included if they had more than one first-degree relative (parent or sibling) with type 2 diabetes and were aged 30–60 years. Those who were already diagnosed with type 2 diabetes or metabolic syndrome were excluded. Subjects who were already receiving lifestyle intervention in the Specific Counseling Guidance (SCG) program were also excluded. The SCG is a Japanese national diabetes prevention program for adults at high risk for diabetes. Subjects with an increased waist size (male: over 33.5 inch, female: over 35.4 inch) or BMI (over 25 kg/m2) and with more than one of following factors will receive lifestyle education and follow up from a public health nurse: lipidemia, hypertension, hyperglycemia, and smoking. The eligibility of subjects was assessed from a medical questionnaire which all the examinees routinely would submit when they visit the institution for their annual medical check-up. Subjects were invited to participate in this study after they completed their medical check-up. If eligibility criteria were met, subjects were given information about the entire design of study and written consent was obtained from those who agreed to participate in this study. Given the three-armed design of the study, subjects were randomly allocated to one of three groups: genetic counseling and lifestyle intervention group (GC + LI), lifestyle intervention alone group (LI), and no-intervention group. The no-intervention group, which received only general information about healthy lifestyle, was intended to investigate the effect of the lifestyle intervention alone. This study aimed to show the effect of genetic counseling on outcomes by comparing the genetic counseling and lifestyle intervention group with the lifestyle intervention alone group. We calculated the necessary sample size to be 64 per study group to detect a moderate effect size (0.5 SD) in the primary outcome of entire study (energy intake), with 80 % power at the 5 % significance level. Assuming a dropout rate of 10 %, 72 participants are needed for each group (Nishigaki et al. 2012).
Intervention
Participants in the GC + LI group received 10 min of a brief genetic counseling session by a single genetic counselor certified by Japanese Society of Human Genetics and Japanese Society for Genetic Counseling. The genetic counseling session was semi-structured according to a booklet that had been developed by the authors. The details of the booklet have been described elsewhere (Nishigaki et al. 2011). Briefly, the booklet consists of four components that each reflects a core element of the Health Belief Model. The session aims to let subjects adequately perceive the following four elements: seriousness of diabetes, their genetic and environmental susceptibility to diabetes, benefits of lifestyle change in genetically predisposed people for modifying total diabetes risk, and concrete guidance on favorable lifestyle change. After the second data collection, both groups received general information on diabetes prevention about a favorable dietary and exercise lifestyle. Simultaneously, both groups started receiving 6-months of indirect, computer-based lifestyle intervention which analyzes the dietary and physical activity behavior of the subject and generates recommendations about lifestyle modification tailored to each individual (Nishigaki et al. 2012) .
Outcome Measures
For the purposes of this study, we developed a brief questionnaire assessing attitudes toward and recognition of diabetes and its prevention. The principle framework of the questionnaire was based on the Health Belief Model in accordance with the intervention design. The questionnaire contained five questions. The first four questions were based on the core elements of the Health Belief Model: perceived susceptibility, perceived severity, perceived controllability as measure of self-efficacy, and perceived barriers. The fifth question was added to assess level of anxiety. The question “How do you estimate your likelihood of developing diabetes?” was used to assessed perceived susceptibility and was rated on a scale from “Very unlikely” (converted to a score of 1) to “Very likely” (score of 5). Wording of the other four item was as follows: for perceived severity of diabetes—“Diabetes isn’t a severe disease”; for perceived controllability about diabetes onset—“I cannot avoid diabetes onset because I am genetically predisposed to diabetes”; perceived barriers towards diabetes prevention—“I don’t know what type of lifestyle is useful for diabetes prevention”; and for anxiety about diabetes onset—“I feel anxiety for getting diabetes.” Participants were asked to indicate their agreement/disagreement with each of these four items [Scale: “Strongly disagree” (score of 1) to “Strongly agree” (score of 5)]. After confirming the validity of the questionnaire in a pilot study with a small sample (n = 8), the questionnaire was launched.
Outcome measures were assessed three times: immediately after recruitment (baseline), 1 week after the intervention and 1 year after the intervention. The first (baseline) questionnaire was delivered and collected face-to-face, and the second (1 week) and third (1 year) questionnaire were delivered and collected via mail.
Background characteristics data were collected at the time of recruitment by another questionnaire. Information gathered included whether they are living together with someone; occupational status; educational status; dietary habits; physical activity. Biomedical data were collected at recruitment and included information about tri-glycerides, low density lipoprotein fasting blood glucose, and HbA1C. Subjects were also asked by questionnaire whether they had any of the following: impaired glucose tolerance, abnormalities of lipid metabolism, hypertension or hyperuricemia.
Statistical Analysis
Comparisons of outcome between groups were conducted using the Wilcoxon rank sum test. All statistical analyses were conducted using SAS version 9.2 software (SAS Institute, Cary, N.C., USA), and the significance level was set at 0.05. The institutional review board of the hospital approved all protocols for this study.
Results
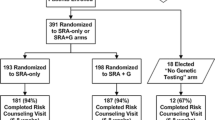
Five hundred thirty eight examinees were eligible to participate in this study. Two hundred sixteen consented to participate for an acceptance rate of 40.1 %. Seventy five of those participants were allocated to the GC + LI group, and 70 were allocated to the LI group. Figure 1 shows the participant flow during the 1-year study period. Finally, 51 (68 %) subjects in the GC + LI group and 53 (76 %) in the LI group completed the 1-year survey. There were no significant differences in background characteristics at baseline between the two groups. Average BMI level and biomedical data were in the normal range for both groups (Table 1). There were also no significant differences in background characteristics between completers and non-completers.
Baseline outcome distributions are shown in Table 2. Both groups showed a similar distribution of outcomes, and no differences were found between the groups. Across both groups, approximately 40 % of participants perceived that their diabetes risk was higher than normal (“Likely” or “Very likely”: 34.6 % in the GC + LI group and 40.6 % in the LI group). Sixty to 70 % of participants disagreed that diabetes is a trivial disease (“Strongly disagree” or “Disagree”: 69.3 % in the GC + LI group and 57.9 % in the LI group). Across both groups, less than half of the participants disagreed that diabetes onset is uncontrollable (“Strongly disagree” or “Disagree”: 38.7 % in the GC + LI group and 36.2 % in the LI group). More than half of the participants indicated feeling anxiety about their potential for developing diabetes onset (“Strongly agree” or “Agree”: 53.3 % in the GC + LI group and 59.4 % in the LI Control group). Approximately 40 % of participants indicated they do not know what type of lifestyle is useful for diabetes prevention (42.7 % in the GC + LI group and 42.0 % in the LI group).
Table 3 shows the outcome distributions in both groups at 1 week and 1 year after the genetic counseling session. At 1 week after intervention, significantly more subjects in the GC + LI group perceived that diabetes onset is controllable (62.3 % in the GC + LI and 35.0 % in the LI group, p = 0.0014, Wilcoxon rank sum test). This effect of genetic counseling was maintained at 1 year after the intervention (58.8 % in the GC + LI and 34.0 % in the LI group, p = 0.038, Wilcoxon rank sum test). There were no significant differences between the groups in outcome measures other than perceived controllability while .
Discussion
Results of this study indicates that diabetes genetic counseling for first-degree relatives of type 2 diabetic patients can successfully modify perceived controllability. Genetic counseling in this study emphasized adequate recognition about a diabetes risk factor: people can modify their total risk for diabetes onset by lifestyle change, even though they are genetically predisposed to diabetes. Participants in the GC + LI group did not show increased anxiety compared to LI group even though they received information about their diabetes predisposition. These results support findings that risk education regarding disease heredity is not harmful if it is given in an adequate setting (Pierce et al. 2000; Pijl et al. 2009). Knowledge from the existing literature and results of the current study provide evidence about the importance of communication with professionals regarding adequate understanding of hereditary risk related to type 2 diabetes.
No significant differences were found in HBM core elements other than perceived controllability. Perceived severity might be addressed by general diabetes information, which was given to both groups. Similarly, perceived barriers would have been addressed by lifestyle intervention teaching in both groups. Perceived susceptibility was expected to be modified by risk counseling as part of genetic counseling. However, there was no difference between the two groups. It is unclear why risk perception remains unchanged. It may be that raising participants’ feeling of controllability had the effect of lessening their total perceived susceptibility even while genetic counseling increased their awareness of genetically predisposed risk. The overall perception of susceptibility might therefore remain stable. These results showing stable risk perception and improved controllability are similar to those of an earlier study in a Western country investigating illness perceptions among people with family history and symptomatic high risk people (Pijl et al. 2009).
Practice Implications
The results of this study suggest the usefulness of genetic counseling in public health. We developed 10-min intervention based on HBM with other elements than controllability. However, we found intergroup difference just in the controllability. Information about severity, general risk factor of diabetes, and barriers towards preventive behavior are usually covered in general education about prevention for diabetes. Therefore, in the clinical setting, it may be sufficient if medical professionals discuss the controllability in addition to general diabetes education. If subjects believe that they cannot change their diabetes risk because of their heredity, it can be explained to them that they can impact their “total” risk by modifying their environmental risk. Of course, genetic counseling, such as was provided in this study should not be applied to subjects without any family history of diabetes. If subjects without family history received the genetic counseling in this study, their risk perception might be underestimated, since the intervention was intended to modify risk perception by emphasizing the importance of family history as a risk factor of diabetes onset.
Research Recommendations
It is unclear whether the changes in attitude towards heredity in diabetes actually lead to behavioral changes such as dietary improvements and physical activity. While improvement in perceived controllability theoretically leads subjects to behavioral change, direct investigation of relationship between attitudinal changes and health outcomes would be useful to strengthen the results of this study.
Study Limitations
Some limitations of this study should be mentioned. First, the overall acceptance rate in this trial was 40.1 % (216 of 538 eligible examinees). This low acceptance rate involves a sampling bias. For example, the sample in this study might consist of subjects who were more worried diabetes or more motivated about preventive behavior. However, it is unclear whether the bias led to under- or over-estimation for the outcome measures of HBM elements. Second, this study was conducted at a single outpatient clinic center in an urban area of Tokyo, and most of the examinees were employed as a full-time office worker. This might also have caused some sampling bias, such as a higher educational status or higher availability of information. Thirdly, the genetic counseling in this study might be too specific because a single genetic counselor provided it. However, it can be replicated by other genetic counselors because it was highly constructed by booklet. Finally, psychometric properties of the questionnaire, other than face validity, have not been confirmed. We used single item questions to measure each element of the HBM. A recent study has shown that a single item question about diabetes controllability had known-group validity (Gutierrez and Long 2011). However, it is unclear whether single item questions can measure other elements of the HBM in this population. Our conclusions may also be limited by the self-reportnature of the questionnaire. Participants answered all of the questions based on their subjective perception. For example, the “normal” level of risk or “understanding” of how to prevent diabetes is different from participant to participant. Development of more robust measures for health belief regarding genetic aspects in type 2 diabetes with sufficient psychometric properties is needed to clarify the results of this study.
Conclusion
Brief genetic counseling about diabetes for healthy adults with family history of type 2 diabetes showed a positive effect on modifying negative perceived controllability for diabetes without provoking unnecessary psychological burden (defined as anxiety). Genetic counseling can be utilized as a motivation enhancement approach in the field of diabetes prevention.
References
Anand, S. S., Meyre, D., Pare, G., Bailey, S. D., Xie, C., Zhang, X., et al. (2013). Genetic information and the prediction of incident type 2 diabetes in a high-risk multiethnic population: the EpiDREAM genetic study. Diabetes Care, 36(9), 2836–2842. doi:https://doi.org/10.2337/dc12-2553.
Arkadianos, I., Valdes, A. M., Marinos, E., Florou, A., Gill, R. D., & Grimaldi, K. A. (2007). Improved weight management using genetic information to personalize a calorie controlled diet. Nutrition Journal, 6, 29.
Bao, W., Hu, F. B., Rong, S., Rong, Y., Bowers, K., Schisterman, E. F., et al. (2013). Predicting risk of type 2 diabetes mellitus with genetic risk models on the basis of established genome-wide association markers: a systematic review. American Journal of Epidemiology. doi:https://doi.org/10.1093/aje/kwt123.
Baum, A., Friedman, A. L., & Zakowski, S. G. (1997). Stress and genetic testing for disease risk. Health Psychology, 16(1), 8–19.
Bloss, C. S., Schork, N. J., & Topol, E. J. (2011). Effect of direct-to-consumer genomewide profiling to assess disease risk. New England Journal of Medicine, 364(6), 524–534. doi:https://doi.org/10.1056/NEJMoa1011893.
Chiu, M., Austin, P. C., Manuel, D. G., Shah, B. R., & Tu, J. V. (2011). Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care, 34(8), 1741–1748. doi:https://doi.org/10.2337/dc10-2300.
Dagogo-Jack, S. (2012). Predicting diabetes: our relentless quest for genomic nuggets. Diabetes Care, 35(2), 193–195. doi:https://doi.org/10.2337/dc11-2106.
Grant, R. W., Moore, A. F., & Florez, J. C. (2009). Genetic architecture of type 2 diabetes: recent progress and clinical implications. Diabetes Care, 32(6), 1107–1114.
Gutierrez, J., & Long, J. A. (2011). Reliability and validity of diabetes specific Health Beliefs Model scales in patients with diabetes and serious mental illness. Diabetes Research and Clinical Practice, 92(3), 342–347. doi:https://doi.org/10.1016/j.diabres.2011.02.018.
Hariri, S., Yoon, P. W., Moonesinghe, R., Valdez, R., & Khoury, M. J. (2006a). Evaluation of family history as a risk factor and screening tool for detecting undiagnosed diabetes in a nationally representative survey population. Genetics in Medicine, 8(12), 752–759.
Hariri, S., Yoon, P. W., Qureshi, N., Valdez, R., Scheuner, M. T., & Khoury, M. J. (2006b). Family history of type 2 diabetes: a population-based screening tool for prevention? Genetics in Medicine, 8(2), 102–108.
Harrison, T. A., Hindorff, L. A., Kim, H., Wines, R. C. M., Bowen, D. J., McGrath, B. B., et al. (2003). Family history of diabetes as a potential public health tool. American Journal of Preventive Medicine, 24(2), 152–159.
Khoury, M. J., Valdez, R., & Albright, A. (2008). Public health genomics approach to type 2 diabetes. Diabetes, 57(11), 2911–2914.
Kuzuya, T., & Matsuda, A. (1982). Family histories of diabetes among Japanese patients with type 1 (insulin-dependent) and type 2 (non-insulin-dependent) diabetes. Diabetologia, 22(5), 372–374.
Leventhal, H., Weinman, J., Leventhal, E. A., & Phillips, L. A. (2008). Health psychology: the search for pathways between behavior and health. Annual Review of Psychology, 59, 477–505.
Markowitz, S. M., Park, E. R., Delahanty, L. M., O’Brien, K. E., & Grant, R. W. (2011). Perceived impact of diabetes genetic risk testing among patients at high phenotypic risk for type 2 diabetes. Diabetes Care, 34(3), 568–573. doi:https://doi.org/10.2337/dc10-1960.
Muhlenbruch, K., Jeppesen, C., Joost, H. G., Boeing, H., & Schulze, M. B. (2013). The value of genetic information for diabetes risk prediction—differences according to sex, age, family history and obesity. PLoS One, 8(5), e64307. doi:https://doi.org/10.1371/journal.pone.0064307.
Nishigaki, M., Kobayashi, K., Hitomi, T., Yokomura, T., Yokoyama, M., Seki, N., et al. (2007). Perception of offspring risk for type 2 diabetes, among patients with type 2 diabetes and their adult offsprings. Diabetes Care, 30(12), 3033–3034.
Nishigaki, M., Sato, E., Ochiai, R., Shibayama, T., & Kazuma, K. (2011). Impact of a booklet about diabetes genetic susceptibility and its prevention on attitudes towards prevention and perceived behavioral change in patients with type 2 diabetes and their offspring. Advances in Preventive Medicine, 2011, 7 pages. doi:https://doi.org/10.4061/2011/365132.
Nishigaki, M., Tokunaga-Nakawatase, Y., Nishida, J., Taru, C., Miyawaki, I., Sanada, H., et al. (2012). Randomized controlled trial of the effectiveness of genetic counseling and a distance, computer-based, lifestyle intervention program for adult offspring of patients with type 2 diabetes: background, study protocol, and baseline patient characteristics. Journal of Nutrition and Metabolism, 831735. doi:https://doi.org/10.1155/2012/831735.
Pierce, M., Ridout, D., Harding, D., Keen, H., & Bradley, C. (2000). More good than harm: a randomised controlled trial of the effect of education about familial risk of diabetes on psychological outcomes. British Journal of General Practice, 50(460), 867–871.
Pijl, M., Timmermans, D. R. M., Claassen, L., Janssens, A. C. J. W., Nijpels, G., Dekker, J. M., et al. (2009). Impact of communicating familial risk of diabetes on illness perceptions and self-reported behavioral outcomes: a randomized controlled trial. Diabetes Care, 32(4), 597–599. doi:https://doi.org/10.2337/dc08-1049.
Rosenstock, I. M. (1966). Why people use health services. Milbank Memorial Fund Quarterly, 44(3), 94–127.
Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the Health Belief Model. Health Education Quarterly, 15(2), 175–183.
Stolerman, E. S., & Florez, J. C. (2009). Genomics of type 2 diabetes mellitus: implications for the clinician. Nature Reviews Endocrinology, 5(8), 429–436.
Valdez, R., Yoon, P. W., Liu, T., & Khoury, M. J. (2007). Family history and prevalence of diabetes in the U.S. population: the 6-year results from the National Health and Nutrition Examination Survey (1999–2004). Diabetes Care, 30(10), 2517–2522.
Vassy, J. L., & Meigs, J. B. (2012). Is genetic testing useful to predict type 2 diabetes? Best Practice & Research Clinical Endocrinology & Metabolism, 26(2), 189–201. doi:https://doi.org/10.1016/j.beem.2011.09.002.
Vassy, J. L., Shrader, P., Jonsson, A., Fox, C. S., Lyssenko, V., Isomaa, B., et al. (2011). Association between parental history of diabetes and type 2 diabetes genetic risk scores in the PPP-Botnia and Framingham Offspring Studies. Diabetes Research and Clinical Practice, 93(2), e76–79. doi:https://doi.org/10.1016/j.diabres.2011.04.013.
Vorderstrasse, A. A., Cho, A., Voils, C. I., Orlando, L. A., & Ginsburg, G. S. (2013). Clinical utility of genetic risk testing in primary care: the example of type 2 diabetes. Personalized Medicine, 10(6), 549–563. doi:https://doi.org/10.2217/pme.13.47.
Whiting, D. R., Guariguata, L., Weil, C., & Shaw, J. (2011). IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Research and Clinical Practice, 94(3), 311–321. doi:https://doi.org/10.1016/j.diabres.2011.10.029.
Acknowledgments
This study was supported by a Grant-in-Aid for Young Scientists (B) 22792255 from the Ministry of Education, Culture, Sports, Science and Technology (MEXT).
Disclosure of Interest
We have no conflict of interest to declare. Authors have full control of all primary data and agree to allow the journal to review our data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishigaki, M., Tokunaga-Nakawatase, Y., Nishida, J. et al. The Effect of Genetic Counseling for Adult Offspring of Patients with Type 2 Diabetes on Attitudes Toward Diabetes and its Heredity: A Randomized Controlled Trial. J Genet Counsel 23, 762–769 (2014). https://doi.org/10.1007/s10897-013-9680-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-013-9680-5