Abstract
Significant research has focused on intimate partner violence (IPV) victimization among women Veterans, yet much less is known about women Veterans’ IPV perpetration. Although military sexual trauma (MST) is a predictor of IPV victimization, military sexual assault (MSA), a component of MST, may predict especially adverse consequences for women Veterans. This study examined the unique effects of MSA on IPV victimization of, and perpetration by, women Veterans, and investigated posttraumatic stress disorder (PTSD) symptoms and prior IPV victimization as potential mediators of IPV perpetration. Participants included 187 women Veterans drawn from a larger web-based survey. We assessed the two components of MST (MSA and harassment) at Time 1 (T1), PTSD symptoms at Time 2 (T2), IPV victimization at T2 and Time 3 (T3), and IPV perpetration at T3. MSA predicted multiple subtypes of IPV victimization and perpetration, whereas harassment predicted neither. Those who reported MSA were more likely to experience T3 psychological and sexual IPV victimization, with PTSD symptoms significantly mediating this path. MSA was also directly related to T3 psychological IPV perpetration and indirectly related to physical and sexual IPV perpetration through PTSD symptoms. MSA was directly related to T2 PTSD symptoms while T2 IPV victimization was directly related to T3 IPV perpetration. These findings underscore that women Veterans’ IPV perpetration may be in response to their own IPV victimization through self-defense and/or due to their PTSD symptoms. Results support prevention, screening, and treatment for IPV victimization and PTSD symptoms to lower risk of future IPV revictimization and perpetration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intimate partner violence (IPV) includes actual or threatened physical violence, sexual violence or coercion, or psychological aggression by an intimate partner (Breiding et al. 2015). These types of experiences are alarmingly common among women Veterans. In fact, a greater proportion of women Veterans experience IPV in their lifetimes as compared to non-veteran peers (33% vs. 24%; Dichter et al. 2011). The type(s) of IPV women experience may have important consequences for differentiated health outcomes, with sexual violence shown to be especially detrimental to IPV survivors (Bonomi et al. 2007; Dichter et al. 2014; Pico-Alfonso et al. 2006). Compared to women Veterans without IPV experiences, those who experienced sexual IPV were up to more than three times as likely to report poorer overall health, difficulty sleeping, cigarette smoking, and problem drinking, and disclose a mental health diagnosis such as posttraumatic stress disorder (PTSD) or depression (Dichter et al. 2014). Yet although sexual IPV may be associated with the most pronounced negative outcomes for physical health, psychological IPV (which includes verbal abuse, intimidation, putdowns, dominance and isolation, etc.), may be uniquely adverse and longstanding, particularly in the domain of psychological outcomes (Dichter et al. 2014; Pico-Alfonso 2005). Experience of psychological aggression is associated with PTSD symptoms (Street and Arias 2001), depression (Coker et al. 2002), anxiety (Taft et al. 2006), shame (Street and Arias 2001), heavy alcohol and drug use (Coker et al. 2002), among other harmful effects. In fact, in a sample of women seeking domestic violence services, psychological IPV was shown to be the strongest predictor of PTSD symptoms compared with all IPV types (Pico-Alfonso 2005). As such, research has focused on identifying the potential pathways and consequences of IPV experiences and PTSD symptoms following IPV experiences, including IPV revictimization and IPV perpetration.
IPV Revictimization
Intimate partner violence victimization is often recurring, with 22–46% of those who have experienced IPV reporting additional victimization (i.e., revictimization) over a 6-months period (Iverson et al. 2011; Iverson et al. 2013b). Future experiences of IPV victimization are especially common among those with PTSD symptoms following interpersonal trauma experiences. Explanations for the relationship between interpersonal trauma (e.g. IPV) and IPV revictimization include decreased ability to detect future risk, cope with risk, and respond to risk (Iverson et al. 2013b); a pathway through re-experiencing symptoms of PTSD (Kuijpers et al. 2012); and difficulties with emotional regulation (Ehring and Quack 2010). In fact, in a study identifying PTSD reexperiencing symptoms as the factor predicting IPV revictimization, 26% reported physical IPV revictimization and 58% reporting psychological IPV revictimization (Kuijpers et al. 2012). Taken together, these explanations provide frameworks for understanding why IPV survivors are at risk for IPV revictimization in the same or different intimate relationship.
IPV Perpetration
Between 17% and 73% of women Veterans may use violence in their relationships (Portnoy et al. 2018a; Creech et al. 2017, respectively). Although additional research is needed to identify the potential gender differences in the function and impact of IPV perpetration, understanding the predictors and factors associated with IPV perpetration among women Veterans is key to preventing future violence. In addition to increasing risk for revictimization, women with PTSD symptoms stemming from, or exacerbated by, interpersonal trauma such as MST and IPV, may be more likely to perpetrate IPV themselves (Creech et al. 2017; Kuijpers et al. 2012). A growing body of research demonstrates that women Veterans’ PTSD symptoms (Kirby et al. 2012; Taft et al. 2011), and IPV victimization history (Creech et al. 2017; Dutra et al. 2012) are associated with their IPV perpetration. Although IPV perpetration may be partially attributed to PTSD symptoms, which are associated with later emotion regulation difficulties (Ehring and Quack 2010), other factors contributing to IPV perpetration among women Veterans remain unknown.
IPV Perpetration as Self-Defense
The causes and motivation of women’s use of violence in relationships is a longstanding and often controversial question. Many have suggested that the causes of women’s IPV perpetration differ from men’s, and that women are more likely to use relationship violence in self-defense or as a consequence of their own IPV victimization (e.g., Kimmel 2002). Self-defense as an attribution for women’s IPV perpetration has been supported in a number of studies with women-only civilian samples (Babcock et al. 2003; Leisring 2012; Miller and Meloy 2006; Rosen et al. 2005; Swan and Snow 2006). However, no research to date examines the self-defense theory within a sample of women Veterans, a unique population due to their military experiences (including the experience of military sexual trauma) and heightened rates of IPV victimization as compared to civilian women (Dichter et al. 2011).
Military Sexual Trauma
Military sexual trauma (MST) refers to sexual assault and repeated threatening sexual harassment during military service. Experiences of MST are associated with numerous negative outcomes including readjustment difficulties following military service, substance use disorders, poorer overall physical, psychological, and social health (Skinner et al. 2000), and IPV victimization (Iverson et al. 2013a; Kimerling et al. 2016). Such experiences are overwhelmingly common among service members, particularly women (Kimerling et al. 2010). Nearly two out of five women Veterans (38.4%) report MST experiences (Wilson 2018), with estimates of up to nearly half (49%) among women Veterans who served in support of the recent conflicts in Iraq and Afghanistan (Barth et al. 2016).
Experiences of MST are associated with both IPV victimization (e.g., Iverson et al. 2013a) and IPV perpetration (e.g., Creech et al. 2017), and as such, may be a unique predictor of IPV among women Veterans. For example, in one study of women VA patients reporting unwanted sexual experiences during military service, MST was associated with doubled increased risk for past year-IPV victimization (Iverson et al. 2013a). In terms of IPV perpetration, more nuanced studies of mediation demonstrate that PTSD symptoms may be differentially associated with psychological IPV perpetration specifically, rather than other IPV subtypes (Dutra et al. 2012; Gold et al. 2007). In contrast, women Veteran’s physical aggression against their partners is uniquely predicted by having experienced physical IPV themselves (Dutra et al. 2012). These distinctions provide support for the consideration that women’s IPV perpetration may be in response to their own victimization, as explored in the present study. Moreover, when women perpetrate IPV in the context of having been victimized (e.g., in self-defense or bidirectional violence), it may increase their own risk for further IPV victimization (Kuijpers et al. 2012). Evidence for the potential role of PTSD symptoms and IPV victimization as factors that may impact women’s IPV perpetration points to the need for further clarification regarding the differing risk factors, pathways, and motives associated with women’s use of IPV, especially over time and through repeated observation.
Conceptualizing MST
The VA’s universal MST screening program utilizes a two-item MST clinical screen to assess military experiences: 1) sexual assault and 2) repeated threatening sexual harassment (Kimerling et al. 2007). To date, much of the research examining MST collapses these screening items into a single variable. In doing so, the two potentially different experiences, military sexual harassment (MSH) and military sexual assault (MSA), are often combined, including in studies examining the links between MST and IPV (Dichter et al. 2017; Iverson et al. 2013a; Kimerling et al. 2016). Accordingly, the potentially unique contributions of MSH and MSA to IPV risk remain unknown.
Disaggregating MST into its MSH and MSA components is important for several reasons. First, the prevalence of MSH and MSA is distinctly different. In a nationally representative sample of women Veterans receiving VA care, 55% reported MSH while 23% reported MSA (Skinner et al. 2000). Additionally, MSH and MSA appear conceptually and practically distinct and may result in different consequences, with sexual assault leading to more damaging outcomes as compared to harassment. Using a more robust measurement of sexual harassment and assault in a sample of former reservists, Street et al. (2008) found that all participants who reported MSA also reported MSH. In fact, MSH appears to be commonly reported alongside MSA, yet not all Veterans who experience harassment in the military also report experiencing sexual assault. Compared to those with MSH only, those with MSA have greater risk of lifetime and current PTSD (Street et al. 2008). Despite the increasingly well-documented literature on the associations between MST and IPV, there is no research to date examining the unique contributions of MSH and MSA on IPV victimization and perpetration.
The Present Study
The main objective of this study was to investigate the pathways among the components of MST (MSH and MSA) and future IPV victimization and IPV perpetration. Specifically, we used a prospective longitudinal design to evaluate the following hypotheses: 1) MSH and MSA would have different associations with future IPV victimization, with MSA having a stronger association than MSH; 1a) the association between MSA and IPV victimization would vary by IPV subtypes, and 1b) these relationships would be mediated by PTSD symptoms. We similarly hypothesized that 2) MSA would have a stronger association with future IPV perpetration than did MSH, 2a) the association between MSA and IPV perpetration would vary by IPV subtypes, and 2b) these relationships would be mediated by PTSD symptoms. Lastly, we hypothesized that 3) associations between MST and IPV perpetration would be mediated by women’s own IPV victimization and that the mediating effect of PTSD on IPV perpetration would no longer be significant once controlling for women’s IPV victimization.
Methods
Procedure and Sample
The sample consisted of women Veterans who participated in the Women Veterans and IPV-related Care Survey (WVICS), a national study of women Veterans’ IPV-related health needs. Potential participants were identified and contacted by GfK, a survey research firm that recruits national random samples and is representative of approximately 97% of U.S. households (see Iverson et al. 2016 for a detailed description of GfK’s Knowledgepanel®). Of the 548 eligible women Veterans in the database, 411 participated in WVICS Time 1 (T1) assessment (75% participation rate). Data was collected at two additional time points for women who were still part of the Knowledgepanel®: Time 2 (T2) (18 months after T1) in which 266 women participated, and Time 3 (6 months after T2) in which 190 women participated. IPV perpetration was only assessed at T3. The present longitudinal study consists of participants who completed the measures of interest at all three time points, resulting in a final study sample of 187 women Veterans.
Measures
Time 1
At T1, we assessed demographic characteristics including age, relationship status, racial identity, sexual orientation, education attained, and status of employment. This time point also included VA’s validated 2-item MST screener (McIntyre et al. 1999) which consists of MSH (i.e., “When you were in the military, did you ever receive unwanted, threatening or repeated sexual attention (for example, touching, cornering, pressure for sexual favors, or inappropriate verbal remarks, etc.?”), and MSA (i.e., “When you were in the military, did you have sexual contact against your will or when you were unable to say no (for example, after being forced or threatened or to avoid other consequences?”). These items have demonstrated high sensitivity and specificity of .89 to .92, respectively, when compared to a clinical interview (McIntyre et al. 1999). Responses to each item were dichotomized (0 = no, 1 = yes).
Time 2
Eighteen months after T1, we assessed PTSD symptoms using the PTSD Checklist-5 (PCL-5; Weathers et al. 2013), a 20-item self-report measure of current DSM-5 PTSD symptom severity associated with traumatic experiences, anchored to general stressful events. Participants respond to PCL-5 items on a 5-point scale. A sum score was created with higher scores indicating higher levels of PTSD symptoms (α = 0.97). The PCL-5 has demonstrated good internal consistency, test-retest reliability, and convergent and discriminant validity with previous samples of Veterans (Bovin et al. 2016).
Time 2 and 3
We used the Revised Conflict Tactics Scale (CTS-2; Straus et al. 1996) to assess prior year IPV victimization at Time 2 and, at Time 3, 6 months after T2, past 6-months IPV victimization and IPV perpetration. The CTS2 consists of 78 items assessing IPV behaviors for which respondents report the frequency of occurrence by either their partner (i.e., 39 statements assessing victimization) or themselves (i.e., 39 statements assessing perpetration). For each statement, participants indicated how frequently they experienced and engaged in each behavior (past 18 months at T2 and in the past 6 months at T3). At T2, we administered the victimization items only; at T3 we administered both the victimization and perpetration items. Consistent with previous research, we administered the three subscales most germane to determining the presence of IPV victimization and perpetration: physical assault (e.g., shoving, punching, choking, and beating up), sexual aggression and coercion (e.g., forcing a partner to do various sexual acts), and severe psychological aggression (e.g., threatening to hit or throw something and destroying things). Responses were scored on a seven-point scale ranging from 0 (“never”) to 6 (“>20 times”). The CTS-2 has well-established psychometric properties across various populations, including good reliability and good construct, convergent, and discriminant validity (Pico-Alfonso 2005; Rabin et al. 2009; Straus et al. 1996). Presence of IPV victimization and perpetration was determined by creating dichotomous outcomes (i.e., frequency > 0) for each of the three CTS-2 subscales, as well as the overall IPV victimization and perpetration scales, a practice consistent with previous research (Houry et al. 2004; Straus et al. 1996).
Data Analysis
We examined descriptive statistics to assess the proportion of women Veterans who reported MSA, MSH, and IPV victimization and perpetration. We then conducted three path analyses to test study hypotheses. First, we conducted a path model to simultaneously assess the total and direct effects of T1 MSA and MSH on T3 IPV victimization subtypes (Hypotheses 1 and 1a), as well as the indirect mediating effect through T2 PTSD symptoms (Hypothesis 1b). To test our second set of hypotheses, we performed a nearly identical path model, assessing IPV perpetration subtypes. Similar to prior research, almost all participants who reported MSA also reported MSH. Therefore, for both models, we dummy coded military sexual traumas into three groups: those who never experienced MST or MSH (the reference group), those who experienced MSH only, and those who experienced MSA (with or without MSH). IPV victimization and perpetration were entered as three dichotomized subtypes: psychological IPV, sexual IPV, and physical IPV. Lastly, we performed a third path model to examine the mediation of MSA on T3 perpetration through both T2 PTSD and T2 victimization (Hypothesis 3). To do so, we conducted an identified model that examined all direct and indirect paths from T1 MSA to both T2 PTSD and T2 IPV victimization (dichotomized as 0 = none, 1 = any), and from T2 variables to T3 IPV perpetration (dichotomized as 0 = none, 1 = any). Next, we ran a more parsimonious model removing all paths other than the hypothesized links between T1 MSA and T2 PTSD symptoms, T2 PTSD symptoms and T2 IPV victimization, and T2 IPV victimization and T3 perpetration, and made modifications as necessary. Mediation was tested by assessing for the presence of a significant indirect effect using a Sobel test. Significant findings were confirmed using a percentile bootstrap procedure with 5000 resamples. We performed all path models using the lavaan package in R, using listwise deletion to account for missing data (<7% was missing across analyses). Because the outcomes variables were dichotomous, we examined path models using diagonally weighted least squares estimation with robust standard errors. This estimation method has been found to work well with non-normally distributed data even with small sample sizes. To examine model fit we used Hu and Bentler’s (1999) criteria of CFI and TLI > .95 and a RMSEA <.06, indicating good fit. Statistical significance of all tests was set at p < .05.
Results
Table 1 presents the demographic characteristics of the sample, along with the MSH and MSA status (assessed at T1) and IPV victimization and perpetration experiences (at T3). The mean age of women Veterans who participated was 54 years and the majority of the sample identified as White/non-Hispanic (72.2%). Most of the participants identified as heterosexual (89.3%), with half reporting being married or living with an intimate partner (59.4%). Almost half of the sample indicated receiving a Bachelor’s degree or higher (47.1%) and half of the participants were employed (50.3%). There were no differences between those who completed all three surveys compared to those that did not on demographic characteristics (i.e., age, race/ethnicity, education, relationship status, and employment) or IPV and MST experiences.
MST and IPV
Approximately half of the women Veterans in the sample (84; 46.5%) reported a history of MST, with 84 women reporting MSH only (44.9%) and 36 women reporting MSA with or without MSH (19.3%, of whom only 3 women did not also report MSH). At T2, slightly more than half reported past year IPV victimization (101; 54.0%). Of the women with data on IPV victimization at T3 (n = 179), a quarter reported past 6-months IPV victimization (48; 25.7%), with 35 women reporting severe psychological IPV victimization (18.7%), 20 reporting physical IPV victimization (10.7%), and 23 reporting sexual IPV victimization (12.3%). Also at T3, 31 women reported past 6-months IPV perpetration (16.6%), with 28 women reporting severe psychological IPV perpetration (15.0%), 16 reporting physical IPV perpetration (8.6%), and 9 reporting sexual IPV perpetration (4.8%). Within the sample of women who perpetrated IPV at T3, all but one (96.8%) had experienced IPV victimization at T2 or T3. A detailed description of the subsample of women Veterans who reported IPV perpetration as well as the differences between those who reported perpetration and victimization is described elsewhere (Portnoy et al. 2018a).
Predicting IPV Victimization
Figure 1 shows the results of our path model assessing the relationships between MSH and MSA with T3 IPV victimization, along with the potential mediating role of T2 PTSD symptoms (hypothesis 1). The direct, indirect, and total effects are provided in Table 2. Compared to women who had never experienced MSH or MSA, women who had experienced MSH did not show any increased associations with T3 sexual, psychological, or physical IPV victimization. Neither the direct effects of MSH on T3 IPV, nor the indirect effect through T2 PTSD symptoms, were significant. Additionally, MSH was only marginally related to increased T2 PTSD symptoms. Conversely, women with MSA experiences had greater T2 PTSD symptoms and stronger associations with both T3 psychological IPV and sexual IPV, yet not physical IPV, compared to women without MSH or MSA. In support of hypotheses, the association of MSA with T3 psychological and sexual IPV was mediated by T2 PTSD symptoms. MSA had a significant indirect effect through T2 PTSD on sexual IPV (β = .10, p < .05) and a marginally significant indirect effect through T2 PTSD on T3 psychological IPV (β = .09, p = .057). Controlling for T2 PTSD symptoms, there was no longer any effect of MSA on any T3 IPV victimization variables.
Path model assessing the relationships between military sexual assault, military sexual harassment, PTSD symptoms, and IPV victimization. Standardized estimates for direct effects are shown. Total effects without mediators are shown in parentheses. Indirect effects are provided in Table 2. †p < .10; *p < .05; **p < .01; ***p < .001
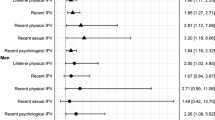
Predicting IPV Perpetration
The path model predicting T3 IPV perpetration is shown in Fig. 2 (hypothesis 2). For women Veterans in our sample, MSH was not related to T2 PTSD symptoms or to any of the IPV perpetration outcomes. There was also no indirect effect of MSH on T3 IPV perpetration through T2 PTSD symptoms. Although MSA was related to T3 IPV perpetration outcomes, the pattern of results was not expected. Overall, MSA was associated with T3 psychological IPV perpetration, yet the direct effect was only marginally significant and the hypothesized indirect effect through PTSD symptoms was not significant. Therefore, PTSD symptoms did not mediate the relationship of MSA with T3 psychological IPV perpetration. Conversely, MSA showed the hypothesized mediated effect through T2 PTSD symptoms on T3 physical IPV and T3 sexual IPV, yet the overall total effects for T3 physical and sexual IPV were not significant.
Path model assessing the relationships between military sexual assault, military sexual harassment, PTSD symptoms, and IPV perpetration. Standardized estimates for direct effects are shown. Total effects without mediators are shown in parentheses. Indirect effects are provided in Table 2. †p < .10; *p < .05; **p < .01; ***p < .001
Mediating Role of PTSD Symptoms and IPV Victimization in Perpetration
Lastly, we tested whether MSA was related to T3 IPV perpetration through an indirect effect of prior IPV victimization (hypothesis 3). The previous path models (Figs. 1 and 2) showed that T2 PTSD symptoms mediated the associations between MSA and T3 IPV victimization and perpetration. Conceptually, we believed that MSA would lead to both PTSD symptoms and IPV victimization at T2. Yet, given that PTSD leads to IPV victimization, and based on past research underscoring the pervasiveness of bidirectional IPV and women’s violence perpetration as self-defense, we predicted that only T2 IPV victimization would be related to T3 IPV perpetration when T2 PTSD and T2 IPV victimization were included in the model together. Therefore, in the final path model we assessed whether T2 PTSD symptoms or T2 IPV victimization would individually mediate the association with T3 IPV perpetration. We found that both the indirect effect of T2 PTSD symptoms on T3 IPV perpetration (β =. -00), and the indirect effect of T2 IPV victimization on T3 perpetration (β = .06) were not significant. Rather, T1 MSA directly predicted T2 PTSD symptoms, T2 PTSD symptoms were associated with T2 victimization, and T2 IPV victimization was associated with increased risk of T3 IPV perpetration. Neither the direct paths from MSA to T2 IPV victimization nor from T2 PTSD to T3 perpetration were significant. Controlling for T2 PTSD and T2 IPV victimization, the association between MSA and T3 IPV perpetration remained significant. We thus assessed a more parsimonious path model that retained the paths from MSA to T2 PTSD and T2 IPV victimization to T3 perpetration. This parsimonious model had a poor fit (χ2 = 11.02, p < .05, CFI = .91, TLI = .81, RMSEA = .12). Yet, retaining the direct path between MSA and T3 IPV perpetration yielded a significantly better fit, χ2 = 8.52, p < .05. Therefore, this path was retained. The final model removing the two nonsignificant paths shown in Fig. 3 had a near perfect fit to the data (χ2 = 2.00, ns, CFI = 1.00, TLI = 1.00, RMSEA = .001).
Path model assessing whether T2 PTSD symptoms and T2 IPV victimization mediate the path from T1 MSA to T3 IPV perpetration. A more parsimonious model (not shown), removing the nonsignificant paths above had a near perfect fit: χ2 = 2.00, ns, CFI = 1.00, TLI = 1.00, RMSEA = .001. Standardized estimates are shown. *p < .05; **p < .01; ***p < .001
Discussion
In the present study, we sought to identify the relationship between the components of MST (MSH and MSA) and future IPV victimization and perpetration. We expected that the association of MSA with future IPV victimization and perpetration would vary by IPV subtypes and be mediated by PTSD symptoms. We also expected that women’s own IPV victimization would mediate the relationship between MSA and IPV perpetration. Overall, the study findings supported our hypotheses. When disaggregating the components of MST, MSA was significantly associated with PTSD symptoms at T2 while MSH was not. Additionally, while MSA predicted multiple forms of recent IPV victimization and perpetration, MSH predicted neither. MSA was significantly associated with both past 6-months psychological and sexual IPV victimization. Furthermore, PTSD symptoms significantly mediated the path from MSA to sexual IPV victimization, and MSA was no longer associated with any IPV types once controlling for PTSD symptoms, demonstrating that PTSD symptoms are a key component to increased risk for IPV victimization following MSA exposure. The relationship between MSA and recent IPV perpetration looked more complex. Although MSA was related to past 6-months psychological IPV perpetration, PTSD symptoms did not mediate this relationship. Conversely, although prior MSA exposure predicted past 6-months physical and sexual IPV perpetration through the mediated effect of PTSD symptoms, the overall relationship between MSA and these IPV types was not significant.
Model fit indices of our final path model incorporating MSA, PTSD symptoms, IPV victimization, and IPV perpetration showed an excellent overall fit to the data. First, the total effect of MSA at T1 predicted overall IPV perpetration reported at T3. Also, T1 MSA was directly related to T2 PTSD symptoms and T2 IPV victimization was directly related to IPV perpetration reported at T3. Finally, there was a significant association between PTSD symptoms and IPV victimization at T2. Conceptually, our final path model suggests prior IPV victimization is more predictive of future IPV perpetration as compared with PTSD symptoms. Our findings also build on the literature demonstrating MST as a risk factor for IPV victimization by increasing our understanding of the role that PTSD symptoms play in this process. Moreover, this study adds to emerging research on women’s IPV perpetration. Findings illustrate that women Veterans’ use of violence in relationships may be due to PTSD symptoms from MSA (Fig. 2) and/or in response to their own IPV victimization (Fig. 3). These findings increase support for the theory of self-defense and/or bidirectional explanations for women Veterans’ perpetration of IPV. To our knowledge, this study is the first to investigate the self-defense theory of IPV perpetration within a sample of women Veterans. In light of the present findings and related past studies, prevention, screening, and treatment for sexual assault and PTSD symptoms may lower the risk of future IPV revictimization and IPV perpetration.
Disaggregating MST
This study provides support for studying the components of MST (MSH and MSA) separately rather than in aggregate. Study findings revealed a relationship between MSA (but not MSH) and recent IPV victimization and perpetration, suggesting that previously identified associations between MST and IPV may in fact be driven by MSA alone. As such, for some research questions, including the one here, it may provide more meaningful information to examine these experiences separately. These results may also indicate the importance of primary prevention efforts to decrease military sexual trauma and support the Department of Defense’s current efforts to implement prevention programs. Intervening in the process prior to MSA exposure is critical. Notably, all but three women Veterans in our sample who reported MSA also reported MSH experiences. As such, sexual harassment may be a significant risk factor for sexual assault and reports of MSH can serve as an opportunity to enact prevention for possible future sexual assault. Unlike other trauma during military service (e.g., combat trauma) MST is a potentially preventable trauma exposure, yet it effects nearly half of recently returning women Veterans (Barth et al. 2016). So, while a response to sexual trauma (e.g. intervention) is critical and should be made available for women Veterans, prevention efforts that decrease MST exposure during military service should also be broadly implemented and evaluated.
PTSD Symptoms and IPV
We found that PTSD symptoms mediated the path from MSA to psychological and sexual IPV victimization. This study is consistent with past research demonstrating that PTSD symptoms increase risk for future traumas, including IPV victimization (e.g., Ehring and Quack 2010; Iverson et al. 2013b; Kuijpers et al. 2012). Prior studies have found that both PTSD symptoms (e.g., re-experiencing, hyperarousal, difficulties concentrating, avoidance, and emotional numbing; Iverson et al. 2013b; Krause et al. 2006; Kuijpers et al. 2012), and related interpersonal difficulties stemming from trauma exposure (e.g., relationship conflict, anger, and emotion dysregulation; Ehring and Quack 2010) may be involved with heightened risk of future trauma, such as IPV. Research also shows that for women sexual assault survivors, PTSD symptoms, maladaptive coping strategies, and negative social reactions from others are reciprocally reinforcing (Ullman and Relyea 2016). Thus, the emotional distress or challenges following MSA exposure may interfere with women Veteran’s access to resources, social support, or use of effective coping strategies, potentially contributing to risk for future interpersonal trauma, such as IPV. Experiences of interpersonal violence, both in terms of MSA and IPV, may impact one’s ability to detect future risk and cope effectively with that risk, thereby increasing risk of future IPV (Iverson et al. 2013b). The large segment of women Veterans exposed to MST and IPV is especially concerning given that women Veterans with histories of interpersonal trauma report chronic and recurrent trauma exposure alongside lower self-reported resilience when compared to those who experience traumas that does not include MST or IPV (Portnoy et al. 2018b).
The present study findings support prior research that suggests identifying and treating PTSD symptoms among MST survivors, may also reduce risk for future IPV victimization (Iverson et al. 2011). Although many studies examine the outcomes of MST within treatment-seeking samples, our study demonstrates the associations between MSA, PTSD symptoms, and IPV within a general sample of women Veterans. Survivors of interpersonal trauma, such as sexual assault, do not always immediately seek treatment, and trauma symptoms can persist for a long period of time without treatment; therefore, including non-treatment seekers in studies of the sequela of MST is critical. Moreover, although screening for both PTSD and MST have been implemented in VA, IPV screening implementation is still in the early stages of adoption. Yet accurate screening tools exist for IPV screening and women Veterans find screening for both IPV victimization and perpetration acceptable (Iverson et al. 2014; Portnoy et al. 2018a, respectively). In light of the present study findings illustrating the significant relationship between IPV victimization and perpetration, enhancing efforts to detect IPV among women Veterans and connect those who experience IPV to services may serve to decrease future trauma-related symptoms as well as future IPV perpetration.
This research adds to a growing body of research demonstrates that women Veterans’ PTSD symptoms (Kirby et al. 2012; Taft et al. 2011), and IPV victimization history are also associated with their IPV perpetration (Creech et al. 2017; Dutra et al. 2012). A similar conceptual framework as the one described above was adopted in order to develop Strength at Home (SAH), a trauma-informed, cognitive-behavioral, treatment for Veterans who perpetrate relationship violence. In the only randomized controlled clinical trial to date evaluating IPV perpetration treatment for Veteran men, Taft and colleagues showed that SAH reduces future physical and psychological IPV use (Creech et al. 2018; Taft et al. 2016), PTSD symptoms (Creech et al. 2018), and alexithymia (Berke et al. 2017). Present study findings demonstrate significant paths between PTSD symptoms and IPV perpetration among women Veterans, emphasizing the value of trauma-informed intervention for IPV use among women, as well. Future studies should evaluate the effects of SAH and other trauma-informed IPV perpetration interventions in samples of women Veterans who have used violence in their relationship or may be at risk to do so. However, unlike past studies demonstrating that women’s perpetration of psychological IPV is associated with PTSD symptoms (Dutra et al. 2012; Gold et al. 2007), the present study showed that PTSD symptoms mediate women’s physical and sexual (but not psychological) IPV perpetration (Fig. 2). Perhaps in our sample of women Veterans, variables other than PTSD that were not examined in this study were more strongly associated with psychological IPV perpetration. For example, relationship dissatisfaction has been found to be a unique risk factor for recent psychological IPV perpetration among women Veterans (Creech et al. 2017). As such, future research of psychological IPV perpetration by women Veterans would benefit from including such relationship-specific variables into their studies.
There is a growing interest in women Veterans’ IPV perpetration as more women are joining the Armed Forces, performing more diverse tasks during military service, and reintegrating into their families following military discharge. Yet limited research has examined women Veterans’ IPV perpetration, including the potentially differential patterns of IPV perpetration among women Veterans. As such, research on sexual IPV perpetration by women Veterans specifically is lacking. Our study is the first to demonstrate a significant relationship between sexual assault during military service and self-reported recent sexual IPV perpetration mediated by PTSD symptoms. Many of the same PTSD-related explanations described above likely account for women Veterans’ perpetration of sexual violence. An additional consideration for these findings includes the specific types of IPV behaviors assessed with the CTS-2. Speculatively, women who endorse items related to insisting on sex may be reflecting difficulties in sexual and relationship communication and/or pressuring their male partners to have sex without a condom in order to become pregnant.
Importantly, these findings offer further support for the critical role that prior interpersonal trauma, in this case military sexual assault and IPV, and PTSD symptoms together play in women’s violence perpetration. Many have posited that the purpose, motives, and function of women’s IPV perpetration may be different from men’s, and several studies have shown that civilian women are likely to use relationship violence in self-defense. However, the present study is the first to examine the self-defense theory of IPV perpetration in a sample of women Veterans. Our findings shed light on the possible mechanisms through which IPV experiences and future IPV perpetration may be related. Taken together, these path models indicate that an MSA history predicts future physical and sexual IPV perpetration through PTSD symptoms, and that recent IPV victimization predicts IPV perpetration. These findings demonstrate that for women Veterans in our sample, IPV perpetration appears to follow PTSD symptoms and their own IPV victimization. Because IPV victimization was assessed at T2, we cannot definitively know that the women in our sample were perpetrating T3 IPV in self-defense or using reciprocal violence directly following episodes of IPV victimization. However, our path model suggests that these are plausible explanations as IPV perpetration was assessed 6 months after victimization, during which time it is likely that the IPV victimization persisted. Furthermore, despite the correlation between PTSD symptoms and IPV victimization at T2, the strongest path in the model was the one from IPV victimization to perpetration. Finally, within the sample of women who perpetrated IPV at T3, nearly all experienced IPV victimization at T2 or T3. These analyses provide contextualization of the pathways from MSA to IPV perpetration, illustrating that women’s use of violence in relationships may be largely explained by their own IPV victimization or through self-defense. However, the use of violence in relationships is complex and rarely attributable to singular or isolated factors. Future research examining women Veterans’ IPV use is needed, especially given that perpetrating IPV may create an environment in which women are at heightened risk for IPV victimization (Fergusson et al. 2005). Daily diary studies may be one way to tease out the process and complexities of bidirectional IPV and help understand the temporal relationship between victimization and perpetration.
Limitations
Study findings should be considered in light of several limitations. First, it is possible that the paths between MSA, PTSD symptoms, and IPV are accounted for by variables that were not included in the study. For example, due to the relatively small number of individuals reporting subtypes of IPV victimization and IPV perpetration, we were not powered to examine how background characteristics may have affected the path models. Future research would benefit from examining this model using a larger set of risk factors, protective factors, and mediators of the MST-PTSD-IPV relationship. Second, this study assessed MST experiences in a dichotomous fashion. It is possible that women who experienced more severe or frequent MST were less likely to complete all three surveys. Third, our sample of women who reported recent IPV perpetration was small (n = 31). Although robust diagonal weighted least squares is more robust in smaller sample sizes than other path model estimation methods, the moderate sample we had here can result in less stable estimates than larger sample sizes. As such, future research should replicate the current study in larger samples of women Veterans; this is especially important to clarify the prevalence and risk factors of sexual IPV perpetration, which only nine women reported. Fourth, the current analysis used variable focused approaches that examined the relationships between two components of MST, PTSD, and multiple forms of IPV. Yet the majority of participants who had one form of IPV victimization or IPV perpetration had more than one form. Therefore, future studies using person-centered approach that examined groups with different patterns of victimization and perpetration history may be useful. Finally, future research should investigate these findings in non-Veteran, mixed-gender, samples to test whether the results generalize to other demographic groups that have experienced sexual trauma.
Measurement issues may also be of concern. Both MSA and MSH were assessed with one-item measures. These are the standard screening items within the VA, yet more rigorous assessment of MSA and MSH may produce different results. Second, although the CTS-2 is considered a gold standard for IPV assessment, it is not a comprehensive measure of sexual aggression in relationships. Moreover, the CTS-2 assesses the presence of IPV behavior but neglects context, including preceding factors and circumstances, in which IPV occurs. As such, a significant critique of using the measure among women is its inability to meaningfully account for instances in which women use physical means, or forms of self-defense that resemble IPV, to defend themselves (Kimmel 2002). This is especially relevant for our sample of women Veterans as the strongest association in our path model was the one in which IPV victimization predicted IPV perpetration.
Few studies disaggregate the construct of MST into sexual harassment and sexual assault (Skinner et al. 2000); doing so in the present study enabled us to assess the potentially unique contributions of each MST component. This was the first study to our knowledge to demonstrate the unique effect of past military sexual assault on future IPV perpetration in addition to victimization, as well as the first to test the self-defense theory of women’s IPV perpetration in a sample of women Veterans. Furthermore, we illustrated that PTSD is critical in the relationship between MSA and multiple forms of IPV. Our findings suggest that PTSD symptoms and IPV victimization are relevant in explaining risk for IPV perpetration among women Veterans, demonstrating the importance of detecting and treating both types of IPV as well as PTSD symptoms. This is especially notable given that the purpose, motives, and risk factors associated with women’s use of violence in relationships may be interconnected and complex. Understanding the motives and risk factors of IPV perpetration unique to women Veterans can inform the development of prevention and treatment programs, which may differ from those geared towards men. In so far as MSA appears to predict future IPV victimization and perpetration, PTSD symptoms seem to play a strong role in this process. As such, a comprehensive approach that combines prevention, screening, and treatment for MST, IPV, and PTSD symptoms are critical to addressing the health needs of women Veterans returning from military conflicts.
References
Babcock, J. C., Miller, S. A., & Siard, C. (2003). Toward a typology of abusive women: Differences between partner-only and generally violent women in the use of violence. Psychology of Women Quarterly, 27(2), 153–161.
Barth, S. K., Kimerling, R. E., Pavao, J., McCutcheon, S. J., Batten, S. V., Dursa, E., Peterson, M. R., & Schneiderman, A. I. (2016). Military sexual trauma among recent veterans: Correlates of sexual assault and sexual harassment. American Journal of Preventive Medicine, 50(1), 77–86.
Berke, D. S., Macdonald, A., Poole, G. M., Portnoy, G. A., McSheffrey, S., Creech, S. K., & Taft, C. T. (2017). Optimizing trauma-informed intervention for intimate partner violence in veterans: The role of alexithymia. Behaviour Research and Therapy, 97, 222–229.
Bonomi, A. E., Anderson, M. L., Rivara, F. P., & Thompson, R. S. (2007). Health outcomes in women with physical and sexual intimate partner violence exposure. Journal of Women's Health, 16(7), 987–997.
Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391.
Breiding, M. J., Basile, K. C., Smith, S. G., Black, M. C., & Mahendra, R. R. (2015). Intimate partner violence surveillance: Uniform definitions and recommended data elements. Atlanta: National Center for Injury Prevention and Control.
Coker, A. L., Davis, K. E., Arias, I., Desai, S., Sanderson, M., Brandt, H. M., & Smith, P. H. (2002). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23, 260–268.
Creech, S. K., Macdonald, A., & Taft, C. (2017). Use and experience of recent intimate partner violence among women veterans who deployed to Iraq and Afghanistan. Partner Abuse, 8(3), 251–271.
Creech, S. K., Benzer, J. K., Ebalu, T., Murphy, C. M., & Taft, C. T. (2018). National implementation of a trauma-informed intervention for intimate partner violence in the Department of Veterans Affairs: First year outcomes. BMC Health Services Research, 18(1), 582.
Dichter, M. E., Cerulli, C., & Bossarte, R. M. (2011). Intimate partner violence victimization among women veterans and associated heart health risks. Women's Health Issues, 21, S190–S194. https://doi.org/10.1016/j.whi.2011.04.008.
Dichter, M. E., Marcus, S. C., Wagner, C., & Bonomi, A. E. (2014). Associations between psychological, physical, and sexual intimate partner violence and health outcomes among women veteran VA patients. Social Work in Mental Health, 12(5–6), 411–428.
Dichter, M. E., Haywood, T. N., Butler, A. E., Bellamy, S. L., & Iverson, K. M. (2017). Intimate partner violence screening in the veterans health administration: Demographic and military service characteristics. American journal of preventive medicine, 52(6), 761–768.
Dutra, L., de Blank, G., Scheiderer, E., & Taft, C. (2012). Correlates of female veterans' perpetration of relationship aggression. Psychological Trauma Theory Research Practice and Policy, 4(3), 323–329.
Ehring, T., & Quack, D. (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41, 587–598.
Fergusson, D. M., Horwood, L. J., & Ridder, E. M. (2005). Partner violence and mental health outcomes in a New Zealand birth cohort. Journal of Marriage and Family, 67, 1103–1119. https://doi.org/10.1111/j.1741-3737.2005.00202.x.
Gold, J. I., Taft, C. T., Keehn, M. G., King, D. W., King, L. A., & Samper, R. E. (2007). PTSD symptom severity and family adjustment among female Vietnam veterans. Military Psychology, 19, 71–81. https://doi.org/10.1080/08995600701323368.
Houry, D., Feldhaus, K., Peery, B., Abbott, J., Lowenstein, S. R., Al-Bataa-de-Montero, S., & Levine, S. (2004). A positive domestic violence screen predicts future domestic violence. Journal of Interpersonal Violence, 19(9), 955–966. https://doi.org/10.1177/0886260504267999.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55.
Iverson, K. M., Gradus, J. L., Resick, P. A., Suvak, M. K., Smith, K. F., & Monson, C. M. (2011). Cognitive-behavioral therapy for PTSD and depression symptoms reduces risk for future intimate partner violence among interpersonal trauma survivors. Journal of Consulting and Clinical Psychology, 79, 193–202. https://doi.org/10.1037/a0022512.
Iverson, K. M., Litwack, S. D., Pineles, S. L., Suvak, M. K., Vaughn, R. A., & Resick, P. A. (2013a). Predictors of intimate partner violence revictimization: The relative impact of distinct PTSD symptoms, dissociation, and coping strategies. Journal of Traumatic Stress, 26(1), 102–110.
Iverson, K. M., Mercado, R., Carpenter, S. L., & Street, A. E. (2013b). Intimate partner violence among women veterans: Previous interpersonal violence as a risk factor. Journal of Traumatic Stress, 26, 767–771.
Iverson, K. M., Huang, K., Wells, S. Y., Wright, J. D., Gerber, M. R., & Wiltsey-Stirman, S. (2014). Women veterans' preferences for intimate partner violence screening and response procedures within the veterans health administration. Research in Nursing & Health, 37(4), 302–311.
Iverson, K. M., Stirman, S. W., Street, A. E., Gerber, M. R., Carpenter, S. L., Dichter, M. E., ... Vogt, D. (2016). Female veterans' preferences for counseling related to intimate partner violence: Informing patient-centered interventions. General Hospital Psychiatry, 40, 33–38.
Kimerling, R., Gima, K., Smith, M. W., Street, A., & Frayne, S. (2007). The veterans health administration and military sexual trauma. American Journal of Public Health, 97, 2160–2166. https://doi.org/10.2105/AJPH.2006.092999.
Kimerling, R., Street, A. E., Pavao, J., Smith, M. W., Cronkite, R. C., Holmes, T. H., & Frayne, S. M. (2010). Military-related sexual trauma among veterans health administration patients returning from Afghanistan and Iraq. American Journal of Public Health, 100, 1409–1412. https://doi.org/10.2105/AJPH.2009.171793.
Kimerling, R., Iverson, K. M., Dichter, M. E., Rodriguez, A. L., Wong, A., & Pavao, J. (2016). Prevalence of intimate partner violence among women veterans who utilize veterans health administration primary care. Journal of General Internal Medicine, 31(8), 888–894.
Kimmel, M. S. (2002). “Gender symmetry” in domestic violence: A substantive and methodological research review. Violence Against Women, 8(11), 1332–1363.
Kirby, A. C., Beckham, J. C., Calhoun, P. S., Roberts, S. T., Taft, C. T., Elbogen, E. B., & Dennis, M. F. (2012). An examination of general aggression and intimate partner violence in women with posttraumatic stress disorder. Violence and Victims, 27(5), 777–792.
Krause, E. D., Kaltman, S., Goodman, L., & Dutton, M. A. (2006). Role of distinct PTSD symptoms in intimate partner reabuse: A prospective study. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 19(4), 507–516.
Kuijpers, K. F., van der Knaap, L. M., & Winkel, F. W. (2012). PTSD symptoms as risk factors for intimate partner violence revictimization and the mediating role of victims' violent behavior. Journal of Traumatic Stress, 25(2), 179–186.
Leisring, P. A. (2012). Physical and emotional abuse in romantic relationships: Motivation for perpetration among college women. Journal of Interpersonal Violence, 28, 1437–1454. https://doi.org/10.1177/0886260512468236.
McIntyre, L. M., Butterfield, M. I., Nanda, K., Parsey, K., Stechuchak, K. M., McChesney, A. W., Koons, C., & Bastian, L. A. (1999). Validation of a trauma questionnaire in veteran women. Journal of General Internal Medicine, 14(3), 186–189.
Miller, S., & Meloy, M. (2006). Women’s use of force: Voices of women arrested for domestic violence. Violence Against Women, 12, 89–115. https://doi.org/10.1177/1077801205277356.
Pico-Alfonso, M. A. (2005). Psychological intimate partner violence: The major predictor of posttraumatic stress disorder in abused women. Neuroscience & Biobehavioral Reviews, 29(1), 181–193.
Pico-Alfonso, M. A., Garcia-Linares, M. I., Celda-Navarro, N., Blasco-Ros, C., Echeburúa, E., & Martinez, M. (2006). The impact of physical, psychological, and sexual intimate male partner violence on women's mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. Journal of Women's Health, 15(5), 599–611.
Portnoy, G. A., Haskell, S. G., King, M. W., Maskin, R., Gerber, M. R., & Iverson, K. M. (2018a). Accuracy and acceptability of a screening tool for identifying intimate partner violence perpetration among women veterans: a pre-implementation evaluation. Women’s Health Issues, 28(5), 439–445.
Portnoy, G. A., Relyea, M. R., Decker, S., Shamaskin-Garroway, A., Driscoll, M., Brandt, C. A., & Haskell, S. G. (2018b). Understanding gender differences in resilience among veterans: Trauma history and social ecology. Journal of Traumatic Stress, 31(6), 845–855. https://doi.org/10.1002/jts.22341.
Rabin, R. F., Jennings, J. M., Campbell, J. C., & Bair-Merritt, M. H. (2009). Intimate partner violence screening tools: A systematic review. American Journal of Preventive Medicine, 36, 439–445. https://doi.org/10.1016/j.amepre.2009.01.024.
Rosen, K. H., Stith, S. M., Few, A. L., Daly, K. L., & Tritt, D. R. (2005). A qualitative investigation of Johnson’s typology. Violence and Victims, 20, 319–334. https://doi.org/10.1891/vivi.20.3.319.
Skinner, K. M., Kressin, N., Frayne, S., Tripp, T. J., Hankin, C. S., Miller, D. R., & Sullivan, L. M. (2000). The prevalence of military sexual assault among female Veterans' Administration outpatients. Journal of Interpersonal Violence, 15(3), 291–310.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The revised conflict tactics scale (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17, 283–316. https://doi.org/10.1177/019251396017003001.
Street, A. E., & Arias, I. (2001). Psychological abuse and PTSD in battered women: Examining the roles of shame and guilt. Violence and Victims, 16(1), 65–78.
Street, A. E., Stafford, J., Mahan, C. M., & Hendricks, A. (2008). Sexual harassment and assault experienced by reservists during military service: Prevalence and health correlates. Journal of Rehabilitation Research and Development, 45(3), 409–420.
Swan, S., & Snow, D. (2006). The development of a theory of women’s use of violence in intimate relationships. Violence Against Women, 12, 1026–1045.
Taft, C. T., O’Farrell, T. J., Torres, S. E., Panuzio, J., Monson, C. M., Murphy, M., et al. (2006). Examining the correlates of psychological aggression among a community sample of couples. Journal of Family Psychology, 20, 581–588.
Taft, C. T., Watkins, L. E., Stafford, J., Street, A. E., & Monson, C. M. (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79(1), 22–33. https://doi.org/10.1037/a0022196.
Taft, C. T., Macdonald, A., Creech, S. K., Monson, C. M., & Murphy, C. M. (2016). A Randomized Controlled Clinical Trial of the Strength at Home Men's Program for Partner Violence in Military Veterans. The Journal of clinical psychiatry, 77(9), 1168–1175.
Ullman, S. E., & Relyea, M. (2016). Social support, coping, and posttraumatic stress symptoms in female sexual assault survivors: A longitudinal analysis. Journal of Traumatic Stress, 29(6), 500–506.
Weathers, F. W., B. T. Litz, T. M. Keane, P. A. Palmieri, B. P. Marx, and P. P. Schnurr. 2013. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
Wilson, L. C. (2018). The prevalence of military sexual trauma: A meta-analysis. Trauma, Violence & Abuse, 19(5), 584–597. https://doi.org/10.1177/1524838016683459.
Funding Statement
This research was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development (HSR&D) as part of Dr. Katherine Iverson’s HSR&D Career Development Award (CDA 10–029), and HSR&D Award PPO 17–044 and her Presidential Early Career Award for Scientists and Engineers (USA 14–275). Dr. Iverson is an fellow with the Implementation Research Institute, at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (5R25MH08091607) and the VA HSR&D Services, Quality Enhancement Research Initiative. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Portnoy, G.A., Relyea, M.R., Street, A.E. et al. A Longitudinal Analysis of Women Veterans’ Partner Violence Perpetration: the Roles of Interpersonal Trauma and Posttraumatic Stress Symptoms. J Fam Viol 35, 361–372 (2020). https://doi.org/10.1007/s10896-019-00061-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-019-00061-3






