Abstract
Intimate partner violence affects one in three U.S. women. Children often witness the violence. Methods: A 4-year cohort analysis of 300 mother-child dyads used latent growth curve techniques to examine the impact of partner violence on mothers’ and children’s mental health and function over time. The dyads entered the study when the mother sought safe shelter or justice services. Data was collected every four months, 13 times. Results: Four models were derived, each with good fit. Maternal age, Adverse Childhood Events, and ethnicity determined the level of maternal PTSD, depression, and anxiety at baseline. Mothers’ self-efficacy and marginalization determined if maternal mental health symptoms decreased or increased over 4-years. Maternal symptom levels determined if child dysfunctions persisted over time. Conclusion: This analysis provides longitudinal evidence that maternal mental health determines children’s recovery from or persistence of behavioral dysfunctions. Primary prevention and informed referral has the potential to improve child outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The latest National Intimate Partner and Sexual Violence Survey is an ongoing nationally representative random-digit–dial telephone survey of the non-institutionalized English- and Spanish-speaking U.S. population, aged ≥18 years. Findings indicated that 31.5% of American women experience intimate partner violence (IPV) at some point during their lives (Breiding et al. 2014). Severe IPV, such as being hit with something hard, kicked or beaten, or being burned on purpose, was reported by 22.3% of the surveyed women. Almost 9% of the women reported rape by an intimate partner (lifetime prevalence 8.8%). Women who report IPV also report long-term mental health problems, especially Post Traumatic Stress Disorder (PTSD) and depression (Johnson and Zlotnick 2012).
Women abused by intimate partners have often experienced previous victimization in their own childhood homes, either physical or sexual abuse or neglect (Abramsky et al. 2011; Cannon et al. 2010; Felitti et al. 1998). Women who experience IPV frequently have children who witness the violence. National surveys indicate that each year millions of U.S. children are exposed to parental IPV (Hamby et al. 2011; Jouriles et al. 2009). Close to half of these children are exposed to acts of severe IPV (Jouriles et al. 2009).
The children become secondary victims of the violence and frequently exhibit adjustment difficulties, especially externalizing and internalizing problems (Blair et al. 2015; Binder et al. 2013). Exposure to violence and the pass through effect of maternal mental health predicting child behavioral function has been validated with structural models using cross-sectional data (Fredland et al. 2015; Fredland et al. 2016; McFarlane et al. 2014).
Determining the intergenerational impact of IPV and subsequent child dysfunction over time will enable targeted primary, secondary, and tertiary prevention strategies to prevent and interrupt the pass through of violence from mother to child. Toward this end, a longitudinal study is underway to examine the relationship between mothers’ trauma and child functioning over a 4-year period. The purpose of this longitudinal study is to establish the impact and strength of association between variables that determine the intergenerational transmission of poor functioning of mothers on dysfunctions of their children over time.
Aim
The purpose of this 4-year longitudinal analysis is to establish the impact and strength of association between variables that determine the intergenerational transmission of poor functioning of mothers on dysfunctions of their children over time.
Methods
Procedures and Sample
This research is part of an Internal Review Board approved multi-year study, the details are explained elsewhere (McFarlane et al. 2012). In brief, 300 women reporting IPV were recruited from shelters (n = 150) and the district attorney’s office (n = 150) in a large urban area in the U.S.
Women eligible for the study spoke English or Spanish; reported intimate partner violence; qualified for shelter or a protection order; and had at least one child between 18 months and 16 years. Following signed informed consent, baseline measures of frequency and severity of abuse, IPV danger assessment, mental health measures of depression, anxiety, somatization, and post-traumatic stress disorder (PTSD), measures of self-efficacy, marginalization, and the mothers’ and abusers’ history of adverse childhood experiences (ACE) were collected. Additionally, an index child’s functioning was assessed using the Child Behavior Checklist and the mother was asked if the child had heard, seen, or tried to stop the abuse against the mother.
The measures were repeated every four months. Interviews were conducted in English and Spanish. Four years into the study, 92% of the mothers (n = 277) and their children were retained. Among the 23 mothers not retained, eight mothers withdrew from the study, 14 mothers were lost to follow-up, and one mother died of a heart attack. The retained 277 mothers completed all measures, every four months for four years, resulting in 13 evenly distributed measurement periods. The interviews were completed by an experienced interviewer at a time and location convenient for the mother. A safety and retention protocol was followed (McFarlane 2007).
At baseline, the largest percentage of mothers self-identified as being Spanish or Hispanic (56.7%). Although the majority of mothers were U.S. born (64.3%), 36% were immigrants, primarily from Mexico. The median age of the mothers and children was 30 years and seven years, respectively. There were slightly more boys (50.7%) than girls (49.3%,). More than half of children (52.3%) had witnessed their mother’s physical abuse.
Measures
All survey items were prefaced with “during the last four months”. Participants were first interviewed within 48-h of initial contact with either the safe shelter or justice services. Measures chosen for this analysis were examined in earlier cross-sectional, structural models (baseline and 24 months) and linked to the intergenerational transmission of violence (Fredland et al. 2015; Fredland et al. 2016; McFarlane et al. 2014). Those cross-sectional predictive models of maternal mental health on child functioning were theoretically and statistically significant.
Post-Traumatic Stress Disorder
PTSD symptomatology was assessed using the 7-item symptom scale for PTSD, which is a subset of items extracted from the National Institute of Mental Health Diagnostic Interview Schedule for PTSD (Breslau et al. 1999). When the 7-item scale was evaluated for predictive validity in a National Epidemiological Survey, a score of four or more on the 7-item scale identified cases of PTSD with sensitivity of 78%, specificity of 97%, positive predictive value of 75%, and negative predictive value of 98%. The percentage of correctly classified respondents was 96% (Bohnert and Breslau 2011).
Brief Symptom Inventory (BSI)
This 18-items shorter version of the BSI-53 includes three measures of psychological distress: depression, anxiety, and somatization, and one measure of overall psychological distress: the global severity index. Internal consistency reliability ranges from 0.74 to 0.89 on the subscales. Test-retest reliability over two weeks ranged from 0.68 to 0.91 (Derogatis and Lazarus 2001).
Achenbach Child Behavior Checklist (CBCL)
This measure of child behavioral functioning has two forms. One for ages 1.5 to 5 years and another for 6–18 years (Achenbach and Rescorla 2000; Achenbach and Rescorla 2001). The CBCL provides a parental report of the extent of a child’s behavioral problems and social competencies (Achenbach and Rescorla 2001). The parent rates the presence and frequency of certain child behaviors on a 3-point scale (0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true). The recall period is the previous two months for young children and six months for older children. The CBCL includes two broad factors of behavioral problems: internalizing and externalizing with mean scale scores for national normative samples as well as clinically referred and non-referred samples of children. Extensive psychometric testing has yielded favorable validity and reliability for English and Spanish versions of the tool (Achenbach and Rescorla 2000; Achenbach and Rescorla 2001). For this study raw scores were converted into standard scores based on a child’s age and gender, as recommended by instrument developers. Due to unequal group sizes, children who did not have Normative scores were collapsed into one group (e.g., Borderline/Clinical levels).
Adverse Childhood Experiences (ACE)
The ACE, a 10-item scale, measures a variety of negative household experiences including childhood abuse (sexual and physical), domestic violence, and drug and alcohol abuse (Centers for Disease Control and Prevention 1997, 2010). Mothers were asked to respond to whether or not they experienced a particular event as a child. Higher scores indicate a greater number of ACEs.
General Self-Efficacy Scale (GSE)
This 10-item instrument assesses perceived self-efficacy for coping and adaptation after stressful life events. Responses to each item are made on a 4-point scale: 1 = Not at all true, 2 = Hardly true, 3 = Moderately true, 4 = Exactly true. The possible range of scores is 10 to 40. Criterion-related validity is documented in numerous correlation studies where positive correlations were found with favorable emotions and negative correlations were found with depression, anxiety, and somatization. In samples from 23 countries, Cronbach’s alphas ranged from .76 to .90 with the majority of alphas in the high .80s (Schwarzer and Jerusalem 1995).
Koci Marginality Index (KMI)
This 5-item, abbreviated version of the KMI-95 items and KMI-70 items uses a 5-point Likert scale to assess women’s marginality, their perception of living on the periphery of the social center. Women are asked to endorse five questions with responses of: 1 = Strongly Disagree, 2 = Disagree, 3 = Neither Disagree or Agree, 4 = Agree, and 5 = Strongly Agree. Responses are summed and scores range from 5 to 25. An example of a question is: “Meeting new people is hard for me”. The higher the score, the more marginalized the woman. The internal consistency of the (KMI-70) was Cronbach alpha 0.96 and the shorter 5-item version was 0 .84 (Koci et al. 2012).
Data Analysis
Latent growth curve modeling (LGC) was used to analyze the change of maternal PTSD scores and BSI global scores, children’s CBCL internalizing and externalizing scores, and the relationships among them over time. A linear model failed to provide adequate fit, so a quadratic model was used to delineate the trends. The model was built in the Structure Equation Modeling (SEM) framework. Three latent variables, intercept, linear component, and quadratic component, were estimated to describe the characteristics of the trends. The intercept reflected the initial levels, the linear component reflected the change rates, and the quadratic component reflected the curvature of the curve. Model fit was assessed by inspecting the comparative fit index (CFI), root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR) (Kline 2010). The CFI is considered an incremental measure of fit. Values greater than .90 indicate acceptable model fit and values greater than .95 indicate excellent model fit. The RMSEA examines the extent to which the model, with unknown but optimally chosen parameter values, fits the population covariance matrix. Values greater than .10 indicate that the model is a poor fit. Values ranging from .05 to .08 indicate that the model is an acceptable fit. Values less than .05 indicate that the model is an excellent fit to the data. The SRMR examines the absolute difference between the observed and the model-implied correlations. Values less than .10 indicate acceptable fit. Values less than .08 indicate good fit.
First, unconditioned growth curve models were fitted for maternal PTSD scores, maternal BSI global scores, and children’s internalizing and externalizing scores. Then, time-invariant covariates and time-variant covariates were added into the models. By checking the model fit statistics and significance of each covariate, the best models were selected. The covariates that were not significant were removed from the model as long as the overall model quality did not suffer by their removal. The time-invariant covariates assessed included mother’s age, months in abusive relationship, mother’s education, mother’s race/ethnicity, child’s gender, child heard/seen/tried to stop abuse, mother’s immigrant status, site (district attorney (DA) or shelter services), mother’s adverse childhood events (ACE) score. The time-variant covariates assessed included self-efficacy, marginalization, severity of violence, and danger assessment.
All analyses were conducted in Mplus Version 7.31 (Muthén and Muthén 2012). The maximum likelihood estimator was used. Prior to testing the LGC models, multiple imputations were used to recover missing data, and the average results were presented.
Results
The means and standard deviations of the outcome variables at each of the time points are presented in Table 1, and the results of unconditioned LGC are presented in Table 2. As shown, the models for maternal PTSD and BSI global scores (i.e., depression, anxiety, and somatization) failed to achieve adequate fit; however, the models for CBCL internalizing and externalizing scores fit well. The intercepts, linear components, and quadratic components were statistically significant for all models except the quadratic component in the CBCL externalizing model. The intercepts of the models indicate the starting values of the outcome variables. The negative linear component indicates that the outcome variable was decreased, and the positive quadratic component indicates that the decrease became slower over time.
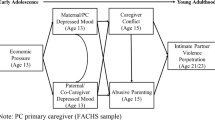
Next, the time-invariant and time-variant covariates were added into the model. The model of maternal PTSD scores is presented in Table 3. After adding covariates, the model fit well, RMSEA = .028, CFI = .958, SRMR = .040. As shown in Fig. 1, mother’s age and mother’s ACE score had significant effects on the intercept, p < .01, p < .001 respectively. Older mothers had higher initial PTSD scores, and mothers with higher ACE scores had higher initial PTSD scores. Ethnicity had significant effects on the linear component, p < .01. Hispanic mothers’ PTSD decreased faster than that of non-Hispanic mothers. Self-efficacy and marginalization had significant effects on PTSD at each time point, all p values < .01. The effects of self-efficacy were negative and became stronger as time progressed from entry into the study to 48 months. Mothers who had higher self-efficacy had lower PTSD. The effects of marginalization were positive. Mothers who were more marginalized had higher PTSD.
The model for maternal BSI Global scores (i.e., depression, anxiety, and somatization) is also presented in Table 3. The model fit well, RMSEA = .034, CFI = .942, SRMR = .041. As shown in Fig. 2, mother’s age, mother’s and abuser’s ACE score, and ethnicity had significant effects on the intercept, all p values < .05. Older mothers had higher initial BSI Global scores (i.e., depression, anxiety, and somatization). Mothers with higher ACE scores had higher initial BSI Global scores (i.e., depression, anxiety, and somatization). Hispanic mothers had lower initial BSI Global scores (i.e., depression, anxiety, and somatization). Self-efficacy and marginalization had significant effects on BSI Global scores (i.e., depression, anxiety, and somatization) at each time point, all p values < .01. The effects of self-efficacy were negative and became stronger at later time points. Mothers who had higher self-efficacy had lower BSI Global scores (i.e., depression, anxiety, and somatization). The effects of marginalization were positive. Mothers who were more marginalized had higher BSI Global scores (i.e., depression, anxiety, and somatization).
The model for CBCL internalizing scores fit well, (RMSEA = .039, CFI = .946, SRMR = .106) and is presented in Table 4. As shown in Fig. 3, service site (district attorney) or shelter), child’s gender, child’s age, mother’s ACE score, and child’s witnessing of mother’s physical abuse had significant effects on the intercept, all p values < .05. Children whose mothers went to District Attorney’s (DA) office for justice services had lower initial internalizing scores compared to those whose mothers sought assistance at a shelter. Boys had higher initial internalizing scores compared to girls. Older children had higher initial internalizing scores compared to younger children. Children whose mothers had higher ACE scores and children who had witnessed the physical abuse of their mothers had higher initial internalizing scores. Mother’s PTSD and BSI global scores (i.e., depression, anxiety, and somatization) had significant effects on internalizing scores at most of time points, all p values < .05. The effects of PTSD were positive and more crucial at early time points. Children whose mothers had higher PTSD scores had higher internalizing scores. The effects of BSI global scores (i.e., depression, anxiety, and somatization) were positive and significant at the first 12 time points. Children whose mothers had higher BSI global scores (i.e., depression, anxiety, and somatization) had higher internalizing scores.
The model for CBCL externalizing score fit well (RMSEA = .044, CFI = .935, SRMR = .088) (Table 4). Service site, child’s gender, mother’s ACE score, and immigrant status had significant effects on the intercept, all p values < .01 (Fig. 4). Children whose mother went to DA had lower initial externalizing scores, compared to those whose mother went to a shelter. Boys had higher initial externalizing scores compared to girls. Children whose mothers had higher ACE scores had higher initial externalizing scores. Children whose mothers were immigrants had lower initial externalizing scores compared to those whose mothers were born in the U.S. Ethnicity had significant effects on the linear component, p < .01. Hispanic children’s externalizing scores decreased faster than those of non-Hispanic children. Mother’s PTSD scores had significant effects on externalizing scores at seven time points, all p values < .05. Children whose mothers had higher PTSD scores had higher externalizing scores. Mother’s BSI global scores (i.e., depression, anxiety, and somatization) had positive significant effects on externalizing scores at ten time points, all p values < .05. Children whose mothers had higher BSI global scores (i.e., depression, anxiety, and somatization) had higher externalizing scores.
Discussion
This 4-year analysis provides longitudinal evidence that mother’s ACEs, coupled with intimate partner violence, predicts poor maternal mental health, specifically PTSD, depression, anxiety, and somatization. Maternal mental health is worsened by low self-efficacy and high marginalization and improved by high self-efficacy and low marginalization at each measurement point over the 4-years. Mother’s mental health was associated with children’s recovery from or persistence of internalizing and externalizing problems over the same 4-year period. Children whose mothers had higher PTSD, depression, anxiety, and somatization scores displayed more internalizing behaviors, such as depression and anxiety. Children who had seen the physical abuse of their mother had higher internalizing scores (i.e. depression and anxiety) at the start of study, as did boys, compared to girls, and older youth, compared to younger children. Similarly, children with mothers reporting higher PTSD, depression, anxiety, and somatization displayed more externalizing behaviors, such as hostile and aggressive actions. At the start of study, boys had higher externalizing scores and Hispanic children had lower externalizing scores.
Linking Determinants of Dyad Dysfunction to Informed Prevention
The role of ACE on poor adult health is well documented, beginning with the seminal work of Felitti and colleagues (Felitti et al. 1998). The magnified impact of ACE on the mental health, especially depression and PTSD, of women reporting IPV is documented in a recent systematic literature review (Montalvo-Liendo et al. 2015). The intersection of ACE and IPV compounds to impede positive parenting (Symes et al. 2015) and further intensifies the negative impact of poor maternal mental health on child dysfunction (Fredland et al. 2015). The current thinking is that interventions and policy that focus on reducing ACE for the current generation of children and adolescents will support better health outcomes as they age. Although ACE cannot be reversed, poor maternal mental health can be improved and thus impact their children in positive ways. The consistent and strong associations this study documents between worse maternal mental health and more child behavior problems over a four-year period (and conversely better maternal mental health and fewer child behavior problems) suggests that intergenerational transmission of poor outcomes can be interrupted, and reversed, if maternal self-efficacy and/or marginalization are improved.
Researchers have been struggling with the problem of where and when to intervene and with whom to best intervene to mitigate negative health outcomes for the children of abused women. Positive culturally relevant parenting, counseling/mentoring, financial support, job skills are among strategies discussed and implemented in various forms. Although the evidence for which strategies are likely to produce the most improvement on child health is unclear; it appears from these findings that improving maternal mental health will likely have positive benefits on the children in these families. Such improvements might be achieved by increasing mothers’ self-efficacy and decreasing marginalization.
Few intervention studies have addressed the mother-child dyad in families characterized by IPV. However, the current findings are consistent with the results of several studies targeting mental health outcomes for children exposed to IPV, in which reductions in mothers’ trauma symptoms and psychological distress contributed to improvements in child functioning (Graham-Bermann et al. 2007;Jouriles et al. 2009; Overbeek et al. 2015). These findings are consistent with the results of several longitudinal studies suggesting that maternal mental health symptoms mediate the association between children’s witnessing IPV and child functioning. Although a variety of mental health (Dutton et al. 2013; Johnson et al. 2011) and advocacy interventions (Bybee and Sullivan 2000) for abused women have demonstrated an improvement in maternal mental health and overall functioning, the impact of these interventions on children’s mental health was not measured. It seems plausible that in families in which there has been IPV, significant improvements in child functioning can be obtained by improving maternal mental health.
Realizing a New Reality for Maternal Child Functioning
The 2012 U. S. Preventive Services Task Force recommends health professionals screen women 14 to 46 years old for IPV and provide referral services offering support to abused women (U. S. Preventative Services Task Force 2012). A child health visit can provide a safe opportunity to screen mothers for abuse and discuss the possible negative effect on child behavior. The American Academy of Pediatrics (AAP) Committee on Child Abuse and Neglect identifies the importance of increasing awareness of partner violence to promote the health and wellbeing of children exposed to partner violence in the home (AAP 1998). In 2012 the AAP endorsed a recommendation that pediatricians recognize and screen for social determinants of health (American Academy of Pediatrics, Council on Community Pediatrics 2016). The AAP recognizes the life-long negative effects of “toxic stress” on children (Shonkoff et al. 2012) and in 2016 reaffirmed the policy statement recommending active assessment and community investment to reduce poverty and sources of toxic stress (AAP 2016). The AAP recommends a dual generational approach to address family and child mental health during routine health visits. This includes screening for maternal mental health issues and providing referral when indicated. The findings from this study support the AAP position, advocating for increasing resources that address maternal mental health and behavioral issues, particularly in poor communities (AAP 2016).
Conclusion
Our data demonstrate the close link between maternal childhood adversity, IPV, poor maternal mental health, and behavioral and mental health problems of children living with household violence. Our findings contribute to understanding the intergenerational transmission of adversity. We demonstrate the potential for interruption of the cyclical nature of adversity with interventions focused on improving maternal mental health, potentially by increasing maternal self-efficacy and decreasing marginalization.
References
Abramsky, T., Watts, C. H., Garcia-Moreno, C., Devries, K., Kiss, L., Ellsberg, M., et al. (2011). What factors are associated with recent intimate partner violence? Findings from the WHO multi-country study on women’s health and domestic violence. BMC Public Health, 11(109), 1–17. doi:10.1186/1471-2458-11-109.
Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA Preschool Forms & Profiles. Burlington: University of Vermont, Department of Psychiatry.
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA School-Age Forms & Profiles. Burlington: University of Vermont, Department of Psychiatry.
American Academy of Pediatrics, Committee on Child Abuse and Neglect. (1998). The role of the pediatrician in recognizing and intervening on behalf of abused women. Pediatrics, 101, 1091–1092.
American Academy of Pediatrics, Council on Community Pediatrics. (2016). Poverty and child health in the United States. Pediatrics, 137(4), e20160339. doi:10.1542/peds.2016-0339.
American Academy of Pediatrics, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics. (2016). Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics. doi:10.1542/peds.2011-2662.
Blair, F., McFarlane, J., Nava, A., Gilroy, H., & Maddoux, J. (2015). Child witness domestic abuse: Baseline data analysis for a 7-year study. Pediatric Nursing, 41(1), 23–29.
Binder, B., McFarlane, J., Maddoux, J., Nava, A., & Gilroy, H. (2013). Children in distress: Functioning of youngsters of abused women and implications for child maltreatment prevention. Journal of Child Care Practice, 19(3), 237–252. doi:10.1080/13575279.2013.785935.
Breiding, M. J., Smith, S. G., Basile, K. C., Walters, M. L., Chen, J., & Merrick, M. (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization--national intimate partner and sexual violence survey, United States, 2011. MMWR Surveillance Summary, 63(8), 1–18.
Bohnert, K. M., & Breslau, N. (2011). Assessing the performance of the short screening scale for post-traumatic stress disorder in a large nationally-representative survey. International Journal of Methods in Psychiatric Research, 20(1), e1–e5. doi:10.1002/mpr.331 Available in Wiley Online Library.
Breslau, N., Peterson, E. L., Kessler, R. C., & Schultz, L. R. (1999). Short screening scale for DSM-IV posttraumatic stress disorder. American Journal of Psychiatry, 156, 908–911.
Bybee, D. I., & Sullivan, C. M. (2000). The process through which a strengths-based intervention resulted in positive change for battered women over time. American Journal of Community Psychology, 30, 103–132.
Cannon, E. A., Bonomi, A. E., Anderson, M. L., Rivara, F. P., & Thompson, R. S. (2010). Adult health and relationship outcomes among women with abuse experiences during childhood. Violence and Victims, 25, 291–305.
Centers for Disease Control and Prevention (1997). Prevalence of individual adverse childhood experiences. Retrieved from http://www.cdc.gov/violenceprevention/acestudy/prevalence.html.
Centers for Disease Control and Prevention. (2010). Adverse childhood experiences reported by adults-five states, 2009. Morbidity and Mortality Weekly Report, 59(49), 1609–1613 Retrieved from www.cdc.gov/mmwr/preview/mmwrhtml/mm59.
Derogatis, L. R., & Lazarus, L. (2001). Brief symptom inventory-18. Administration, scoring and procedures manual. Minneapolis: NCS Pearson.
Dutton, M. A., Bermudez, D., Matas, A., Majid, H., & Myers, N. L. (2013). Mindfulness-based stress reduction for low-income, predominantly african american women with PTSD and a history of intimate partner violence. Cognitive and Behavioral Practice, 20(1), 23–32. doi:10.1016/j.cbpra.2011.08.003.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258.
Fredland, N., McFarlane, J., Gilroy, H., Nava, A., Paulson, R., & Pennings, J. (2015). Connecting partner violence to poor functioning for women and children: Modeling intergenerational outcomes. Journal of Family Violence., 30(5), 555–566. doi:10.1007/s10896-015-9702-1.
Fredland, N., McFarlane, J., Symes, L., Maddoux, J., Pennings, J., Paulson, R., et al. (2016). Modeling the intergenerational impact of partner abuse on maternal and child function at 24mos post outreach. Nursing Outlook, 64(2), 156–169. doi:10.1016/j.outlook.2015.10.005.
Graham-Bermann, S. A., Lynch, S., Banyard, V., DeVoe, E. R., & Halabu, H. (2007). Community-based intervention for children exposed to intimate partner violence: An efficacy trial. Journal of Consulting and Clinical Psychology, 75, 199–209.
Hamby, S., Finkelhor, D., Turner, H., & Ormrod, R. (2011). Children’s exposure to interpersonal violence and other family violence. U. S. Department of Justice, Juvenile Justice Bulletin. Retrieved from https://www.ncjrs.gov/pdffiles/ojjdp/232272.pdf.
Johnson, D. M., & Zlotnick, C. (2012). Remission of PTSD after victims of intimate violence leave a shelter. Journal of Traumatic Stress, 25, 203–206. doi:10.1002/jts.21673.
Johnson, D. M., Zlotnick, C., & Perez, S. (2011). Cognitive-behavioral treatment of PTSD in residents of battered women shelters: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 79(4), 542–551. doi:10.1037/a0023822.
Jouriles, E. N., McDonald, R., Rosenfield, D., Stephens, N., Corbitt-Shindler, D., & Miller, P. C. (2009). Reducing conduct problems among children exposed to intimate partner violence: A randomized clinical trial examining effects of project support. Journal of Consulting and Clinical Psychology, 77(4), 705–717. doi:10.1037/a0015994.
Kline, R. B. (2010). Principles and practice of structural equation modeling, 3 edn. New York: Guilford Press.
Koci, A., McFarlane, J., Nava, A., Gilroy, H., & Maddoux, J. (2012). Informing practice regarding marginalization: The application of the Koci marginality index. Issues in Mental Health Nursing, 33, 858–886. doi:10.3109/01612840.2012.713081.
McFarlane, J., Nava, A., Gilroy, H., Paulson, R., & Maddoux, J. (2012). Testing two global models to prevent violence against women and children: Methods and policy implications for a seven year prospective study. Issues in Mental Health Nursing, 33(12), 871–881. doi:10.3109/01612840.2012.731135.
McFarlane, J., Symes, L., Binder, B., Maddoux, J., & Paulson, R. (2014). Maternal-child dyads of functioning: The intergenerational impact of violence against women on children. Maternal Child Health Journal, 18(4), 2236–2243. doi:10.1007/s10995-014-1473-4.
McFarlane, J. (2007). Strategies for successful recruitment and retention of abused women for longitudinal studies. Issues in Mental Health Nursing, 28, 883–897.
Montalvo-Liendo, N., Fredland, N., McFarlane, J., Fuqin, L., Koci, A., & Nava, A. (2015). The intersection of partner violence and adverse childhood experiences: Implications for research and clinical practice. Issues in Mental Health Nursing, 36(12), 989–1006.
Muthén, L. K., & Muthén, B. O. (2012). Mplus user’s guide, 7 edn. Los Angeles: Muthén & Muthén.
Overbeek, M. M., deSchipper, J. C., Willemen, A. M., Lamers-Winkelman, F., & Schuengel, C. (2015). Mediators and treatment factors in intervention for children exposed to interparental violence. Journal of Clinical Child and Adolescent Psychology, 9, 1–17. doi:10.1080/15374416.2015.1012720.
Schwarzer, R., & Jerusalem, M. (1995). Generalized self-efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio (pp. 35–37). Windsor: NFER-Nelson.
Shonkoff, J. P., Siegel, B. S., & Dobbins, M. I. (2012). Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics, 129(1), e224–e231. doi:10.1542/peds.2011-2662.
Symes, L., Maddoux, J., McFarlane, J., & Pennings, J. (2015). A risk assessment tool to predict sustained PTSD symptoms among women reporting abuse. Journal of Women’s Health., 25(4), 340–347. doi:10.1089/jwh.2015.5287.
U. S. Preventative Services Task Force (2012). Screening women for interpersonal violence. Retrieved from http://www.uspreventiveservicestaskforce.org/.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McFarlane, J., Fredland, N.M., Symes, L. et al. The Intergenerational Impact of Intimate Partner Violence against Mothers on Child Functioning over four Years. J Fam Viol 32, 645–655 (2017). https://doi.org/10.1007/s10896-017-9913-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-017-9913-8