Abstract
Posttraumatic stress disorder (PTSD) is a debilitating condition that impacts anywhere from 2 to 39% of primary care patients. Research suggests overall health, instances of hospitalizations, emergency room visits, and utilization of primary care services are impacted by a diagnosis of PTSD. Evidenced based treatments such as cognitive process therapy and prolonged exposure (PE) are available in specialty mental health but pose many barriers to treatment and implementation into primary care. This case study serves as the first known case example with an ethnic minority civilian, examining the treatment of PTSD within the Primary Care Behavioral Health Model using the brief (5 visits), PE protocol for primary care (PE-PC). PTSD was assessed using the PCL-5. Additional variables were assessed and tracked with the following tools: PHQ-9 (depressive symptoms), GAD-7 (anxiety symptoms), QLES-SF (quality of life), and the AAQ-2 (psychological flexibility) pre/post treatment, 6 months post-treatment and 9 months post-treatment. The patient reported clinically significant decreases in symptoms of PTSD, depression, and anxiety symptoms. Additionally, the patient’s scores on quality of life and psychological flexibility improved. Brief, exposure-based treatment for PTSD can be delivered within the PCBH model. This treatment may result in improved quality of life and has the potential to reduce health care costs. This case encourages the treatment of PTSD within primary care, increasing access to care for patients. Future research is needed to further investigate this protocol in primary care with underserved, civilian populations and to explore patient attitudes toward brief treatment for PTSD in a primary care setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
PTSD Prevalence in Primary Care
As with the general population, assessing the prevalence of PTSD in the primary care setting is difficult to accurately capture. In a sample of 232 individuals across two primary care clinics 9% of primary care patients met criteria for full PTSD with 25% meeting for partial PTSD (Gillock, Zayfert, Hegel, & Ferguson, 2005). These findings are in line with Liebschutz et al. (2007) which found in an urban primary care clinic, patients were at a 34% risk for developing PTSD in their lifetime with 23% of patients currently meeting PTSD criteria. Greene, Neria, & Gross, 2016) provide support to prior research and places prevalence rates of PTSD in primary care between 2% to 39.1% depending on clinic patient population. In addition to this risk, these authors found that women were more likely to screen positive for PTSD compared to their male counterparts. This finding of women being at an increased risk for PTSD in the primary care setting was expanded by other studies to also include those women identified as non-white and of older age (Meredith et al., 2016; Westphal et al., 2011; Löwe et al., 2011).
This wide range of detection can be attributed to a myriad of reasons such as shame, lack of screening, misdiagnosis, or lack of information. When Liebschutz et al. (2007) reviewed patient records, they found that only 11% of patients had been accurately identified with PTSD. This lack of detection warrants a better approach to those potentially suffering from PTSD in primary care. Greene et al. (2016) suggest physicians should develop a different frame of mind that includes the physical and somatic difficulties patients experience with PTSD. Through this new framework, PCP’s may better identify PTSD as an interrelated issue between physical and mental health rather than one siloed as a mental health condition. This change in mentality may assist those seeking treatment for PTSD as Roberts, Gilman, Breslau, Breslau, and Koenen (2011) found that of ethnic minorities only 35% of African Americans, 42% of Hispanics, and 32% of Asians sought treatment for their PTSD symptoms compared to 53% of Caucasians.
The prevalence of PTSD in the primary care setting is also difficult to accurately measure as Liebschutz et al. (2007) notes due in part to the many measures’ researchers use to assess populations and the populations represented in study clinics. A common first stage screening tool for PTSD in primary care is the five-item Primary Care Screen for the DSM-5 (PC-PTSD-5; Prins et al., 2015). If the first stage screening tool is positive, a patient can then be assess using a second stage tool. Measures of PTSD include: PTSD Checklist for DSM-5 (PCL-5), Clinician-Administered PTDS Scale for DSM-5 (CAPS-5), PTSD Symptom Scale Interview (PSS-I-5), Structured Clinical Interview; PTSD Module (SCID-5), Impact of Events Scale-Revised (IES-R), Short PTSD Rating Interview (SPRINT; “PTSD Assessment Instruments,” 2018). It is important to note that within the primary care setting, the administration of a structured clinical interview is not always possible due to time constraints and staffing issues. In these situations, it is recommended that a validated self-report measure (e.g., PCL-5) be used on follow-up should additional assessment be required.
PTSD and the Impact on Health Status and the Health System
The impact of mental health and its relation to physical health is well documented and continues to develop as research advances on this subject (Doherty & Gaughran, 2014; McEwen, 2003). The association between mental health and physical health is well researched in the area of cardiac medicine examining the effects of depression and the risk of developing coronary artery disease (Serrano, Setani, Sakamoto, Andrei, & Fraguas, 2011). Given the above relationship, PTSD as another major mental health condition may play a larger role in the development of other physical health conditions such as diabetes, chronic pain, and hypertension than previously thought. Indeed, PTSD has been found to be a potential risk factor for the development of coronary heart disease (CHD), cardiac related mortality, metabolic diseases, chronic pain, irritable bowel syndrome, rheumatoid arthritis, and other somatic complaints (Andersen, Wade, Possemato, & Ouimette, 2010; Boscarino, Forsberg, & Goldberg, 2010; Edmondson, Kronish, Shaffer, Falzon, & Burg, 2013; Kubzansky, Koenen, Spiro, Vokonas, & Sparrow, 2007; Libby, 2006; Liebschutz et al., 2007).
The identification of PTSD as an antecedent to disease processes with biological alterations may help to explain patient change in medical utilization. Gillock et al. (2005) found that individuals with PTSD used medical services at higher rates compared to individuals not diagnosed with PTSD. A growing body of research is beginning to demonstrate a robust connection between PTSD and frequent emergency room (ER) visits and increased utilization of health care services (Cohen et al., 2010; Deykin et al., 2001; Fagan, Galea, Ahern, Bonner, & Vlahov, 2003; Kartha et al., 2008; Polusny et al., 2008; Raven et al., 2017; Vu et al., 2015).
This connection also extends to posttraumatic stress symptoms (PTSS), otherwise known as subthreshold PTSD. Over a three-month period, those with PTSD and PTSS utilized healthcare services (including ER visits) at a greater rate on average (3.37 vs. 2.54) compared to those who did not (Gillock et al., 2005). Those with PTSS and probable PTSD, on average had higher ER costs ($17 per person) and greater total adjusted health care costs (e.g., inpatient care, outpatient care, medications, physician fees; $838 per person) over the last 12 months (Lamoureux-Lamarche, Vasiliadis, Préville, & Berbiche, 2016).
What is Primary Care Behavioral Health and Why Treat PTSD in Primary Care
Primary Care Behavioral Health (PCBH) is a team-based approach consisting of the primary care team (i.e. primary care provider/PCP, medical assistant, nurses, etc.) and a behavioral health consultant (BHC) collaboratively working together to improve health for the entire clinic population. BHCs provide additional help to patients for improving chronic disease outcomes (e.g., diabetes, chronic pain), making lifestyle changes (e.g., quitting smoking, weight management, medication adherence) and addressing mental health care (e.g., anxiety, substance use disorders (Bridges et al., 2015). The focus of the approach is managing behavioral health problems and biopsychosocial influences impacting patient health conditions. This can be achieved through direct patient intervention by the BHC or “upskilling” the primary care team’s approach to biopsychosocial management of health conditions overall. The BHC works as a team member with the PCP where consultation is provided to the patient until the patient’s functioning or symptoms begin to improve. Upon the patient’s improvement (ending of an episode of care), the PCP assumes complete ownership of the patients care; however, the patient can re-engage with the BHC at any time for the original concern or a new one. At times patients who need a higher level of care will be referred to specialty mental health, but the BHC may continue to see the patient if this transition is not possible (Reiter, Dobmeyer, & Hunter, 2018). Core components necessary to effectively provide PCBH services are outlined in Robinson and Reiter (2016) through the “GATHER” acronym: Generalist, Accessibility, Team-Based, High Productivity, Educator, and Routine (Reiter et al., 2018).
Upon referral to the BHC by the PCP, patients typically receive a “warm hand off” in which the initial visit takes place. All BHC visits in this clinic take place in an exam room to be consistent with the primary care culture and to decrease stigmatization of behavioral health (i.e., rather than taking the patient to a different part of the clinic for the behavioral health visit). In consultation with the patient and PCP, follow-up visits are determined based on the patient’s need for care. After the episode of care is complete, patients continue to receive care from their PCP and health care providers as needed (e.g., clinical pharmacist, registered dietician). Ongoing communication between PCPs and BHCs regularly occurs at this clinic through both in-person interaction (e.g., “curbside” consult) and via the shared electronic medical record (EMR; Robinson & Reiter, 2016).
Effective evidence-based psychotherapies for PTSD are available in specialty mental health settings; however, many patients do not receive treatment due to barriers such as limited time, provider accessibility, long wait times, stigma, and hesitancy to discuss trauma and emotional concerns (Davis, Ressler, Schwartz, Stephens, & Bradley, 2008; Ede et al., 2015; Vogt, 2011). Furthermore, not all specialty mental health providers in the community have the experience or the training to provided evidence-based psychotherapy for PTSD (Finley et al., 2018; Rosen et al., 2017). Individuals that seek treatment in the community often do so after significant delays (Sayer et al., 2009; Trusz, Wagner, Russo, Love, & Zatzick, 2011), which can result in a prolonged period of reduced quality of life. As a result of specialties not located within primary care, PCP’s are often left hoping that their referral lead to treatment and frequently receive limited feedback or communication from any specialty service, including behavioral health (Zuchowski et al., 2015). Therefore, if PCP’s perceive there are no mental health resources, they are more inclined to treat PTSD symptoms in the primary care setting (Meredith et al., 2009). Considering these barriers to care and PCP’s likelihood to treat PTSD, it is important that PCP’s and BHC’s work together to address PTSD in the primary care setting. On site treatment increases the likelihood that patients will engage in treatment, enabling primary care to have a greater impact on patients who would not accept a referral to specialty mental health services (Engel, 2005; Ogbeide, Landoll, Nielsen, & Kanzler, 2018).
Assessment and Treatment of PTSD in Primary Care: The Prolonged Exposure Protocol for Primary Care (PE-PC)
Assessment
Traditionally, PTSD is assessed using a formal clinical interview and psychological assessment (e.g., Clinician-Administered PTSD Scale for DSM-5; PTSD Symptom Scale Interview for the DSM-5). Although this is the gold standard, time constraints in the primary care setting do not allow for this type of assessment process. Instead, in primary care, the use of a focused clinical interview as well as brief behavioral assessment, (e.g., PTSD Checklist for DSM-5; PCL-5; Blevins, Weathers, Davis, Witte, & Domino, 2015), is used to assess for symptoms of PTSD in adults (score range: 0 to 80). Because of the comorbidity with other psychiatric disorders, it is recommended that clinicians also screen for depression (e.g., PHQ-9; Kroenke, Spitzer, & Williams, 2001; score range: 0 to 27), anxiety (e.g., GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006; score range: 0 to 21), and substance misuse (e.g., AUDIT, Johnson, Lee, Vinson, & Seale, 2013, score range: 0 to 40; DAST, Yudko, Lozhkina, & Fouts, 2007, score range: 0 to 10) to aid in shared decision-making regarding treatment options. Using brief screening measures not only help with diagnostic clarification but can also be repeated to track psychiatric symptoms over time. Lastly, the clinician should consider the use of a brief measure that targets quality of life in order to assess impairment in functioning to help refine the diagnostic process and refine treatment goals (Haagsma et al., 2012).
Treatment
The recommended first line and evidenced-based psychological treatments for PTSD are Prolonged Exposure and Cognitive Processing Therapy (APA Guidelines, 2017). Prolonged Exposure (PE) was developed by Foa and colleagues (1999) and is defined as, “…repeated exposure to avoided situations and memories associated with a trauma” (Cigrang et al., 2017). Cognitive Processing Therapy (CPT) was developed by Resick and Schnike (1992) and focuses on the negative cognitions (e.g., thoughts of guilt and shame) impacting symptoms presentation and functioning associated with the trauma. In 2011, a Prolonged Exposure protocol for the primary care setting (PE-PC) was developed by Jeff Cigrang, PhD and Sheila Rauch, PhD. The PE-PC protocol has been utilized in active duty military populations as well as with veterans and treatment outcomes show promise in primary care. Specifically, research has demonstrated that almost half of patients who completed PE-PC no longer met criteria for PTSD an additionally, patients who received PE-PC treatment continued to show functional improvement 6 months after treatment had ended (Cigrang et al., 2011, 2017). Treatment exclusion criteria included: moderate to severe suicide risk, current alcohol dependence, psychotic disorder, significant dissociative disorder, and severe cognitive impairment (Cigrang et al., 2011). The content of the PE-PC protocol was consistent with emotional processing theory, drawn from the PE model (Cahill & Foa, 2007) and designed to fit within the context of four 30-min primary care visits within the PCBH model. The primary care protocol consists of imaginal exposure and in vivo exposure—similar to traditional PE. However, within the 30-min visit, imaginal exposure is written by the patient and then read aloud by the patient followed by emotional processing of the trauma memory. In vivo exposure is similar to traditional PE: creating an exposure hierarchy based on subjective units of distress (SUDs) ratings and setting behavioral goals to decrease avoidance by engagement in activities on exposure hierarchy. At the initial visit (visit 0 of the PE-PC protocol), behavioral health screening tools (e.g., PHQ-9, GAD-7, PCL-5) as well as a quality of life tool would be administered.
The BHC would conduct a contextual interview (Robinson & Reiter, 2016) or a functional assessment (Hunter, Goodie, Oordt, & Dobmeyer, 2017) of the presenting problem (i.e., PTSD). The patient would then be presented with psycho-education on PTSD and the various treatment options: PE-PC, referral to specialty mental health for trauma-focused treatment such as CPT or PE, brief symptoms management in primary care (e.g., focusing on symptoms of negative affectivity, symptoms of avoidance, or symptoms of hypervigilance, or self-help materials for PTSD). Once the patient selects a treatment option, follow-up would be provided depending on what is selected. Assuming the PE-PC protocol was selected, each visit in the protocol is typically scheduled every 2 weeks. At the end of the treatment episode, the patient and BHC can discuss next steps through shared decision making (e.g., ending the treatment episode, adding an additional PE-PC visit, referring to specialty mental health; Rotar, Van Den Berg, Schäfer, Kringos, & Klazinga, 2018).
Case Specific Considerations
The patient in this case is of ethnic minority decent as well as of low socioeconomic status (SES), it is important that the BHC attend to diversity-related variables that impact treatment. In this case, the focus was the use of “cultural humility” when interacting with the patient. Cultural humility is defined as being aware of how a patient’s culture can impact health behaviors and using this awareness when providing clinical services to patients (Miller, 2009). This approach was initially developed to address power inequities between patients and health care providers by encouraging an ongoing process of learning and self-reflection (Rajaram & Bockrath, 2014). This lens was used throughout the treatment process for the patient, giving options which is also consistent with a general patient-centered approach to care.
Identifying which PTSD treatment would be the most beneficial for patient is an important issue to consider. Simiola, Ellis, Thompson, Schnurr, and Cook (2019) examined variables that behavioral health providers consider when selecting an evidence-based PTSD intervention with a patient. Variables that were recommended to consider were: the type and nature of the traumatic event, the patient’s primary symptoms, the patient’s cognitive or personality type, the patient’s prior experience with PE or CPT, the patient’s treatment preference, the patient’s problem, and the patient’s overall goal for treatment. These considerations were taken into account when engaging the patient described in the current course of treatment.
Assessment and Treatment for Presented Case
Mrs. Paz was assessed and treated in a family medicine clinic, specifically within the PCBH consultation model. This primary care clinic also serves as a continuity clinic for a family medicine residency. The culture of the clinic in which Mrs. Paz was treated is largely integrated (i.e., level 5–6 integration). The BHC that performed the PE-PC protocol is a board-certified clinical health psychologist and was formally trained by the PE-PC protocol developers (Rauch & Cigrang Training Institute, LLC).
Mrs. Paz was referred to the BHC through a warm hand off by her PCP at a new patient visit to establish care. The PCP recognized possible symptoms of PTSD during the PCP visit which triggered the warm hand off. At the initial visit (visit 0), Mrs. Paz engaged with the BHC through the contextual interview (Bauman, Beachy, & Ogbeide, 2018; Robinson & Reiter, 2016) as well as patient education about factors that contribute to the development and maintenance of PTSD symptoms, with an emphasis on the role of avoidance. The following variables that impacted the BHC’s choice of engaging the patient in PE-PC included:
-
although patient had multiple traumas, the patient identified a specific memory that was particularly bothersome in which her nightmares were focused on;
-
the patient’s primary symptoms centered on avoidance;
-
after providing psychoeducation about all the treatment options, the patient preferred PE-PC; and
-
the patient’s goal for treatment was to interact more often with her children and attend social events with them outside of the home—something that she had avoided for many years.
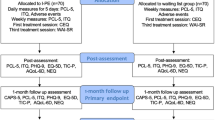
The patient completed the PCL-5, PHQ-9, GAD-7, AAQ-2 (Acceptance and Action Questionnaire-2; measures psychological flexibility; Bond et al., 2011), and the Quality of Life and Enjoyment Scale-Short Form (QLES-SF; Stevanovic, 2011) at the beginning of treatment and the end of treatment (visit 0 and visit 4; in the exam room at the start of the visit, privately and independently). The patient’s details from the contextual interview are described in Table 1.
Although the patient presents with other behaviors that could warrant intervention (e.g., stress eating, improving social network/decreasing social isolation), this BHC was working under the assumption these other behaviors were symptoms of PTSD therefore by treating PTSD, the other behaviors may resolve or the patient may be open to addressing the other behaviors once the PTSD symptoms are addressed.
At the second treatment visit (visit 1), BHC provided Mrs. Paz with the patient workbooks and reviewed the concepts of imaginal and in vivo exposure with the patient. She was provided a “Confronting Uncomfortable Memories” activity workbook to be completed at home and brought back for use in subsequent visits (Cigrang et al., 2011). The workbook asks the patient to write a first-person, detailed narrative of the traumatic event associated with the greatest level of current distress and preoccupation, including recollection of personal thoughts, feelings, and physical reactions (imaginal exposure). There are also emotional processing questions, such as, “How has this event changed what you think about yourself?” and, “How has this event changed how you think about others?” The patient is asked to record their level of distress before and after the writing exercise using a 0-100 SUDs with 0 = no distress and 100 = highest possible distress.
Mrs. Paz was then instructed to write and then read the trauma narrative and her answers to the emotional processing questions for at least 30 min three times per week. Although Mrs. Paz experienced years of trauma, she was able to select a particularly distressing event to use for the imaginal exposure exercise. The BHC also introduced in vivo exposure to the patient. The patient is asked to record their level of distress before and after the in vivo exposure using a 0-100 SUDs with 0 = no distress and 100 = highest possible distress. The patient will also track how often the in vivo exposure took place each week and how many minutes they were able to complete the exercise. Through SMART goal setting, the BHC engaged the patient in selecting the days of the week and time of day for the imaginal exposure exercise as well as the in vivo exposure exercise.
Visits 2 through 4 began with the BHC asking about the past 2 week’s experience of writing and reading the memory as well as the in vivo exposure. The BHC reviewed the pattern of SUDS ratings and discussed habituation with Mrs. Paz, praised her for having done whatever she could do, and problem-solved any issues that may have arisen. Mrs. Paz was then asked to write and read the narrative and her answers to the emotional processing questions out loud to the BHC. The remainder of each 30-min visit was devoted to trauma-associated emotional processing that includes review of exposures and her thoughts and emotions related to those exposures and how that impacts beliefs about herself and world at the time of the trauma and now. At the conclusion of visit two and three, the BHC prescribed continued weekly writing and reading of the memory at least three times per week (write a new version at the start of each week). Mrs. Paz also continued the in vivo exposure exercise weekly. At the conclusion of the last visit, the BHC engaged Mrs. Paz in conversation about her perception of treatment gains using the outcome scores and discussed whether a referral to the specialty mental health clinic was indicated. Mrs. Paz indicated that she did not need a referral to specialty mental health care, indicating that she had experienced functional and symptom improvement. During the treatment period, Mrs. Paz presented for each visit on time, every 2 weeks (10-week treatment period in total) and was adherent to the treatment protocol. She was able to complete imaginal and in vivo exposure exercises outside of the visit based on bi-weekly SMART goals that were set (e.g., imaginal exposure exercise was done three times a week for 30 min; in vivo exposure goals set each week such as going to a crowded grocery store or a busy park were completed as well). This may have been attributed to the BHC’s use of SMART goal setting during each visit as well as the use of Motivational Interviewing principles. No modifications to the treatment protocol were made by the BHC.
Outcome Assessment
Measures
The primary outcome assessment selected for Mrs. Paz was the PCL-5 (PTSD symptoms; Weathers et al., 2013). Mrs. Paz was also administered the PHQ-9, GAD-7, QLES-SF (quality of life), and the AAQ-2 pre/post treatment, 6 months post-treatment and nine- months post-treatment.
Outcomes
Mrs. Paz reported a clinically significant decrease in PTSD, depression, and anxiety symptoms. Overall, the PCL-5 score decreased from a 66 (significant impairment; 31 or above indicative of probable PTSD) to a 14 (minimal impairment) at the end of treatment. Her PCL-5 score 9 months post-treatment = 7. Mrs. Paz’s depression scores decreased from a 22 (severe) to a 13 (moderate), at 6 months was a 0, and 9 months, a 3. The patient’s anxiety scores decreased from a 20 (severe) to a 10 (moderate), at 6 months was a 1, and at 9 months = 5. Quality of life increased from a 29 to a 38 (scores range from 11 to 55 with higher scores = improved quality of life). At 6 months, quality of life was a 48. At 9 months = 44. Psychological flexibility was assessed post-treatment as well as six months post-treatment and decreased from a 29 to a 7 (scores range from 49 to 7 with lower scores = improved psychological flexibility). At 9 months, score = 9. Outcomes can be found in Fig. 1.
Qualitative Feedback
Mrs. Paz also provided qualitative feedback on her experience with the PE-PC protocol. She was provided with hard copy of the questions to provide her written response at the end of the treatment episode. Her responses are below:
What was the most helpful thing you learned about yourself going through the PTSD treatment protocol in primary care?
“Learning to accept my trauma and not allowing the trauma to have a hold on my life.”
If there was a patient who was nervous about starting this treatment protocol for PTSD, what advice would you give them?
“I would tell them that at first, it will be difficult. But once they are able to accept what happened to them, life does become much easier once we understand our emotions and our triggers.”
What do you want behavioral health providers or medical providers to know about introducing this treatment protocol to patients in primary care?
“To have patience, because each story is different.”
Summary and Conclusions
Mrs. Paz’s treatment is an example of how PTSD can be successfully treated within the confines of the PCBH model. The patient not only reported decreased PTSD symptoms, she also experienced improved mood and overall functioning despite experiencing PTSD symptoms the majority of her adult life, highlighting the effectiveness of the PE-PC protocol. Psychological flexibility is a variable not assessed in previous PE-PC research with military and veteran populations. Psychological flexibility is defined as “contacting the present moment fully as a conscious human being, and based on what the situation affords, changing or persisting in behavior in the service of chosen values” (“Working with ACT,” n.d.). For example, an individual building psychological flexibility in their life would seek to maintain awareness of their values (e.g., being a parent, building meaning friendships) and make daily decisions consistent with these values within changing external situations of which they have little control (e.g., stress in relationships, losing a job due to cutbacks, witnessing a traumatic event). Because of the connection between psychological flexibility and health status as well as the concept of avoidance (i.e., the more patients avoid, the more psychologically inflexible they present), it was important to begin to examine this variable with psychological treatments for PTSD that address avoidance (Robinson, Gould, & Strosahl, 2011). Mrs. Paz also provided qualitative feedback expressing satisfaction with this treatment in the primary care setting, encouraging other patients with debilitating symptoms of PTSD to be treated with this protocol (Ogbeide et al., 2018). To the knowledge of the authors, this is the first study to examine the PE-PC protocol in primary care with an ethnic minority civilian. Future research directions include a pilot project of this protocol in primary care with civilian, underserved populations.
The PE-PC protocol may then be evaluated for efficacy and compared with longer treatments in civilian, underserved populations. In addition to reduced health care costs by addressing PTSD in primary care, brief treatments may be increasingly acceptable to patients due to reduced time commitment. This case did not track subjective units of distress (SUDs); future studies could collect this information to improve the understandings of the mechanisms of change for this treatment protocol. Future research may also further explore patient attitudes toward brief treatment for PTSD in primary care settings. This case highlights the benefits of PCBH, which allows for increased access to behavioral health care within the context of primary care. In Mrs. Paz’s case, she was able to receive a warm hand off the same day as her PCP visit. Mrs. Paz’s past medical history included Obesity and Pre-Diabetes—conditions that were not being attended to (i.e., lack of engagement in medical care) related to PTSD symptoms (e.g., avoidance). Now that the PTSD symptoms have been treated, she is more engaged in medical care and ready to begin behavior change for her other health issues. This would be an important variable to examine with other patients with PTSD symptoms. It is also possible that Mrs. Paz was more likely to accept a BHC visit because it was embedded in primary care, as this increases treatment accessibility and often reduces stigma (Ogbeide et al., 2018). Thus, treating PTSD within this model may increase access to care for more patients experiencing this burdensome condition. In conclusion, the presented case provides an example of translating and adapting care within the PCBH model. Mrs. Paz’s notable decrease in PTSD symptoms suggests that such a treatment may be very effective in this setting. The case highlights the need for additional research on brief treatment of PTSD in civilian populations and encourages identification and treatment of PTSD in the primary care setting.
References
American Psychological Association. (APA; 2017). Clinical Practice Guideline for the Treatment of PTSD. https://www.apa.org/ptsd-guideline/ptsd.pdf
Andersen, J., Wade, M., Possemato, K., & Ouimette, P. (2010). Association between posttraumatic stress disorder and primary care provider-diagnosed disease among Iraq and Afghanistan veterans. Psychosomatic Medicine, 72, 498–504. https://doi.org/10.1097/PSY.0b013e3181d969a1.
Bauman, D. E., Beachy, B. R., & Ogbeide, S. A. (2018). Diabetes Management. In A. Maragakis & W. O’Donohue (Eds.), Principle-based stepped care and brief psychotherapy for integrated care settings. Cham, Switzerland: Springer.
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. https://doi.org/10.1002/jts.22059.
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., … Zettle, R. D. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire: II: A revised measure of psychological inflexibility and experiential avoidance. Behaviour Therapy, 42, 676–688. https://doi.org/10.1016/j.beth.2011.03.007.
Boscarino, J. A., Forsberg, C. W., & Goldberg, J. (2010). A twin study of the association between PTSD symptoms and rheumatoid arthritis. Psychosomatic Medicine, 72(5), 481–486. https://doi.org/10.1097/psy.0b013e3181d9a80c.
Bridges, A. J., Gregus, S. J., Rodriguez, J. H., Andrews, A. R., III, Villalobos, B. T., Pastrana, F. A., & Cavell, T. A. (2015). Diagnoses, intervention strategies, and rates of functional improvement in integrated behavioral health care patients. Journal of Consulting and Clinical Psychology, 83, 590.
Cahill, S. P., & Foa, E. B. (2007). Psychological theories of PTSD (pp. 55–77). Handbook of PTSD: Science and practice.
Cigrang, J. A., Rauch, S. A., Avila, L. L., Bryan, C. J., Goodie, J. L., Hryshko-Mullen, …, STRONG STAR Consortium. (2011). Treatment of active-duty military with PTSD in primary care: Early Findings. Psychological Services, 8(2), 104–113. https://doi.org/10.1037/a0022740.
Cigrang, J. A., Rauch, S. A., Mintz, J., Brundige, A. R., Mitchell, J. A., Najera, E., …, Goodie, J. L. (2017). Moving effective treatment for posttraumatic stress disorder to primary care: A randomized controlled trial with active duty military. Families, Systems, & Health, 35(4), 450–462. https://doi.org/10.1037/fsh0000315.
Cohen, B. E., Gima, K., Bertenthal, D., Kim, S., Marmar, C. R., & Seal, K. H. (2010). Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. Journal of General Internal Medicine, 25, 18–24. https://doi.org/10.1007/s11606-009-1117-3.
Davis, R. G., Ressler, K. J., Schwartz, A. C., Stephens, K. J., & Bradley, R. G. (2008). Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 21, 218–222. https://doi.org/10.1002/jts.20313.
Deykin, E. Y., Keane, T. M., Kaloupek, D., Fincke, G., Rothendler, J., Siegfried, M., & Creamer, K. (2001). Posttraumatic stress disorder and the use of health services. Psychosomatic Medicine, 63(5), 835–841. https://journals.lww.com/psychosomaticmedicine/Abstract/2001/09000/Posttraumatic_Stress_Disorder_and_the_Use_of.18.aspx
Doherty, A. M., & Gaughran, F. (2014). The interface of physical and mental health. Social Psychiatry and Psychiatric Epidemiology, 49, 673–682. https://doi.org/10.1007/s00127-014-0847-7.
Ede, V., Okafor, M., Kinuthia, R., Belay, Z., Tewolde, T., Alema-Mensah, E., & Satcher, D. (2015). An examination of perceptions in integrated care practice. Community Mental Health Journal, 51, 949–961. https://doi.org/10.1007/s10597-015-9837-9.
Edmondson, D., Kronish, I. M., Shaffer, J. A., Falzon, L., & Burg, M. M. (2013). Posttraumatic stress disorder and risk for coronary heart disease: A meta-analytic review. American Heart Journal, 166, 806–814. https://doi.org/10.1016/j.ahj.2013.07.031.
Engel, C. C. (2005). Improving primary care for military personnel and veterans with posttraumatic stress disorder: The road ahead. General Hospital Psychiatry, 27, 158–160. https://doi.org/10.1016/j.genhosppsych.2005.01.001.
Fagan, J., Galea, S., Ahern, J., Bonner, S., & Vlahov, D. (2003). Relationship of self-reported asthma severity and urgent health care utilization to psychological sequelae of the September 11 terrorist attacks on the world trade center among New York City area residents. Psychosomatic Medicine, 65, 993–996. https://doi.org/10.1097/01.PSY.0000097334.48556.5F.
Finley, E. P., Noël, P. H., Lee, S., Haro, E., Garcia, H., Rosen, C., …, Pugh, J. A. (2018). Psychotherapy practices for veterans with PTSD among community-based providers in Texas. Psychological Services, 15(4), 442–452. https://doi.org/10.1037/ser0000143.
Foa, E. B., Dancu, C. V., Hembree, E. A., Jaycox, L. H., Meadows, E. A., & Street, G. P. (1999). A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology, 67, 194–200. https://doi.org/10.1037/0022-006X.67.2.194.
Gillock, K. L., Zayfert, C., Hegel, M. T., & Ferguson, R. J. (2005). Posttraumatic stress disorder in primary care: prevalence and relationships with physical symptoms and medical utilization. General Hospital Psychiatry, 27, 392–399. https://doi.org/10.1016/j.genhosppsych.2005.06.004.
Greene, T., Neria, Y., & Gross, R. (2016). Prevalence, detection and correlates of PTSD in the primary care setting: A systematic review. Journal of Clinical Psychology in Medical Settings, 23(2), 160–180. https://doi.org/10.1007/s10880-016-9449-8.
Haagsma, J. A., Polinder, S., Olff, M., Toet, H., Bonsel, G. J., & van Beeck, E. F. (2012). Posttraumatic stress symptoms and health-related quality of life: A two year follow up study of injury treated at the emergency department. BMC Psychiatry, 12(1), 1–8.
Hunter, C., Goodie, J., Oordt, M., & Dobmeyer, D. (2017). Integrated behavioral health in primary care: Step-by-step guidance for assessment and intervention (2nd ed.). Washington, DC: American Psychological Association.
Johnson, J., Lee, A., Vinson, D., & Seale, P. (2013). Use of AUDIT-based measures to identify unhealthy alcohol use and alcohol dependence in primary care: A validation study. Alcoholism: Clinical and Experimental Research, 37, 253–259.
Kartha, A., Brower, V., Saitz, R., Samet, J. H., Keane, T. M., & Liebschutz, J. (2008). The impact of trauma exposure and post-traumatic stress disorder on healthcare utilization among primary care patients. Medical Care, 46, 388–393. https://doi.org/10.1097/MLR.0b013e31815dc5d2.
Kroenke, K., Spitzer, R., & Williams, J. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of Internal Medicine, 16, 606–613.
Kubzansky, L. D., Koenen, K. C., Spiro, A., Vokonas, P. S., & Sparrow, D. (2007). Prospective study of posttraumatic stress disorder symptoms and Coronary Heart Disease in the Normative Aging Study. Archives of General Psychiatry, 64, 109–116. https://doi.org/10.1001/archpsyc.64.1.109.
Lamoureux-Lamarche, C., Vasiliadis, H. M., Préville, M., & Berbiche, D. (2016). Healthcare use and costs associated with post-traumatic stress syndrome in a community sample of older adults: Results from the ESA-Services study. International Psychogeriatrics, 28, 903–911. https://doi.org/10.1017/S1041610215001775.
Libby, P. (2006). Inflammation and cardiovascular disease mechanisms. The American Journal of Clinical Nutrition, 83, 456S–460S. https://doi.org/10.1093/ajcn/83.2.456S.
Liebschutz, J., Saitz, R., Brower, V., Keane, T., Lloyd-Travaglini, C., Averbuch, T., & Samet, J. (2007). PTSD in urban primary care: High prevalence and low physician recognition. Journal of General Internal Medicine, 22, 719–726. https://doi.org/10.1007/s11606-007-0161-0.
Löwe, B., Kroenke, K., Spitzer, R., Williams, J., Mussell, M., Rose, M., …, Spitzer, C. (2011). Trauma exposure and posttraumatic stress disorder in primary care patients: Cross-sectional criterion standard study. The Journal of Clinical Psychiatry, 72(3), 304–312. https://doi.org/10.4088/JCP.09m05290blu.
McEwen, B. S. (2003). Mood disorders and allostatic load. Biological Psychiatry, 54, 200–207. https://doi.org/10.1016/S0006-3223(03)00177-X.
Meredith, L., Eisenman, D., Han, B., Green, B., Kaltman, S., Wong, E., …, Tobin, J. (2016). Impact of Collaborative Care for underserved patients with PTSD in primary care: A randomized controlled trial. Journal of General Internal Medicine, 31(5), 509–517. https://doi.org/10.1007/s11606-016-3588-3.
Meredith, L. S., Eisenman, D. P., Green, B. L., Basurto-Dávila, R., Cassells, A., & Tobin, J. (2009). System factors affect the recognition and management of post-traumatic stress disorder by primary care clinicians. Medical Care, 47(6), 686–694. https://doi.org/10.1097/mlr.0b013e318190db5d.
Miller, S. (2009). Cultural humility is the first step to becoming global care providers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 38, 92–93.
Ogbeide, S. A., Landoll, R. R., Nielsen, M. K., & Kanzler, K. E. (2018). To go or not go: Patient preference in seeking specialty mental health versus behavioral consultation within the primary care behavioral health consultation model. Families, Systems, & Health, 36, 513–517. https://doi.org/10.1037/fsh0000374.
Polusny, M. A., Ries, B. J., Schultz, J. R., Calhoun, P., Clemensen, L., & Johnsen, I. R. (2008). PTSD symptom clusters associated with physical health and health care utilization in rural primary care patients exposed to natural disaster. Journal of Traumatic Stress, 21, 75–82. https://doi.org/10.1002/jts.20281.
Prins, A., Bovin, M. J., Kimerling, R., Kaloupek, D. G., Marx, B. P., Pless Kaiser, A., & Schnurr, P. P. (2015). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5). [Measurement instrument].
PTSD Assessment Instruments. (2018, September 26). https://www.apa.org/ptsd-guideline/assessment/
Rajaram, S., & Bockrath, S. (2014). Cultural competence: New conceptual insights into its limits and potential for addressing health disparities. Journal of Health Disparities Research and Practice, 7, 82–89.
Raven, M. C., Tieu, L., Lee, C. T., Ponath, C., Guzman, D., & Kushel, M. (2017). Emergency department use in a cohort of older homeless adults: Results from the HOPE HOME study. Academic Emergency Medicine, 24, 63–74. https://doi.org/10.1111/acem.13070.
Reiter, J. T., Dobmeyer, A. C., & Hunter, C. L. (2018). The primary care behavioral health (PCBH) model: An overview and operational definition. Journal of Clinical Psychology in Medical Settings, 25, 109–126. https://doi.org/10.1007/s10880-017-9531-x.
Resick, P. A., & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60, 748–756. https://doi.org/10.1037/0022-006X.60.5.748.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in exposure to traumatic events, development of Posttraumatic Stress Disorder, and treatment-seeking for Posttraumatic Stress Disorder in the United States. Psychological Medicine, 41, 71–83. https://doi.org/10.1017/S0033291710000401.
Robinson, P., Gould, D., & Strosahl, K. (2011). Real behavior change in primary care: Improving patient outcomes and increasing job satisfaction. Oakland, CA: New Harbinger Publications.
Robinson, P. J., & Reiter, J. T. (2016). Behavioral consultation and primary care: A guide to integrating services (2nd ed.). Geneva, Switzerland: Springer.
Rosen, C. S., Eftekhari, A., Crowley, J. J., Smith, B. N., Kuhn, E., Trent, L., …, Ruzek, J. I. (2017). Maintenance and reach of exposure psychotherapy for posttraumatic stress disorder 18 months after training. Journal of Traumatic Stress, 30(1), 63–70. https://doi.org/10.1002/jts.22153.
Rotar, A. M., Van Den Berg, M. J., Schäfer, W., Kringos, D. S., & Klazinga, N. S. (2018). Shared decision making between patient and GP about referrals from primary care: Does gatekeeping make a difference. PLoS ONE, 13, 1–9. https://doi.org/10.1371/journal.pone.0198729.
Sayer, N. A., Friedemann-Sanchez, G., Spoont, M., Murdoch, M., Parker, L. E., Chiros, C., & Rosenheck, R. (2009). A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry Interpersonal and Biological Processes, 72(3), 238–255. https://doi.org/10.1521/psyc.2009.72.3.238.
Serrano, C. V., Jr., Setani, K. T., Sakamoto, E., Andrei, A. M., & Fraguas, R. (2011). Association between depression and development of coronary artery disease: Pathophysiologic and diagnostic implications. Vascular Health and Risk Management, 7, 159–164. https://doi.org/10.2147/VHRM.S10783.
Simiola, V., Ellis, A., Thompson, R., Schnurr, P., & Cook, J. (2019). Provider perspectives on choosing Prolonged Exposure or Cognitive Processing Therapy for PTSD: A national investigation of VA residential treatment providers. Practice Innovations, 4(3), 194–203. https://doi.org/10.1037/pri0000091.
Spitzer, R., Kroenke, K., Williams, J., & Löwe, B. (2006). A brief measure for assessing Generalized Anxiety Disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. https://doi.org/10.1001/archinte.166.10.1092.
Stevanovic, D. (2011). Quality of life enjoyment and satisfaction questionnaire: Short form for quality of life assessments in clinical practice: A psychometric study. Journal of Psychiatric and Mental Health Nursing, 18, 744–750. https://doi.org/10.1111/j.1365-2850.2011.01735.
Trusz, S. G., Wagner, A. W., Russo, J., Love, J., & Zatzick, D. F. (2011). Assessing barriers to care and readiness for cognitive behavioral therapy in early acute care PTSD interventions. Psychiatry Interpersonal & Biological Processes, 74(3), 207–223. https://doi.org/10.1521/psyc.2011.74.3.207.
Vogt, D. (2011). Mental health-related beliefs as a barrier to service use for military personnel and veterans: A review. Psychiatric services, 62(2), 135–142.
Vu, F., Daeppen, J. B., Hugli, O., Iglesias, K., Stucki, S., Paroz, S., …, Bodenmann, P. (2015). Screening of mental health and substance users in frequent users of a general Swiss emergency department. BMC Emergency Medicine, 15(1), 15–27. https://doi.org/10.1186/s12873-015-0053-2.
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5)—Standard [Measurement instrument]. https://www.ptsd.va.gov/
Westphal, M., Olfson, M., Gameroff, M., Wickramaratne, P., Pilowsky, D., Neugebauer, R., …, Neria, Y. (2011). Functional impairment in adults with past Posttraumatic Stress Disorder: Findings from primary care. Depression and Anxiety, 28(8), 686–695. https://doi.org/10.1002/da.20842.
“Working with ACT”. (n.d.). Using mindfulness and values in the workplace to improve performance and wellbeing. https://workingwithact.com/about/about-this-site/
Yudko, E., Lozhkina, O., & Fouts, A. (2007). A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of Substance Abuse Treatment, 32, 189–198.
Zuchowski, J. L., Rose, D. E., Hamilton, A. B., Stockdale, S. E., Meredith, L. S., Yano, E. M., …, Cordasco, K. M. (2015). Challenges in referral communication between VHA primary care and specialty care. Journal of General Internal Medicine, 30(3), 305–311. https://doi.org/10.1007/s11606-014-3146-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stacy Ogbeide, Alex Young, Brittany Houston, and Cory Knight declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ogbeide, S.A., Young, A., Houston, B. et al. Treating Post-traumatic Stress Disorder with a Prolonged Exposure Protocol Within Primary Care Behavioral Health: A Case Example. J Clin Psychol Med Settings 28, 575–583 (2021). https://doi.org/10.1007/s10880-020-09747-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-020-09747-z