Abstract
Pediatric feeding problems occur in 25–40% of all children and disproportionately affect children with health and/or developmental concerns. Children with autism spectrum disorder (ASD) are at particularly high risk for feeding difficulties, though the connection between ASD and feeding problems is not well understood. As issues related to problematic feeding behavior frequently present to outpatient pediatric clinics, there is a need to understand the common factors that contribute to the development of both adaptive and maladaptive feeding behaviors. The current study examined predictors of problematic feeding behavior in children with and without ASD. Parents of children with ASD reported significantly greater child disruptive behavior, parenting stress, child feeding difficulties, and problematic parental feelings and strategies regarding feeding. Child disruptive behavior and parenting stress contributed the most variance in the prediction of child feeding difficulties and the relation between child disruptive behavior and feeding difficulties was partially mediated by parental strategies and feelings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is, perhaps, nothing more important for developing infants and children than feeding. Infants and very young children are dependent on caregivers for obtaining food, which is necessary to sustain life. As opposed to “eating,” the term “feeding” usually refers to the interaction between the caregiver and child that is necessary for young children to eat. In most cases, the process of feeding develops naturally. In a substantial minority of the population, however, issues with feeding arise at some point in early childhood. Up to 50% of toddlers and young children exhibit some pediatric feeding difficulties, which are heterogeneous in their presentation and etiology (Burklow, Phelps, Schultz, McConnell, & Rudolph, 1998; Crist & Napier-Phillips, 2001; Manikam & Perman, 2000). Common feeding issues include food refusal, extreme food selectivity or “pickiness,” food avoidance behaviors (e.g., crying, whining, pushing food away), and lack of self-feeding (Kerwin, 1999).
Food refusal may result in inadequate intake and poor growth sometimes referred to as “failure to thrive.” In children with normal growth, disruptive mealtime behavior and food selectivity (i.e., restriction of the range of foods in one’s diet) are the most commonly reported feeding problems (de Moor, Didden, & Korzilius, 2007; Lewinsohn et al., 2005). Children with food selectivity may fail to eat from entire food groups, refuse all novel foods, and exhibit extreme selectivity based on tastes, feel, brand, temperature, and presentation (Bachmeyer et al., 2009; Shore, Babbitt, Williams, Coe, & Snyder, 1998). Even when nutritional intake is adequate, situational feeding challenges can arise when children with severe food selectivity need to eat away from home or access to preferred foods is otherwise restricted (Rogers, Magill-Evans, & Rempel, 2012). Parent–child attachment and family functioning may also be negatively affected by food selectivity problems (Greer, Gulotta, Masler, & Laud, 2008; Satter, 1990). While many feeding problems will resolve without intervention or with low-intensity treatment, severe and chronic feeding problems persist in approximately 3–10% of children (Burklow et al., 1998). Considering the potential consequences, it is important to determine the factors that contribute to feeding problems in some children and healthy feeding behaviors in others. Problematic feeding behaviors appear to develop through a range of etiological pathways within a complex relation of biological, social, and psychological factors (Burklow et al., 1998; Field, Garland, & Williams, 2003; Kerwin, 1999).
Relationships Between Child Factors and Feeding Problems
Several physiological conditions are known to predispose children to feeding difficulties (Rommel et al., 2003). Patients with chronic gastrointestinal issues (Mackner et al., 2001), pulmonary issues (Jones, Morgan, & Shelton, 2002), and/or prematurity (Delaney & Arvedson, 2008) represent a large portion of children treated for feeding disorders. Most often, feeding problems in children with chronic medical issues be traced to factors such as painful eating, craniofacial and dental issues, or side effects of medications (Babbitt et al., 1994). Even in the absence of chronic conditions, children suffering from acute choking episodes or illnesses that result in vomiting or diarrhea are at risk for developing negative associations with feeding (Chatoor et al., 2001).
Children with developmental disorders are also at a high risk for developing feeding problems due to causes that are not well understood (Manikan & Perman, 2000). Children with autism spectrum disorder (ASD) are particularly prone to issues related to food selectivity (Schreck, Williams, & Smith, 2004). For children with ASD, problems with the mechanics of chewing and swallowing tend to be secondary to primary concerns related to food refusal and disruptive mealtime behaviors (Rogers et al., 2012; Sharp et al., 2013). Children with ASD have been found to be more likely to require specific utensils and specific presentations to accept foods, and more likely to only accept foods of certain texture than control children (Schreck et al., 2004). The relation between ASD symptoms and feeding problems is likely complex and indirect; Martins, Young, and Robson (2008) matched children with ASD to children without ASD and siblings of children with ASD based on their levels of adaptive functioning and found only marginal differences in the level of child problematic feeding for children with ASD.
Given that ASD and medical issues do not fully explain the prevalence of problematic feeding behaviors, researchers have begun to investigate additional child behavioral factors associated with problematic feeding. Johnson et al. (2014) theorized that children’s various behavioral responses at mealtimes may be due to their temperamental characteristics and individual behavioral repertoires. Indeed, previous studies have found that feeding problems are more prevalent in children who are difficult, demanding, or unsociable (Hagekull, Bohlin, & Rydell, 1997) and children who have additional disruptive behaviors (Sharp et al., 2013). This relation may be causal; Blissett and Farrow (2007) found that difficult behavioral temperament at 6 months of age is associated with infants’ food refusal and negative mealtime behavior at 1 year. A follow-up study (Haycraft, Farrow, Meyer, Powell, & Blissett, 2011) found that school-age children, who were more characteristically emotionally reactive expressed lower enjoyment of food, ate more slowly, and were “fussier” during feeding. Studies including large samples of preschool and school-age children with ASD (Allen et al., 2015; Johnson et al., 2014) have also found strong positive relationships between levels of externalizing behavior problems and feeding problems.
Relationships Between Parent Factors and Feeding Problems
In addition to child characteristics, certain parent characteristics and behaviors put children at higher risk for developing behavioral feeding problems. Parents of children with a variety of organic and non-organic feeding issues have been found to have higher emotional stress, and higher stress may be intensified by additional health concerns and developmental problems (Gueron-Sela, Atzaba-Poria, Meiri, & Yerushalmi, 2011). In particular, parents of children with ASD are known to report high levels of general stress, parenting stress, and relational strain, even when compared to parents of children with other health problems and/or special needs (Schieve, Blumberg, Rice, Visser, & Boyle, 2007).
Interestingly, when parents perceive their child to be underweight, they are more likely to use coercive feeding tactics (Galloway, Fiorito, Francis, & Birch, 2006). Unfortunately, parent concern can lead to tense mealtime interactions that may have the counterproductive effect of intensifying children’s food aversion and refusal behaviors. Rigal, Chabanet, Issanchou, and Monnery-Patris (2012) found that children’s feeding problems were associated with both permissive feeding styles (e.g., indulging the children’s desires by preparing only what the child likes) and authoritarian styles (e.g., using coercive tactics, bargaining, or physical force).
For children with ASD, maladaptive feeding practices are mediated by parents’ anxiety about their child’s health and well-being (Gueron-Sela et al., 2011). The interaction between parenting stress and feeding problems also appears to be child-specific. Nadon et al. (2011) found that parents who had one child with ASD and one typically developing child were more stressed during meals with their child with ASD than during meals with their sibling. Thus, the development of parents’ maladaptive feeding strategies appears to be related to their individual responses to their child’s particular vulnerability and behavior rather than a direct function of parent traits and eating habits.
The association of child factors with parent strategies was also well illustrated in a study in which Canadian parents with both typically developing children and children with ASD were surveyed on their mealtime parenting practices (Nadon, Feldman, Dunn, & Gisel, 2011). Parents reported that they were more likely to give their child with ASD a different meal when they complained than their typically developing siblings. They also reported that they were more likely to allow distractions, provide only food the child liked, and use visual aids during meals for their child with ASD.
Current Aims
The current study extends previous work in further examining relationships between biopsychosocial factors and children’s feeding. This study specifically aimed to examine the roles of parent feeding strategies and child disruptive behavior as proximal predictors of problematic feeding behavior. Given that disruptive behaviors and self-regulatory problems are more prevalent in children with ASD (Lecavalier, Leone, & Wiltz, 2006), we intended to evaluate the extent to which feeding problems in children with ASD can be accounted for by broader deficits in behavioral regulation.
Rather than examining separate pathways to development of feeding for children with or without ASD, the current study aimed to unify previous studies findings in examining common predictors of problematic feeding across ASD diagnostic status. Additionally, this study aimed to extend and unify previous findings within pediatric subgroups to a diverse sample of healthcare-seeking families.
Method
Participants
Participants in the current study included 156 children (96 males, 61 females) and their accompanying parent/guardian. In order to be included in the study, children were required to be between the ages of 2–8 years (inclusive), and parents were required to be English speakers/readers. In families with more than one qualified parent and/or child, only one parent and one child (selected by family per their preference) were included in the study. Medical information regarding children’s current medical and developmental diagnostic information was collected from retrospective reviews of children’s medical charts. Diagnosis of ASD was determined by the presence of a formal report by a physician, psychologist, or other qualified professional. All ASD evaluations included standardized results from either the Autism Diagnostic Interview, Revised (ADI-R; Lord, Rutter, & Le Couteur, 1994) or the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2; Rutter, DiLavore, Risi, Gotham, & Bishop, 2012).
According to information obtained from medical chart reviews, participant children were assigned to exclusive categories by primary developmental diagnostic status; 66 children were diagnosed with ASD and 90 were determined to be typically developing, with no documented developmental concerns. Children with known developmental issues other than ASD were excluded from the study.
Mothers were the primary participating caregivers (89.2% of total sample), and 49% were married. Caregivers’ highest level of education ranged from less than high school (3% of the sample) to completion of graduate school (9%). The modal household income for the sample was less than $20,000, with 29% of the total sample reporting $5000–$19,999 annually and 11% reporting less than $5000 annual income. On average, participants reported a 1:1 ratio of adults to children living in the household. See Table 1 for additional demographic information.
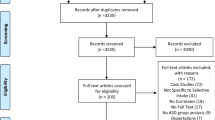
Procedure
Participants were recruited from pediatric primary care and sub-specialty clinic waiting rooms at a university-affiliated children’s hospital. Ninety-two percent (92%) of all parents approached agreed to participate and completed all study measures. Medical information regarding children’s current medical and developmental diagnostic information was collected from retrospective reviews of children’s medical charts. Diagnosis of ASD was determined by the presence of a formal report by a physician, psychologist, or other qualified professional utilizing standardized results from either the ADI-R (Lord et al., 1994) or the ADOS-2 (Rutter et al., 2012). Children who had not been suspected of or evaluated for ASD according to their chart and parent report were assigned to the “Non-ASD” group.
Measures
Eyberg Child Behavior Inventory (ECBI; Eyberg & Pincus, 1999; Eyberg, Boggs, & Reynolds, 1980). The ECBI is a 36-item parent-report measure of children’s general disruptive behavior and is appropriate for use with children between the ages of 2 to 16 years. The ECBI contains both an Intensity and a Problem Scale. For the current study, only the ECBI Intensity scale was used, which assesses the frequency a child displays each of 36 problematic behaviors. Scores on the Intensity scale range from 36 to 252, and an Intensity score greater than 131 indicates the presence of clinical levels of problem behavior (Eyberg & Pincus, 1999). The ECBI has been shown to have good psychometric properties, including adequate to strong internal consistency, test–retest reliability, convergent validity, and treatment sensitivity in populations of typical children and children with conduct problems, ASD, intellectual disabilities, and learning disabilities (Bagner & Eyberg, 2007; Cone & Casper-Beliveau, 1997; Eyberg & Pincus, 1999; Funderburk, Eyberg, Rich, & Behar, 2003; Jeter, Zlomke, Shawler, & Sullivan, 2017; Robinson, Eyberg, & Ross, 1980; Webster-Stratton & Hammond, 1997). The ECBI has strong documented psychometric properties and has demonstrated convergent validity with parent-rated measures of child behavior and direct observations of child behavior (Boggs, Eyberg, & Reynolds, 1990; Funderburk et al., 2003). In the current sample, the Intensity scale demonstrated excellent reliability with Cronbach’s Alpha of .957 (total sample).
Parenting Stress Index-Short Form (PSI-SF; Haskett, Ahern, Ward, & Allaire, 2006). The PSI-SF is a self-report measure of stress in the parent–child relationship which yields a total stress score and three subscales: (1) parental distress, (2) parent–child dysfunctional interaction, and (3) difficult child. Total stress raw scores of 86 and higher are determined to be clinically significant. The PSI-SF has been used extensively as a measure of parent stress for parents of children with ASD (Weitlauf, Vehorn, Taylor, & Warren, 2014). The PSI-SF has demonstrated good psychometric properties with parents of typical children, low income/minority children, children with conduct problems, and children with intellectual disability and ASD (Bagner & Eyberg, 2007; Davis & Carter, 2008; Reitman, Currier, & Stickle, 2002; Zaidman-Zait et al., 2010). For the total sample of the current study, the PSI subscales demonstrated strong internal consistency (Parental Distress alpha = .887, parent–child dysfunctional interaction alpha = .901; Difficult Child alpha = .920).
Behavioral Pediatrics Feeding Assessment Scale (BPFAS; Crist & Napier-Phillips, 2001; Crist et al., 1994). The BPFAS is a 36-item measure of children’s problematic feeding behavior and feeding strategies and reactions of their parents. The first 25 items assess child behavior related to feeding (e.g., has problems chewing food, spits out food) and the last 10 items assess parent feeling about and strategies addressing feeding and mealtime problems (e.g., I feel confident my child gets enough to eat). Parents rate each item to indicate how often a specific behavior or feeling occurs using a 5-point Likert scale, ranging from 1 (never happens) to 5 (always happens). The BPFAS yields three scores indicative of mealtime behavior problems: child behavior total frequency (BPFAS-Child), parent’s feelings/strategies frequency (BPFAS-Parent), and total frequency (BPFAS-Total). Research by Dovey, Jordan, Aldridge, & Martin (2013) suggests that BPFAS-Total scores above 81, BPFAS-Child scores above 61, and BPFAS-Parent scores above 20 indicate clinical feeding difficulties. In the current sample, the BPFAS demonstrated strong internal consistency, BPFAS-Total α = .916, BPFAS-Child α = .885, BPFAS-Parent α = .800.
Results
Missing Data Analyses
Prior to conducting analyses for hypothesis testing, study data were reviewed to ensure appropriateness for the proposed analyses. Data were analyzed using SPSS 25. Initial inspection of the data revealed no missing data for ASD diagnostic status. Individual missing item values on measures were imputed according to procedures suggested by each measure’s respective authors and publishers. Cases missing one composite score were found to be more likely to be missing other composite scores, and therefore cases were retained in the dataset, but deleted listwise from individual analyses.
Comparison of ASD and Non-ASD Samples
Composite scores for all parent-report measures (ECBI Frequency, BPFAS-Child Frequency, BPFAS-Parent Frequency, PSI-SF Total) were examined using a multivariate analysis of covariance (MANCOVA) using group (ASD or non-ASD) as the independent variable. Because samples were not matched by demographic characteristics, between-groups differences were examined and accounted for. There was not a significant difference in the average age across the ASD and non-ASD groups (t(150) = 1.126, p = .265). However, Chi-square analyses indicated differences in ethnicity (x2 = 38.76, p = .000) and child gender (x2 = 4.86, p = .032). Specifically, children diagnosed with ASD were more predominantly male and more heavily African American than the group of children without ASD. As such, ethnicity and child gender were entered as covariates in group analyses.
A significant multivariate main effect for ASD diagnostic status was found, Wilks’ Lambda F (4, 134) = 8.00, p < .001, η 2p = .19. A Bonferroni adjustment was utilized on all post hoc ANCOVAs. Significant univariate main effects for ASD diagnostic status were obtained for ECBI, Intensity, PSI-SF, BPFAS-Child, and BPFAS-Parent. See Table 2 for univariate statistics. Results revealed that, as predicted, mean ECBI Intensity scores, PSI-SF scores, BPFAS-Child scores, and BPFAS-Parent scores were significantly higher for the ASD group than for the non-ASD group (p < .01).
Examination of correlations between ECBI Intensity, PSI-SF, BPFAS-Child, and BPFAS-Parent scores were examined for each group separately. For children with ASD, positive and significant correlations were revealed across all analyses. As expected, as ECBI Intensity scores increased, PSI-SF scores increased. Scores for BPFAS-Child were also positively associated with both ECBI Intensity scores and PSI-SF scores, as well as BPFAS-Parent scores. A similar pattern of relations was found for children without ASD with the exception of BPFAS-Parent scores and PSI-SF scores, which were not significantly related in the non-ASD sample. See Table 3 for a summary of the intercorrelations by diagnostic group.
Prediction of Child Problematic Feeding Behavior
To examine the prediction of child problematic feeding, a hierarchical multiple linear regression was conducted (Table 4). As general child disruptive behavior and parent problematic feeding strategies were hypothesized to be more proximal risk factors in the prediction of problematic feeding behavior compared to more distal general parenting stress, child gender, and child ethnicity, ECBI Intensity and BPFAS-Parent scores were entered first into the regression, followed by ASD diagnostic status, PSI-SF scores, child ethnicity, and child gender.
The hierarchical multiple regression revealed that at step one ECBI Intensity scores and BPFAS-Parent scores contributed significantly to the regression model, F (2, 138) = 107.418, p < .001. These variables accounted for 61% of the variance in BPFAS-Child scores. Introducing PSI-SF scores, ASD diagnosis, child ethnicity, and child gender explained an additional 2% variance in childhood feeding issues, which was not a significant change. Neither PSI-SF, ASD diagnosis, or child ethnicity were significant predictors of child feeding concerns. This would suggest that ECBI Intensity scores and BPFAS-Parent scores explain the most variance in BPFAS-Child scores.
Mediation by Parent Feeding Feelings and Strategies
To follow up on previous results, the present study examined the role of parental feeding feelings and strategies as a mediator in the relation between child general disruptive behavior and problematic feeding behavior. A bootstrapping sampling procedure recommended by Preacher and Hayes (2008) was performed using ECBI Intensity as a predictor of BPFAS-Child, with BPFAS-Parent as the mediating variable. ASD diagnostic status was entered in as a covariate due to previous findings of significant differences across measures by ASD status. The SPSS Macro for Multiple Mediation (MATRIX procedure) was applied to conduct this analysis (Preacher & Hayes, 2008). Indirect bootstrapping procedures were utilized with a 5000 bootstrapped sample and a 95% confidence interval.
Results indicated that, even after controlling for ASD diagnosis, ECBI Frequency was a significant predictor of BPFAS-Parent, b = 0.05, SE= .013, p < .001, and child BPFAS-Child, b = .20, SE = .03, p < .001. This indicates that as child disruptive behavior increased, problematic parental feeding feelings and strategies and child feeding problems increased. When controlling for ASD status, BPFAS-Parent was a significant predictor of BPFAS-Child, b = 1.61, SE = .15, p < .001. This would suggest that as problematic parental feeding feelings and strategies increased, child feeding concerns also increased. After controlling for diagnosis and BPFAS-Parent, the strength of the relationship between ECBI Intensity and BPFAS-Child decreased, b = .12, SE = .02, p < .001. See Fig. 1 for an illustration of relationships within the model.
Discussion
The current study aimed to describe, compare, and examine prediction of feeding problems in pediatric patients with and without ASD. The study measured and compared problematic child feeding behavior, child disruptive behavior, parenting stress, problematic parent feeding approaches, and child problematic feeding behavior between groups. As possible targets for prevention and treatment, relative contributions of parenting stress, child disruptive behavior, and problematic parent feeding to children’s levels of problematic feeding behavior were also examined and compared between groups.
This study confirmed and extended previous studies’ findings of higher parent-reported child disruptive behavior, parenting stress, child feeding problems, and parenting maladaptive parent feeding strategies in children with ASD. Building on the work of previous researchers (Allen et al., 2015; Blissett, Meyer & Haycraft, 2011; Hagekull et al., 1997; Johnson et al., 2014), this study illustrated a robust predictive effect of children’s level of disruptive behavior on their level of problematic feeding behavior. Although previous studies’ findings have identified this association within diagnostic subgroups, the current study was the first to generalize the finding across a sample of ethnically and socioeconomically diverse families seeking pediatric healthcare services.
The study also sought to explain additional factors contributing to children’s problematic feeding behavior. The biopsychosocial model of normative and problematic pediatric feeding (Berlin, Davies, Lobato, & Silverman, 2009) posits that children’s vulnerability factors lead to feeding problems, which contribute to parents’ parenting stress and the use of maladaptive feeding strategies, which, in turn, further contribute to children’s feeding problems. A hierarchical model including ASD diagnostic status, disruptive behavior, parent problematic feeding, and parenting stress explained a sizeable variability in child problematic feeding. As expected, most of the variance was accounted for by general disruptive child behavior and parent feeding strategies. Parent problematic feeding behavior was found to be a greater contributor than child disruptive behavior. More distal factors in the model, ASD diagnostic status, ethnicity, and parenting stress accounted for a small portion of the remaining variance and did not significantly predict child problematic feeding behavior.
As issues related to feeding are increasingly presenting in outpatient health care settings (Allen et al., 2015; Sharp, Jaquess, Morton, & Herzinger, 2010), the study findings add to the knowledge of common factors that contribute to the development of both adaptive and maladaptive feeding behaviors. The current study adds to the growing body of research investigating the relationship between general disruptive behavior and children’s problematic feeding behavior. This is an area which was largely neglected within the early feeding literature, as feeding disorders have previously been examined within the context of physiological conditions and internalizing symptomology. As recommended in many previous studies, this study examined parent feeding factors in addition to child factors. With increased knowledge of the relationships among multiple elements that contribute to feeding behaviors, treatments can become more targeted to intervene preventatively in the primary areas of influence.
Although this study confirmed that children with ASD are at a particularly high risk for disordered feeding, the findings also lend credit to the theory that common issues and mechanisms influencing feeding are shared across children with ASD, other at-risk populations, and typically developing children (Martins et al., 2008). The absence of ASD from the predictive model in this study suggests that the connection between feeding problems and ASD is not a direct consequence of core ASD symptomology.
Taken together, study findings have implications for prevention, screening, and intervention efforts. Within the overall model, results indicated a significant, large effect of ASD diagnostic status on child and parent functioning. Consistent with previous findings, these results support diagnosis of ASD as a specific risk factor for behavioral dysregulation, feeding issues, and parent–child relationship problems. Thus, in order to maintain function and well-being families of children diagnosed with ASD require additional health accommodations, behavioral services, and family supports.
The proximal factors in the prediction of feeding problems are promising targets for prevention and intervention efforts, as both child disruptive behavior and parent strategies/approaches have shown to be responsive to therapy. For example, the current findings suggest that such prevention and intervention efforts can be applied broadly, and possibly more efficiently, across developmental diagnostic statuses, and that parents should be involved as essential targets in feeding interventions for children with and without ASD. In consideration of the influence of parent feelings and approaches on the feeding interaction, parents of children with feeding disorders may also benefit from individualized interventions to target anxiety and distress tolerance.
Additionally, if child disruptive behavior and maladaptive parent feeding approaches can be identified early, providers can disseminate parent training and education that may prevent children from developing feeding disorders. Efforts specifically targeted towards preventing problematic feeding behavior in children with ASD should consider focusing on skills-based interventions known to promote appropriate general child behavior. In particular, anticipatory parent management training may prove helpful in preventing behavior problems and feeding problems in children with ASD.
In contrast to ASD diagnostic status, parent feeding behavior and child disruptive behavior are known to be responsive to behavioral intervention. Study findings highlight the importance of addressing parental perceptions, feelings, and strategies regarding feeding in prevention of children’s feeding problems. Findings indicate that the presence of disruptive behaviors may negatively impact parental strategies and feelings at mealtimes. This in turn may increase a children’s risk for feeding difficulties. From a clinical standpoint, the presence of a mediating effect indicates that interventions which effectively teach parents effective tools for managing and responding to disruptive child behavior could indirectly lead to improved feeding behavior. This is a beneficial finding from a public health standpoint, as interventions targeting broader issues such as general disruptive behavior are likely more cost effective than applying multiple interventions to specific behaviors.
While the cross-sectional nature of the current study precludes inferences of cause and effect, the strength of the results strongly suggests that child general disruptive behavior represents a key area for the prevention of feeding problems in diverse pediatric clinic settings. Future longitudinal studies should look more precisely at parent and child behavioral predictors of problematic feeding. Notably, given that parent and child behaviors were parent-reported in the current study, it will also likely be important to intervene on the level of parent perceptions of child behavior. Additionally, it would be beneficial for future studies to determine whether this effect can be replicated using observational measures of child and parent behavior.
Limitations
This study is unique in that it compared relations between disruptive behavior and feeding behavior in children with ASD to a clinic sample of comparison children with a higher prevalence of known feeding risk factors (e.g., developmental delay, preterm/low birthweight, chronic medical issues) than samples obtained outside of the pediatric clinic setting. The study sample was also ethnically and socioeconomically diverse, and consisted of both underweight and overweight children. Unfortunately, however, in the current sample, ASD status was confounded by differences in ethnicity, sex, and parent age. To allow comparative conclusions to be based solely on diagnostic status, future studies should recruit comparison children matched on ethnicity, sex, and parent age.
This study contributes to the literature through applying a common measure of feeding problems (i.e., the BPFAS) across children with and without ASD, which is important for allowing conclusions to be drawn regarding between-groups comparisons. However, caution should be taken in applying results of the current study beyond pediatric clinic populations, as the findings may not generalize to a population-based sample or to a clinician sample of patients presenting for treatment of feeding disorders. Future studies should also consider including other specific measures to get a fuller picture of how parent and child factors interact to influence feeding behavior. For example, parent measures of personality factors, parent eating habits, and general parenting style could facilitate understanding of the individual parent factors involved in parent problematic feeding. Similarly, inventories of child sensory sensitivity and more comprehensive background information on children’s medical and intellectual functioning could enrich the current model’s conceptualization from a physiological standpoint. The current study expanded on the literature regarding the relations between disruptive behavior, parent problematic feeding behavior, ASD, parenting stress, and children’s problematic feeding using a biopsychosocial framework. This study represents one study among several recent studies that have shown that children with ASD have higher levels of disruptive behavior and problematic feeding behavior than typically developing children, though the precise relations between general disruptive behavior and problematic feeding behavior are still not entirely clear. Due to the complexity of factors involved in pediatric feeding behavior, treating feeding disorders clinically is complicated. Hopefully, with continued replication and extension of this research, knowledge obtained from previous studies and the current study will further contribute to the development of evidence-based prevention, assessment, and treatment of pediatric feeding disorders.
References
Allen, S., Smith, I., Duku, E., Vaillancourt, T., Szatmari, P., Bryson, S., … Georgiades, S. (2015). Behavioral pediatrics feeding Assessment scale in young children with autism spectrum disorder: Psychometrics and associations with child and parent variables. Journal of Pediatric Psychology,40, 581–590.
Babbitt, R. L., Hoch, T. A., Coe, D. A., Cataldo, M. F., Kelly, K. J., Stackhouse, C., & Perman, J. A. (1994). Behavioral assessment and treatment of pediatric feeding disorders. Journal of Developmental & Behavioral Pediatrics, 15(4), 278–291.
Bachmeyer, M., Piazza, C., Fredrick, L., Reed, G., Rivas, K., & Kadey, H. (2009). Functional analysis and treatment of multiply controlled inappropriate mealtime behavior. Journal of Applied Behavior Analysis,42, 641–658.
Bagner, D., & Eyberg, S. (2007). Parent–child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child and Adolescent Psychology,36, 418–429.
Berlin, K., Davies, W., Lobato, D., & Silverman, A. (2009). A biopsychosocial model of normative and problematic pediatric feeding. Children’s Health Care,38, 263–282.
Blissett, J., & Farrow, C. (2007). Predictors of maternal control of feeding at 1 and 2 years of age. International Journal of Obesity, 31(10), 1520–1526.
Blissett, J., Meyer, C., & Haycraft, E. (2011). The role of parenting in the relationship between childhood eating problems and broader behaviour problems. Child: Care, Health and Development,37, 642–648.
Boggs, S., Eyberg, S., & Reynolds, L. (1990). Concurrent validity of the Eyberg child behavior inventory. Journal of Clinical Child Psychology,19, 75–78.
Burklow, K., Phelps, A., Schultz, J., McConnell, K., & Rudolph, C. (1998). Classifying complex pediatric feeding disorders. Journal of Pediatric Gastroenterology and Nutrition,27, 143–147.
Chatoor, I., Ganiban, J., Harrison, J., & Hirsch, R. (2001). Observation of feeding in the diagnosis of posttraumatic feeding disorder of infancy. Journal of the American Academy of Child and Adolescent Psychiatry,40, 595–602. https://doi.org/10.1097/00004583-200105000-00020.
Cone, J. D., & Casper-Beliveau, S. (1997). The Eyberg Child Behavior Inventory: Psychometric properties when used with children with developmental disabilities. In annual meeting of the Association for the Advancement of Behavior Therapy, Miami, FL.
Crist, W., McDonnell, P., Beck, M., Gillespie, C., Barrett, P., & Mathews, J. (1994). Behavior at mealtimes and the young child with cystic fibrosis. Journal of Developmental and Behavioral Pediatrics,15, 157–161.
Crist, W., & Napier-Phillips, A. (2001). Mealtime behaviors of young children: A comparison of normative and clinical data. Journal of Developmental and Behavioral Pediatrics,22, 279–286.
Davis, N., & Carter, A. (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders,38, 1278–1291.
Delaney, A. L., & Arvedson, J. C. (2008). Development of swallowing and feeding: Prenatal through first year of life. Developmental Disabilities Research Reviews, 14(2), 105–117.
de Moor, J., Didden, R., & Korzilius, H. (2007). Parent-reported feeding and feeding problems in a sample of Dutch toddlers. Early Child Development and Care,177, 219–234.
Dovey, T., Jordan, C., Aldridge, V., & Martin, C. (2013). Screening for feeding disorders. Creating critical values using the behavioural pediatrics feeding assessment scale. Appetite,69, 108–113.
Eyberg, S., Boggs, S., & Reynolds, L. (1980). Eyberg child behavior inventory. Portland: University of Oregon Health Sciences Center.
Eyberg, S. & Pincus, D. (1999). Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory-Revised: Professional Manual. Psychological Assessment Resources.
Field, D., Garland, M., & Williams, K. (2003). Correlates of specific childhood feeding problems. Journal of Pediatrics and Child Health,39, 299–304.
Funderburk, B., Eyberg, S., Rich, B., & Behar, L. (2003). Further psychometric evaluation of the Eyberg and Behar rating scales for parents and teachers of preschoolers. Early Education and Development,14, 67–82.
Galloway, A. T., Fiorito, L. M., Francis, L. A., & Birch, L. L. (2006). ‘Finish your soup’: Counterproductive effects of pressuring children to eat on intake and affect. Appetite, 46(3), 318–323.
Greer, A., Gulotta, C., Masler, E., & Laud, R. (2008). Caregiver stress and outcomes of children with pediatric feeding disorders treated in an intensive interdisciplinary program. Journal of Pediatric Psychology,33, 612–620.
Gueron-Sela, N., Atzaba-Poria, N., Meiri, G., & Yerushalmi, B. (2011). Maternal worries about child underweight mediate and moderate the relationship between child feeding disorders and mother–child feeding interactions. Journal of Pediatric Psychology, 36(7), 827–836.
Hagekull, B., Bohlin, G., & Rydell, A. (1997). Maternal sensitivity, infant temperament, and the development of early feeding problems. Infant Mental Health Journal,18, 92–106.
Haskett, M., Ahern, L., Ward, C., & Allaire, J. (2006). Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child and Adolescent Psychology,35, 302–312.
Haycraft, E., Farrow, C., Meyer, C., Powell, F., & Blissett, J. (2011). Relationships between temperament and eating behaviours in young children. Appetite, 56(3), 689–692.
Johnson, C., Turner, K., Stewart, P., Schmidt, B., Shui, A., Macklin, E., … Hyman, S. (2014). Relationships between feeding problems, behavior problems and nutritional quality in children with ASD. Journal of Autism and Developmental Disorders,44, 2175–2184.
Jones, M., Morgan, E., & Shelton, J. (2002). Follow-up of the high-risk infant. Dysphagia and oral feeding problems in the premature infant. Neonatal Network, 21(2), 51–57.
Kerwin, M. (1999). Empirically supported treatments in pediatric psychology: Severe feeding problems. Journal of Pediatric Psychology,24, 193–214.
Lecavalier, L., Leone, S., & Wiltz, J. (2006). The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research, 50(3), 172–183.
Lewinsohn, P., Holm-Denoma, J., Gau, J., Joiner, T., Striegel-Moore, R., Bear, P., & Lamoureux, B. (2005). Problematic eating and feeding behaviors of 36-month-old children. International Journal of Eating Disorders,38, 208–219.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders,24, 659–685.
Mackner, L., McGrath, A., & Stark, L. (2001). Dietary recommendations to prevent and manage chronic pediatric health conditions: Adherence, intervention, and future directions. Journal of Developmental and Behavioral Pediatrics,22, 130–143.
Manikam, R., & Perman, J. (2000). Pediatric feeding disorders. Journal of Clinical Gastroenterology,30, 34–46.
Martins, Y., Young, R., & Robson, D. (2008). Feeding and eating behaviors in children with autism and typically developing children. Journal of Autism and Developmental Disorders,38(10), 1878–1887.
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011). Mealtime problems in children with autism spectrum disorder and their typically developing siblings: A comparison study. Autism, 15(1), 98–113.
Preacher, K., & Hayes, A. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods,40(3), 879–891.
Reitman, D., Currier, R., & Stickle, T. (2002). A critical evaluation of the parenting stress index-short form (PSI-SF) in a head start population. Journal of Clinical Child and Adolescent Psychology,31(3), 384–392.
Rigal, N., Chabanet, C., Issanchou, S., & Monnery-Patris, S. (2012). Links between maternal feeding practices and children’s eating difficulties. Validation of French tools. Appetite, 58(2), 629–637.
Robinson, E., Eyberg, S., & Ross, A. (1980). The standardization of an inventory of child conduct problem behaviors. Journal of Clinical Child & Adolescent Psychology,9(1), 22–28.
Rogers, L., Magill-Evans, J., & Rempel, G. (2012). Mothers’ challenges in feeding their children with autism spectrum disorder—Managing more than just picky eating. Journal of Developmental and Physical Disabilities,24(1), 19–33.
Rommel, N., De Meyer, A., Feenstra, L., & Veereman-Wauters, G. (2003). The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. Journal of Pediatric Gastroenterology and Nutrition,37(1), 75–84.
Rutter, M., DiLavore, P., Risi, S., Gotham, K., & Bishop, S. (2012). Autism diagnostic observation schedule: ADOS-2. Los Angeles: Western Psychological Services.
Satter, E. (1990). The feeding relationship: Problems and interventions. The Journal of Pediatrics,117(2), S181–S189.
Schieve, L., Blumberg, S., Rice, C., Visser, S., & Boyle, C. (2007). The relationship between autism and parenting stress. Pediatrics,119(Supplement 1), S114–S121.
Schreck, K., Williams, K., & Smith, A. (2004). A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders,34(4), 433–438.
Sharp, W., Berry, R., McCracken, C., Nuhu, N., Marvel, E., Saulnier, C., ... Jaquess, D. (2013). Feeding problems and nutrient intake in children with autism spectrum disorders: A meta-analysis and comprehensive review of the literature. Journal of Autism & Developmental Disorders, 43(9), 2159–2173. https://doi.org/10.1007/s10803-013-1771-5.
Sharp, W., Jaquess, D., Morton, J., & Herzinger, C. (2010). Pediatric feeding disorders: A quantitative synthesis of treatment outcomes. Clinical Child and Family Psychology Review,13(4), 348–365.
Shore, B., Babbitt, R., Williams, K., Coe, D., & Snyder, A. (1998). Use of texture fading in the treatment of food selectivity. Journal of Applied Behavior Analysis,31(4), 621–633.
Webster-Stratton, C., & Hammond, M. (1997). Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology,65(1), 93.
Weitlauf, A., Vehorn, A., Taylor, J., & Warren, Z. (2014). Relationship satisfaction, parenting stress, and depression in mothers of children with autism. Autism,18(2), 194–198.
Zaidman-Zait, A., Mirenda, P., Zumbo, B., Wellington, S., Dua, V., & Kalynchuk, K. (2010). An item response theory analysis of the parenting stress index-short form with parents of children with autism spectrum disorders. Journal of Child Psychology and Psychiatry,51(11), 1269–1277.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical Approval
Prior to recruitment and data collection, Intuitional Review Board Approval was obtained from the first author’s home institution and each data collection site provided administrative approval for the conduct of the current research project. Legal guardians were provided with study information and provided documented informed consent prior to completing any study measures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murphy, J., Zlomke, K., VanOrmer, J. et al. Impact of Disruptive Behavior in Childhood Feeding Difficulties. J Clin Psychol Med Settings 27, 406–415 (2020). https://doi.org/10.1007/s10880-019-09646-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-019-09646-y




