Abstract
Young children with T1D frequently display challenging eating behaviors interfering with diabetes management. The current study explored the feasibility and acceptability of a behavioral parent feeding training session with young children with type 1 diabetes. As part of a larger intervention pilot focused on healthy eating and physical activity, 9 young children (Mage = 4.22) with type 1 diabetes (T1D) and their mothers participated in a novel/non-preferred food training session. Parents were taught strategies and then were given an opportunity to use the strategies with their child. The paradigm was video recorded and content was coded for parent and child behavior. Feasibility was high, and all parents rated the feeding session as acceptable. All parents demonstrated using at least one behavioral feeding skill (M = 3.38, SD = 1.60). All 9 (100%) children touched at least one of their non-preferred foods (M = 2.05, SD = 0.75), and 5 (56%) ate at least one novel/non-preferred food (M = 1.65, SD = 0.87). Parents of young children with T1D demonstrated use of parenting skills after receiving brief instructions, with more children than not trying at least one novel/non-preferred food.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Feeding challenges are a common complaint among parents of many young children, with about 14–50% of preschool aged children demonstrating difficulties with eating (Cano, Hoek, Bryant-Waugh, 2015). Common eating challenges include a range of behaviors including food refusal, food neophobia, slowness in eating, prolonged meal times, and display of negative emotions during meal times (Cano et al., 2015). There is a range of severity of eating challenges from minor picky eating to total food refusal (Carruth, Ziegler, Gordon, & Barr, 2004). Consequences for food refusal can include malnutrition, dehydration, and growth retardation (De Moor, Didden, & Korzilius, 2007).
Environmental factors play an important role in exacerbation and maintenance of food refusal. When children learn that they can avoid or escape the aversive situation of being presented a non-preferred food by refusing to eat, food refusal is negatively reinforced. These behaviors become problematic when the list of preferred foods continues to shrink, resulting in a reduced dietary intake and quality (Cano et al., 2015). Parents of children with food refusal experience significant distress, concern for their child’s long-term health, and feelings of incompetence relating to their ability to feed their child (Cano et al., 2015; De Moor, Didden, & Korzilius, 2007). Though feeding challenges are relatively common in young children and typically decline on their own by age 5, many parents report lasting high levels of stress surrounding mealtimes (Chisholm et al., 2011), and these concerns are often exacerbated for parents of children with chronic illnesses requiring dietary management.
Common and Effective Feeding Strategies
Several effective feeding strategies have been identified in the literature to decrease food refusal in both typically-developing children and those with feeding difficulties (Lukens & Silverman, 2014; Nekitsing, Blundell-Birtill, Cockroft, & Hetherington, 2018). Altering the feeding structure (e.g., consistent meal times), manipulating hunger (e.g., eliminating grazing in between meal times, increasing the child’s hunger during scheduled meal times), employing contingency management (e.g., differential attention), and shaping (e.g., reinforcement of successive approximations) are components of behavioral parent feeding training (Fischer & Silverman, 2007; Silverman, 2015). Modeling and praise have been associated with increased consumption and higher reported child enjoyment of food (Addessi et al., 2005). Increasing the number of times novel foods may need to be presented and using praise for eating approach behaviors (e.g., touching, smelling, licking) have been linked with improved child eating (Rowell & McGlothlin, 2015). For example, for a target of taking a bite of a vegetable, the parent could successively praise and reinforce the child for having the vegetable on his plate, smelling it, touching it, licking it without swallowing, and then ultimately taking a bite and swallowing. Other strategies include contingency management and discrimination training (Silverman, 2015).
Ineffective Feeding Strategies
Research in typically-developing children has identified common behavioral feeding strategies that parents often use that are likely to decrease children’s food consumption. Common ineffective strategies include restriction (e.g., blocking access to “unhealthy” or undesired foods), pressure to eat, and coercion (e.g., demanding the child finish their food, making the child eat a less desired food in order to have access to a desired food). Birch et al. (2003) found that restricting food access actually increased in children’s interest in, requests for, and consumption of those foods. By contrast, hunger manipulation involves feeding on a specific schedule with the goal of increasing the child’s appetite at meal and snack times. Using a desired food as a reward for eating an undesired/novel food is also associated with a decreased liking of the undesired/novel food (i.e., offering gummy bears in exchange for eating broccoli can lead to a further decrease in broccoli consumption; Mikula, 1989). Additionally, parental pressure or coercion to eat has been related to decreased consumption of fruits and vegetables (Galloway et al., 2006).
Feeding Challenges Among Children with T1D
The consequences of developmentally normative feeding challenges are potentially more severe in children with chronic illnesses (Borge, Wefring, Lie, & Nordhagen, 2004). Parents of children with a chronic illness report higher prevalence of feeding challenges compared to their counterparts (Borge, Wefring, Lie, & Nordhagen, 2004). Children are more likely to have behavioral problems at mealtimes when their parents are more concerned about their food consumption and health (Crist et al., 1994). Children with one of the most common childhood chronic illnesses, type 1 diabetes (T1D), are encouraged to consume a balanced diet of fruits, vegetables, and whole grains while also addressing insulin needs (Rovner & Nansel, 2009). A key component of diabetes management includes nutrition management and tracking carbohydrate consumption to properly match and administer the insulin dose necessary for glycemic control (Nansel et al., 2015). To optimize the effects of insulin, parents are counseled to administer insulin 20 –30 min prior to eating based on the carbohydrates in the meal (American Diabetes Association, 2017). However, inconsistent eating patterns can make prediction for insulin dosing and timing difficult, as well as increase the risk of hypoglycemia if insulin is administered yet the child eats less than expected (Patton, Dolan, & Powers, 2006). Hypoglycemia can cause short- and long-term medical complications including seizures, unconsciousness, coma, and even death (Bade-White & Obrzut, 2009). Therefore, fear of hypoglycemia leads to high parent stress surrounding insulin administration and food consumption for these young children (Monaghan et al., 2015).
Parents of young children with diabetes report a number of strategies to manage dietary needs, including delaying insulin administration to after the meal. This practice can better match dosage to amount eaten, though it prevents the insulin from working to reduce the initial blood glucose peak and can lead to hyperglycemia (Goonetilleke, Pollitzer, & Mann, 2004). Others describe resorting to an over-reliance on the highly palatable, high carbohydrate foods that they are more certain their child will eat (Cano et al., 2015). While this reduces the likelihood of the immediate dangers of hypoglycemia, this practice is also problematic as it results in more variable blood glucose levels and can limit the variety of foods the child will accept, restricting the nutrients they receive and making it harder to manage diabetes (Nansel et al., 2015). Further, if the parent provides a more palatable/less healthy option when the child refuses the original meal, a cycle of inadvertently reinforcing food refusal may begin (Sherry et al., 2004).
Due to the negative impact on health outcomes food neophobia can have on young children with T1D, additional supports are needed for families to better manage common picky eating and food neophobia. Though the behavioral parenting strategies described above (i.e., modeling and encouragement) have demonstrated success in children with obesity and in non-disease populations, they are unexplored in young children with T1D. The purpose of this study was to evaluate the feasibility and acceptability of conducting a behavioral parenting feeding training session to reduce picky eating as part of a larger six-session behavioral pilot intervention focused on healthy eating and physical activity promotion in young children with T1D (Tully, Aronow, Mackey, Henderson, Wang, & Streisand, in press). We hypothesized that it would be feasible and acceptable to include one in-clinic parent–child ‘snack’ session as part of the larger intervention feasibility study.
Method
Participants
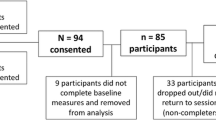
Primary caregivers of young children (2–5 years, Mage = 4.2) with T1D were recruited for this pilot from an outpatient diabetes clinic in a pediatric academic medical center in a mid-Atlantic city (see Table 1). Eligibility criteria included being in the adult age range (≥ 21+ years of age), English fluency, and having a child with ≥ 1 year duration of T1D (Mage of diagnosis = 2.4 years) with no other life-threatening diseases or developmental disability that might impact participation. Children following all diabetes regimens, with any level of glycemic control, were eligible. Families with any feeding/eating presentation were eligible; none reported histories of receiving formal feeding interventions. Ten parent–child dyads enrolled; one dyad dropped out after completing baseline questionnaires; this report focuses on the nine that completed the intervention sessions. All primary caregivers were mothers and 56% (N = 5) were married. The sample was 56% (N = 5) Caucasian and 44% (N = 4) African American. The sample mean A1c was above recommended guidelines of less than 7.5% for all youth (M = 8.1% ± 0.9; 22% A1c below 7.5%, ADA, 2017).
Measures
To meet the primary aim of this paper to determine the feasibility and acceptability of a brief eating challenge as part of an intervention, results focus on participant completion and satisfaction data. Following completion of the overall 6-session treatment program, parents completed a 37-item satisfaction survey reporting on the perceived acceptability and usefulness of the program content. One question asked about the family’s usefulness rating for the in-clinic parent–child ‘snack’ behavioral feeding intervention. Qualitative interviews were conducted at the 6-month follow-up to further assess feasibility and acceptability of in-clinic parent–child ‘snack’ session as well as the intervention as a whole. Three psychologists and members of the study team conducted the qualitative interviews using 14 open-ended questions that were collaboratively created by the PI (last author) and study team. Questions focused on assessing feasibility, acceptability, as well as any areas in need of content expansion. Examples of questions included, “What, if anything, would you change about the program?”
Procedure
Pilot Intervention
This paper reports on procedures from one in-clinic parent–child ‘snack’ session from a six-session manualized healthy eating and physical activity promotion feasibility study for parents of young children with T1D. Other phone based and nutrition-focused sessions in the larger intervention taught macronutrient education, encouraged providing high quality foods with a particular focus on increasing protein consumption, involving children in meal preparation, and handling child misbehavior at meals. Three psychologists (first, fourth, and last authors), who assisted in program development, served as interventionists. Each session was manualized to promote treatment adherence by interventionists. The manual served as a guide providing a session outline, teaching points, reminders to reinforce the parent to build parent self-efficacy for using new skills, and homework assignments. The in-clinic parent–child ‘snack’ behavioral feeding parenting session (session 2 of 6), required participants to come to the medical center, and the remainder of the sessions were delivered by telephone. Interventionists used individualized goal setting to assign tasks to families to complete in the 1–2 weeks between each session.
Potential participants were recruited via letter through clinic lists. From 25 letters sent, 10 mothers enrolled (83% of those who were reached and eligible). Top reasons for declining participation included concerns over time commitment and travel distance. All parents reported on their child’s dietary patterns at the in-person study orientation. Using a standard list of foods, parents self-reported their child’s preferred and non-preferred/novel foods while children played with a food sticker book and a healthy eating coloring book. Parents were prompted to provide protein, fruit, and vegetable preferred and non-preferred food options. Given the specific aims of this manuscript, only details of the behavioral feeding parenting session are presented below.
Behavioral Feeding Parenting Session
The behavioral feeding skill session was adapted from previous work (e.g., Galloway, Fiorito, Francis, & Birch, 2006). General feeding principles were discussed using the study manual, including maintaining appropriate boundaries and feeding roles, implementing predictable meal and snack times with limited duration, expecting the need for high presentation repetition to combat food neophobia, and providing appropriate feeding environments. Along with education regarding general feeding principles, parents were taught 6 behavioral feeding strategies including modeling (putting the food on the skewer, tasting the food), narrating (describing what they are doing with the food), shaping with selective attention (i.e., encouraging touching food, or encouraging tasting without emphasizing swallowing), downplaying importance (e.g., not giving direct commands about the food), and making it a game (e.g., competitions to make the loudest crunch sound). In addition, parents were taught using reverse psychology (i.e., “I bet you won’t be able to eat that!”) as an exploratory feeding strategy. Parents were also instructed to avoid coercive tactics (bribing, threatening, and criticizing).
Parents spent the first half of the in-clinic parent–child ‘snack’ feeding session alone with their interventionist (15–20 min) learning to use the parenting feeding strategies just detailed. During this time, children played a food-based tablet computer game with a trained research assistant (e.g., chopping fruit, cooking, etc). Parents were supplied with a list of the carbohydrate counts for the food that was to be offered to their child in the next phase of the session, in order to determine if any insulin adjustments or additional blood glucose checks were needed before starting.
After parents were finished in the skill acquisition phase, their child joined them and was presented with small pieces of three preferred and three non-preferred/novel foods (see Fig. 1). As a primary goal of the overall intervention was on increasing protein content of the breakfast meal, at least two items were protein selections (e.g., hardboiled egg, cheese stick) with the remainder including fruits and vegetables. Children were given the instruction to make a rainbow with the different colors of food on their toothpick. Parents used the behavioral feeding skills with the goal of increasing their child’s acceptance of the novel/non-preferred foods while the interventionist observed. Following the feeding training session, the child returned to play with the research assistant, and the interventionist reviewed the feeding interaction and provided feedback to the parent with emphasis on reinforcement for skills performed well. The session was video recorded for fidelity monitoring and data collection.
Image of a feeding training session plate set up. Plate included in feeding sessions depicting 3 preferred and 3 non-preferred foods. Foods displayed are (clockwise from top) diced turkey, blueberries, grapes, cucumber, red bell pepper, and hard-boiled egg. Children were instructed to build colorful patterns of food on the sword shaped toothpicks in the center
Session Coding
The interventionist coded the feeding training session for parent and child feeding behavior content and parent engagement; one objective rater later coded each video recording to provide double coding of each recording. The objective coder was trained by one of the interventionists (first author) by reading scoring guides and empirical articles relating to the method, reviewing specific practice segments, and practicing scoring sessions. The coder met with the interventionist weekly to discuss the coding process, review reliability assessments, and to prevent coder drift (Margolin et al., 1998). Coding was completed for 10 actions using Likert-type scales including amount of parenting feeding behaviors (0 = not at all, 5 = behavior occurred more than 5 times), enthusiasm, and engagement (0 = none, 5 = a lot) displayed and child eating behaviors (e.g., counts of how many foods each child tried). A two-way random effects intraclass coefficient model was used to determine rating reliability, and the agreement between raters (interventionist and objective rater) was moderate (ICC = 0.71; Shrout & Fleiss, 1979).
Statistical Analyses
Given the focus of this paper is on the feasibility and acceptability of the feeding training session within the context of the larger behavioral intervention, mixed methods were used to analyze feasibility and parent satisfaction. Descriptions of the behaviors observed in session are provided. For the qualitative interviews, two coders working independently extracted themes from the field notes until saturation was met. Coders met with the remaining study team to review themes and resolve discrepancies. The participant satisfaction questionnaire and qualitative interviews were examined for evidence of acceptability. Feasibility was defined through time (i.e., demonstration of a short session), fidelity (i.e., a session that can be implemented with high fidelity), and safety (i.e., evidence of the absence of patient harm). Evidentiary support for acceptability was defined as parental uptake measured by demonstration of feeding skills, good feedback in qualitative interviews, as well as high parent reported self-reported satisfaction on questionnaires (≥ 4.00, scale 1–5, 5 is very high satisfaction) and in response to researchers during the paradigm.
Results
All of the 9 parents and children who completed the first intervention session also completed the session 2 feeding training session. The session took approximately 45 min (M = 48.86, SD = 6.79), with the feeding rehearsal component with the child in the room averaging less than 10 min of the overall session (M = 6.37, SD = 2.30). Interventionists self-reported 98% adherence to the session manual. A subsample of the study recordings (20%) were reviewed by the principal investigator and study coordinator for fidelity monitoring and found to have 100% adherence. Since the children ate relatively small amounts of the foods, no parents reported administering additional insulin. Parents reported no medical concerns for their children in relation to the feeding session.
With regards to acceptability, parents rated the session as either “very useful” or “somewhat useful” (M = 4.67, SD = 0.50; 1–5, 5 = very useful). In qualitative interviews about the feeding session, one parent reported, “it was surprising to see him eat [non-preferred food]! I had stopped making it because I thought he would never eat it, so that was crazy.” Parent anecdotal response to interventionists about the feeding training session was generally positive. Before the interaction began, three parents predicted their child would not eat a non-preferred food, and reported surprise when their child did indeed try the non-preferred food. Two parents reported perceptions that the novel environment and attention played a role in increasing their child’s likelihood to try previously non-preferred foods. Parents also reported the hands-on nature of the task, and their child’s ready acceptance of the new foods, made them reconsider breakfast food choices and how they could fit new foods into the family’s morning routines. For example, three parents reported intentions to hard-boil several eggs ahead of time and provide them for breakfasts on subsequent days; two others discussed the value of serving fast non-traditional breakfast foods (e.g., roll of deli sliced meat, cheese stick).
All parents used more than one feeding strategy during the feeding training session (M = 3.56; SD = 1.60; see Table 2). The most commonly used strategies were narrating (100%) and modeling (100%), followed by downplaying importance of trying a new food (67%), making it a game (56%), shaping (22%) and reverse psychology (22%; Fig. 2). Only one parent demonstrated criticism (11%) and none displayed bribery or coercion. Parents who showed more interventionist-rated enthusiasm for the feeding task trended toward using more behavioral feeding skills (r = .67, p = .05). However, there was no relationship between interventionist-rated parent enthusiasm and child acceptance of novel/non-preferred food (r = .24, p = .53). All children touched at least one of their non-preferred foods; five ate at least one novel/non-preferred food (see Fig. 3).
Conclusion
A brief one-time, in-clinic parent feeding training session was feasible with parents of young children with T1D, as part of a larger telephone based intervention. The majority of parents reported high acceptability and feasibility of the intervention. As a whole, the feeding training session took less than an hour (with less than 10 min required from the child) suggesting high potential for translation into clinic settings. Exploratory results were promising demonstrating initial evidence of utility for a feeding training session for parents of young children with T1D. All parents who participated in the behavioral parenting feeding training session demonstrated use of the feeding techniques to encourage acceptance of novel foods. Each child touched at least one non-preferred/novel food; the majority of children ate or tasted at least one novel/non-preferred foods. In the context of shaping, these successive approximations (e.g., touching, smelling, licking, tasting without swallowing) are all approach behaviors toward accepting and eating novel/non-preferred food (e.g., Stark, 2003). It is possible that participation in this session may have helped parents increase their self-efficacy to use behavioral parenting feeding skills at home with their children to encourage a higher quality diet. Parents who feel competent in their ability to deal with problematic feeding behaviors are more likely to use positive behavioral feeding strategies and have more positive feeding interactions (Bocknek, Brophy-Herb, Banerjee, 2009).
These results must be understood within the context of study limitations. The sample for this pilot was small by design to test feasibility; however, further study is needed to understand how these results translate to larger populations. The larger randomized controlled trial, currently underway, will provide more information about efficacy and generalizability. In addition, parents’ familiarity or use of behavioral parent feeding strategies at baseline was not objectively measured or controlled, so it is unclear if the behaviors seen during the intervention were a direct result of the content taught. Additionally, some skills might have been easier to learn and perform in a short amount of time than others (e.g., modeling versus initiating a game). For a true test of behavior change, it would be recommended to measure behavior and familiarity with these skills at baseline. Additional assessment using an observational-based system in the home environment is also recommended to see if skills learned at the clinic setting translated to the real world. Quantitative analysis could also be conducted through a follow-up questionnaire which could assess parents’ rates of feeding strategies and child feeding patterns post intervention. Last, no participants reported on needing to administer insulin to compensate for the very small amounts of food eaten during this in-clinic experiment. However, it is possible that parents would administer insulin for a calculated amount before initiating this type of snack challenge at home, and it is recommended that they have a neutral food available to offer to compensate for the insulin administered if the child does not eat the non-preferred food. It’s recommended to use a food that parents are certain the child will accept, such as milk, but is not highly preferred (e.g., do not use favorite fruits or candy) as the latter could inadvertently continue to reinforce food refusal.
In sum, this one-session behavioral parent feeding intervention demonstrated feasibility and acceptability to parents of young children with T1D. Initial results suggested parents were successful in demonstrating parenting strategies after a single teaching session, and that children showed approach behaviors toward acceptance of new/non-preferred foods. There are implications for clinical practice that a one-time brief session within a subspecialty clinic with a behavioral health specialist focusing parent behavioral feeding skills is possible, and may have high impact. Whether these results generalize to larger samples of youth with T1D, other illness populations, is an important question for future research.
References
Addessi, E., Galloway, A. T., Visalberghi, E., & Birch, L. L. (2005). Specific social influences on the acceptance of novel food in 2–5 year old children. Appetite, 45, 264–271.
American Diabetes Association. (2017). Children and adolescents. Diabetes Care 40, S105–S113. https://doi.org/10.2337/dc17-S015.
Bade-White, P., & Obrzut, J. E. (2009). The neurocognitive effects of type 1 diabetes mellitus in children and young adults with and without hypoglycemia. Journal of Developmental and Physical Disabilities, 21, 425–440. https://doi.org/10.1007/s10882-009-9151-y.
Birch, L. L., Fisher, J. O., & Davison, K. K. (2003). Learning to overeat: Maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. The American Journal of Clinical Nutrition, 78, 215–220.
Bocknek, E. L., Brophy-Herb, H. E., & Banerjee, M. (2009). Effects of parental supportiveness on toddlers’ emotion regulation over the first three years of life in a low-income African American sample. Infant Mental Health Journal, 27, 5–25. https://doi.org/10.1002/imhj.
Borge, A. I. H., Wefring, K. W., Lie, K. K., & Nordhagen, R. (2004). Chronic illness and aggressive behaviour: A population-based study of 4-year olds. European Journal of Developmental Psychology, 1, 19–29.
Cano, S. C., Hoek, H. W., & Bryant-Waugh, R. (2015). Picky eating: The current state of research. Current Opinion in Psychiatry, 28, 448–454. https://doi.org/10.1097/YCO.0000000000000194.
Cano, S. C., Tiemeier, H., Van Hoeken, D., Tharner, A., Jaddoe, V. W. V., Hofman, A., … Hoek, H. W. (2015). Trajectories of picky eating during childhood: A general population study. International Journal of Eating Disorders, 48, 570–579. https://doi.org/10.1002/eat.22384.
Carruth, B. R., Ziegler, P. J., Gordon, A., & Barr, S. I. (2004). Prevalence of picky eaters among infants and toddlers and their caregivers’; decisions about offering a new food. Journal of the Academy of Nutrition and Dietetics, 104, 57–64. https://doi.org/10.1016/j.jada.2003.10.024.
Chisholm, V., Atkinson, L., Donaldson, C., Noyes, K., Payne, A., & Kelnar, C. (2011). Maternal communication style, problem-solving and dietary adherence in young children with type 1 diabetes. Clinical Child Psychology and Psychiatry, 16, 443–458. https://doi.org/10.1177/1359104510373312.
Crist, W., McDonnell, P., Beck, M., Gillespie, C. T., Barrett, P., & Mathews, J. (1994). Behavior at mealtimes and nutritional intake in the young child with cystic fibrosis. Developmental and Behavioral Pediatrics, 15, 157–161.
De Moor, J., Didden, R., & Korzilius, H. (2007). Behavioural treatment of severe food refusal in five toddlers with developmental disabilities. Child: Care, Health and Development, 33, 670–676. https://doi.org/10.1111/j.1365-2214.2007.00734.x.
Fischer, E., & Silverman, A. (2007). Behavioral conceptualization, assessment, and treatment of pediatric feeding disorders. Seminars in Speech and Language, 28, 223–231.
Galloway, A. T., Fiorito, L. M., Francis, L. A., & Birch, L. L. (2006). ‘Finish your soup’: Counterproductive effects of pressuring children to eat on intake and affect. Appetite, 46, 318–323.
Goonetilleke, R., Pollitzer, M., & Mann, N. (2004). Insulin for toddlers with difficult diabetes. Diabetes Care. https://doi.org/10.2337/diacare.27.6.1505.
Lukens, C. T., & Silverman, A. H. (2014). Systematic review of psychological interventions for pediatric feeding problems. Journal of Pediatric Psychology, 39, 903–917. https://doi.org/10.1093/jpepsy/jsu040.
Margolin, G., Oliver, P., Gordis, E., O’Hearn, H., Medina, A., Ghosh, C., & Morland, L. (1998). The nuts and bolts of behavioral observation of marital and family interaction. Clinical Child & Family Psychology Review, 1, 195–213.
Mikula, G. (1989). Influencing food preferences of children by ‘if-then’ type instructions. European Journal of Social Psychology, 19, 225–241. https://doi.org/10.1002/ejsp.2420190304.
Monaghan, M., Herbert, L. J., Wang, J., Holmes, C., Cogen, F. R., & Streisand, R. (2015). Mealtime behavior and diabetes-specific parent functioning in young children with type 1 diabetes. Health Psychology, 34, 794–801. https://doi.org/10.1037/hea0000204.
Nansel, T. R., Laffel, L. M. B., Haynie, D. L., Mehta, S. N., Lipsky, L. M., Volkening, L. K., … Liu, A. (2015). Improving dietary quality in youth with type 1 diabetes: Randomized clinical trial of a family-based behavioral intervention. International Journal of Behavioral Nutrition and Physical Activity, 12, 58. https://doi.org/10.1186/s12966-015-0214-4.
Nekitsing, C., Blundell-Birtill, P., Cockroft, J. E., & Hetherington, M. M. (2018). Systematic review and meta-analysis of strategies to increase vegetable consumption in preschool children aged 2–5 years. Appetite, 1, 138–154. https://doi.org/10.1016/j.appet.2018.04.019.
Patton, S. R., Dolan, L. M., & Powers, S. W. (2006). Parent report of mealtime behaviors in young children with type 1 diabetes mellitus: Implications for better assessment of dietary adherence problems in the clinic. Journal of Developmental and Behavioral Pediatrics, 27, 202–208. https://doi.org/10.1097/00004703-200606000-00004.
Rovner, A. J., & Nansel, T. R. (2009). Are children with type 1 diabetes consuming a healthful diet? A review of the current evidence and strategies for dietary change. The Diabetes Educator, 35, 97–107. https://doi.org/10.1177/0145721708326699.
Rowell, K., & McGlothlin, J. (2015). Helping your child with extreme picky eating. Oakland: New Harbinger Publications, Inc.
Sherry, B., McDivitt, J., Birch, L., Cook, F., Sanders, S., Prish, J., Francis, L., & Scanlon, K. (2004). Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. Journal of the Academy of Nutrition and Dietetics, 104, 215–221.
Shrout, P. E., & Fleiss, J. L. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86, 420–428.
Silverman, A. (2015). Behavioral management of feeding disorders of childhood. Annals of Nutrition & Metabolism, 66, 33–42. https://doi.org/10.1159/000381375.
Stark, L. (2003). Can nutrition counselling be more behavioural? Lessons learned from dietary management of cystic fibrosis. Proceedings of the Nutrition Society, 62, 793–799. https://doi.org/10.1079/PNS2003294.
Tully, C., Aronow, L., Mackey, E., Henderson, C., Wang, J., & Streisand, R. (in press). Development and preliminary outcomes of a healthy eating and physical activity intervention for parents of young children with type 1 diabetes. Journal of Pediatric Health Care.
Funding
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (Grant Number DP3DK103998-01) awarded to Randi Streisand, Ph.D.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Carrie Tully, Corrine Ahrabi-Nejad, Leann L. Birch, Eleanor Mackey, and Randi Streisand declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animal Rights and Informed Consent
Institutional Review Board approval was obtained prior to the start of recruitment and all participants provided informed consent prior to beginning the study.
Rights and permissions
About this article
Cite this article
Tully, C., Ahrabi-Nejad, C., Birch, L.L. et al. Feasibility of Including Behavioral Feeding Training Within a Parent Intervention for Young Children With Type 1 Diabetes. J Clin Psychol Med Settings 26, 220–227 (2019). https://doi.org/10.1007/s10880-018-9577-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-018-9577-4