Abstract
Although spine surgery (SS) and spinal cord stimulators (SCSs) can provide significant relief for patients with intractable pain, their effectiveness is variable. Previously, a number of pre-operative psychosocial risk factors have predicted suboptimal outcomes of these procedures. However, recent research has found that “patient activation”—the extent to which patients are engaged and active in their own health care—can predict positive surgical results. The purpose of the current investigation was to determine whether patient activation helps explain associations between established psychosocial risk factors and suboptimal outcomes. Candidates for SS and SCS (n = 1254; 56.3% women, mean age 50.4 years) consented to participate in an outcome study prior to their pre-surgical psychological evaluation. Of those, 46.3% returned self-report measures an average of 180 days (SD = 79.1) post-surgery. Bootstrapped mediation analyses indicated that patient activation mediates numerous associations between psychosocial risk factors and suboptimal outcomes. That is, patients’ involvement in obtaining information, decision making, and their resilience can explain why some patients do not experience adverse surgical results when pre-surgical psychosocial risk factors are present. Pre-surgical psychological evaluations should include examination of patient strengths in addition to psychosocial risk factors, so that treatments can be appropriately individualized and the most effective surgical results obtained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Whereas spine surgery (SS) is effective in providing pain relief and improving functioning for many patients (Mirza et al., 2013; Weinstein et al., 2006), some individuals fail to achieve desired results. A growing body of research indicates that psychosocial factors can predict some of these unfavorable outcome. Recent studies (Block, Ben-Porath, & Marek, 2013; Block, Marek, Ben-Porath, & Kukal, 2017; Block, Marek, Ben‐Porath, & Ohnmeiss, 2014; Marek, Block, & Ben-Porath, 2015, 2017) have utilized the Minnesota Multiphasic Personality Inventory-2-Restructured Form (MMPI-2-RF) (Ben-Porath & Tellegen, 2008/2011; Tellegen & Ben-Porath, 2008/2011) to examine psychosocial risk factors for reduced surgical outcome. Across these studies, several constructs have been found to consistently predict poorer outcomes.
The strongest overall predictor of diminished results from SS and spinal cord stimulation is demoralization, assessed on the MMPI-2-RF via the Demoralization scale (RCd). This construct is broadly defined by Ben-Porath (2012) as “a pervasive and affect-laden dimension of unhappiness and dissatisfaction with life (p. 46).” Scores on RCd, as well as one of its components, Self-Doubt (SFD), are correlated with poorer results at 6-month post-spine surgery and spinal cord stimulation, including lower return to work rates, greater use of opioid medication, less improvement in pain and in self-reported physical disability, as well as worse overall outcome and poorer satisfaction with surgical results (Block et al., 2013, 2014, 2017; Marek et al., 2015, 2017). Somatic Complaints, assessed by scale RC1 and its subscale score, Malaise (MLS), are also associated with less pain reduction and functional improvement after both types of surgical procedures (Block et al., 2017; Marek et al., 2015, 2017). Finally, poorer interpersonal functioning (primarily familial conflicts), assessed by the MMPI-2-RF scale FML, is also associated with diminished effectiveness of surgical procedures (Block et al., 2013, 2014, 2017; Marek et al., 2015, 2017).
Although research to date has focused on identification of psychosocial risk factors for poorer outcomes, other psychosocial factors could operate as strengths—ones which might be associated with improved surgical results. One such potential strength factor, patient activation, has recently been identified. Patient activation, which has been defined as the “extent to which patients are engaged and active in their own health care,” (Hibbard, Stockard, Mahoney, & Tusler, 2004) is measured by the Patient Activation Measure (PAM) (Hibbard et al., 2004). The domains evaluated by the PAM include the following: (1) belief that taking an active role in health is important; (2) having the confidence and knowledge to take action; (3) taking health-related action; (4) staying on course under stress. Higher PAM scores have been associated with better general health behaviors and treatment outcomes in a broad range of medical conditions (Remmers et al., 2009). Recently, PAM scores of SS patients were found to be significantly correlated with greater engagement in post-operative physical therapy and with greater post-operative functional improvement (Skolasky, Mackenzie, Wegener, & Riley, 2008, 2011).
The purpose of this study is to determine whether patient activation mediates some of the psychosocial factors previously found to be associated with reduced outcome of SS and spinal cord stimulation. In this study, patients referred for pre-surgical psychological evaluation completed both the MMPI-2-RF and the PAM. Outcome was assessed by patients’ self-ratings of pain reduction, functional ability, expectations, and satisfaction at approximately 6-month post-operation. Relying on prior research to guide MMPI-2-RF scales included in the analyses (Block et al., 2013, 2014, 2017; Marek et al., 2015, 2017), it was hypothesized that greater patient activation would mediate the association between higher pre-surgical MMPI-2-RF scale scores and post-surgical outcomes. The following scale scores on the MMPI-2-RF were used: Demoralization (RCd), Somatic Complaints (RC1), Low Positive Emotions (RC2), Dysfunctional Negative Emotions (RC7), MLS, SFD, Family Problems (FML), Negative Emotionality/Neuroticism-Revised (NEGE-r). These scales were selected because they have consistently yield significant correlations with both SS and spinal cord stimulator (SCS) outcomes (Block et al., 2013, 2014, 2017; Marek et al., 2015, 2017).
Method
Participants
Pre-operative Sample
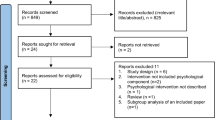
The initial sample comprised 1574 consecutive patients who presented for SS or a spinal cord stimulator. They were asked to participate in an outcome study at the time of their pre-surgical psychological evaluation. The outcome study aimed to identify pre-surgical risk factors associated with poor outcomes in these populations. Of the initial sample, 1276 patients gave consent to participate in the study. An additional 22 participants were excluded from further analyses because they produced invalid MMPI-2-RF protocols as outlined in the MMPI-2-RF Technical Manual (Tellegen & Ben-Porath, 2008/2011). There were no statistically significant differences between those who invalided the MMPI-2-RF and those who produced valid scores on the instrument. The remaining sample (n = 1254) included for the current study comprised 43.6% men and 56.3% women. The mean age of the sample was 50.41 years [standard deviation (SD) = 13.11] and the mean years of education was 13.45 years (SD = 2.88). Regarding surgery type, 61.7% underwent various conventional spine surgeries whereas 38.3% obtained a SCS. Of those who underwent conventional SS, 66.5% obtained a fusion, 10.8% obtained a Laminectomy/Discectomy/Decompression, 9.2% had an artificial disc replacement, 4.9% Discogram/Discography, and the other 8.6% had various other surgeries (e.g., Rhizotomy, Hybrid).
Post-operative Sample
Outcome data for 581 patients who received and mailed back packets containing post-operative measures were available. Patients returned outcome measures within 180 days (SD = 79.1) post-surgery and no demographic variables predicted attrition over time. The post-operative’s sample characteristics were similar to those reported above. In regard to gender, 40.6% were men and 59.4% were women. The mean age of the sample was 50.20 years (SD) = 13.03 and the mean years of education was 13.53 years (SD = 2.83). Regarding surgery type, 70.7% underwent various conventional spine surgeries, whereas 29.3% obtained a SCS.
Measures
Minnesota Multiphasic Personality Inventory-2-Restructured Form (MMPI-2-RF) (Ben-Porath & Tellegen, 2008/2011; Tellegen & Ben-Porath, 2008/2011)
The MMPI-2-RF is a 338-item test designed to assess personality and psychopathology. The items are scored across 9 validity scales 42 substantive scales. The test has published normative data for use in SS and SCS populations (Block & Ben-Porath, 2018) and has been validated for use in these settings (Block et al., 2013). The following scales were included in this study based on the findings of prior research (Block et al., 2017; Marek et al., 2015, 2017), because they have consistently been predictive of outcomes in these settings: Demoralization (RCd), Somatic Complaints (RC1), Low Positive Emotions (RC2), Dysfunctional Negative Emotions (RC7), MLS, SFD, FML, NEGE-r.
Oswestry Disability Index (ODI) (Fairbank, Couper, Davies, & O'Brien, 1980; Fairbank & Pynsent, 2000)
The ODI is a 10-item, self-report measure that assesses functional disability due to pain. The measure was administered at patients’ pre-surgical evaluation and at the short-term outcome. Total scores were derived by summing the raw scores, dividing the sum raw score by 50, and then multiplying by 100 to produce an index score representing percentage of functional disability. The measure demonstrates good reliability and validity in spine and SCS settings (Block et al., 2017; Fairbank & Pynsent, 2000; Fisher & Johnston, 1997; Marek et al., 2015). In the current sample, the ODI demonstrated good reliability coefficients at the pre-operative (α = .85; inter-item correlation = .40) and short-term (α = .90; inter-item correlation = .52) time points.
Patient Activation Measure-Short Form (PAM-13) (Hibbard, Mahoney, Stockard, & Tusler, 2005; Hibbard et al., 2004)
The PAM is a 13-item, self-report measure designed to assess patient’s engagement in treatment (termed activation). The PAM has yielded good reliability, criterion-related validity, and predictive validity in other samples (Hibbard et al., 2004, 2005). In the current sample, the measure yielded good internal consistency (α = .91) and good mean inter-item correlations (r = .46).
Pain and Spine Surgery Evaluation Survey (Marek et al., 2015)
This survey assesses pain, pain interference with lifestyle, emotional states, whether patients’ felt that the surgical procedure met their expectations, and whether they were satisfied with the procedure. The current investigation explored the responses on the pain item, the item assessing whether that the surgical procedure met their expectations, and the item assessing whether they were satisfied with the procedure. Patients were asked to rate their pain, whether the procedure met their expectation, and how satisfied they were with the outcome on three-dimensional scales ranging from 0 (Not at All) to 10 (Extremely).
Procedures
All consented patients underwent a pre-surgical psychological evaluation. This included a thorough review of medical records, a semi-structured interview with a clinical psychologist, psychological testing, and application of an algorithm designed to predict the prognosis of surgical candidates (Block, 2013). Patients were invited to consent to participate in the follow-up study prior to being evaluated. Participants were asked to consent to have data collected during three follow-up periods after their surgery: 3 months, 1, and 2 years post-operative. The study is ongoing, and only data collected at the time of the patients’ initial follow-up are used in this report. Participants were mailed packets that included the ODI and the Pain and Spine Surgery Evaluation Survey. The surgery date was recorded at the time of the psychological evaluation. However, because the surgery date was variable (e.g., due to rescheduling or cancelations), it was not uncommon for patients to receive their packets outside of the 3-month follow-up period. As reported above, a total of 581 patients received and mailed back these packets within 180 days (SD = 79.1) post-surgery and no demographic variables predicted attrition over time.
Statistical Analyses
Pearson Product-Moment Correlations were calculated between PAM scores, MMPI-2-RF scores, ODI scores, and Pain and Spine Surgery Evaluation Survey ratings and are reported in Table 1. Results were interpreted based on their magnitude using Hemphill’s (2003) classifications of < .20 indicating a small effect size, .20–.30 indicating a medium effect size, and > .30 indicating a large effect size. Only correlations within the medium effect size ranges or higher were interpreted.
To test whether PAM scores mediated the association between pre-surgical MMPI-2-RF scales and outcomes, bootstrapped mediation procedures were conducted (Hayes, 2013; Preacher, Rucker, & Hayes, 2007). Several models were tested. Abbreviated results are reported in Table 2 and a full statistical report is listed in the Online Supplemental Table 1. All beta weights reported are unstandardized. If 0 is not contained in the 95% confidence interval (CI), the coefficients reported are statistically significant at p < .05. A test of mediation was considered statistically significant if the indirect effect beta weights did not contain zero within their associated 95% CI derived from 5000 bootstrap resamples. Full Information Maximum Likelihood was used to handle missing data across time (Enders & Bandalos, 2001). Mplus version 8 was used for the mediation analyses and correlations were calculated using IBM SPSS version 24. The study was approved by Kent State University’s Institutional Review Board.
Results
Correlations
Table 1 lists correlations between PAM scores, MMPI-2-RF scores, pain ratings, ODI scores, and Pain and Spine Surgery Evaluation Survey ratings. Looking first at correlations associated with PAM scores, all pre-surgical MMPI-2-RF scores were modestly to substantially negatively associated pre-surgical PAM scores. Moreover, pre-surgical PAM scores were modestly associated with lower post-operative ODI scores and higher expectation and satisfaction scores. Interestingly, pre-surgical PAM scores were not associated with pre-operative pain levels when assessed at the same time prior to surgery.
Higher MMPI-2-RF scale scores on Demoralization, Somatic Complaints, MLS, and SFD were associated with higher post-surgical pain ratings. In regard to correlations between the pre-surgical MMPI-2-RF scales and pre-surgical ODI scores, higher scores on Demoralization, Somatic Complaints, Low Positive Emotions, Dysfunctional Negative Emotions, MLS, SFD, and NEGE-r were modestly related to higher pre-surgical ODI scores. The pattern and strength of the associations between pre-surgical MMPI-2-RF scale scores and post-operative ODI scores were similar with one exception: Dysfunctional Negative Emotions was not meaningfully associated with postoperative ODI scores. The MLS scale was also modestly and negatively associated with expectation and satisfaction scores.
Mediation Analyses
Table 2 lists summaries of the mediation analyses for each of the four outcome measures. A full statistical report of the mediation analyses is reported in Online Supplemental Table 1. In mediation analyses where post-operative pain and ODI scores were used as the dependent variable, pre-surgical pain and ODI scores, respectively, were entered in the model as well. Pre-surgical MMPI-2-RF scale scores were used as independent variables and pre-surgical PAM scores were used as the mediator. As an example, the first block of analyses outlined in Supplemental Table 1 uses post-operative ODI scores as the dependent variable, Demoralization (RCd) as the independent variable, and PAM scores as the mediator variable. The a path illustrates that the higher the pre-surgical score on RCd, the lower the pre-surgical score on the PAM (B = − .31). The b path suggests that higher pre-surgical PAM scores are predictive of lower post-operative ODI scores (B = − .77). The c path suggests that the higher the pre-surgical RCd score, the higher the post-operative ODI scores were (B = .80; without adding PAM scores to the model). The c′ path also suggests that higher pre-surgical RCd scores predict higher post-operative ODI scores (B = .53; while controlling for the effect of PAM scores on post-operative ODI scores), but that its predictive strength weakens when PAM scores are included in the model. To test whether the aforementioned weakened association was statistically significant, a test of indirect effects is reported (c–c′). Because 0 is not in the 95% CI, it can be concluded that statistically significant meditation is occurring. Thus, patients who are feeling demoralized prior to surgery tend to report greater functional disability around 180 days (SD = 79.1) postoperatively; however, this association is mediated when the patient also reports a high amount of engagement in treatment. By and large, there were statistically significant mediation paths across most models with a few exceptions. No statistical mediation effects were evidenced when using post-operative pain ratings as a dependent measure. PAM scores did not mediate the relationship between higher pre-surgical MLS scores and patients reporting that surgical results were not meeting their expectations. PAM scores also did not mediate the association between higher pre-surgical Somatic Complaints scores and patients reporting poorer satisfaction with surgical results.
Discussion
The current results indicate that poorer SS and SCS results are associated with previously identified psychosocial risk factors assessed by the MMPI-2-RF. Further, in line with the findings of Skolasky et al. (2011) higher pre-surgical levels of patient activation assessed by the PAM are associated with improved surgery results. Additionally, PAM scores measured prior to surgery negatively correlated with the MMPI-2-RF scales, implying that patients who tend to be more active in their healthcare also evidence lower psychosocial risk factors. Finally, the unique finding of this study is that patient activation mediates the association between psychosocial risk factors and surgery results, such that more activated patients did not show the same detriment in outcome associated with the psychological risk factors as did those patients who were not as positively activated.
Associations between MMPI-2-RF scales and other criteria have been reported in prior research (Block et al., 2013, 2014, 2017; Marek et al., 2015, 2017) and are presented as a combined sample here. Patients who are demoralized, pain-focused, experience exhaustion, and are unable to experience positive emotion (all characteristics assessed by the MMPI-2-RF scales examined in this study) are unlikely to have the motivation, energy, and resilience necessary to be strongly engaged in maintaining and improving their health and fitness. On the other hand, results indicated that patients who are more active in their healthcare tended to have more favorable outcomes. This is consistent with research both within and outside SS population. Patients who tend to be more active in their healthcare are less likely to require rehospitalization, are more adherent to post-surgical care instructions, and are properly taking (or weaning off) pain medications (Hibbard et al., 2004, 2005; Skolasky et al., 2008, 2011). The finding of the current investigation is that patient activation mediated the association between psychosocial risk factors and outcome. It follows that patients who may present as being demoralized or report higher than average Somatic Complaints may not exhibit a diminished outcome if they are at the same time more oriented, autonomous, and active in taking care of their health.
These results have several implications for both clinical practice and research. First, the current results suggest that previous research on pre-surgical psychological evaluation may have been too narrowly focused. By exclusively examining psychosocial risk factors, previous studies have ignored patient strengths and positive characteristics, thus possibly underestimating patients’ abilities to achieve good outcomes. Other medical conditions in which pre-surgical psychological evaluation is utilized often include evaluation of positive patient characteristics similar to those assessed by the PAM (Block & Sarwer, 2013). For example, in developing guidelines for psychosocial evaluation of bariatric patients endorsed by the American Society for Metabolic and Bariatric Surgery, Sogg, Lauretti, and West-Smith (2016) suggest examination of persistence, which was defined as “an ability to continue to pursue one’s goals despite immediate setbacks and frustration” (p. 737), as well as exploring patients’ understanding of bariatric procedure risk, benefits and requirements. Sogg et al. (2016) suggest that examining such factors may lead to improved outcomes and may provide new avenues toward optimizing surgical results. Similarly, in the evaluation of candidates for bone marrow and stem cell transplant, Austin and Rini (2013) recommend identifying patients’ “health literacy,” suggesting that patients who are equipped with good information about transplant care and adhere to it are more likely to actively practice good self-care, monitor symptoms appropriately, and experience less distress in regards to their illness and recovery. It is perhaps, for similar reasons, that higher levels of patient activation, as assessed by PAM, have been found to be associated with improved health outcomes across a broad range of medication conditions, including following a low fat diet in patients with high cholesterol, routinely exercising in patients with arthritis, and testing for, and control of hemoglobin A1C in diabetics (Remmers et al., 2009). Considered together, such findings indicate that the accuracy of pre-surgical evaluations of SS and SCS candidates may be improved by assessing patient activation and perhaps other indicators of positive patient engagement with their health status.
Indeed, patient activation is not the only positive factor that may have an impact on SS results. Other positive factors have been explored in the context of chronic pain treatment, including resilience (Sturgeon & Zautra, 2010) positive pain coping strategies such as mindfulness and acceptance (McCracken & Vowles, 2014), and social support (Cano, 2004). The current results point to the need for additional research to explore the potential impact of such psychological strengths on surgery results even in patients who have minimal risk factors, as this may lead to predictions of better outcomes and better targeted treatments.
Because higher patient activation scores can mediate psychosocial risk factors, it seems likely that surgery results may be improved by working to increase patient activation: assisting patients in obtaining information about their conditions; helping them to question themselves and their physicians about treatments; improving their overall health and fitness; and coaching patients to be resilient through difficult periods during recovery. The current results found that higher PAM scores prior to surgery are associated with lower levels of adverse psychological factors assessed by the MMPI-2-RF. Thus, future studies should focus on evaluating the effectiveness of treatments that increase activation for those whose psychological test reveals them to be at greatest risk for poor surgery results.
Although PAM scores mediated many of the associations between pre-surgical MMPI-2-RF scores and outcomes in this study, they did not mediate associations with patients’ reported pain levels after surgery. There are a few explanations for these negative findings. First, it could be that the pain measure used in this study, an 11-point scale of average pain, is simply too broad, requiring patients to examine and quantify the fluctuating subjective experience of pain across time into a single rating score. Multiple pain reports, examined over discrete periods, might yield better differentiated results. Alternatively, it may be that patient activation exerts its impact more directly on the behavioral outcomes of surgery, as assessed by the ODI, compared to the more subjective experience of pain. There were also a few other instances where PAM scores did not mediate associations between pre-surgical MMPI-2-RF scores and outcomes. PAM scores did not mediate the association between MLS and surgery meeting patient expectations. Higher scores on RC1 and MLS are associated with patients reporting numerous physical health problems including, but not limited to, pain, headaches, fatigue, low energy, and sexual dysfunction. To some extent, it is possible that patients with higher activation, who have a history of strong engagement in promoting their own health and wellness may be less able to accept that surgery will not completely overcome functional limitations or achieve total pain relief. A similar explanation likely explains why mediation was not observed when examining RC1 and patients feeling satisfied with their surgical outcome. At any rate, because PAM scores also mediate the impact of psychosocial risk factors on satisfaction with surgery results, improvement in the ability to function may be more important to patients than is reduction of pain.
These results have some limitations that must be noted. First, we combined candidates for SS and SCS candidates. Although our previous research has reported similarities of MMPI-2-RF scales and their associations with the outcomes in the two surgery types (Block et al., 2013, 2014, 2017; Marek et al., 2015, 2017), the mediation effects may operate differently for the two patient groups. Unfortunately, there was not enough statistical power to test for differential effects at this juncture. Further research with a larger number of participants will better illuminate this point. Second, the outcome measures used in this study were all self-report. More objective outcome measurement, such as behavioral observation or digital quantification of activity levels, medication use, return to work, etc., may reveal different results.
Conclusions
Extensive research indicates that certain psychosocial factors are associated with negative outcomes of SS and spinal cord stimulation. The current results indicate that patient activation—patient’s involvement in obtaining information, decision making, and resilience during times of stress—mediates such adverse effects. Pre-surgical psychological evaluations should include examination of patient strengths in additional to psychosocial risk factors, so that treatments can be appropriately individualized and the most effective surgical results obtained.
References
Austin, J. E., & Rini, C. (2013). Bone marrow and stem cell transplant. Washington, DC: American Psychological Association.
Ben-Porath, Y. S. (2012). Interpreting the MMPI-2-RF (1 ed.). Minneapolis, MN: University of Minnesota Press.
Ben-Porath, Y. S., & Tellegen, A. (2008/2011). The Minnesota multiphasic personality inventory-2 restructured form (MMPI-2-RF): Manual for administration, scoring, and interpretation. Minneapolis, MN: University of Minnesota Press.
Block, A. R. (2013). Spine surgery. In A. R. Block & D. B. Sarwer (Eds.), Presurgical psychological screening: Understanding patients, improving outcomes (pp. 43–60). Washington, DC: APA Press.
Block, A. R., & Ben-Porath, Y. S. (2018). MMPI-2-RF user’s guide for the spine surgery and spinal cord stimulator candidate interpretive reports. Minneapolis, MN: University of Minnesota Press.
Block, A. R., Ben-Porath, Y. S., & Marek, R. J. (2013). Psychological risk factors for poor outcome of spine surgery and spinal cord stimulator implant: A review of the literature and their assessment with the MMPI-2-RF. The Clinical Neuropsychologist, 27(1), 81–107. https://doi.org/10.1080/13854046.2012.721007.
Block, A. R., Marek, R. J., Ben-Porath, Y. S., & Kukal, D. (2017). Associations between pre-implant psychosocial factors and spinal cord stimulation outcome: Evaluation using the MMPI-2-RF. Assessment, 24(1), 60–70. https://doi.org/10.1177/1073191115601518.
Block, A. R., Marek, R. J., Ben-Porath, Y. S., & Ohnmeiss, D. D. (2014). Associations between minnesota multiphasic personality inventory-2-restructured form (MMPI-2-RF) scores, workers’ compensation status, and spine surgery outcome. Journal of Applied Biobehavioral Research, 19(4), 248–267.
Block, A. R., & Sarwer, D. B. (2013). Introduction. In A. R. Block & D. B. Sarwer (Eds.), Presurgical psychological screening: Understanding patients, improving outcomes (1st ed., pp. 3–24). Washington, DC: American Psychological Association.
Cano, A. (2004). Pain catastrophizing and social support in married individuals with chronic pain: The moderating role of pain duration. Pain, 110(3), 656–664.
Enders, C. K., & Bandalos, D. L. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457.
Fairbank, J. C., Couper, J., Davies, J. B., & O’Brien, J. P. (1980). The Oswestry low back pain disability questionnaire. Physiotherapy, 66(8), 271–273.
Fairbank, J. C., & Pynsent, P. B. (2000). The Oswestry Disability Index. Spine (Phila Pa 1976), 25(22), 2940–2952 (discussion 2952).
Fisher, K., & Johnston, M. (1997). Validation of the Oswestry low back pain disability questionnaire, its sensitivity as a measure of change following treatment and its relationship with other aspects of the chronic pain experience. Physiotherapy Theory and Practice, 13(1), 67–80.
Hayes, A. (2013). Introduction to mediation, moderation, and conditional process analysis. A regression-based approach. New York: Guilford. ISBN 1609182308.
Hemphill, J. F. (2003). Interpreting the magnitudes of correlation coefficients. American Psychologist, 58(1), 78–80. https://doi.org/10.1037/0003-066X.58.1.78.
Hibbard, J. H., Mahoney, E. R., Stockard, J., & Tusler, M. (2005). Development and testing of a short form of the patient activation measure. Health Services Research, 40(6p1), 1918–1930.
Hibbard, J. H., Stockard, J., Mahoney, E. R., & Tusler, M. (2004). Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39(4p1), 1005–1026.
Marek, R. J., Block, A. R., & Ben-Porath, Y. S. (2015). The Minnesota multiphasic personality inventory-2-restructured form (MMPI-2-RF): Incremental validity in predicting early postoperative outcomes in spine surgery candidates. Psychological Assessment, 27(1), 114–124. https://doi.org/10.1037/pas0000035.
Marek, R. J., Block, A. R., & Ben-Porath, Y. S. (2017). Validation of a psychological screening algorithm for predicting spine surgery outcomes. Assessment. https://doi.org/10.1177/1073191117719512.
McCracken, L. M., & Vowles, K. E. (2014). Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. American Psychologist, 69(2), 178.
Mirza, S. K., Deyo, R. A., Heagerty, P. J., Turner, J. A., Martin, B. I., & Comstock, B. A. (2013). One-year outcomes of surgical versus nonsurgical treatments for discogenic back pain: A community-based prospective cohort study. The Spine Journal, 13(11), 1421–1433.
Preacher, K. J., Rucker, D. D., & Hayes, A. F. (2007). Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research, 42(1), 185–227.
Remmers, C., Hibbard, J., Mosen, D. M., Wagenfield, M., Hoye, R. E., & Jones, C. (2009). Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? The Journal of Ambulatory Care Management, 32(4), 320–327.
Skolasky, R. L., Mackenzie, E. J., Wegener, S. T., & Riley, L. H. 3rd (2008). Patient activation and adherence to physical therapy in persons undergoing spine surgery. Spine, 33(21), E784–E791. https://doi.org/10.1097/BRS.0b013e31818027f1.
Skolasky, R. L., Mackenzie, E. J., Wegener, S. T., & Riley, L. H. 3rd (2011). Patient activation and functional recovery in persons undergoing spine surgery. J Bone Joint Surg Am, 93(18), 1665–1671. https://doi.org/10.2106/JBJS.J.00855.
Sogg, S., Lauretti, J., & West-Smith, L. (2016). Recommendations for the pre-surgical psychosocial evaluation of bariatric surgery patients. Surgery for Obesity and Related Diseases. https://doi.org/10.1016/j.soard.2016.02.008.
Sturgeon, J. A., & Zautra, A. J. (2010). Resilience: A new paradigm for adaptation to chronic pain. Current Pain and Headache Reports, 14(2), 105–112.
Tellegen, A., & Ben-Porath, Y. S. (2008/2011). The Minnesota multiphasic personality inventory-2 restructured form (MMPI-2-RF): Technical manual. Minneapolis. Minneapolis, MN: University of Minnesota Press.
Weinstein, J. N., Tosteson, T. D., Lurie, J. D., Tosteson, A. N., Hanscom, B., Skinner, J. S., … Deyo, R. A. (2006). Surgical vs nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA, 296(20), 2441–2450.
Funding
This study was partially funded through a grant from the University of Minnesota Press to the first author, Andrew Block.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yossef Ben-Porath is a paid consultant to the MMPI-2-RF publisher, the University of Minnesota and Distributor, Pearson. As co-author of the MMPI-2-RF, he receives royalties on sales of the test. Andrew R. Block and Ryan J. Marek declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Block, A.R., Marek, R.J. & Ben-Porath, Y.S. Patient Activation Mediates the Association Between Psychosocial Risk Factors and Spine Surgery Results. J Clin Psychol Med Settings 26, 123–130 (2019). https://doi.org/10.1007/s10880-018-9571-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-018-9571-x