Abstract
Purpose
New-generation anesthesia machines administer inhalation anesthetics and automatically control the fresh gas flow (FGF) rate. This study compared the administration of minimal flow anesthesia (MFA) using the automatically controlled anesthesia (ACA) module of the Mindray A9 (Shenzhen, China) anesthesia machine versus manual control by an anesthesiologist.
Methods
We randomly divided 76 patients undergoing gynecological surgery into an ACA group (Group ACA) and a manually controlled anesthesia group (Group MCA). In Group MCA, induction was performed with a mixture of 40–60% O2 and air with a 4 L/min FGF until the minimum alveolar concentration (MAC) reached 1. Next, MFA was initiated with 0.5 L/min FGF. The target fraction of inspired oxygen (FiO2) value was 35–40%. In Group ACA, the MAC was defined as 1, and the FiO2 was adjusted to 35%. Depth of anesthesia, anesthetic agent (AA) consumption, time to achieve target end-tidal AA concentration, awakening times, and number of ventilator adjustments were analyzed.
Results
The two groups showed no statistically significant differences in depth of anesthesia or AA consumption (Group ACA: 19.1 ± 4.9 ml; Group MCA: 17.2 ± 4.5; p-value = 0.076). The ACA mode achieved the MAC target of 1 significantly faster (Group ACA: 218 ± 51 s; Group MCA: 314 ± 169 s). The number of vaporizer adjustments was 15 in the ACA group and 217 in the MCA group.
Conclusion
The ACA mode was more advantageous than the MCA mode, reaching target AA concentrations faster and requiring fewer adjustments to achieve a constant depth of anesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction and purpose
The low-flow anesthesia (LFA) technique uses a semi-closed rebreathing system in which at least 50% of exhaled air, after absorbing carbon dioxide, wholly or partially returns unused anesthetic gases for the patient’s inspiration after being mixed with a specified amount of fresh gas [1, 2]. Baker and Simionescu (1984) define LFA as a rate of 0.5–1.0 L/min and minimal flow anesthesia (MFA) as a rate of 0.25–0.5 ml/min [3].
Modern anesthesia machines use two distinct anesthesia management modules. The first conventional method is manually controlled anesthesia (MCA), and the second is automatically controlled anesthesia (ACA). In the MCA technique, anesthesiologists manually regulate inspired/expired gas concentrations and FGF during general anesthesia. This requires an anesthetist’s expertise and attention, mainly to avoid problems such as those involving the differences in gas concentration settings on the anesthesia machine and respiratory system and the delay between FGF changes and the end-tidal fraction of the anesthetic agent (Et-AA) [4]. The principal risks of LFA administered with MCA are accidental hypoxia and low inhaled doses of anesthetic agent (AA) [5]. During the induction and maintenance phases of anesthesia, the use of halogenated agents with the lowest possible fresh gas flow (FGF) rates is recommended, and a low flow technique is now aimed at achieving FGF, ideally a minimum flow of < 0.5 L/min [6]. When targeting these, it is important to protect both the workload on the anesthesiologist and patient safety. Efforts are being made to facilitate anesthesia administrations with modern anesthesia workstations and to create a greener operating room environment. This aims to simplify anesthesia procedures and create a more environmentally friendly operating room environment.
Our study examined the ACA and MCA methods in MFA to compare hemodynamic parameters, depth of anesthesia, time to reach target AA concentration, recovery time, anesthesiologist workload, and consumption data on the AA. We hypothesized that anesthesia administered with the ACA method would reach target AA values more quickly, at a lower cost, and with less workload than that administered with the MCA method and with equal anesthetic depth.
2 Materials and methods
After obtaining approval from the Sakarya University Faculty of Medicine Clinical Research Ethics Committee (no. 102,934; 07 February 2022), we studied 76 consecutive patients admitted to the operating room for elective gynecological surgery with an open abdominal technique and general anesthesia at Sakarya University Training and Research Hospital. The inclusion criteria were patients 18–65 years of age with an American Association of Anesthesiologists (ASA) classification of I–III and an expected surgery duration of longer than one hour. The exclusion criteria included contraindications to any of the AAs used, a body mass index (BMI) above 30, and neurological disorders. All the study’s patients provided written informed consent at least one day before the surgery. The clinical trial number is NCT05554263 (https://clinicaltrials.gov).
As premedication, midazolam (0.03 mg/kg) was administered intravenously 30 min before the operation. After monitorization, an epidural catheter (Premium One epidural anesthesia kit, 18 G, Egemen, Turkey) was inserted through the lower thoracic intervertebral space (T10–12) in all patients. After applying an epidural test dose (3 ml 1.5% lidocaine) to confirm that the catheter was not in the intravascular or subarachnoid area, 8–10 ml of a mixture prepared with 0.125% bupivacaine and 5 mcg/ml fentanyl for preemptive analgesia was administered through the epidural catheter before surgery. Analgesia was maintained by an hourly intraoperative epidural injection.
All the patients were preoxygenated with 80% inspiratory O2 via a respiratory face mask with a flow rate of 6 L/min for 3 min. The patients were intubated for the induction of anesthesia when adequate muscle relaxation had been achieved following the intravenous administration of lidocaine (1 mg/kg), propofol (2–3 mg/kg), rocuronium bromide (0.6–1.2 mg/kg), and fentanyl (1 mcg/kg). We used the same anesthesia machine for all patients (Mindray A9, Shenzhen, China). After the patients were intubated, they were segregated into a manually controlled anesthesia group (Group MCA; n = 38) and an automatically controlled anesthesia group (Group ACA; n = 38).
The Mindray A9’s manual mode was used in Group MCA. The patients’ demographic data were recorded on the anesthesia machine, the FiO2 alarm was set to 32%, and anesthesia was initiated. Measurements began when the patient was connected to the ventilator, which was preset to a 40–60% O2-air mixture and FGF of 4 L/min; the sevoflurane vaporizer was set to 2.5%. The FGF was reduced to 0.5 L/min and the sevoflurane was set at 4% to maintain target minimum alveolar concentration (MAC), after reaching the target value of MAC (1 MAC).The initial target value of 1 MAC was confirmed, and the AA concentration was adjusted according to SEDLine™ (Massimo Corporation, Irvine, CA, USA) monitoring (patient state index [PSI] value: 25–50). All these adjustments were made by an assigned anesthesiologist who was not involved in the study and who was experienced in MFA. The O2 concentration was adjusted to be 35–40% FiO2 throughout the operation. Fifteen minutes before the end of the surgical procedure, only the sevoflurane vaporizer was turned off without changing the FGF. At the end of the surgical procedure, the FGF was increased to 4 L/min and the O2 concentration raised to 80%; the patients were antagonized with sugammadex (4–8 mg/kg) and extubated when they responded to verbal stimuli. The anesthesiologist was instructed to avoid changes in flow rates. In the event of undershooting the 35% inspiratory oxygen concentration target, the anesthesiologist increased the inspiratory oxygen fraction; the anesthesiologist reduced the FiO2 in the event of overshooting the 40% inspiratory oxygen concentration target.
In Group ACA, the target values (FiO2: 35%; Et-AA concentration: 1 MAC; FGF: 0.5 L/min) were set once using the Mindray A9’s autocontrol mode. After the target value of MAC 1 was reached, the anesthesia machine automatically reduced the FGF to 0.5 L/min. During the operation, target AA concentrations were manually adjusted by an assigned anesthesiologist who was not involved in the study and who was experienced in MFA, maintaining PSI values of 25–50. The sevoflurane vaporizer was turned off approximately 15 min before the end of the surgical procedure, and the FGF continued at 0.5 L/min in autocontrol mode until the end of the surgery. Then, the FGF was increased to 4 L/min and the O2 concentration raised to 80%; the patients were antagonized with sugammadex (4–8 mg/kg) and extubated when they responded to verbal stimuli.
The AA concentration was adjusted so that the PSI value was between 25 and 50 in both groups. When the PSI value was above 50, the MAC value was increased by 0.1, and when it fell below 25, the MAC value was decreased by 0.1. When a decrease of more than 20% was observed in the mean arterial pressure value compared to the baseline (and when the PSI value was within the target range), 5 mg of ephedrine was given.
The anesthesiologist’s number of inspiratory oxygen fraction adjustments and changes in vaporizer setting to achieve and maintain target values were recorded as manual adjustments in the protocol and counted by investigators (who were constantly in the operating room).
The researchers recorded the demographic data of all the patients and measured their MAC, FiO2, Et-CO2, heart rate, systolic arterial pressure, mean arterial pressure, diastolic arterial pressure, peripheral oxygen saturation (SpO2), and PSI values. The researchers also recorded the duration of intraoperative vaporizer (the period after intubation from when the patient was connected to the anesthesia machine and the vaporizer turned on to when the vaporizer was turned off), anesthetic gas (air, O2) consumption, sevoflurane consumption and cost, time to reach the MAC 1 target value, and awakening time (the period from the closure of the vaporizer to extubation). At the end of the anesthesia, the amount of AA consumed per case was recorded as the total consumption data, and the hourly consumption was calculated manually as an average.
2.1 Statistical analysis
The data were statistically analyzed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 20.0 for Windows) program. The normality of continuous data was evaluated using the Shapiro-Wilk test. The Pearson’s chi-square test was used to compare the qualitative data, and the data were expressed as numbers and percentages. In comparing the quantitative data, Student’s t-test was used for those with normal distribution, and the data were expressed as mean and standard deviation (mean ± SD). In the analysis of variables that did not show normal distribution, the Mann Whitney U test was used, and the data were given as a median and interquartile range. All tests used a statistical significance level of p = .05.
2.2 Power analysis
A preliminary study conducted to calculate the sample size indicated that 34 patients were required in each group to verify a 5% difference in the AA consumption amounts between the groups (alpha = 0.05, beta = 0.80). Each group included 38 patients to tolerate a 10% data loss during the study period.
3 Results
Our study recruited 76 patients (38 in Group MCA and 38 in Group ACA). The two groups had similar demographic data and duration of surgery and anesthesia (Table 1).
When the PSI values between both groups were compared, it was observed that they were similar at all times (Fig. 1).
We compared sevoflurane delivery time and air and O2 consumption and found no statistically significant difference (p = .285, p = .182, p = .065, respectively). We also compared the consumption and cost of sevoflurane between the groups. Group MCA consumed 17.2 ± 4.5 ml of sevoflurane with a cost of 78.98 ± 21.07 TL, whereas Group ACA consumed an average of 19.1 ± 4.9 ml of sevoflurane with a cost of 87.98 ± 22.5 TL, but the difference was not statistically significant (p = .076) (Table 2). Analysis of the hourly sevoflurane consumption was not significantly different between groups (p = .249). MAC 1 was reached 30% faster in the ACA group compared to the MCA group. (p = .001). There was no difference between the groups in terms of awakening time (p = .266) (Table 2). The average total number of adjustments made per case, both FiO2 and AA, was nearly zero in the ACA group, compared to 10 in the MCA group (Table 2).
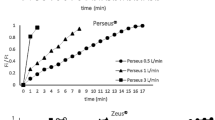
According to the PSI values obtained for all 38 patients in Group MCA, the number of adjustments made on the vaporizer was consistently 217 across all time points. In contrast, in Group ACA, the number of adjustments made for AA for all 38 patients was 15, which was statistically lower (median 6 [4–7]; median 0 [0–0] respectively; p < .001). When the distribution of adjustments for AA in Group MCA was examined over time, it was observed that the adjustments were most frequently made at the 5th minute by the anesthetist, followed by the 30th and 60th minutes (Fig. 2).
4 Discussion
In this study, we compared the MCA and ACA methods for MFA. While there was no difference in depth of anesthesia, air-O2 consumption, sevoflurane consumption and cost, or awakening time, we observed that the time to reach the target AA concentration was shorter using the ACA method and the anesthesia workload was significantly reduced.
Differences in the technology and working principles of new anesthesia machines have entered our daily lives with the technology’s development. The fully automated system ushers in the era of ACA in which anesthetists set targets (such as Et-AA concentration) [7]. The era of Automated Controlled Anesthesia (ACA), where anesthetists set specific targets such as Et-AA concentration, is ushered in by fully automated systems [7]. Among the anesthesia workstations utilizing automatic control systems, the minimal fresh gas flow varies: GE Healthcare Aisys Carestation is set at 500 ml/min, Dräger Zeus (CCA - Closed Circuit module), while both Mindray A9 and Maquet Flow-i are set at 300 ml/min. This variability underscores the importance of ongoing advancements in anesthesia workstation technology. These advancements play a crucial role in improving efficiency and optimizing resource utilization in clinical settings. Our study used the Mindray A9, which we have not previously encountered in the literature and which has a newly developed ACA mode.
Because the target MAC values are determined by the anesthetist via automated anesthesia control and are automatically adjusted by the machine during anesthesia, machines are predicted to provide a more stable depth of anesthesia than manual methods [8]. In our study, we determined the target AA concentration as MAC 1, adjusted the target MAC value according to the intraoperative PSI values, and concluded that both methods provide a stable depth of anesthesia; this result is similar to that of previous studies [9, 10].
Inhalation AAs can be costly, and FGF speeds and vaporizer settings represent AA costs and potential cost-saving targets. While automated control anesthesia aims to provide more stable anesthesia, it is also expected to consume less AA, but many different results have been reported in the literature due to varying methodologies related to the consumption comparison analysis of MFA and MCA administration.
In their study, Lortat-Jacob et al. investigated the clinical benefits and economic effects of the Zeus anesthesia machine and ACA and MCA methods; they enrolled 80 patients who underwent major abdominal and urological surgery lasting longer than one hour. The study concluded that the target-controlled technique reduced O2 and desflurane consumption by 65% and nitrous oxide (N2O) consumption by 80% [11].
Singaravelu and Barclay used a GE Aisys anesthesia machine and included a more comprehensive patient group in terms of anesthesia duration. The inhalation anesthetic consumption was 27 (21–33) ml/h in the ACA group and 45 (29–62) ml/h in the MCA group. Their results showed that using ACA decreased the consumption of inhalation anesthetics by 40–55% over similar anesthesia times [12]. Similar studies in the literature report that the use of automated modules reduces AA consumption [9, 11,12,13,14]. Contrary to these studies, De Cooman et al.’s study with the Zeus anesthesia machine found that inhalation AA (desflurane + N2O) consumption increased with ACA [15]. Other studies in the literature have shown the ACA and MCA methods to have similar AA consumption [4, 16].
Our study used the Mindray A9, a different anesthesia machine than used in other studies. When we calculated the hourly cost of sevoflurane, we observed that it was 36 (33–41) TL/h with ACA and 38 (36–44) TL/h with MCA, so sevoflurane consumption and cost were similar in both groups. We thought that using similar FGFs with both methods and AA administration times effectively achieved these results.
Many different results have been reported regarding the time required to reach the target AA values with MCA methods versus automated control anesthesia. Lugancelo et al. established the FGF as 1 L/min and concluded that patients reached the target Et-AA faster with the MCA method, but they attributed this result to the fact that the vaporizer was completely open during the initial period of anesthesia in the MCA group [4]. An in vitro anesthesia study compared the automated module of the Zeus anesthesia machine with the manual modes of the Primus and Zeus machines using different FGFs and concluded that ACA reached the target values faster [14]. Wetz et al. observed that an ACA group required 178 s to reach the target Et-sevoflurane concentration of 1.2–1.4%, whereas an MCA group required 275 s, so the target values were reached significantly faster in the ACA group [16]. In other research, Struys et al. and Wetz et al. observed that the target Et-AA concentrations determined by ACA were reached more rapidly [17, 18]. In our study, we reached the conclusion that achieving the target AA concentration required 314 s using the MCA, whereas only 218 s were required in the ACA. Notably, we observed that the ACA method allowed reaching the target Et-AA concentrations 30% faster compared to the MCA method. In MFA, there is a notable reduction in the concentration of anesthetic gas released into the atmosphere from waste gas systems [14]. The administration of MFA using modern and advanced anesthesia machines holds significant promise for diminishing the contribution of anesthetic gases to environmental pollution [19]. The primary strategy for minimizing vapor consumption involves reducing the FGF throughout the case. This reduction in FGF at each stage of inhalational anesthesia effectively decreases total vapor consumption. This not only enhances efficiency but also contributes to a more environmentally sustainable and cost-effective approach to anesthesia management [20].
Factors affecting awakening time include fat solubility of AA, AA concentration, consumption time of inhalation anesthetics, the patient’s alveolar ventilation level, intraoperative analgesic drugs, patient characteristics, and the anesthesiologist’s awakening technique. Supporting previous studies, our study found no difference between the groups’ awakening times from the closure of the vaporizer to extubation [4, 11].
The administration of MFA using the MCA method involves continually adjusting the inspired and exhaled gas concentrations and the vaporizer, which occupies both the anesthesiologist’s workload and attention [8]. The workload savings provided by the ACA method can be even more significant when the anesthesiologist’s attention is diverted (e.g., by critical events or crises) [4, 17]. Lortat-Jacob et al.’s study found that, with MCA, the anesthesiologist should adjust the settings every four minutes on average. In contrast, with ACA, they should be changed every 10 min [11]. In our study, we observed that the initial 15 min of anesthesia in 38 patients undergoing MCA represented the phase requiring the most adjustments by the anesthesiologist. The average number of adjustments made was 6 for Et-AA and 4 for FiO2. In contrast, for 38 patients using ACA, we found an average of nearly 0 adjustments for Et-AA and 0 adjustments for FiO2. We had predicted that this would facilitate MFA administration through a more clinically acceptable workload with the ACA method and that automated MFA administration could be used more widely in this way. The most straightforward and conventional strategy to minimize the frequency of anesthesiologist interventions is undeniably the maintenance of a high fresh gas flow. This approach, while effective, raises questions about the economic and ecological aspects, particularly in terms of AA wastage. One significant advantage of automated control lies in its user-friendly nature, simplifying MFA administration and likely fostering increased adherence to MFA policies over time. Indeed, in a study monitoring FGF rates in a section of a New Zealand hospital, Kennedy R. and French observed that the introduction of automated Aisys systems initially increased average FGF rates to 1.5 L/min. However, after 12 months, the rates decreased to 1.09 L/min. The reduction in the number of necessary adjustments not only simplifies the anesthesia process but also, due to its economic and environmental benefits, may promote the increased utilization of automated MFA systems [21].
The most significant limitation of our study is that the patient’s uptake of AAs cannot be given in the Mindray A9 device. For this reason, the purchase amount was not included in our account. In addition, hourly AA consumption data could not be obtained with the Mindray A9. Therefore, the amount of AA consumed per case at the end of anesthesia was taken as the total consumption data, and hourly consumption was calculated manually as an average.
5 Conclusion
The observations and results of our study indicate that the ACA method is more advantageous than the manual mode in terms of the number of adjustments required to achieve a constant depth of anesthesia and that the target values are reached faster. Auto-controlled anesthesia reliably contributes to precision anesthesia, preventing the anesthesiologist from wasting time with continual vaporizer and FiO2 adjustments. Moreover, it allows anesthesiologist to devote more time to the patient. In this way, while creating a safer environment for the patient, it also significantly reduces the anesthesiologist’s workload.
Data availability
Not applicable.
References
Baum JA, Aitkenhead AR. Low-flow anaesthesia. Anaesthesia. 1995;(50 Suppl):37–44. https://doi.org/10.1111/j.1365-2044.1995.tb06189.x.
Baum JA, Nunn G. Low flow anaesthesia: the theory and practice of low flow, minimal flow and closed system anaesthesia. 2nd ed. Boston: Butterworth-Heinemann; 2001.
Simionescu R. Safety of low flow anaesthesia. Circular. 1986;3:7–9.
Lucangelo U, Garufi G, Marras E, Ferluga M, Turchet F, Bernabè F, Comuzzi L, Berlot G, Zin WA. End-tidal versus manually-controlled low-flow anaesthesia. J Clin Monit Comput. 2014;28(2):117–21. https://doi.org/10.1007/s10877-013-9516-8.
Nunn G. Low-flow anaesthesia. Continuing Education in Anaesthesia. Crit Care Pain. 2008;8(1):1–4. https://doi.org/10.1093/bjaceaccp/mkm052.
Buhre W, De Robertis E, Gonzalez-Pizarro P. The Glasgow declaration on sustainability in Anaesthesiology and Intensive Care. Eur J Anaesthesiol. July 2023;40(7):461–4. https://doi.org/10.1097/EJA.0000000000001862.
Patil VP, Shetmahajan MG, Divatia JV. The modern integrated anaesthesia workstation. Indian J Anaesth. 2013;57(5):446–54. https://doi.org/10.4103/0019-5049.120139.
Sieber TJ, Frei CW, Derighetti M, Feigenwinter P, Leibundgut D, Zbinden AM. Model-based automatic feedback control versus human control of end-tidal isoflurane concentration using low-flow anaesthesia. Br J Anaesth. 2000;85(6):818–25. https://doi.org/10.1093/bja/85.6.818.
Arora K, Swami A, Puppala P, Rai A. Comparative study of automated end tidal control versus manual fresh gas flow adjustment with respect to gas usage and delivery during low flow anesthesia. Anesth Crit Care. 2020;2(2):39–51.
Skalec T, Górecka-Dolny A, Zieliński S, Gibek M, Stróżecki Ł, Kübler A. Comparison of anaesthetic gas consumption and stability of anaesthesia using automatic and manual control over the course of anaesthesia. Anaesthesiol Intensive Ther. 2017;49(1):34–9. https://doi.org/10.5603/AIT.2017.0008.
Lortat-Jacob B, Billard V, Buschke W, Servin F. Assessing the clinical or pharmaco-economical benefit of target controlled desflurane delivery in surgical patients using the Zeus anaesthesia machine. Anaesthesia. 2009;64(11):1229–35. https://doi.org/10.1111/j.1365-2044.2009.06081.x.
Singaravelu S, Barclay P. Automated control of end-tidal inhalation anaesthetic concentration using the GE Aisys Carestation™. Br J Anaesth. 2013;110(4):561–6. https://doi.org/10.1093/bja/aes464.
Mostad D, Klepstad P, Follestad T, Pleym H. Desflurane consumption with automated vapour control systems in two different anaesthesia machines. A randomized controlled study. Acta Anaesthesiol Scand. 2021;65(7):895–901. https://doi.org/10.1111/aas.13825.
Tay S, Weinberg L, Peyton P, Story D, Briedis J. Financial and environmental costs of manual versus automated control of end-tidal gas concentrations. Anaesth Intensive care. 2013;41(1):95–101. https://doi.org/10.1177/0310057X1304100116.
De Cooman S, Lecain A, Sosnowski M, De Wolf AM, Hendrickx JF. Desflurane consumption with the Zeus during automated closed circuit versus low flow anesthesia. Acta Anaesthesiol Belg. 2009;60(1):35–7.
Yardımcı ZA. (2021) Düşük Akım Anestezı̇sı̇ Uygulanan Hastalarda End-Tı̇dal Kontrolün Manuel Kontrollü Teknı̇ğe Göre Klı̇nı̇k ve Sevofluran Kullanımının Farmakoekonomı̇k Etkı̇sı̇nı̇n Değerlendı̇rı̇lmesı̇. Dissertation, Gazı̇osmanpaşa University.
Wetz AJ, Mueller MM, Walliser K, Foest C, Wand S, Brandes IF, Waeschle RM, Bauer M. End-tidal control vs. manually controlled minimal-flow anesthesia: a prospective comparative trial. Acta Anaesthesiol Scand. 2017;61(10):1262–9. https://doi.org/10.1111/aas.12961.
Struys MM, Kalmar AF, De Baerdemaeker LE, Mortier EP, Rolly G, Manigel J, Buschke W. Time course of inhaled anaesthetic drug delivery using a new multifunctional closed-circuit anaesthesia ventilator. In vitro comparison with a classical anaesthesia machine. Br J Anaesth. 2005;94(3):306–17. https://doi.org/10.1093/bja/aei051.
Brattwall M, Warrén-Stomberg M, Hesselvik F, et al. Brief review: theory and practice of minimal fresh gas flow anesthesia. Can J Anesth/J Can Anesth. 2012;59:785–97. https://doi.org/10.1007/s12630-012-9736-2.
Kennedy RR. Seeing the wood for the trees: insights into reducing inhalational agent consumption. Acta Anaesthesiol Scand. 2021;65(7):861–2. https://doi.org/10.1111/aas.13926.
Kennedy RR, French RA. A ten-year audit of fresh gas flows in a New Zealand hospital: the influence of the introduction of automated agent delivery and comparisons with other hospitals. Anaesth Intensive care. 2014;42(1):65–72. https://doi.org/10.1177/0310057X1404200112.
Funding
This study was supported by Sakarya University Scientific Research Projects (BAP) Commission under project number 2022-7-25-62.
Author information
Authors and Affiliations
Contributions
K.H. conducted the statistical analysis of the data. P.O. applied power analysis with a sample patient group at the beginning of the study. Literature search was performed by R.Ş. T.T.A. reviewed and made revisions, outlining the main points of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflicts of interest related to the present work.
Ethical approval
This study was conducted in accordance with the ethical approval of the Sakarya University Faculty of Medicine Clinical Research Ethics Committee, dated February 7, 2022, with protocol number 102934.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Şerefoğlu, R., Kocayiğit, H., Palabıyık, O. et al. Comparison of automated and manual control methods in minimal flow anesthesia. J Clin Monit Comput (2024). https://doi.org/10.1007/s10877-024-01163-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10877-024-01163-0