Abstract
Introduction
The intermittent intrapulmonary deflation (IID) technique is a recent airway clearance technique that intends to delay the onset of expiratory flow limitation (EFL) during exhalation. We showed in a previous study that IID increased the expiratory volume of COPD patients compared to quiet breathing and positive expiratory pressure (PEP) therapy. We hypothesized that it was due to the attenuation of the EFL.
Objectives
To verify the physiologic effects of IID and PEP techniques on EFL with a mechanical lung model.
Methods
A mechanical lung model was created to assess the effects of IID and PEP techniques. The thorax was simulated by a plexiglas box in which an adult test lung was connected. A calibration syringe simulated the inspiratory phase. Later, with activation of the IID, the expiratory phase was driven by the deflation generated by the device. With PEP, the expiration occurred maintaining an expiratory pressure between 5 and 10 cmH2O. A pneumotachograph and a pressure transducer were placed in series for flow, volumes and pressure measurements.
Results
The model reproduced physiological characteristics of EFL. However, the deflation of the model was slowed by IID and PEP, and flow remained almost constant, so flow limitation was reduced.
Conclusion
The IID and PEP attenuate EFL and increase exhaled volume in the in vitro model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Expiratory flow limitation (EFL) is a well-defined, phenomenon in which the flow of air during expiration is limited, leading to incomplete exhalation of the lung volume during a respiratory cycle [1,2,3]. EFL can occur in individuals with respiratory diseases such as chronic obstructive pulmonary disease (COPD) and asthma, as well as during exercise and in certain body positions. Several mechanisms as an increased airway resistance, lung compliance (with augmented cholinergic bronchial tone), and excessive airways collapsibility contribute to the EFL [4, 5].
Excessive EFL is common in patients with chronic obstructive pulmonary diseases (COPD) [6,7,8], affecting more than half of patients with moderate or severe airway obstruction [1, 2, 9]. It is functionally relevant in these patients because it is associated to air trapping which leads to disabling symptoms such as exercise limitation and dyspnea [1, 2, 7].
Some airway clearance techniques are used under the assumption of reducing EFL. For instance, positive expiratory pressure (PEP) therapy involves an active exhalation against a pre-defined resistance via an external device [10]. The induced physiologic effects have been referred to the slowing down of expiratory flow that decreases the pressure drop across the airway wall, preventing premature airway closure but also to the increased intrabronchial pressure that maintains the airways open during exhalation [11,12,13]. The increased expiratory volume occurs due to the decreased airway collapse that results in a greater lung emptying, lower functional residual capacity (FRC), improved ventilation distribution, and gas exchange [10]. However, breathing against an expiratory resistance may be difficult to tolerate for severe patients with COPD, since their respiratory muscles are already exposed to high resistive loads by airway obstruction [12].
In response to the drawbacks of techniques requiring active exhalation, new technologies are being developed, one example of which is intermittent intrapulmonary deflation (IID), designed to aid the elimination of bronchial secretions during relaxed expiration [14]. The IID technique generates intermittent negative pressure, interrupted at a frequency of 12 Hz during the expiratory phase, thereby generating consecutive low-frequency vibrations [14]. Moreover, the lung deflation is performed passively. Because of the passive and relaxed expiration required by the device, the IID technique intends to delay the onset of early bronchial collapse in patients with obstructive lung diseases. In a previous study [15], we observed that IID increased the expiratory volume of moderate to severe COPD patients compared to quiet breathing and PEP. Our hypothesis was that the greater expiratory volume was due to the attenuation of the EFL.
Therefore, the aim of this study was to verify the physiologic effects of IID and PEP technique on EFL with a mechanical lung model.
2 Methods
2.1 Experimental lung model
An experimental lung model was built to assess the effects of IID and PEP techniques (Fig. 1). The thorax compartment was simulated by a Plexiglas box (27 cm x 27 cm x 40 cm) in which an adult test lung (RÜSCH antistatic – Teleflex, Wayne, USA) (1 l; compliance 0.04 l.cm H2O-1) was connected. The airway compartment included a Starling resistor: a 12 cm polypropylene tube (inner diameter: 3 cm) in which a rubber airway (compliance 0.01 l.cm H2O− 1; resistance 5.7 cm H2O.l− 1.s) was placed in. A calibration syringe (3 l) was connected to the thorax compartment to simulate the inspiratory phase. In order to maintain the lung and the airway under the same “pleural” pressure, a connection was placed linking both compartments. At the top of the system, we connected a one-way valve to allow air intake during inspiration. Between the airway compartment and the one-way valve, a pneumotachograph connected to a pressure transducer (MP100 System and AcqKnowledge software, BIOPAC Systems, Santa Barbara, California) were placed in series to measure the flow, volume and pressure at a sampling rate of 1000 Hz. The IID device (Simeox – PhysioAssist - Aix-en-Povence, France) or the PEP device (PARI-PEP systems II, PARI, Starnberg, Germany) was connected to the other end of the pressure transducer via a T-piece (Fig. 1). The measurements were also taken after inserting a resistance component (20 cm H2O.l− 1.s) placed between the Plexiglas and the Starling resistor simulating the expiratory resistance of patients with COPD.
Experimental lung model with IID. 1: 3 l calibration syringe; 2: connections; 3: Plexiglas box; 4: Adult test lung; 5: polypropylene tube; 6: connection linking lung and airway compartments; 7: rubber band; 8: pneumotachograph; 9: pressure transducer; 10: One-way valve; 11: IID circuit; 12: IID device. 5 and 7 correspond to the starling resistor. For the measurements with PEP, it was connected at the location of the IID circuit and device in the figure replacing number 11 and 12 in the figure
In vivo study. System assembly with IID: 1: IID tube; 2: connections; 3: pressure transducer; 4: pneumotachograph; 5: IID mouthpiece. PEP was connected instead of IID tube [1] during PEP measurements and without IID tube or PEP for measurements without any device
Six experimental conditions were studied: control expiration (i.e., expiration without any device), expiration with PEP and expiration with IID, all of them measured with and without the added resistance.
2.2 Measurements and outcomes
The measurements in control condition (without devices) were done as following: an experimenter (JRFFDM) displaced the syringe piston during inspiratory phase which caused a pressure decrease inside the Plexiglas box (equivalent to a decrease in pleural pressure) and the air was, in turn, aspirated into the lung bag. During the active expiration phase, the experimenter operated the syringe piston until the lung was completely deflated or when no expiratory flow was measured (i.e. during airway closure). A respiratory rate of 12 breaths per minute was considered to the measurements.
To allow measurements with IID and PEP, the devices were connected as described beforehand and showed in Fig. 1. Independently of the experimental condition tested, the inspiratory phase occurred by displacement of the syringe piston. The expiratory phase with IID was driven by the deflation generated by the IID after its activation. With PEP, expiratory phase occurred via the experimenter who displaced the syringe piston while maintaining an expiratory pressure between 5 and 10 cm H2O during the whole expiratory phase. Inspiratory and expiratory phases were standardized using a metronome. Flow, pressure and volume signals were obtained as described before and used as outcome to verify the impact of IID and PEP devices on airway collapse. Three maneuvers were analyzed in each setting. High-amplitude flow oscillations were filtered out using a moving average filtering with Matlab R2020b software.
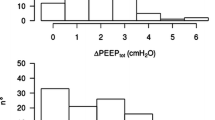
Data from a previous study [15] were taken and representative flow-volume curves of patients with COPD were superposed and analyzed. In this previous study, the subjects randomly performed a slow vital capacity maneuver either without any device, with IID, or with PEP devices. Data from two patients who had severe or very severe COPD according to GOLD [4] were randomly selected.
2.3 Statistics
The Kruskal-Wallis ANOVA test was used to compare expiratory volumes between devices and conditions. Data are reported as mean ± standard deviation (SD). All analyzes were performed using SPSS v.27 (IBM SPSS Statistics software 27, Armonk, NY). A p-value less than 0.05 was considered as statistically significant.
3 Results
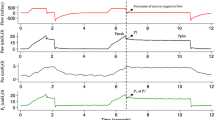
The effects of IID and PEP on experimental lung model are shown in Fig. 4. The expiratory flow-volume curve without added device or resistance (SPONT) shows no flow limitation (Fig. 4, left). By contrast, the addition of resistance caused a decrease in expiratory flow and extreme flow limitation, up to and including airway closure (Fig. 4, right).
Flow-volume curves obtained in the experimental lung model without resistance (up left panel) and with added resistance (up right panel). SPONT-curves represent the measurements without device (i.e. control); IID-curves represent the measurements with IID and PEP-curves represents the measurements with PEP. High-amplitude flow oscillations caused by the IID have been filtered out. Corresponding pressure curves output from PEP (down left panel) and IID device (down right panel)
However, no airway collapse was observed with IID and PEP as they reduced the expiratory flow throughout expiration.
Expiratory volumes were comparable between both devices, but they decreased in the control when compared with the added resistance settings. The volumes without added resistance were 0.99 ± 0.02 l, 1.03 ± 0.01 l and 0.96 ± 0.02 l (p > 0.05) and with added resistance: 0.69 ± 0.03 l, 1.03 ± 0.05 l and 1.02 ± 0.02 l, p < 0.05 for respectively, spontaneous, IID and PEP.
The characteristics of two patients with COPD from an ancillary study [15] are shown in Table 1. The flow-volume curves of each condition (i.e.: slow vital capacity maneuver without devices, with IID, and with PEP) were superimposed and displayed in Fig. 5. In both participants, the expiratory volume obtained with IID was visually greater than that obtained in slow vital capacity (SPONT).
The left side of Fig. 5 shows Participant 1 with a very severe COPD according to GOLD [4] (FEV1 = 19.2%predicted), without any device (SPONT), with IID and with PEP. With IID, expiratory flows were visually greater than in SPONT expiration for most of the expiration. His spontaneous expiratory flows were low and we assume that they were lower than those determined by the IID and PEP. The right side of Fig. 5 shows Participant 2 had a severe COPD (FEV1 = 38.7%predicted). The spontaneous (SPONT) expiratory flows were clearly higher comparing with IID and PEP condition, with the result that they exceeded those imposed by the IID.
In both participants, the expiratory volume obtained with IID was higher than that obtained in slow vital capacity (see SPONT in Fig. 4).
4 Discussion
Our study demonstrated that the higher expiratory volume with IID comparing to PEP and control condition observed in COPD patients, is due to the attenuation of the expiratory flow limitation. With IID technique, expiratory flow is kept constant, and any flow limitation was observed in in vitro model. This study confirms the results of the ancillary study [15] in patients with COPD in which the expiratory volume obtained with IID was greater than that obtained in other conditions analyzed.
Expiration is driven by the pressure gradient from alveolar pressure to atmospheric pressure at the airway opening. During a quiet expiration, the alveolar pressure is only determined by the elastic recoil forces of the rib cage and lungs [3]. Below the FRC, the expiration becomes active which involves the active use of expiratory muscles, thus increasing pleural pressure [16]. As this pressure also acts on the airways, the “equal pressure point”, which occurs when the pressure inside the airways is equal to the intrapleural pressure is reached in the airways, resulting in expiratory flow limitation [5]. In COPD patients, both increase in airway resistance and compliance lead to more severe flow limitation, occurring in the more severe patients, even during quiet breathing.
In the lung model, the IID limits expiratory flow and prevents flow limitation once flow rate decreases below 0.2 l/s. However, this mono-compartmental model cannot reproduce the behavior of several small and large airways, which explains why expiratory flow decreases abruptly in our lung model with resistance. The abrupt decrease in expiratory flow is due to the complete collapse of the airway with the Starling resistor at the end of balloon emptying in the control maneuver (right panel, Fig. 4).
In the patient with very severe COPD, the IID reduces expiratory flow limitation for flows below 0.25 l/s. Finally, in the patient with severe COPD, the effect is only noticeable at the end of expiration, again, when the spontaneous flow is lower than that imposed by IID. It can also be noticed that the increase in exhaled volume related to IID is less important in the moderate COPD patient.
The IID acts by generating an intermittent intrapulmonary air deflation during relaxed exhalation [17] i.e., by expiratory flow control. The gas flowing through the airways are not only determined by the resistance of these bronchi, but also by the pressure gradient. This implies that expiratory flow rates also represent the pressures developed by the expiratory muscles [18]. Owing to the slow and passive expiratory flow intermittently interrupted with the IID, the device minimizes the expiratory pressure required to empty the lungs. Therefore, early airway collapse is delayed, which may explain the greater expiratory volume observed under the IID condition when compared with control SPONT maneuver.
The development of EFL is functionally relevant in patients with chronic obstructive diseases, with an increase in end-expiratory lung volume and a decrease in inspiratory capacity with a concomitant increase in respiratory work [1]. These factors together with dynamic airway compression during expiration may contribute to the sensation of dyspnea [1, 19]. In physical therapy, techniques that provide expiratory positive pressure are used in order to slow expiratory flow which decreases the pressure drop across the airway wall, keeping the airways open during expiration and increasing exhaled air volume [20]. However, this therapy requires active exhalation against a pre-defined resistance [10,11,12] which may be difficult to tolerate in patients with severe COPD, since their respiratory muscles are already exposed to high resistive loads by airway obstruction [10].
4.1 Perspectives
In this study, IID and PEP attenuate the EFL in the mechanical lung model, increasing the expiratory volume. In our ancillary study, the expiratory volume obtained with IID was greater when compared to spontaneous breathing or with PEP. In this case, the positive expiratory pressure imposed by PEP requires an added work of the expiratory muscles since expiration is active and therefore dependent on expiratory muscle strength. The expiratory phase in the mechanical lung model was not dependent of expiratory muscle force, and it represents a mono-compartmental model that cannot reproduce the behavior of several small and large airways. Future research could take it in consideration in order to simulated small and large airways.
5 Conclusion
In conclusion, we demonstrated that, IID and PEP decreased the EFL, preventing airway closure in in vitro model, thereby replicating what is observed in patients with COPD.
5.1 Quick look
5.1.1 Current knowledge
Therapies involving active exhalation against a pre-defined resistance have been referred to reduce expiratory flow limitation. Breathing against an expiratory resistance may be difficult to tolerate in severe patients with COPD. The intermittent pulmonary deflation technique produces an intermittent intrapulmonary air deflation in the bronchial tree during a relaxed expiration.
5.1.2 What this paper contributes to our knowledge
The expiratory flow limitation was reproduced in the in vitro model. The IID and PEP maintain a constant expiratory flow which limit the airway collapse. The IID increase the expiratory volume in COPD patients and its effect on flow limitation varies with COPD severity.
References
Tantucci C. Expiratory flow limitation definition, mechanisms, methods, and significance. Pulm Med. 2013;2013:749860.
Aarli BB, Calverley PM, Jensen RL, Dellaca R, Eagan TM, Bakke PS, et al. The association of tidal EFL with exercise performance, exacerbations, and death in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2179–88.
Fry DL, Hyatt RE. Pulmonary mechanics. A unified analysis of the relationship between pressure, volume and gasflow in the lungs of normal and diseased human subjects. Am J Med. 1960;29:672–89.
The Global Strategy for Diagnosis MaPoC. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2023 [updated 2023. Available from: https://goldcopd.org/2023-gold-report-2/.
Pride NB, Permutt S, Riley RL, Bromberger-Barnea B. Determinants of maximal expiratory flow from the lungs. J Appl Physiol. 1967;23(5):646–62.
Orvoen-Frija E, Benoit M, Catto M, Chambouleyron M, Duguet A, Emeriau JP, et al. Chronic Obstructive Pulmonary Disease (COPD) in the elderly. Rev Mal Respir. 2010;27(8):855–73.
Global strategy for the. diagnosis, management, and prevention of chronic obstructive pulmonary disease (2020 report). 2020.
Tantucci C. Assessment and treatment of airflow obstruction in patients with chronic obstructive pulmonary disorder: a guide for the clinician. Expert Rev Respir Med. 2021;15(3):385–91.
Chiari S, Bassini S, Braghini A, Corda L, Boni E, Tantucci C. Tidal expiratory flow limitation at rest as a functional marker of pulmonary Emphysema in moderate-to-severe COPD. COPD. 2014;11(1):33–8.
Fagevik Olsen M, Lannefors L, Westerdahl E. Positive expiratory pressure - common clinical applications and physiological effects. Respir Med. 2015;109(3):297–307.
Clini E. Positive expiratory pressure techniques in respiratory patients: old evidence and new insights. Breathe. 2009;6(2):153–9.
Fagevik Olsen M, Westerdahl E. Positive expiratory pressure in patients with Chronic Obstructive Pulmonary disease–a systematic review. Respiration. 2009;77(1):110–8.
Myers TR. Positive expiratory pressure and oscillatory positive expiratory pressure therapies. Respir Care. 2007;52(10):1308–26. discussion 27.
Walicka-Serzysko K, Postek M, Jeneralska N, Cichocka A, Milczewska J, Sands D. ePS3.09 the effect of chest physiotherapy with the Simeox airway clearance technology in the treatment of cystic fibrosis pulmonary exacerbation - open-label study. J Cyst Fibros. 2019;18:46–S7.
Ribeiro Fonseca Franco, de Macedo J, Reychler G, Liistro G, Poncin W. Short-term effect of the intermittent intrapulmonary deflation technique on air trapping in patients with Chronic Obstructive Pulmonary Disease. Respiratory Care In press.
West JB. Pulmonary Pathophysiology. The Williams and Wilkins Company. 1978:p.227.
Giovannetti P, Morin L, Lafforgue O, Poncet S, Favier J, Reynaud-Gaubert M. Étude SIMETOL: évaluation de la tolérance et l’efficacité d’une procédure innovante de drainage bronchique assistée par Simeox® dans la mucoviscidose en alternative à La kinésithérapie respiratoire conventionnelle. Rev Mal Respir. 2019;36:A22.
Zach MS. The physiology of forced expiration. Paediatr Respir Rev. 2000;1(1):36–9.
O’Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2001;164(5):770–7.
Bellone A, Spagnolatti L, Massobrio M, Bellei E, Vinciguerra R, Barbieri A, et al. Short-term effects of expiration under positive pressure in patients with acute exacerbation of Chronic Obstructive Pulmonary Disease and mild acidosis requiring non-invasive positive pressure ventilation. Intensive Care Med. 2002;28(5):581–5.
Funding
The Simeox device was lent by the company PhysioAssist for the whole duration of this study. The company had no involvement in this study in any way.
Author information
Authors and Affiliations
Contributions
JRFFM and GL designed and drafted the study, analysed the data, and revised the manuscript. GR and WP provided critical revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
Ethics approval
The ancillary study mentioned was carried out in accordance with the Helsinki Declaration and approved by Comité d’Éthique Hospitalo-Facultaire Saint-Luc – UCL no. B403201940373 and registered at Clinical Trial as NCT04157972.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro Fonseca Franco de Macedo, J., Reychler, G., Poncin, W. et al. Effects of the intermittent intrapulmonary deflation technique on expiratory flow limitation: an in vitro study. J Clin Monit Comput 38, 69–75 (2024). https://doi.org/10.1007/s10877-023-01093-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01093-3