Abstract
Purpose
The standard procedure for low-flow anesthesia usually incorporates a high fresh gas flow (FGF) of 4–6 L/minute during the wash-in phase. However, the administration of a high FGF (4–6 L/min) increases the inhaled anesthetic agent consumption. This study was designed to compare the sevoflurane consumption at 2 rates of flow and vaporizer concentration during the wash-in period.
Methods
Patients were randomly enrolled into high FGF (HFGF) (n = 30) and low FGF (LFGF) (n = 30) groups. During the wash-in, the HFGF group received 4 L/minute FGF with a sevoflurane vaporizer setting of 2.5%, and the LFGF group received 1 L/minute FGF with a vaporizer setting of 8%. Once the wash-in was complete, anesthesia maintenance was performed with 0.5 L/min FGF with a vaporizer setting of 2.5–4.5% in both groups. The patient demographic data, bispectral index values, hemodynamic variables, wash-in time, sevoflurane consumption during the wash-in phase, and total sevoflurane consumption were analyzed.
Results
The median sevoflurane consumption in the wash-in phase was 8.2 mL (7.1–9.3) in the HFGF group and 2.7 mL (2.2–3.1) in the LFGF group (p = 0.001). The mean total sevoflurane consumption was 17.41 ± 3.58 mL in the patients who received HFGF and 14.93 ± 3.57 mL in the LFGF group (p = 0.001). The mean wash-in completion time was 12.49 ± 2.79 min in the HFGF group and 3.35 ± 0.67 min in the LFGF group (p = 0.001).
Conclusions
The anesthetic agent consumption during the wash-in phase was approximately 3 times lower with the administration of sevoflurane at 1 L/minute FGF than the use of 4 L/minute FGF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Low-flow anesthesia (LFA) is a technique in which the rebreathing fraction amounts to at least 50%; that is, when at least 50% of the exhaled gas mixture is returned to the patient after CO2 removal in the next inspiration with the help of a rebreathing anesthesia system [1]. The primary advantages include reducing heat loss and preserving humidity in the airways. Additionally, it creates less environmental pollution as a result of reduced release of anesthetic agents into the atmosphere, and decreases the cost associated with anesthetic gas [2, 3]. These advantages and technological developments that have increased the safety of the technique have increased the popularity of the use of low-flow anesthesia [4,5,6].
Intravenous (IV) induction of hypnotics and analgesics is time-limited. Anesthesia can be maintained with inhalational anesthetics if total IV anesthesia is not the method of choice; however, the application of inhalational anesthesia requires a wash-in period. This is the time required from initiation until the desired end-tidal inhalation anesthetic agent concentration to provide adequate depth of anesthesia is reached. A goal of the wash-in period is to avoid unnecessarily prolongation yet also to maintain an adequate depth of anesthesia during the transition from IV to inhaled anesthesia. An extended wash-in phase combined with the decreasing effects of IV anesthetics can result in an inadequate depth of anesthesia and even patient awareness [7]. Therefore, a high fresh gas flow (FGF) is routinely used during the wash-in process to reach the targeted end-tidal concentration in the anesthesia circuit and alveoli quickly. Early administration of a high FGF is an important determinant of the total inhalational anesthetic agent (IAA) consumption [8]. The pharmacology of IAA is another factor that can affect the wash-in time. With a blood/gas partition coefficient of 0.68, sevoflurane can establish a fairly fast equilibration between alveolar and blood concentration and is a good choice of IAA to be used in LFA [9]. Proper adjustments of FGF and vaporizer setting during the wash-in period can reduce IAA consumption and the time needed to reach the maintenance period [10].
IAA consumption is directly affected by both the FGF and the anesthetic vaporizer setting (VS). The hypothesis of this study was that, during the wash-in phase, volatile anesthetic consumption could be decreased by reducing FGF while compensating for the dilutional effect of rebreathing by increasing the vaporizer setting. Although studies in the literature have evaluated the results of using high concentrations of gas and low FGF during the wash-in phase [11, 12], to our knowledge, no study has examined IAA consumption in the wash-in phase. The primary aim of this study was to assess the difference in IAA consumption in cases of 4 L/minute FGF with a sevoflurane VS of 2.5% and 1 L/minute with a VS of 8% during the wash-in period in patients who underwent elective gynecological surgery.
2 Materials and methods
This prospective, randomized, single-blind, controlled trial was conducted at a research and training hospital between February 1, 2020 and January 1, 2021. The study protocol was approved by the Kartal Dr. Lutfi Kırdar Research and Training Hospital Ethics Committee on January 2, 2020 (protocol no: 2020-514-169-13) and registered with ClinicalTrials.gov (NCT04743193). All of the patients provided written informed consent prior to enrollment and the principles of the Declaration of Helsinki were observed throughout the study.
A total of 60 female patients aged 18–65 years with an American Society of Anesthesiologists (ASA) classification of I-II who underwent elective gynecological surgery under general anesthesia were included. Patients who did not provide informed consent, had severe cardiovascular or respiratory disease, or a body mass index (BMI) of > 35 kg/m2 were excluded. The patients were divided into 2 groups: 4 L/minute FGF (HFGF Group), with sevoflurane VS of 2.5%, and 1 L/minute FGF (LFGF Group), with sevoflurane VS of 8% during the wash-in period with 50% oxygen and 50% air. The group assignment was determined using the closed envelope method. A Drager Perseus A500 anesthesia device (Drägerwerk AG & Co. KGaA, Lübeck, Germany) was used in all cases. The carbon dioxide absorber was replaced and the device was leak-tested prior to the administration of anesthesia. All of the patients underwent standard monitoring, including peripheral capillary oxygen saturation (SpO2), electrocardiography, body temperature, end-tidal carbon dioxide (EtCO2), mean arterial pressure (MAP), and bispectral index (BIS; Covidien BIS Vista, Medtronic plc, Dublin, Ireland) measurements. Vascular access was established primarily on the dorsum of the hand with a 20-g IV cannula. After premedication with 0.03 mg/kg IV midazolam, general anesthesia induction was performed with 1–2 mg/kg propofol, 1–2 mcg/kg fentanyl, and 0.6 mg/kg rocuronium in all of the study patients. Following endotracheal intubation, patients were ventilated with a tidal volume of 6–8 mL/kg (according to ideal body weight) at a 12–14/minute respiratory rate.
During the wash-in phase, the sevoflurane VS was 2.5% with a FGF of 4 L/minute in the HFGF group, and 8% with a 1 L/minute FGF in the LFGF group. After reaching a minimum alveolar concentration (MAC) level of 1, the FGF was reduced to 0.5 L/minute in both groups. Remifentanil infusion (0.1-0.3mcg/kg/min) and sevoflurane (VS: 2.5–4.5%) was used to maintain anesthesia in both groups, with a target BIS value in the range of 40–60. The wash-in time and IAA consumption of all of the patients were recorded. The BIS values and hemodynamic variables were also recorded every 15 min. The sevoflurane vaporizer was turned off approximately 15 min before the end of the operation, and the wash-out phase was initiated in coordination with the surgical team with the FGF set to 0.5 L/minute. As the final suturing was concluded, the wash-out was completed using a FGF of 6 L/minute with 100% oxygen. When spontaneous ventilation effort was observed, decurarization was achieved using 0.01 mg/kg atropine and 0.03 mg/kg neostigmine. Once sufficient muscle strength and spontaneous respiratory depth were observed, the patient was extubated and taken to the recovery unit.
2.1 Sample size calculation
A reference study of sevoflurane [13] had a medium effect size (d = 0.65). Power analysis calculations indicated that at least 60 individuals (minimum of 30 in each group) would be needed for our study to achieve 80% power at a 95% confidence level.
2.2 Statistical analysis
Continuous variables were presented as the mean ± SD or median (interquartile range [IQR]). The Shapiro-Wilk test was used to assess normal distribution. Whenever parametric test assumptions were provided, an independent samples t-test was used to compare independent groups. Otherwise, the Mann-Whitney U test was used to compare independent groups. The difference between categorical variables was analyzed with a chi-squared test. Statistical significance was accepted at p < 0.05. All of the statistical analyses were performed using IBM SPSS Statistics for Windows, Version 25.0 software (IBM Corp., Armonk, NY, USA).
3 Results
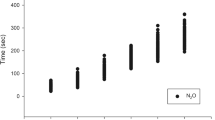
A total of 60 patients were included in the study (Fig. 1). The demographic data of the groups, including ASA class, age, BMI, and duration of anesthesia and surgery, were similar (p > 0.05) (Table 1). There was no difference in the heart rate, MAP, SpO2, or EtCO2 values (p > 0.05) (Fig. 2a,b,c,d). In addition, there was no significant difference in the BIS values between groups (p > 0.05) (Fig. 3).
The median sevoflurane consumption during the wash-in period was 8.2 mL (IQR: 7.1–9.3 mL) in the HFGF group and 2.7 mL (IQR: 2.2–3.1 mL) in the LFGF group while the mean wash-in time was 12.49 ± 2.79 min and 3.35 ± 0.67 min respectively (p = 0.001) (Table 2).
The difference between the anesthetic agent consumption and the anesthetic uptake during the wash-in period was 5.25 mL (IQR: 4.4–6.12 mL) in the HFGF group and 1.35 mL (IQR: 1.1–1.52 mL) in the LFGF group (p = 0.0001) (Table 2).
Sevoflurane consumptions at the 15th minute were 8.85 mL (IQR: 7.98–10.28 mL) and 5.45 mL (IQR: 4.6–6.1 mL) for the HFGF and LFGF groups respectively (P = 0.0001). The mean total quantity of agent consumption after anesthesia was 17.41 ± 3.58 mL in the HFGF group and 14.93 ± 3.57 mL in the LFGF group (p = 0.01) (Table 3).
4 Discussion
The anesthetic agent consumption during the wash-in phase was lower in the LFGF group than the HFGF group, which directly affects the 15 th minute and the total consumptions. The results of this study indicate that increasing rebreathing during wash-in can significantly reduce IAA consumption. In addition, the induction of inhalational anesthetics with 1 L/minute FGF using a sevoflurane VS of 8% significantly shortened the wash-in time.
The advantages of low-flow anesthesia with high VS during the wash-in phase in terms of anesthetic agent consumption have been noted in various studies. Horwitz et al. [11] reported that using a FGF of 1.0 or 0.5 L/minute with a sevoflurane VS of 6% during wash-in resulted in a time to reach 1 MAC of 6.2 ± 1.3 and 15.2 ± 2.4 min, respectively. Moreover, the total amount of agent consumed was 19% less with the administration of 0.5 L/minute. In another study, Bahar et al. [7] used 1 L/minute FGF with a desflurane VS of 18% in the wash-in phase and reported a time to reach a MAC value of 0.7 of 2.9 ± 0.5 min, and a mean anesthetic agent consumption at the end of the operation of 0.33 ± 0.05 mL/minute. In these studies, high concentrations of IAA were used in the wash-in phase of anesthesia, and a shortened wash-in period was observed. Similarly, in our study, we used high concentrations of IAA in the LFGF group in the wash-in phase and we found that the wash-in phase was shorter. Previous studies have also indicated that the use of LFGF and high concentrations of anesthetic agent reduced consumption. However, these studies primarily evaluated the total consumption of IAA and did not fully examine the effect of IAA consumption during the wash-in phase. Our research assessed IAA consumption during the wash-in phase, which constitutes an important part of the total consumption, and demonstrated that it can be reduced. Our findings revealed that the wash-in phase IAA consumption in the HFGF group was greater than that of the LFGF group. Although the anesthesia maintenance was the same in both groups, minimal flow with a similar duration, the total consumption was greater in the HFGF group than the LFGF group, indicating that the savings of LFA during the wash-in period were preserved throughout the process.
Different methods can be used during the LFA wash-in phase. Horwitz et al. [11] evaluated wash-in phase duration with a sevoflurane VS of 6% in groups of 0.5 L/minute and 1 L/minute FGF. In the 0.5 L/minute group, the wash-in period lasted approximately 15 min, and the authors prepared for the administration of additional intravenous anesthetic agents in the event of inadequate depth of anesthesia. In our study, the application of 1 L/minute FGF with an 8% sevoflurane setting resulted in a reduced wash-in duration with the maintained targeted BIS values, signifying that the depth of anesthesia was sufficient. The use of a high concentration of sevoflurane (8%) with a higher flow (4–8 L/min) may reduce the wash-in time. However, there is a potential risk due to the combination of the ongoing effects of intravenous anesthetic agents and an inhalational anesthetic, which may result in an excessive depth of anesthesia. The application of 0.5 or 0.75 L/minute FGF coupled with an 8% sevoflurane VS during the wash-in phase may result in a lower IAA consumption, but requires further investigation.
Reduced consumption would provide important benefits both in terms of preventing environmental pollution and lowering costs. In our study, we found that the sevoflurane consumption during the wash-in period in the LFGF group was 5.5 mL lower on average per case compared with the HFGF patients.
Since the HFGF group wash-in period was longer, we examined consumption data at the 15th minute, once both groups had completed the wash-in phase, and an important difference in the consumption rate was observed. The average sevoflurane consumption in the LFGF group was 3.4 mL lower than that of the HFGF group per case. For 100 patients the reduction could amount to approximately 340 mL. The savings quickly becomes quite significant. According to information gathered from the medical department of our university hospital, a 250 mL bottle of sevoflurane costs approximately 95 €. Each day, more than 100 patients have general anesthesia in our department, and the extra consumption of 340 mL sevoflurane represents 130 € per day that could be saved.
Inhalation anesthetic agents also have a significant environmental effect. Carbon dioxide (CO2) is a well-known greenhouse gas and is the point of reference in the calculation of the global warming potential (GWP) of various gases [14]. Sevoflurane has a GWP20 of 702 [15], meaning that 1 gr of sevoflurane has the same global warming effect as 702 gr of CO2 over a 20-year time frame. As the specific gravity of sevoflurane is 1.52 gr/mL [14], a quantity of 340 ml is equivalent to 516.8 gr. Thus, this amount of sevoflurane will have a greenhouse effect equivalent to 362.79 kg (516.8 gr *702) of CO2 over a 20-year period. According to the United States Environmental Protection Agency greenhouse gas equivalencies calculator [16], 362.79 kg of CO2 emission is equal to 40.8 gallons of gasoline consumption. Low-flow anesthesia beginning with the wash-in phase offers opportunities to reduce consumption, cost, and environmental impact.
The difference between the quantity of sevoflurane used and the patient uptake provides an instantaneous measurement of the sevoflurane emitted. The determinants of IAA uptake are the blood-gas partition coefficient of the anesthetic agent, the partial pressure difference of the agent between the alveoli and alveolar blood, and the alveolar blood flow [17]. In order to increase uptake, the alveolar partial pressure of IAA must be increased by setting the vaporizer to a higher concentration or administering high FGF to maintain the IAA concentration. However, high FGF administration increases IAA consumption. Arslan et al. [18] highlighted that the use of low-flow anesthesia with high concentration (desflurane 18%) increased the agent uptake by the patient and reduced the emitted and consumed amounts. In our study, the IAA vaporizer was set at 8% with low FGF (1 L/min.). We found that the uptake was increased, resulting in less overall agent consumption and pollution. Our results indicated that a median of 5.25 mL (IQR: 4.4–6.12 mL) of sevoflurane was emitted during the wash-in phase in patients who started with a high-flow, while it was only 1.35 mL (IQR: 1.1–1.52 mL) in the low-flow group with an 8% sevoflurane concentration. The study findings revealed that an initial high-flow application led to a greater quantity of emitted gas beginning early in the wash-in phase. However, a low-flow application with a high concentration significantly reduced the emission.
When the BIS values, SpO2 level, hemodynamic parameters, and EtCO2 values of the groups were evaluated, no difference was seen. In addition we observed that the induction of inhalational anaesthetics with 1 L/min FGF with a sevoflurane VS of 8% shortened the wash-in time. Reduced IAA consumption with LFA was obtained without sacrificing the quality of anesthesia. Furthermore, the fact that the SpO2 values continued to be ≥ 98% demonstrates that early use of low-flow can be administered safely without causing hypoxia.
4.1 Limitations
A primary limitation of our study was the use of a single anesthetic agent. The blood/gas partition coefficient of different agents will have an impact on consumption. In addition, interpretation of the findings is limited by the single-center design.
5 Conclusions
In conclusion, the study results indicated that the use of sevoflurane at 1 L/minute with a VS of 8% during the wash-in phase reduced both IAA consumption and the wash-in time. The use of higher concentrations of IAA with LFA during the wash-in phase offers several benefits, and would appear to be an alternative technique worthy of further examination.
Change history
13 May 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10877-022-00875-5
References
Baum JA, Aitkenhead AR. Low-flow anaesthesia. Anaesthesia. 1995;50:37–44. doi: https://doi.org/10.1111/j.1365-2044.1995.tb06189.x.
Leijonhufvud F, Jöneby F, Jakobsson JG. The impact of fresh gas flow on wash in, wash out time and gas consumption for sevoflurane and desflurane, comparing two anaesthesia machines, a test lung study. F1000Res. 2017;6:1997. doi: https://doi.org/10.12688/f1000research.13064.2.
Sathitkarnmanee T, Tribuddharat S, Suttinarakorn C, Nonlhaopol D, Thananun M, Somdee W, et al. 1-1-12 one-step wash-in scheme for desflurane-nitrous oxide low-flow anesthesia: rapid and predictable induction. Biomed Res Int. 2014;2014:867504. doi: https://doi.org/10.1155/2014/867504.
Kim J, Kang D, Lee H, Ryu S, Ryu S, Kim D. Change of inspired oxygen concentration in low flow anesthesia. Anesth Pain Med. 2020;15(4):434–40. doi: https://doi.org/10.17085/apm.20055.
Leelanukrom R, Tuchinda L, Jiamvorakul P, Koomwong A. Desflurane concentrations and consumptions during low flow anesthesia. J Med Assoc Thai. 2014;97(1):64–70. PMID: 24701731.
Cui Y, Wang Y, Cao R, Li G, Deng L, Li J. The low fresh gas flow anesthesia and hypothermia in neonates undergoing digestive surgeries: a retrospective before-after study. BMC Anesthesiol. 2020;20(1):223. doi: https://doi.org/10.1186/s12871-020-01140-5.
Bahar S, Arslan M, Urfalioglu A, Gisi G, Oksuz G, Bilal B, et al. Low-flow anaesthesia with a fixed fresh gas flow rate. J Clin Monit Comput. 2019;33(1):115–21. doi: https://doi.org/10.1007/s10877-018-0135-2.
Hendrickx JF, Dewulf BB, De Mey N, Carette R, Deloof T, De Cooman SD, et al. Development and performance of a two-step desflurane-O2/N2O fresh gas flow sequence. J Clin Anesth. 2008;20(7):501–7. doi: https://doi.org/10.1016/j.jclinane.2008.05.013.
Brattwall M, Warrén-Stomberg M, Hesselvik F, Jakobsson J. Brief review: theory and practice of minimal fresh gas flow anesthesia. Can J Anaesth. 2012;59(8):785–97. doi: https://doi.org/10.1007/s12630-012-9736-2.
Chatrath V, Khetarpal R, Bansal D, Kaur H. Sevoflurane in low-flow anesthesia using “equilibration point. Anesth Essays Res. 2016;10(2):284–90. doi: https://doi.org/10.4103/0259-1162.172343.
Horwitz M, Jakobsson JG. Desflurane and sevoflurane use during low- and minimal-flow anesthesia at fixed vaporizer settings. Minerva Anestesiol. 2016;82(2):180–5.
Tribuddharat S, Sathitkarnmanee T, Vattanasiriporn N, Thananun M, Nonlhaopol D, Somdee W. 1-1-8 one-step sevoflurane wash-in scheme for low-flow anesthesia: simple, rapid, and predictable induction. BMC Anesthesiol. 2020;20(1):23. doi: https://doi.org/10.1186/s12871-020-0940-2.
Sert H, Muslu B, Gozdemir M, Kurtaran H, Usta B, Kınacı S, et al. Evaluation of recovery and anesthetic gas consumption using remifentanil combined with low-flow sevoflurane anesthesia in tympanoplasty. ORL J Otorhinolaryngol Relat Spec. 2011;73(3):141–6. doi: https://doi.org/10.1159/000327600.
Edmonds A, Stambaugh H, Pettey S, Daratha KB. Evidence-based project: cost savings and reduction in environmental release with low-flow anesthesia. AANA J. 2021;89(1):27–33.
AR6 Climate Change. 2021: The physical science basis. https://www.ipcc.ch/report/ar6/wg1/. Accessed February 18, 2022.
United States Environmental Protection Agency. Greenhouse gas equivalencies calculator. 2018 https://www.epa.gov/energy/greenhouse-gas-equivalencies-calculator. Updated March 2021. Accessed January 12, 2022.
Cowles CE. Inhalation Anesthetics. In: Butterworth JF, Mackey DC, Wasnick JD, editors. Clinical Anesthesiology, 5 th. edn. Mc Graw Hill Education; 2013. pp. 153–73.
Arslan M, Gişi G, Öksüz G, Öksüz H, Bilal B, Boran ÖF, et al. Are high fresh gas flow rates necessary during the wash-in period in low-flow anesthesia? Kaohsiung J Med Sci. 2020;36(10):834–40. doi: https://doi.org/10.1002/kjm2.12251.
Funding
This research did not receive any spesific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Tahsin Simsek: corresponding author, data curation, conceptualization, methodology, writing reviewing & editing. Suleyman Derman: data curation, writing- original draft preparation, software, validation, investigation. Raghad Giuma M Kordi: writing- original draft preparation, conceptualization, methodology. Ayten Saracoglu: visualization, writing - reviewing & editing. Kemal Tolga Saracoglu: supervision, visualization.
Corresponding author
Ethics declarations
Competing interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Kartal Dr. Lutfi Kirdar Training and Research Hospital (Date 02.01.2020/No 2020-514-169-13).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Affiliations of the third and fifth authors are published incorrectly. The correct affiliations are updated in the article.
Rights and permissions
About this article
Cite this article
Simsek, T., Derman, S., Kordi, R. et al. The effect of different flow levels and concentrations of sevoflurane during the wash-in phase on volatile agent consumption: a randomized controlled trial. J Clin Monit Comput 36, 1257–1262 (2022). https://doi.org/10.1007/s10877-022-00846-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00846-w