Abstract
Quantra® Hemostasis Analyzer is a Point of the care device that uses ultrasound technology to assess clot formation. In this study, we establish how Quantra® system performs compared to conventional coagulation tests at low levels of fibrinogen in the blood obtained from pregnant women. 24 mL blood was obtained from each healthy parturient. Blood was analyzed for Quantra® variables (Q): Clot time (CT), Clot stiffness (CS), platelet contribution to CS (PCS), fibrinogen contribution to CS (FCS), and conventional coagulation (CL) tests: PT, aPTT, INR, Factor VIII and fibrinogen. 6 ml blood were centrifuged to obtain pregnant plasma. 30 mL of saline was added to 10 mL of blood to simulate crystalloid resuscitation (DB) and was evaluated for Q and CL. Fractions of pregnant plasma, or nonpregnant plasma (Blood Bank) was added to DB to obtain 15% and 30% clotting factor enriched samples. 4 ml of DB was added to 4 ml of original blood (1:1) to obtain the final sample (resus). Each of the samples were analyzed for Q and CL parameters. Regression analysis and Receiving Characteristics Curves were used to study the relationship between Quantra variables and CL tests. There were remarkably high linear correlations between Fibrinogen and CS (R = 0.93, P < 0.001), fibrinogen and FCS (R = 0.77, P < 0.001). An FCS value 2.45 (sensitivity of 79.2 and specificity of 97.3%), and CS value 10.85 hPa (sensitivity of 83% and specificity of 100%) predicted fibrinogen of 200 mg/dL. This study demonstrates a good correlation between Quantra® CS, FCS and serum fibrinogen.
Clinical Trial Number: NCT04301193.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Unexpected obstetric hemorrhage persists to haunt perinatal care providers and continues as the prominent cause of maternal mortality and morbidity worldwide [1, 2]. This is despite availability of uterotonics, tranexamic acid, fibrinogen concentrate, effective surgical techniques, and blood banking facilities [3]. Major societies have focused on educating their members, on the awareness, prevention, recognition, monitoring and management of peripartum hemorrhage [4]. Perinatal care providers have evaluated numerous strategies of quantifying blood loss accurately and are using them in clinical practice in assessing blood loss and guiding transfusions during obstetric hemorrhage [5,6,7]. However, one of the major obstacles confronting clinicians is the lack of a simple, user friendly point of care (POC) coagulation monitoring device, which provides timely and accurate results to guide clinical management of unexpected obstetric hemorrhage. Conventional coagulation tests such as prothrombin time (PT), activated partial thromboplastin time (aPTT), and fibrinogen take considerable time (30–90 min) before obtaining results [8]. In an effort to provide quicker results of coagulation, newer point of the care devices using cartridge based technologies are being introduced. Thromboelastography (TEG®) 6 s system (Haemonetics, Braintree, Massachusetts, USA), Rotational Throboelastometry (ROTEM®) Sigma (Instrumentation Laboratory, Bedford, Massachusetts, USA), and the Quantra® Hemostasis Analyzer with the QPlus cartridge system (HemoSonics, LLC, Charlottesville, Virginia, USA) are capable of assessing coagulation quickly. In this in-vitro dilution and reconstitution study, we determine how Quantra QPlus system performs compared to conventional coagulation tests at low levels of fibrinogen in the blood obtained from pregnant women. This is the first study to evaluate a POC system for low fibrinogen levels.
2 Quantra QPlus system®
The Quanta® uses Sonic Estimation of Elasticity via Resonance (SEER Sonorheometry technology) [9]. High-frequency ultrasound pulses are utilized to quantify the shear modulus (stiffness) of a blood sample during the process of coagulation. All test sequences such as fluid handling, temperature control (37 °C), ultrasound transmission, data processing and result output are all automated. A focused ultrasound pulse is transmitted into the blood sample to generate a shear wave, causing the sample to resonate once the clot begins to form. As the clot vibrates during resonance, a series of “tracking” ultrasound pulses are transmitted, and the returning echoes are analyzed to estimate the sample’s motion. Repeated acquisition echo signals over time produces a signature curve. From this curve, the stiffness (hPa) of the clot and the start of the clot formation, represented as clot time (seconds), can be directly estimated. Quantra uses a plastic cartridge with embedded reagents. Cartridge based system may have added advantage of not being susceptible to clot disruption caused by rotational mechanisms (pin and cup) of TEG® 5 and ROTEM® technologies. The cartridge has 4 test channels that perform 4 parallel and independent measurements using different reagent combinations in each channel (Cannel 1: Kaolin, calcium, buffers, and stabilizers; Channel 2: Kaolin, heparinase I, calcium, buffers, and stabilizers; Channel 3: Thromboplastin, polybrene, calcium, buffers, and stabilizers; Channel 4: Thromboplastin, polybrene, abciximab, calcium, buffers, and stabilizers). The cartridge encompasses a port for inserting 3 ml blood vacutainer for coagulation analysis.
The QPlus Cartridge was utilized for this investigation. The reagents in channel 1 of this cartridge are optimized for the measurements of clot time, whereas the channel 2 measures clot time without the effect of any potential heparin in the blood sample (Heparinase clot time, CTH). Clot times provide an indication of the functional status of the coagulation factors that lead to fibrin formation. Channel 3 is optimized to provide measurements of clot stiffness, which combines information about platelets and fibrinogen function. Finally, channel 4 is optimized to measure the Fibrinogen contribution to clot stiffness. The calculated difference between Channel 4 and Channel 3 can provide a measure of platelet contribution to clot stiffness.
3 Methods
The study was approved by Institutional Review Board, University of Maryland (National Clinical Trials, NCT04301193). Written informed consent was obtained from all subjects. Thirteen healthy parturients aged 18–40 years with uncomplicated pregnancies at term gestation, between 37 and 41 weeks were enrolled after, presenting for induction of labor or cesarean delivery. Exclusion criteria included hypertension, preeclampsia, gestational diabetes, preexisting coagulopathy, history of deep vein thrombosis, medications that impair coagulation, or history of pulmonary embolism or thrombosis. In addition, parturients on aspirin, non-steroidal inflammatory drugs (NSAIDS), and low molecular weight heparins were also excluded. At the time of intravenous catheter placement, the blood was collected into eight citrated tubes (Beckton Dickinson, Franklin Lakes, NJ), each with a maximum capacity of 2.7 mL of blood and containing 3.2% sodium citrate. Citrated blood from each tube was pooled into a container to eliminate variability in citrate concentration between each vacutainer blood samples.
The variations in fibrinogen concentrations were created by diluting the blood with saline and reconstituting the diluted blood with plasma from the Blood Bank as well as plasma derived from the parturients’ own blood. The use of non-pregnant plasma from Blood Bank and parturients’ own plasma with high fibrinogen and clotting factors may simulate transfusion of plasma, or cryoprecipitate.
A detailed schematic of the protocol methodology is shown in Fig. 1. Three milliliters from the pooled blood was analyzed for the following Quantra parameters of interest (Q): Clot time (CT), clot stiffness (CS), platelet contribution to clot stiffness (PCS), fibrinogen contribution to clot stiffness (FCS). Two milliliters were centrifuged to obtain 1 ml of plasma for conventional coagulation tests (CL) that included PT, aPTT, INR, and fibrinogen, and Factor VIII. Three aliquots containing 2 mL of blood were centrifuged to obtain pregnant plasma. Thirty mL of saline was added to 10 mL of blood to simulate crystalloid resuscitation (Diluted blood-DB). Three ml from DB was evaluated on the Quantra and 2 ml centrifuged to obtain plasma for CL. Fractions of pregnant plasma was added to DB to obtain 15% and 30% clotting factor enriched samples (PP). Nonpregnant plasma was obtained from the Blood Bank and added to aliquots of DB in lieu of pregnant plasma to obtain 15 and 30% (NP) enriched samples. Pregnant plasma contains elevated clotting factors and fibrinogen and is more like cryoprecipitate transfusion. Finally, 4 ml of diluted blood was added to 4 ml of original blood (1:1) to obtain the final sample (resus) to simulate transfusion with plasma, red blood cells and platelets. Each of the samples were analyzed on the Quantra (3 ml) and 2 ml centrifuged to obtain plasma for CL. In all, blood from each parturient provided 7 samples of varying clotting factor strengths. The platelet count was determined in the original sample, diluted, and resuscitated samples using Hematology Analyzer (Beckman Coulter, Brea, California, USA). All samples were analyzed by two hours following blood draw.
3.1 Statistical analysis
Statistical software (SAS) version 9.4 (Cary, North Carolina, USA) was used to analyze the data. The primary outcomes of this study were the area under the receiving operating characteristic (AUROC) curves for fibrinogen and Quantra CS, fibrinogen and FCS. The secondary outcomes were the AUROC for platelets and Quantra PCS. Additional secondary outcome included relationship between PT and Quantra CT, and aPTT and Quantra CT. As exploratory outcomes, the optimal CS and FCS values corresponding to a fibrinogen concentration of 200 mg/dL were also calculated. We chose a fibrinogen concentration of 200 mg/dL based on observations of earlier studies that a fibrinogen level less than 200 mg/dL was associated with progression towards more severe postpartum hemorrhage [10, 11].
Using standard techniques for estimating sample size, a Delong’s test indicated that a total of 61 samples would be sufficient to detect a 0.2 increase in the AUROC from the null hypothesis 0.5, assuming an alpha level of 5% and 90% power [12]. The manuscript was referenced against the STROBE checklist for cohort studies.
Descriptive statistics were used to present baseline values for Quantra, conventional labs and Factor 8 (Mean ± SD, and 95% confidence intervals). One-way Analysis of Variance (ANOVA) was used to evaluate the different data values for each conventional test and Quantra variables. For data values with a significant ANOVA, a post Tukey HSD analysis was performed to determine if one value was significantly different from the prior value within each variable. Regression analysis was also performed between Quantra FCS and fibrinogen, Quantra CS and fibrinogen, Quantra PCS and platelet count, and Quantra CS and platelet count. A logistic regression model, as well as AUROC analyses were performed. Youden’s method was utilized to determine the optimal values of FCS and CS for the detection of fibrinogen < 200 mg/dL, and PCS for platelets < 70 × 109/L. Regression analysis was also performed to determine the relationship between Quantra CT and PT and aPTT.
4 Results
Thirteen parturients were enrolled into the study. The mean age was 31 ± 6.5 yr, gravida was 4 ± 2, and gestational age was 37.4 ± 1.7. Ten of the patients were admitted for elective cesarean delivery and the remaining for induction of labor. The schema protocol provided 89 samples for analysis across varying levels of fibrinogen. These included 11 samples, which were obtained by reconstituting by mixing diluted blood with the patient’s own blood. The first two subjects did not have resuscitated component samples.
The Table 1 shows the mean and standard deviation (SD) for conventional laboratory coagulation tests (PT, INR, aPTT, fibrinogen, platelet) for all category set of samples (baseline, diluted blood, reconstituted 15% and 30% pregnant and non-pregnant plasma enriched samples as well as resuscitated samples). Table 2 shows the trend of Quantra variables from baseline sample to various dilutional and reconstituted concentrations of fibrinogen samples. The 95% confidence intervals for baseline values for Quantra variables in this study were clot time (CT) 120.5–133.5 s, clot stiffness (CS) 27.4–38 hPa, platelet contribution to clot stiffness 23.7–32.1 hPa, and fibrinogen contribution to clot stiffness 3.6–6.2 hPa.
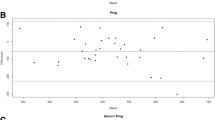
Figure 2A shows how Quantra CS and FCS and fibrinogen levels change with dilution and reconstitution. All three measurements responded similarly to dilution and reconstitution. This is also true for Quantra CT and laboratory PT, and aPTT (Fig. 2B). Figure 2A and B also highlight data points on the trend curves that are significantly different from the preceding data point on the curve (Tukey). Scatterplots show the relationship between Fibrinogen and CS and FCS (Fig. 3A and B). Relationship between platelets and PCS is shown in Fig. 4A, and the relationship between PT, aPTT and CT are shown in Fig. 4C and D. The correlation between fibrinogen concentration in the samples and Quantra CS is strong (R = 0.93, P < 0.001, n = 88, 1 sample resulted in a test error, Fig. 3A). The correlation between fibrinogen and FCS was R = 0.77 (P < 0.001, n = 88, Fig. 3B). The correlation between CT and PT (R = 0.60, p < 0.001), INR (R = 0.60, p < 0.001, Fig. 4C), and aPTT (R = 0.66, P < 0.001, Fig. 4D) also demonstrate moderate strength in association. The Receiver operating cure analysis used to estimate CS and FCS values predictive of a fibrinogen level of 200 mg/dL are shown in Fig. 3C and D respectively. The AUROC for FCS in detecting a fibrinogen < 200 mg/dL was 0.931 (95% CI 0.881–0.980, p < 0.001). The optimal value for the detection of fibrinogen < 200 mg/dL based on Youden’s Index was an FCS of 2.45 hPa. This resulted in a sensitivity of 79.2%, specificity 97.3%, negative predictive value of 76.5% and positive predictive value 97.7%. Furthermore, the ROC curve for CS value in detecting fibrinogen < 200 mg/dL was 10.85 hPa (specificity 100% and sensitivity 83%, Fig. 3C).
A Correlation between fibrinogen and CS (R = 0.93, P < 0.001, n = 88). B Correlation between fibrinogen and FCS (R = 77, P < 0.001, n = 88). C: Receiving Operative Curve estimating CS value for fibrinogen < 200 mg/dL. The estimated value for CS is 10.85 hPa. D: Receiving Operative Curve estimating FCS value for fibrinogen < 200 mg/dL. The estimated value for FCS is 2.45 hPa
A Correlation between platelets and PCS (R = 0.9, P < 0.001, n = 34). B Receiving Operative Curve estimating PCS value for platelets < 70 × 109. The PCS value is estimated as 8. hPa. C Correlation between CT and PT (R = 0.60, P < 0.001, n = 88). D Correlation between CT and aPTT (R = 0.66, P < 0.001), n = 88)
There was also a strong correlation between platelets and PCS (R = 0.90, P < 0.001, n = 34), and platelets and CS (R = 0.90, P < 0.001, n = 34, Fig. 4A). Based on Youden’s Index, the optimal value of PCS for the detection of platelet count of < 70 × 109 was 8.8 hPa (Fig. 4B). At this threshold, this resulted in a sensitivity of 100% and a specificity of 95.6% (Fig. 4).
5 Discussion
The Quantra® QPlus coagulation system requires only three steps to initiate this process: activate the device, insert the reagent cartridge, and load the citrated blue top tube. The coagulation results are displayed in less than 15 min during which the clinician can continue with ongoing clinical management of hemorrhage.
Our study demonstrates that the Quantra parameters broadly replicate trends in conventional coagulation tests, PT, aPTT and fibrinogen (Fig. 2A, B). There is a strong correlation between blood fibrinogen level and CS (R = 0.93, P < 0.001), and FCS (R = 0.77, P < 0.001) implying that Quantra CS and FCS are good predictors for estimating fibrinogen level. The dilutional and reconstitution method used in this study enabled us to test the Quantra CS and FCS at lower range of fibrinogen, which is critical in obstetric hemorrhage. A fibrinogen level below 200 mg/dL is often associated with post-partum hemorrhage [10, 11]. The optimal thresholds for the detection fibrinogen < 200 mg/dL in our study corresponded to Quantra CS of 10.85 hPa, and FCS of 2.45 hPa. In addition, there was also a strong correlation between PCS (platelet contribution to clot formation) and absolute platelet count (r = 0.90, P < 0.001), thus demonstrating that Quantra is also valuable in assessing thrombocytopenia. The optimal threshold for the detection of a platelet count < 70 × 109/L corresponded to a PCS of 8.8 hPa. A platelet count of 70 × 109/L is considered as the minimum threshold for the placement of regional anesthesia, and the PCS estimation of platelet count may have future implications in assessing platelet function before contemplating regional anesthesia in pregnant women.
An important observation made in our study is the considerable variation observed in the baseline fibrinogen in pregnant subjects. It ranged from 268 to 620 mg/dL. It has been previously reported that a fibrinogen of 200 mg/dL is reached after the blood loss of about 2.5–3 L during obstetric hemorrhage in one retrospective study [10]. However, our observations suggest that fibrinogen monitoring is necessary during hemorrhage since presenting baseline fibrinogen levels varied substantially. A parturient with lower range of baseline fibrinogen is more likely to reach a threshold of 200 mg/dL quicker than a parturient with higher baseline fibrinogen. The lack of predictability of starting fibrinogen in parturients during hemorrhage poses extreme challenges in the management of obstetric hemorrhage. Therefore, a quick and reliable measurement of fibrinogen becomes an essential component of systematically managing a parturient with obstetric hemorrhage. Under these circumstances, Quantra CS and FCS can help since the results are obtainable reasonably quickly. It also seems rational to justify the measurement of baseline fibrinogen in high risk obstetric patients to gauge the effect of blood loss on the maternal coagulation. A lower baseline fibrinogen should put the clinicians on alert in assessing blood loss diligently in parturients undergoing labor and delivery, or cesarean delivery.
The Quantra parameters of clot stiffness have been validated to correlate strongly with the fibrinogen as well as corresponding values of existing viscoelastic devices (ROTEM® and TEG®) and standard laboratory values in non-pregnant subjects undergoing cardiopulmonary bypass and during major surgeries [13,14,15]. A strong correlation between Quantra® CS and EXTEM of ROTEM (r = 0.94–0.96), Quantra® FCS with FIBTEM (r = 0.74) and conventional fibrinogen levels (r = 0.87) were observed.[13,14,15]. In our study of pregnant subjects, we limited our comparison of Quantra® parameters to conventional laboratory coagulation tests. Addition of ROTEM®, or TEG® to study all dilutions of samples would have required substantially more blood from the research parturients. Moreover, our intention was not to establish the superiority of one technology over the other, but rather to test a novel device that is deemed suitable for circumstances relevant to obstetric hemorrhage.
Our study findings show the correlation between Quantra CT and PT (R = 0.66, P < 0.01) and aPTT( R = 0.66, P < 0.01) to be moderate These observations are similar to the observations made between PT, aPTT and clot time from viscoelastic based devices where the correlation is minimal to moderate [16,17,18]. This is presumably due to differences in the type of reagents, and principles of the tests [17]. Traditional laboratory coagulations tests (PT, aPTT) are standardized for testing plasma without any cellular components such as platelets, RBCs, leukocytes or endothelial cells. On the other hand, whole blood viscoelastic test includes both cellular and humoral elements of coagulation, although endothelial cells are not included. Given the fact that coagulopathic data can be more rapidly assessed using viscoelastic coagulation tests compared to traditional plasma-based tests, moderate correlations between these two methodologies are clinically acceptable in the setting of acute hemorrhage [19, 20].
Non pregnant plasma and pregnant plasma were used in our study and this allowed samples with various levels of fibrinogen to be tested against Quantra parameters around fibrinogen levels of 200 mg/dL. Furthermore, pregnant plasma contains more factor 8 concentrations compared to non-pregnant plasma (248 versus 57 IU/dL) and the use of pregnant plasma in our study may be considered to simulate administration of cryoprecipitate during obstetric hemorrhage management. We used blood to saline 1:4 dilution to create baseline test sample to lower the fibrinogen concentrations as low as 105 mg/dL and platelets to 55 × 109. Despite this extent of dilution, Quantra QPlus system was able to generate enough shear wave, causing the sample to resonate as the clot formed, thus emphasizing the sensitivity of Quantra device at low fibrinogen concentrations and platelet environment. Pregnancy induced coagulation changes most likely enabled Quantra device to function well. Pregnant subject blood at term has been shown to be relatively resistant to dilutional coagulation changes with respect to platelet adhesion, fibrin polymerization, and thrombin generation [21]. This is most likely due to high functional reserves of fibrinogen, factor VIII, and vWF in pregnant subjects, which is 1.5–2 times the upper normal range of non-pregnant subjects [21].
There are few limitations in this study. First, this is an in-vitro dilution / reconstitution study and interpolation to clinical circumstances is difficult. Further evaluation of Quantra functionality in actual ongoing hemorrhage, during coagulopathy is to be studied. Second, we used pregnant plasma to reconstitute some of the samples for this study, and pregnant plasma contains higher clotting factor levels than the non-pregnant plasma used in clinical practice. However, there was no differences in PT, or aPTT between pregnant and nonpregnant reconstituted samples of same concentration except factor VIII. The higher factor VIII in pregnant plasma might have resulted in better clot stiffness supplementing higher fibrinogen. Synthetic fibrinogen would have been an alternative to pregnant plasma, but it is expensive. However, in practice, transfusion with cryoprecipitate is used which contains higher Factor VIII and fibrinogen. Third, we did not measure hematocrit value in each diluted sample and the extent of contribution of varying red blood cells to clot formation, and hence the effect on Quantra signals could not be assessed. The volume of the blood at each concentration was not sufficient to perform hematocrit analysis for all samples.
In conclusion, this in-vitro study demonstrates a good correlation between Quantra CS, FCS and laboratory fibrinogen. Further studies should investigate the performance of Quantra in clinical circumstances and confirm its ability to guide management of obstetric hemorrhage.
References
O’Brien KL, Shainker SA, Lockhart EL. Transfusion management of obstetric hemorrhage. Transfus Med Rev. 2018;32(4):249–55. https://doi.org/10.1016/j.tmrv.2018.05.003.
Practice Bulletin No. 183 Summary: Postpartum Hemorrhage (2017). Obstet Gynecol 130(4):923–925. https://doi.org/10.1097/AOG.0000000000002346.
Clark SL. Obstetric hemorrhage. Semin Perinatol. 2016;40(2):109–11. https://doi.org/10.1053/j.semperi.2015.11.016.
Main EK, Goffman D, Scavone BM, Low LK, Bingham D, Fontaine PL, Gorlin JB, Lagrew DC, Levy BS, National Partnership for Maternal S, Council on Patient Safety in Women’s Health C. National partnership for maternal safety: consensus bundle on obstetric hemorrhage. Obstet Gynecol. 2015;126(1):155–62. https://doi.org/10.1097/AOG.0000000000000869.
Fedoruk K, Seligman KM, Carvalho B, Butwick AJ. Assessing the association between blood loss and postoperative hemoglobin after cesarean delivery: A prospective study of 4 blood loss measurement modalities. Anesth Analg. 2019;128(5):926–32. https://doi.org/10.1213/ANE.0000000000003449.
Saoud F, Stone A, Nutter A, Hankins GD, Saade GR, Saad AF. Validation of a new method to assess estimated blood loss in the obstetric population undergoing cesarean delivery. Am J Obstet Gynecol. 2019. https://doi.org/10.1016/j.ajog.2019.06.022.
Lumbreras-Marquez MI, Reale SC, Carusi DA, Robinson JN, Scharf N, Fields KG, Farber MK. Introduction of a novel system for quantitating blood loss after vaginal delivery: A retrospective interrupted time series analysis with concurrent control group. Anesth Analg. 2020;130(4):857–68. https://doi.org/10.1213/ANE.0000000000004560.
Toulon P, Ozier Y, Ankri A, Fleron MH, Leroux G, Samama CM. Point-of-care versus central laboratory coagulation testing during haemorrhagic surgery. A multicenter study. Thromb Haemost. 2009;101(2):394–401.
Corey FS, Walker WF. Sonic estimation of elasticity via resonance: A new method of assessing hemostasis. Ann Biomed Eng. 2016;44(5):1405–24. https://doi.org/10.1007/s10439-015-1460-y.
Gillissen A, van den Akker T, Caram-Deelder C, Henriquez D, Bloemenkamp KWM, de Maat MPM, van Roosmalen JJM, Zwart JJ, Eikenboom J, van der Bom JG, TeMp OHSG. Coagulation parameters during the course of severe postpartum hemorrhage: a nationwide retrospective cohort study. Blood Adv. 2018;2(19):2433–42. https://doi.org/10.1182/bloodadvances.2018022632.
Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H, Sibony O, Mahieu-Caputo D, Hurtaud-Roux MF, Huisse MG, Denninger MH, de Prost D, Group PPHS. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007;5(2):266–73. https://doi.org/10.1111/j.1538-7836.2007.02297.x.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Baryshnikova E, Di Dedda U, Ranucci M. A comparative study of SEER sonorheometry versus standard coagulation tests, rotational thromboelastometry, and multiple electrode aggregometry in cardiac surgery. J Cardiothorac Vasc Anesth. 2019;33(6):1590–8. https://doi.org/10.1053/j.jvca.2019.01.011.
Groves DS, Welsby IJ, Naik BI, Tanaka K, Hauck JN, Greenberg CS, Winegar DA, Viola F. Multicenter evaluation of the quantra QPlus system in adult patients undergoing major surgical procedures. Anesth Analg. 2020;130(4):899–909. https://doi.org/10.1213/ANE.0000000000004659.
Zghaibe W, Scheuermann S, Munting K, Blaudszun G, Besser M, Ortmann E, Klein AA. Clinical utility of the Quantra((R)) point-of-care haemostasis analyser during urgent cardiac surgery. Anaesthesia. 2020;75(3):366–73. https://doi.org/10.1111/anae.14942.
Theusinger OM, Levy JH. Point of care devices for assessing bleeding and coagulation in the trauma patient. Anesthesiol Clin. 2013;31(1):55–65. https://doi.org/10.1016/j.anclin.2012.10.006.
Liu C, Guan Z, Xu Q, Zhao L, Song Y, Wang H. Relation of thromboelastography parameters to conventional coagulation tests used to evaluate the hypercoagulable state of aged fracture patients. Medicine (Baltimore). 2016;95(24): e3934. https://doi.org/10.1097/MD.0000000000003934.
Sharma S, Kumar S, Tewari P, Pande S, Murari M. Utility of thromboelastography versus routine coagulation tests for assessment of hypocoagulable state in patients undergoing cardiac bypass surgery. Ann Card Anaesth. 2018;21(2):151–7. https://doi.org/10.4103/aca.ACA_174_17.
Reale SC, Farber MK. Point-of-care coagulation testing for obstetric hemorrhage: time for a theranostic approach? Int J Obstet Anesth. 2019;38:1–3. https://doi.org/10.1016/j.ijoa.2019.04.001.
Sharma SK, Vera RL, Stegall WC, Whitten CW. Management of a postpartum coagulopathy using thrombelastography. J Clin Anesth. 1997;9(3):243–7. https://doi.org/10.1016/s0952-8180(97)00026-3.
Tanaka KA, Bharadwaj S, Hasan S, Judd M, Abuelkasem E, Henderson RA, Chow JH, Williams B, Mazzeffi MA, Crimmins SD, Malinow AM. Elevated fibrinogen, von Willebrand factor, and Factor VIII confer resistance to dilutional coagulopathy and activated protein C in normal pregnant women. Br J Anaesth. 2019;122(6):751–9. https://doi.org/10.1016/j.bja.2019.02.012.
Funding
A portion of the support from HemoSonics, LLC, Charlottesville, Virginia, USA (Hemosonic Quantra Analyzer, QPlus cartridges, laboratory analysis).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kodali, B.S., Karuppiah, A., Bharadwaj, S. et al. Efficacy of sonorheometry point of the care device in determining low fibrinogen levels in pregnant blood: an invitro dilution and reconstitution study. J Clin Monit Comput 36, 1423–1431 (2022). https://doi.org/10.1007/s10877-021-00782-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-021-00782-1