Abstract
Continuous monitoring of the respiratory rate is crucial in an acute care setting. Contact respiratory monitoring modalities such as capnography and thoracic impedance pneumography are prone to artifacts, causing false alarms. Moreover, their cables can restrict patient behavior or interrupt patient care. A microwave Doppler sensor is a novel non-contact continuous respiratory rate monitor. We compared respiratory rate measurements performed with a microwave Doppler sensor mounted on the ceiling of an intensive care unit with those obtained by conventional methods in conscious and spontaneously breathing patients. Participants’ respiratory rate was simultaneously measured by visual counting of chest wall movements for 60 s; a microwave Doppler sensor; capnography, using an oxygen mask; and thoracic impedance pneumography, using electrocardiogram electrodes. Bland–Altman analysis for repeated measures was performed to calculate bias and 95% limits of agreement between the respiratory rate measured by visual counting (reference) and that measured by each of the other methods. Among 52 participants, there were 336 (microwave Doppler sensor), 275 (capnography), and 336 (thoracic impedance pneumography) paired respiratory rate data points. Bias (95% limits of agreement) estimates were as follows: microwave Doppler sensor, 0.3 (− 6.1 to 6.8) breaths per minute (bpm); capnography, − 1.3 (− 8.6 to 6.0) bpm; and thoracic impedance pneumography, 0.1 (− 4.4 to 4.7) bpm. Compared to visual counting, the microwave Doppler sensor showed small bias; however, the limits of agreement were similar to those observed in other conventional methods. Our monitor and the conventional ones are not interchangeable with visual counting.
Trial registration number: UMIN000032021, March/30/2018
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Patients in the acute care setting require continuous monitoring of respiratory rate because it can predict serious adverse events such as unexpected intensive care unit (ICU) admission, cardiopulmonary arrest, and in-hospital mortality [1,2,3]. Various acute risk evaluation systems (early warning scoring system [4] or quick Sequential Organ Failure Assessment (SOFA) score [5]), or ROX index which predict progression to tracheal intubation in patients using nasal high-flow cannula, include respiratory rate as part of their composition [6, 7]. Continuous, not cross-sectional, physiological monitoring based on these scores or index is useful for the early detection of patient deterioration; therefore, continuous monitoring of the respiratory rate is also important for the safety of spontaneously breathing patients in the ICUs, which is the same as that in acute care wards.
In ICUs, both capnography and thoracic impedance pneumography, which are conventional wired contact monitors, are currently used to measure respiratory rates in spontaneously breathing patients. The accuracy of thoracic impedance pneumography, which is affected by many factors (i.e., movement of patients, physiological motion of the thoracic wall such as cough or crying, or electrocardiogram electrode placement) [8, 9], has a high chance for false alarms. Although capnography is generally reported to be more accurate than the thoracic impedance pneumography, it may not work with a nasal high-flow cannula or noninvasive positive pressure ventilation, which are often used in conservative treatment for acute respiratory failure. Existing contact monitors with high false alarm rates or numerous sensor cables can often interrupt patient care in the ICUs [10].
By remotely obtaining the physiological signals from the patients, there is potential to modify the workflow, improve patient safety, reduce the cables, and relieve patient restrictions [11]. Thus far, there have been growing demands for a non-contact, wireless, feasible, and reliable monitor for respiratory rate [10, 12]. Recently, research about non-contact respiratory monitors such as RGB video camera [11], infrared camera systems [13, 14], and thermal imaging camera [15] is increasing. However, these novel technologies are currently under development; therefore, no device is recognized as the gold standard respiratory monitor for everyday clinical practice.
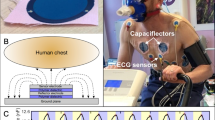
A microwave Doppler sensor is a non-contact device that uses the principle of Doppler shift to detect patient’s movement. In areas of nursing care, a commercialized sensor can be fixed on the ceiling and used for monitoring the abnormal body movements or continuously monitoring the respiratory rates in the elderly. A microwave Doppler sensor has the following advantages compared to RGB, infrared, or thermal imaging camera: (1) microwaves can pass through blankets or medical devices on the patient’s body or face, (2) the patients do not need to sit facing the sensor for measurement, (3) not affected by ambient light or heat sources, and (4) maintaining patient anonymity. Therefore, this sensor can be applied in various situations; however, the utility of the sensor in an acute care setting, including ICUs, has not been evaluated.
This study evaluated the agreement of respiratory rate measured with a microwave Doppler sensor with that measured by each of three conventional methods in spontaneously breathing patients in an ICU setting.
2 Methods
2.1 Participants, measurements, and equipment
This study was conducted between March and August 2018 at the ICU of Yokohama City University Hospital, which includes eight beds (three private rooms and five beds in open wards with curtains that separate individuals). We enrolled consecutive participants aged 20 years or older, who were awake, breathing spontaneously, and required oxygen therapy via a face mask. We excluded patients who needed mechanical ventilation at the time of ICU admission or during hospitalization.
Standard monitoring equipment of our ICU, which includes a pulse oximeter, arterial blood pressure, and electrocardiogram connected to the bedside monitor (IntelliVue™ MX800; Philips, Eindhoven, The Netherlands), was used for all participants. The initial oxygen flow rate via an oxygen mask was 5 L/min, adjusted at the discretion of attending ICU physician.
Visual counting of the chest wall movements of each participant was performed over 60 s by a nurse and was considered a reference respiratory rate. Respiratory rate was also measured using a microwave Doppler sensor, capnography monitor, and thoracic impedance pneumography. The body position during the measurement was not specified.
The microwave Doppler sensor (KONICA MINOLTA, INC., Tokyo, Japan) operates on the principle of Doppler shift. This sensor transmits 2.4-GHz microwaves toward the participant, receives the reflected microwaves, and detects periodic and minute movements of body surface based on phase differences between the transmitted and reflected waves. The baseband signals were separated into signal of respiration and other signals through band-pass filters, which removed the other signals. Respiratory rate was calculated using the respiratory rate waveform constructed during this processing. Details of the microwave Doppler sensor principle are described in Supplementary information 1. The microwave Doppler sensor was installed onto the ceiling above each bed, with an approximate distance of 1.9 m between the bed and the sensor. Although the manufacturer recommends that this sensor be installed just above the center of the bed, we had to install it approximately 1 m away from the center of the bed because of preexisting equipment mounted onto the ceiling. Before starting the study, the irradiation range of microwaves from the sensor was investigated, and bed placement was adjusted within the irradiation area.
Capnometric monitoring of respiratory rate involved an oxygen mask with the expiratory gas sampling port (EcoLite™, INTERSURGICAL, Wokingham, UK), which was connected to a sidestream-type capnometer (LoFlo sidestream CO2 Module™, Philips, Eindhoven, The Netherlands), incorporated into a bedside monitor. Thoracic impedance pneumography consisted of three electrocardiogram electrodes (Vitrode V®, NIHON KOHDEN CORPORATION, Tokyo, Japan), positioned as recommended by the manufacturer and connected to the bedside monitor. Respiratory rate was calculated based on the change in impedance recorded across electrodes during breathing.
2.2 Data acquisition and outcome
Data on participants’ background characteristics and comorbidities recorded within one month of ICU admission were collected from their medical records. SOFA scores were calculated from the data obtained at admission to the ICU. Respiratory rate measurements were performed once per hour after ICU admission, aiming for a total of five measurements per patient obtained by a nurse in-charge, while participant respiratory pattern was stable. The nurse in-charge counted the chest wall movements for 60 s per patient. Immediately after the completion of visual counting, the respiratory rate displayed on the bedside monitor, measured with capnography and thoracic impedance pneumography, was recorded. The respiratory rates measured by capnography and thoracic impedance pneumography displayed on the monitor were derived from the last 8 and 5 waveform samples, respectively. Participant body position (supine or lateral), staff working shift (daytime or nighttime), and room status (private room or open ward) at the time of visual counting were also recorded. The respiratory rate of the microwave Doppler sensor was calculated by the rolling average of 90 s, based on 3 consecutive respiratory rate values, and calculated every 30 s. The microwave Doppler sensor obtained data at 1-min intervals, which were stored on a dedicated server. Data recorded at the same time as that of the visual respiratory rate measurement were extracted from the database and used for analysis. Data from participants with up to five measurement periods were included in the final analysis.
The primary outcomes were estimates of bias and 95% limits of agreement (LOA) (bias ± 1.96 standard deviation [SD] of bias) between respiratory rates determined by visual counting and those determined using the microwave Doppler sensor; 95% LOA represents the precision of the index device. Secondary outcomes were estimates of bias and 95% LOA between respiratory rates obtained by visual counting and those obtained by two conventional methods (i.e., capnography and thoracic impedance pneumography). As an additional secondary outcome, the Clarke Error Grid (CEG) analysis was performed to quantify the impact of the observed differences between devices on the clinical accuracy and consequences for clinical decisions [16].
2.3 Sample size calculation and statistical analysis
We did not calculate the required sample size before starting the study. Sample size calculations for Bland–Altman analysis are controversial, as this analysis is not a statistical test [17]. In addition, sample size calculations for repeated measures are not clearly established [17]. Based on the study feasibility, we set a priori a recruitment target of at least 60 participants.
Patient characteristics and respiratory rate data were imputed into an Excel (Microsoft Corporation, Washington, USA) spreadsheet. Irregular artifact values were removed before statistical analysis. A correlation between respiratory rate obtained by each device and that obtained by visual counting was evaluated using the Spearman correlation coefficient test. Bias and 95% LOA estimates between the respiratory rate measured with each device and that measured by visual counting were calculated by Bland–Altman analysis for repeated measures, using a mixed model, as each individual underwent multiple observations [18]. Bias and SD were estimated by the overall intercept, and marginal SD associated with repeated measures was calculated using a linear mixed-effects regression model, standardizing the data. In this model, the bias between respiratory rate obtained with each device and that obtained by visual counting was used as a response variable. Participants’ body position, staff working shift (daytime or nighttime), and room status (private room or open ward) were included as fixed-effect variables. The random intercept for participants was included in the mixed model. The clinical interchangeability range of 95% LOA was set as ± 3 breaths per minute (bpm) [19]. A post-hoc subgroup analysis was performed to evaluate the bias and LOA between the respiratory rate measured using microwave Doppler sensor and that measured by visual counting for body position. All data were classified into two groups according to the body position: supine or lateral position. Bland–Altman analysis for repeated measures was performed for calculating the estimated bias and SD using the staff working shift and room status as the fixed-effect variables as with the main analysis.
The CEG analysis was performed by breaking down a scatterplot of the reference standard and the devices into five regions. The reference lines in the CEG that mark the boundaries between correct and incorrect treatment decisions were defined with reference to a previous research [20]. The CEG 5 regions are as follows: region A encloses points within 20% of the reference measurement, region B contains points outside 20% of the reference but not leading to unnecessary treatment, region C contains points leading to unnecessary treatment, region D points indicate a potentially dangerous failure to detect bradypnea or tachypnea, and region E represents points leading to reversed treatment decisions (e.g., tachypnea for bradypnea and vice versa). The sensitivity and specificity for tachypnea, defined as a respiratory rate of more than 21 bpm, were calculated.
All data were reported as mean ± SD, median (interquartile range IQR), or count (percentage), as suitable. For all statistical analyses, Prism 7.0 (GraphPad, Inc., San Diego, CA.) and R software, version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria), were used.
3 Results
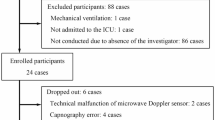
We obtained consent from 60 prospective participants. We excluded eight participants who had not been admitted to the ICU postoperatively. Therefore, data collected from a total of 52 participants were analyzed. The microwave Doppler sensor and thoracic impedance pneumography each obtained 336 data points. Capnography obtained 275 data points after removing 5 data points identified as artifacts (Fig. 1). This difference was due to the gradual reduction in oxygen supplementation and switch to a nasal cannula or room air breathing, which are typically observed in clinical practice. The microwave Doppler sensor and thoracic impedance pneumography did not include irregular artifacts. The median (IQR) respiratory rate obtained by visual counting for all participants was 16 (13–20) bpm (range 7–29).
Most participants (96.2%) were postoperative cases, and the median (IQR) SOFA score was 2 (1–3). One patient had a history of sleep apnea syndrome. More than half of the respiratory rate data were acquired from participants in the supine position, in the open ward, and during nighttime (Tables 1 and 2).
Figure 2A shows the Bland–Altman plot between respiratory rate estimates obtained using the microwave Doppler sensor and those obtained by visual counting. Estimated bias (95% LOA) between the respiratory rate obtained using the microwave Doppler sensor and that obtained by visual counting was 0.3 (− 6.1 to 6.8) bpm. In the post-hoc analysis, estimated bias (95% LOA) between the respiratory rate obtained using microwave Doppler sensor and that obtained by visual counting was 0.2 (− 6.5 to 6.9) bpm for the supine position and 0.4 (− 5.6 to 6.4) bpm for the lateral position (Table 3).
Bland–Altman plot comparing respiratory rates measured by three devices and visual counting. The Bland–Altman plot shows the respiratory rate measured by microwave Doppler sensor (A), capnography (B), and thoracic impedance pneumography and visual counting (C). Bias and 95% limits of agreement (bias ± 1.96 standard deviation of bias) were calculated using a linear mixed-effects regression model. awRR, respiratory rate measured by capnography; bpm, breaths per minute; ecgRR, respiratory rate measured by thoracic impedance pneumography; mdsRR, respiratory rate measured by the microwave Doppler sensor; nsRR, respiratory rate measured by visual counting by a nurse in charge; upper limit, upper 95% limit of agreement (bias + 1.96 standard deviation of bias); lower limit, lower 95% limit of agreement (bias – 1.96 standard deviation of bias)
Estimated bias (95% LOA) between the respiratory rate obtained by capnography and that obtained by visual counting was − 1.3 (− 8.6 to 6.0) bpm (Fig. 2B); the corresponding values for thoracic impedance pneumography and visual counting were 0.1 (− 4.4 to 4.7) bpm (Fig. 2C).
The correlation coefficients between the respiratory rate calculated by visual counting and that calculated with each device were 0.67 (95% confidence interval [CI] 0.61 to 0.73) for the microwave Doppler sensor, 0.69 (95% CI 0.62 to 0.75) for capnography, and 0.86 (95% CI 0.83 to 0.89) for thoracic impedance pneumography. The CEG analysis are indicated in Fig. 3A–C. The percentages of data points in regions A–E and diagnostic accuracy for tachypnea are presented in Table 4. For the adequate treatment decision regions, i.e., regions A or B 97.3% was shown for microwave Doppler sensor, 97.4% for capnography, and 99.4% for thoracic impedance pneumography (Table 4). Few data points, for the three devices, were within regions C, D, or E, which indicate a low potential risk leading to failure to treat, unnecessary treatment, or the confusion of treatment between bradypnea and tachypnea (Table 4). The sensitivity and specificity to detect tachypnea (respiratory rate of more than 21 bpm) of the three devices are indicated in Table 4. The sensitivity and specificity for microwave Doppler sensor were 0.50 (95% CI 0.37–0.63) and 0.94 (95% CI 0.91–0.97), respectively.
Clark Error Grid analysis for respiratory rate measured using microwave Doppler sensor (A), capnography (B), thoracic impedance pneumography (C). Region A encloses points within 20% of the reference; region B contains points outside 20% of the reference, but not leading to unnecessary treatment; region C contains points leading to unnecessary treatment; region D indicates a potentially dangerous failure to detect bradypnea or tachypnea; and region E represents points where events are confusing (e.g., bradypnea for tachypnea or vice versa). awRR, respiratory rate measured by capnography; CI, confidence interval; ecgRR, respiratory rate measured by thoracic impedance pneumography; mdsRR, respiratory rate measured by the microwave Doppler sensor; nsRR, respiratory rate measured by visual counting by a nurse in charge
4 Discussion
The present study demonstrated that the microwave Doppler sensor has a small bias but relatively low precision, compared to those of visual counting of the respiratory wall motion, as it was outside of the range (± 3 bpm) and considered clinically interchangeable. Similarly, in the present study, both capnography and thoracic impedance pneumography showed low precision and were outside the range of the set interchangeability. In the CEG analysis, the three devices had relatively high clinical accuracy and low potential risk leading to inadequate treatment.
The reason the microwave Doppler sensor was associated with a relatively large LOA is unknown. When compared to the supine position, the lateral position may be considered a disadvantage for the effective generation of the Doppler shift because the respiratory chest movements occur vertically to the microwave transmitted from the sensor mounted on the ceiling. However, in the post-hoc analysis, there were no significant differences between LOA for the lateral position and that for the supine position. One possibility may be due to the measuring error caused by the sensor position. This sensor, designed to detect movements of a patient placed just below it, should be installed on the ceiling directly above the bed. However, we had to install it on the ceiling approximately 1 m off the bed center, as other equipment was already placed on the ceiling. The intensity of the transmitted waves decreases as the horizontal distance between the patient and the sensor increases because microwaves that have high directivity irradiate areas immediately below the sensor. In addition, increasing the distance between patient and sensor affects reception of microwaves that attenuate in proportion to the square of distance. These factors may have made it difficult for sensors to distinguish between waveform signals related to participant respiration and the surrounding artifacts such as movement of medical staff. To obtain optimal signals for respiratory rate analysis, sensors may need to be placed closer to the patient, for example, under the bed rather than on the ceiling. Further research will be needed to determine whether these efforts will improve the precision of the sensor.
Demands for a reliable wireless monitor have been increasing recently, in both ICUs and acute care settings [10, 12]. It is currently unclear whether non-contact monitors using camera or radar are ideal wireless monitors in the acute care setting. Wireless wearable monitors seem to be more versatile than non-contact monitors using a camera or radar. However, these monitors may have a risk of data dropout caused by the interruption of network [21], or for the cybersecurity [22]. While a microwave Doppler sensor does not have these disadvantages, it is important that this sensor has some limitations (i.e., sensor detective area is fixed, or unable to detect obstructive respiratory events, or relatively low precision) in replacing conventional monitors. However, we believe that the microwave Doppler sensor unaffected by the dark environment at nighttime or by obstacles or positions on patients, can help reduce the workload of nurses at nighttime and detect patient deterioration at an early stage in the acute care setting. For use in ICUs, where high precision is particularly required, future technological innovations for artifact removal algorithms or for reduction in false alarms may be useful for better accuracy.
The LOA between capnography and visual counting of the respiratory chest wall movement was also large and outside the range of interchangeability. This is an unexpected finding, as good agreement between capnography and visual counting has previously been reported [23, 24]. In fact, capnography has been chosen as the gold standard for respiratory rate monitoring in these studies. The reason for this deviation is unknown but may be among the following. First, the accuracy of capnography-based estimates in non-intubated patients may be affected by the positional relationship between expiratory gas flow and sampling line of the capnometer [25,26,27,28,29]. Our study participants may have moved the oxygen mask away from its ideal position to alleviate discomfort. Second, our participants were largely in the postoperative stage, which might have played a role; for example, opioids can change the distribution of nasal vs. mouth breathing [25,26,27,28,29]. Third, the time frame for collecting data reflecting the capnography respiratory rate displayed on the monitor did not completely match the time frame for visually counting the respiratory rate. To evaluate the impact of this, it may be needed to consider using the respiratory rate derived from the counting of individual capnography waveform, in a further study.
Thoracic impedance pneumography was associated with comparable or even better precision and LOA than the microwave Doppler technique. It is believed that thoracic impedance pneumography is generally prone to artifacts, especially from patients’ body movements. Further study is required to understand to what extent the microwave Doppler method is resistant to artifacts.
The reasons for using the respiratory rate obtained by visual counting were as following; first, to our knowledge, the utility of the microwave Doppler sensor in an acute care setting has not been evaluated. We aimed to evaluate the agreement with respiratory rate obtained by visual counting, which is still widely used in daily clinical practice in acute care or general wards, rather than with existing devices. Second, since the decision to continue or terminate oxygen administration was made from a medical perspective, we were also concerned about the uncertainty of the number of data that could potentially be obtained. However, respiratory rate obtained by visual counting of nurse have been suggested the problems about the inter-observer variation [30, 31]. In our study, we tried to ensure the quality of the reference as much as possible by using the respiratory rate obtained by an experienced ICU nurse as a reference. However, we are concerned about the impact of not being able to fix the observer to one person on our results. In the sensitivity analysis, the bias and 95% LOA for microwave Doppler sensor were similar even when using capnography as a reference: estimated bias (95% LOA) was 1.6 (− 5.4 to 8.6) bpm.
This study has several limitations. First, we performed a single-center study, and most participants were postsurgical cases. Caution should therefore be exercised when applying this procedure on other critically ill patients (e.g., medical, emergency, or pediatric) or patients treated in the general wards. Second, our protocol did not evaluate the feasibility of the microwave sensor use as a continuous respiratory rate monitor for a prolonged period. Third, because the respiratory rate observed in this study ranged from 7 to 29 bpm and there were few data points for extreme tachypnea and bradypnea, we could not conclude whether this monitor functions appropriately at extremely high or low respiratory rates. Similarly, whether this monitor works in the presence of abnormal breathing patterns (e.g., see-saw motion as seen in severe respiratory failure and Cheyne–Stokes pattern) remains to be elucidated.
In conclusion, the non-contact microwave Doppler sensor had a small bias but relatively low precision. In our ICU, the respiratory rate obtained by this sensor was not interchangeable with that obtained by visual counting. Technological innovation or adjustments to the installation location of the microwave Doppler sensor, which will reduce artifacts, may be necessary to obtain good agreement.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Buist M, Bernard S, Nguyen TV, Moore G, Anderson J. Association between clinically abnormal observations and subsequent in-hospital mortality: a prospective study. Resuscitation. 2004;62:137–41. https://doi.org/10.1016/j.resuscitation.2004.03.005.
Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98:1388–92. https://doi.org/10.1378/chest.98.6.1388.
Lynn LA, Curry JP. Patterns of unexpected in-hospital deaths: a root cause analysis. Patient Saf Surg. 2011;5:3. https://doi.org/10.1186/1754-9493-5-3.
Sutherasan Y, Theerawit P, Suporn A, Nongnuch A, Phanachet P, Kositchaiwat C. The impact of introducing the early warning scoring system and protocol on clinical outcomes in tertiary referral university hospital. Ther Clin Risk Manag. 2018;14:2089–95. https://doi.org/10.2147/TCRM.S175092.eCollection2018.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10. https://doi.org/10.1001/jama.2016.0287.
Roca O, Caralt B, Messika J, Samper M, Sztrymf B, Hernández G, García-de-Acilu M, Frat JP, Masclans JR, Ricard JD. An index combining respiratory rate and oxygenation to predict outcome of nasal high flow therapy. Am J Respir Crit Care Med. 2019;199:1368–76. https://doi.org/10.1164/rccm.201803-0589OC.
Roca O, Messika J, Caralt B, García-de-Acilu M, Sztrymf B, Ricard JD, Masclans JR. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016;35:200–5. https://doi.org/10.1016/j.jcrc.2016.05.022.
Wilkinson JN, Thanawala VU. Thoracic impedance monitoring of respiratory rate during sedation—Is it safe? Anaesthesia. 2009;64:455–6. https://doi.org/10.1111/j.1365-2044.2009.05908.x.
Drummond GB, Nimmo AF, Elton RA. Thoracic impedance used for measuring chest wall movement in postoperative patients. Br J Anaesth. 1996;77:327–32. https://doi.org/10.1093/bja/77.3.327.
Poncette AS, Mosch L, Spies C, Schmieding M, Schiefenhövel F, Krampe H, Balzer F. Improvements in patient monitoring in the intensive care unit: Survey study. J Med Internet Res. 2020;22: e19091. https://doi.org/10.2196/19091.
Addison PS, Jacquel D, Foo DMH, Antunes A, Borg UR. Video-based physiologic monitoring during an acute hypoxic challenge: Heart rate, respiratory rate, and oxygen saturation. Anesth Analg. 2017;125:860–73. https://doi.org/10.1213/ANE.0000000000001989
Poncette AS, Spies C, Mosch L, Schieler M, Weber-Carstens S, Krampe H, Balzer F. Clinical requirements of future patient monitoring in the intensive care unit: Qualitative study. JMIR Med Inform. 2019;7: e13064. https://doi.org/10.2196/13064.
Chan P, Wong G, Nguyen TD, Nguyen T, McNeil J, Hopper I. Estimation of respiratory rate using infrared video in an inpatient population: an observational study. J Clin Monit Comput. 2020;34:1275–84. https://doi.org/10.1007/s10877-019-00437-2.
Kwon HM, Ikeda K, Kim SH, Thiele RH. Non-contact thermography-based respiratory rate monitoring in a post-anesthetic care unit. J Clin Monit Comput. 2020;25:1–7. https://doi.org/10.1007/s10877-020-00595-8.
Elphick HE, Alkali AH, Kingshott RK, Burke D, Saatchi R. Exploratory study to evaluate respiratory rate using a thermal imaging camera. Respiration. 2019;97:205–12. https://doi.org/10.1159/000490546.
Clarke WL, Cox D, Gonder-Frederick LA, Carter W, Pohl SL. Evaluating clinical accuracy of systems for self-monitoring of blood glucose. Diabetes Care. 1987;10:622–8. https://doi.org/10.2337/diacare.10.5.622.
Montenij LJ, Buhre WF, Jansen JR, Kruitwagen CL, de Waal EE. Methodology of method comparison studies evaluating the validity of cardiac output monitors: a stepwise approach and checklist. Br J Anaesth. 2016;116:750–8. https://doi.org/10.1093/bja/aew094.
Parker RA, Weir CJ, Rubio N, Rabinovich R, Pinnock H, Hanley J, Lucy McCloughan J, Drost EM, Mantoani LC, MacNee W, McKinstry B. Application of mixed effects limits of agreement in the presence of multiple sources of variability: exemplar from the comparison of several devices to measure respiratory rate in COPD patients. PLoS ONE. 2016;11: e0168321. https://doi.org/10.1371/journal.pone.0168321.eCollection2016.
Bergese SD, Mestek ML, Kelley SD, McIntyre R Jr, Uribe AA, Sethi R, Watson JN, Addison PS. Multicenter study validating accuracy of a continuous respiratory rate measurement derived from pulse oximetry: a comparison with capnography. Anesth Analg. 2017;124:1153–9. https://doi.org/10.1213/ANE.0000000000001852.
Breteler MJM, KleinJan EJ, Dohmen DAJ, Leenen LPH, van Hillegersberg R, Ruurda JP, van Loon K, Blokhuis TJ, Kalkman CJ. Vital signs monitoring with wearable sensors in high-risk surgical patients: A clinical validation study. Anesthesiology. 2020;132:424–39. https://doi.org/10.1097/ALN.0000000000003029.
Clifton L, Clifton DA, Pimentel MAF, Watkinson PJ, Tarassenko L. Predictive monitoring of mobile patients by combining clinical observations with data from wearable sensors. IEEE J Biomed Heal Inform. 2014;18:3. https://doi.org/10.1109/JBHI.2013.2293059.
Michard F, Bellomo R, Taenzer A. The rise of ward monitoring: opportunities and challenges for critical care specialists. Intensive Care Med. 2019;45:671–3. https://doi.org/10.1007/s00134-018-5384-5.
Frasca D, Geraud L, Charriere JM, Debaene B, Mimoz O. Comparison of acoustic and impedance methods with mask capnometry to assess respiration rate in obese patients recovering from general anaesthesia. Anaesthesia. 2015;70:26–31. https://doi.org/10.1111/anae.12799.
Mimoz O, Benard T, Gaucher A, Frasca D, Debaene B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br J Anaesth. 2012;108:872–5. https://doi.org/10.1093/bja/aer510.
Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006;104:228–34. https://doi.org/10.1097/00000542-200602000-00005.
Phillips JS, Pangilinan LP, Mangalindan ER, Booze JL, Kallet RH. A comparison of different techniques for interfacing capnography with adult and pediatric supplemental oxygen masks. Respir Care. 2017;62:78–85. https://doi.org/10.4187/respcare.05111.
van Loon K, van Rheineck Leyssius AT, van Zaane B, Denteneer M, Kalkman CJ. Capnography during deep sedation with propofol by nonanesthesiologists: a randomized controlled trial. Anesth Analg. 2014;119:49–55. https://doi.org/10.1213/ANE.0b013e3182a1f0a2.
Gaucher A, Frasca D, Mimoz O, Debaene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask(R) in extubated patients receiving supplemental oxygen after surgery. Br J Anaesth. 2012;108:316–20. https://doi.org/10.1093/bja/aer383.
Yazigi A, Zeeni C, Richa F, Chalhoub V, Sleilaty G, Noun R. The accuracy of non-invasive nasal capnography in morbidly obese patients after bariatric surgery. Middle East J Anaesthesiol. 2007;19:483–94.
Brabrand M, Hallas P, Folkestad L, Lautrup-Larsen CH, Brodersen JB. Measurement of respiratory rate by multiple raters in a clinical setting is unreliable: A cross-sectional simulation study. J Crit Care. 2018;44:404–6. https://doi.org/10.1016/j.jcrc.2017.12.020.
Lim WS, Carty SM, Macfarlane JT, Anthony RE, Christian J, Dakin KS, Dennis PM. Respiratory rate measurement in adults–how reliable is it? Respir Med. 2002;96:31–3. https://doi.org/10.1053/rmed.2001.1203.
Funding
This study was supported by KONICA MINOLTA, INC (Tokyo, Japan). The microwave Doppler sensor used in this study was provided by KONICA MINOLTA, INC. The company was not involved in the study design, collection, analysis, or interpretation of data, writing of the report, or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
HT: literature search, data collection, manuscript preparation, and manuscript review. MY: literature search, data collection, study design, data analysis, manuscript preparation, and manuscript review. ST: data collection, study design, and manuscript review. TM: study design, data analysis, manuscript preparation, and manuscript review. YS: study design, data analysis, and manuscript review. TG: study design and manuscript review.
Corresponding author
Ethics declarations
Conflict of interest
Shunsuke Takaki received funding for this study from KONICA MINOLTA, INC. The other authors have no competing interests to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of Yokohama City University Hospital (Approval No.: B171200001).
Consent to participate
We obtained consent to participate from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: Part of the data have been presented at the European Society of Anaesthesiology Congress 2019, Vienna, Austria, June 2019.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tanaka, H., Yokose, M., Takaki, S. et al. Evaluation of respiratory rate monitoring using a microwave Doppler sensor mounted on the ceiling of an intensive care unit: a prospective observational study. J Clin Monit Comput 36, 71–79 (2022). https://doi.org/10.1007/s10877-021-00733-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-021-00733-w