Abstract
Pressure support ventilation (PSV) should be titrated considering the pressure developed by the respiratory muscles (Pmusc) to prevent under- and over-assistance. The esophageal pressure (Pes) is the clinical gold standard for Pmusc assessment, but its use is limited by alleged invasiveness and complexity. The least square fitting method and the end-inspiratory occlusion method have been proposed as non-invasive alternatives for Pmusc assessment. The aims of this study were: (1) to compare the accuracy of Pmusc estimation using the end-inspiration occlusion (Pmusc,index) and the least square fitting (Pmusc,lsf) against the reference method based on Pes; (2) to test the accuracy of Pmusc,lsf and of Pmusc,index to detect overassistance, defined as Pmusc ≤ 1 cmH2O. We studied 18 patients at three different PSV levels. At each PSV level, Pmusc, Pmusc,lsf, Pmusc,index were calculated on the same breaths. Differences among Pmusc, Pmusc,lsf, Pmusc,index were analyzed with linear mixed effects models. Bias and agreement were assessed by Bland–Altman analysis for repeated measures. The ability of Pmusc,lsf and Pmusc,index to detect overassistance was assessed by the area under the receiver operating characteristics curve. Positive and negative predictive values were calculated using cutoff values that maximized the sum of sensitivity and specificity. At each PSV level, Pmusc,lsf was not different from Pmusc (p = 0.96), whereas Pmusc,index was significantly lower than Pmusc. The bias between Pmusc and Pmusc,lsf was zero, whereas Pmusc,index systematically underestimated Pmusc of 6 cmH2O. The limits of agreement between Pmusc and Pmusc,lsf and between Pmusc and Pmusc,index were ± 12 cmH2O across bias. Both Pmusc,lsf ≤ 4 cmH2O and Pmusc,index ≤ 1 cmH2O had excellent negative predictive value [0.98 (95% CI 0.94–1) and 0.96 (95% CI 0.91–0.99), respectively)] to identify over-assistance. The inspiratory effort during PSV could not be accurately estimated by the least square fitting or end-inspiratory occlusion method because the limits of agreement were far above the signal size. These non-invasive approaches, however, could be used to screen patients at risk for absent or minimal respiratory muscles activation to prevent the ventilator-induced diaphragmatic dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Pressure support ventilation (PSV) is a ventilatory mode that supports the pressure developed by respiratory muscles during inspiration (Pmusc) with an external positive pressure applied at the airway opening, synchronized with the inspiratory effort. Since PSV supports the spontaneous breathing effort it should be titrated on patient’s instantaneous Pmusc to prevent under- and over-assistance, i.e. PSV-induced respiratory muscle fatigue and atrophy, respectively [1]. Unfortunately, since Pmusc is not easily measured in clinical practice, the degree of support is in fact titrated taking into account the overall clinical appearance of the patient, few breathing pattern parameters as respiratory rate and tidal volume, and, finally the airway pressure (Paw) and airflow waveforms on the ventilator screen.
The esophageal pressure method is the clinical gold standard for Pmusc assessment [2], but it is seldom used in daily practice due its alleged invasiveness and complexity. The least square fitting [3] and the end-inspiratory occlusion methods [4] have been proposed as non-invasive alternatives. The least square fitting is the instantaneous computation of Pmusc derived by solving the equation of motion [5] by Paw, airflow, inspired volume, respiratory system elastance and resistance (Ers and Rrs, respectively) [3]. The end-inspiration occlusion method estimates the end-inspiratory Pmusc as the difference between the Paw applied by the ventilator during the inspiratory phase Paw and the plateau reached by Paw during an end-inspiratory airway occlusion maneuver [4]. Both these methods have been evaluated in physiological studies, conducted on relatively few patients [3, 4] but to our knowledge their validation against the “reference” Pes method is lacking. Thus, it is not clear whether they are sufficiently accurate to guide PSV titration in clinical practice.
The primary aim of this study was to compare Pmusc calculated from Pes with its estimation by the end-inspiration occlusion method (Pmusc,index) and by the least square fitting method (Pmusc,lsf) in critically ill patients ventilated with the PSV mode. The secondary aim was to test the accuracy of Pmusc,lsf and Pmusc,index to detect overassistance during PSV, defined as a near-passive patients (Pmusc ≤ 1 cmH2O).
2 Methods
2.1 Patients
Consecutive patients were recruited in the Intensive Care Unit of Poliambulanza Foundation Hospital (Brescia, Italy) between January 2016 and June 2016. Inclusion criteria were: age > 18 years; dependence on invasive mechanical ventilation (i.e. not ready to be weaned or having failed a spontaneous breathing trial on the day of the study [6]); PSV used as ventilatory mode; absence of flow limitation as assessed by maneuver of compression of the abdomen [7,8,9]. Patients were excluded in case of: hemodynamic instability (defined as mean arterial pressure < 60 mmHg, systolic arterial pressure > 180 mmHg, heart rate < 40/min or > 150/min); PaO2/FIO2 < 150 mmHg; pH < 7.35 with PaCO2 > 45 mmHg; contraindication to perform the maneuver of compression of the abdomen [7]; diagnosis of head injury, intracranial hemorrhage or cerebral ischemia. The protocol was approved by the local ethical committee (Comitato Etico Provinciale di Brescia, approval number NP2245). Written informed consent was obtained from the patient. In case of altered consciousness, the Ethics Committees waived the requirement for consent, as in Italy relatives are not regarded as legal representatives of the patient in the absence of a formal designation. Written informed consent was requested from all surviving patients as soon as they regained their mental competency. All investigations were conducted according to the principles expressed in the Declaration of Helsinki.
Esophageal pressure was measured by an esophageal balloon catheter (Marquat Gbm, Boissy-St-Léger Cedex, France) connected to a pressure transducer (AS3/CS3; Datex-Engstrom Division, Instrumentarium Corp., Helsinki, Finland). The esophageal balloon was introduced 40 cm from the nostril and inflated with 1 ml of air. The occlusion test was used to assess if the esophageal pressure was appropriately transduced [10]. The position of the balloon in the esophagus and its filling volume were optimized to obtain a ratio between esophageal and airway pressure swings during occlusion ranging between 0.8 and 1.2 [11, 12].
2.2 Study protocol
The clinical PSV level at the patient’s enrollment was defined as baseline PSV (PSbase). Successively, in order to explore a wide clinical range of PS assistance, maximal and minimal PS (PSmax and PSmin, respectively) were titrated as follows: PSmax was sought by progressively increasing the PS until disappearance of any sign of inspiratory muscle activity after inspiratory triggering. This was assessed by visual inspection of the Pes, airway pressure and airflow waveforms. For safety reasons, the peak airway pressure was limited to a maximum of 35 cmH2O, regardless of achieving complete absence of inspiratory muscles during inspiratory flow. The PSmin was identified by the lowest PS without dyspnea or rapid shallow breathing (respiratory rate/tidal volume < 100 min−1 l−1). Apart from the PS, all the other ventilatory variables remained constant throughout the study, as previously set by the attending physician.
The three PSV levels (PSbase, PSmin and PSmax) were delivered in random order to each patient for 20 min. At the end of each PS level period, five end-expiratory and end-inspiratory airway occlusion maneuvers were performed. These were performed at the end of each PS period in order to avoid carry over effects originating from the previous PS level. Each occlusion maneuver lasted 3 s and was separated by the previous and next maneuver by at least ten non-interrupted breaths.
2.3 Measurements and calculations
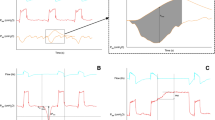
Immediately before the beginning of the occlusion maneuvers, Pes, Paw, airflow and volume curves were recorded for 5 min at the sampling rate of 100 Hz (Datex-Ohmeda S/5 Collect; Datex-Ohmeda Division, Instrumentarium Corp., Helsinki, Finland) and reconstructed from the sampled data through the R software (R Core Team, 2018, R Foundation for Statistical Computing, Vienna, Austria). The following parameters were measured on the occluded breaths: total positive end-expiratory pressure (PEEPtot), i.e. the airway pressure recorded during end-expiratory plateau, end-expiratory plateau esophageal pressure (Pexp,es), end-inspiratory plateau airway pressure (Pplat,aw), end-inspiratory plateau esophageal pressure (Pplat,es). The minimum acceptable length for a plateau was 0.25 s and its adequacy was judged by visual inspection [4]. Any occlusion pressure without a clearly identifiable plateau was discarded. Auto-PEEP was calculated as the difference between PEEPtot and the set PEEP. Airway occlusion pressure at 100 ms (P0.1) was measured as the drop in airway pressure after 100 ms of an inspiratory attempt with occluded airway [13]. The onset of inspiration was identified by a fall in the esophageal pressure, the end of inspiration was identified by the last positive value of the inspiratory flow. Pmusc was estimated as the maximal difference between the relaxation pressure of the chest wall (Pcw) and the esophageal pressure measured during inspiration. Pcw is the product of the inspired volume and the chest wall elastance (Ecw). Ecw was calculated as the ratio (Pplat,es − Pexp,es)/tidal volume. Patients were categorized as ‘near-passive’ if Pmusc was equal or lower than 1 cmH2O, all other patients being classified as ‘active’. The Pressure–Time Product (PTP) was computed as the area between Pcw and Pes during inspiration multiplied by the respiratory rate (Fig. 1, left panel).
Inspiratory effort assessed by esophageal pressure, least square fitting method and inspiratory occlusion method. Pes esophageal pressure, Pmusc inspiratory swing measured between elastic recoil pressure of chest wall and esophageal pressure, Pmusc,lsf Pmusc estimated with least square fitting method, Paw airway pressure, Pmusc,index Pmusc estimated with end-inspiratory occlusion method, PS pressure support level, PEEP positive end-expiratory pressure. a Esophageal pressure, continuous line: esophageal pressure; dashed line: elastic recoil pressure of the chest wall; dotted area: pressure–time product. b Least square fitting method, continuous line: Pmusc,lsf; dashed line: baseline at 0 cmH2O; dotted area: pressure–time product as calculated by least square fitting method. c End-inspiratory occlusion method, continuous line: airway pressure; dashed line: sum of PS and PEEP
2.4 The least square fitting method
The pressure applied to the respiratory system during ventilation (Pappl) can be calculated at any time t by the equation of motion as the sum of elastic pressure (Pel) and resistive pressure (Pres) on the basal pressure (P0) [5]:
Pel(t) is the product between V(t), the volume at the time t, and Ers. Pres(t) is calculated as the flow, V’(t), multiplied by Rrs. Finally, P0 corresponds to PEEPtot. Equation 1 can be rewritten as:
We calculated Ers and Rrs as the coefficients of V and V’, respectively, by fitting the equation of motion during PSmax. In this setting, based on previous report, we assumed that the inspiratory muscles were near totally relaxed, allowing a reliable calculation of passive respiratory mechanics [14, 15].
During assisted mechanical ventilation, Pappl is the sum of the airway pressure (Paw), generated by the mechanical ventilator, and Pmusc. Equation 2 can be rewritten as:
Equation 3 can be rearranged to estimate Pmusc with the least square fitting [3] (Pmusc,lsf):
PTPlsf was calculated as the area delimited by Pmusc,lsf (t) (Fig. 1, right panel).
2.5 The end-inspiratory occlusion method
Pmusc estimation with this method is also known as Pmusc,index or PMI [4]. Pmusc,index was calculated as the difference between Pplat,aw and the pressure applied by ventilator during the inspiratory phase:
where Pplat,aw is the sum of Pel and PEEPtot [16]:
Therefore, Eq. 5 can be rewritten as
and by rearrangements
Since autoPEEP is the difference between PEEPtot and PEEP,
Equation 9 makes evident that Pmusc,index includes both the pressure required to generate the tidal volume and the pressure necessary to overcome auto-PEEP while the Pmusc needed to overcome the resistive load remains undetected.
Pmusc, Pmusc,lsf, Pmusc,index, PTP and PTPlsf were calculated on each breath in which the inspiratory occlusion maneuver was performed.
Each measurement was independently performed by at least 3 authors (among GN, BB, AG, EA, LP) and medians used for the analysis. “Pmusc, Pmusc,lsf, Pmusc,index, PTP and PTPlsf were calculated on all breaths in which the inspiratory occlusion maneuver was performed and that were of sufficient quality to be scored by all the 3 independent scorers”.
2.6 Outcomes
The primary outcome was the agreement between Pmusc calculated through the Pes method (deemed as the gold standard), Pmusc,lsf and Pmusc,index. The secondary outcome was the accuracy of Pmusc,lsf and Pmusc,index to detect near-passive patients (defined as Pmusc ≤ 1 cmH2O, see above).
2.7 Statistical analysis
Data are shown as mean ± standard deviation, median (1st- 3rd quartile) or frequency (percentage).
In order to detect differences among Pmusc, Pmusc,lsf, and Pmusc,index, we calculated a sample size of 18 patients obtained considering a size effect 0.4 on the primary endpoint, alpha error 0.05, power 0.8, T tests family and fixed model single regression coefficient as statistical test (G*Power 3.1.9.2, Heinrich-Heine-Universität, Düsseldorf, Germany [17].
Linear mixed effects models were used to compare variables (PS level as fixed effect, patients as random effect). The methods of Pmusc measurement (esophageal pressure, least square fitting, end-inspiratory pause) and their relationships were similarly analyzed with linear mixed effects models (method and PS levels as fixed effects, patients as random effect). Comparison among groups were analyzed with the Tukey test.
Bias and agreement were assessed by Bland–Altman analysis for repeated measures [18]. The accuracy of Pmusc,lsf and Pmusc,index to detect near-passive patients was assessed by the area under the receiver operating characteristics (ROC) curve. The areas under ROC curves were compared with the DeLong test. We also calculated the positive and negative predictive values and the confidence intervals at 95% level (95% CI), using the values that maximized the sum of sensitivity and specificity as cut-offs.
A p value lower than 0.05 was considered significant. Statistical analyses were performed with R (R Core Team, 2018. R Foundation for Statistical Computing, Vienna, Austria) with packages “lme4” (version 1.1–17) and “multcomp” (version 1.4–8).
3 Results
We studied 18 consecutive patients whose baseline characteristics are shown in Table 1. Breathing pattern, respiratory drive and inspiratory effort data are shown in Table 2. By increasing the PS level, Pmusc and respiratory rate decreased and tidal volume increased.
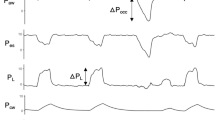
At all the three PSV levels, Pmusc,lsf was not different from Pmusc (p = 0.96), whereas Pmusc,index was significantly lower than Pmusc (p < 0.001) (Fig. 2, top panel). PTPlsf was not different from PTP (p = 0.92, Fig. 2, bottom panel). The relationship between Pmusc and Pmusc,lsf and between Pmusc and Pmusc,index were weak although statistically significant (r2 = 0.34, p < 0.001 and r2 = 0.19, p < 0.001 respectively).
Measured and estimated inspiratory effort at PSmin, PSbase and Psmax. PSmin: minimal pressure support; PSbase: baseline pressure support; PSmax: maximal pressure support (see “Methods” section for explanation). Top: Pmusc: inspiratory swing measured between elastic recoil pressure of chest wall and esophageal pressure; Pmusc,lsf: Pmusc estimated with least square fitting method; Pmusc,index: Pmusc estimated with end-inspiratory occlusion method. Bottom: PTP: Pressure–time product; PTPlsf: PTP estimated with the least square fitting method
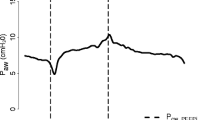
Figure 3 shows the Bland–Altman plots assessing the agreement between Pmusc and Pmusc,lsf (left side) and Pmusc and Pmusc,index (right side). The bias between Pmusc and Pmusc,lsf was zero, whereas the bias between Pmusc and Pmusc,index was 6 cmH2O. Both plots show similar limits of agreement of ± 12 cmH2O across bias.
Title: Bland–Altman plot for measured and calculated inspiratory effort. PSmin minimal pressure support, PSbase baseline pressure support, PSmax maximal pressure support, Pmusc inspiratory swing of the pressure generated by respiratory muscles measured on esophageal pressure, Pmusc,lsf inspiratory swing of the pressure generated by respiratory muscles calculated with least square fitting method, Pmusc,index inspiratory pressure generated by respiratory muscles estimated with end-inspiratory occlusion method. Continuous line: bias; dashed line: 95% limits of agreement
There was a weak relationship between PTP and PTPlsf (r2 = 0.27, p < 0.001), with a bias of -7 cmH2O·s·min−1 (95% limits of agreement: from—192 to 178 cmH2O·s·min−1).
Pmusc,lsf and Pmusc,index were moderately accurate to identify a near-passive patients, with areas under ROC curve of 0.73 (95% CI 0.65–0.81) and 0.87 (95% CI 0.8–0.94), respectively (p = 0.01). Both Pmusc,lsf ≤ 4cmH2O and Pmusc,index ≤ 1cmH2O had very low positive predictive value [0.33 (95% CI 0.23–0.45) and 0.22 (95% CI 0.15–0.31), respectively)] but excellent negative predictive value [0.98 (95% CI 0.94–1) and 0.96 (95% CI 0.91–0.99), respectively)]. The sensitivity and specificity were as follow [0.89 (95% CI 0.72–0.98) and 0.73 (95% CI 0.66–0.79)] for Pmusc,lsf, respectively, and [0.86 (95% CI 0.67–0.96) and 0.55 (95% CI 0.47–0.62)] for Pmusc,index, respectively. In practical terms, one can very likely exclude that a patient is near-passive during PSV when Pmusc,lsf > 4cmH2O or Pmusc,index > 1 cmH2O.
4 Discussion
Our investigation showed that the pressure developed by inspiratory muscles cannot be accurately estimated by the least square fitting or end-inspiratory occlusion as the limits of agreement between measured and estimated inspiratory effort were far above the signal size. However, both non-invasive methods of Pmusc estimation tested in the present study were able to exclude that a patient was near-passive during PSV.
The least square fitting method has been proposed to estimate respiratory mechanics [14] and inspiratory effort during PSV more than 20 years ago [3] and is still in use in some mechanical ventilators. Despite average values of Pmusc and Pmusc,lsf were similar at different PSV levels, we found that the individual estimation of the inspiratory effort by Pmusc,lsf was largely inaccurate. Theoretically there are two main factors that could impair the accuracy of the least square fitting method: flow limitation [19, 20] and high respiratory drive [14]. We excluded flow-limited patients from the study using the manual compression of the abdomen method, that has been shown to detect flow limitation in resting supine and seated subjects, during exercise and mechanical ventilation [7,8,9]. Regarding the respiratory drive, we must point out that P0.1 averaged 1 cmH2O during PSmax (the level at which respiratory system elastance and resistance were calculated with the least square fitting method), a respiratory drive that ensures an effective near-relaxation during PSV [14]. Additionally, by re-assessing the agreement between Pmusc and Pmusc,lsf using only the data of the 11 patients with P0.1 equal or lower than 1 cmH2O, the results shown in Fig. 3 were substantially confirmed (bias 0 cmH2O, 95% limits of agreement from − 10 to 10 cmH2O). For these reasons, we believe that the failure of least square fitting to estimate Pmusc cannot be explained by high respiratory drive. Iotti and coworkers previously showed that the relationship between Pmusc and Pmusc,lsf decreases by increasing the PS [3]. We performed a supplemental analysis by testing the relationship between Pmusc and Pmusc,lsf at PSmax and, confirming the Iotti data, it was not significant (r2 = 0.002, p = 0.59). In summary, despite its solid theoretical basis, our data suggest that Pmusc estimation with the least square fitting is not accurate during PSV.
The end-inspiratory occlusion is a “static” method, that assumes that all the applied pressure (i.e. Paw + Pmusc) is spent to generate the volume and overcome PEEPtot, and that the applied pressure spent to generate the inspiratory airflow is negligible [4]. Accordingly, the Pmusc assessed with the end-inspiratory occlusion method does not include the resistive component of work of breathing and Pmusc at end inspiration is usually lower than the maximum inspiratory deflection of Pmusc during inspiration, as shown in Fig. 1 [4]. Our data confirm the systematic underestimation of Pmusc by Pmusc,index, with an average bias of 6 cmH2O (Fig. 3). The end-inspiratory occlusion method can be performed with multiple occlusions, each at a different inspiratory volume in the tidal volume range [21, 22]. This alternative approach, requiring an external software to control the mechanical ventilator and the assessment of residual Pres at end inspiration, was able to overcome the Pmusc underestimation and to reduce the 95% CI of agreement between Pmusc and Pmusc,index to − 5 to 5 cmH2O [22]. Therefore, we cannot exclude that a more complex application of end-inspiratory occlusion method could yield better results.
Pmusc,index and Pmusc,lsf may prove to maintain a sound clinical usefulness despite their poor agreement with Pmusc. Diaphragm weakness is present in a high percentage of critically ill patients and is associated with increased morbidity and mortality. Indeed, a well recognized cause of diaphragm dysfunction is disuse secondary to ventilator-induced diaphragm inactivity [1] and preserving diaphragmatic contractions during mechanical ventilation attenuates the force loss induced by inactivity [23,24,25]. We found that both the Pmusc,index and Pmusc,lsf were able to exclude a near-passive state during ventilation. Thus, Pmusc,index and Pmusc,lsf may prove clinically useful if they are used to screen for patient’s passivity during PSV. Since we found that the near-passive condition is very unlikely whenever Pmusc,lsf > 4 cmH2O or Pmusc,index > 1 cmH2O, patients with Pmusc,lsf below 4 cmH2O or Pmusc,index below 1 cmH2O should be carefully assessed to exclude absent or minimal activation of inspiratory muscles, a condition often associated with auto-cycling. End-inspiratory occlusion is simpler and easier to perform at the bedside compared with the least square fitting method. Unfortunately some mechanical ventilators do not allow to perform end-inspiratory occlusions during PSV, precluding the assessment of Pplat,aw and hence to infer relevant information about patient’s inspiratory effort and driving pressure [26].
One potential limitation of our study is the choice to explore the entire clinical range of the inspiratory support. This could have negatively affected the agreement between Pmusc and its non-invasive estimates; however, we considered this pragmatic design a strength rather than a limitation, as it sought to validate the least square fitting and the end-inspiratory occlusion methods in a wide range of clinical circumstances. We cannot exclude, however, that different PSV levels than the ones tested in our study would have improved the performance of the non-invasive Pmusc estimation method.
5 Conclusions
In conclusion, our investigation showed that the inspiratory effort during PSV could not be accurately estimated by the least square fitting or end-inspiratory occlusion method. These non-invasive approaches, however, proved valid to screen patients at risk for absent or minimal respiratory muscles activation to prevent the ventilator-induced diaphragmatic dysfunction.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- Ecw :
-
Chest wall elastance
- Ers :
-
Elastance of the respiratory system
- P0 :
-
Basal pressure
- P0.1 :
-
Airway occlusion pressure at 100 ms
- Pappl :
-
Pressure applied to the respiratory system
- Paw :
-
Airway pressure
- Pcw :
-
Relaxation pressure of the chest wall
- Pel :
-
Elastic pressure
- Pexp,es :
-
End-expiratory plateau esophageal pressure
- Pmusc :
-
Pressure developed by respiratory muscles during inspiration
- Pmusc,index :
-
Pmusc estimated by the end-inspiration occlusion method
- Pmusc,lsf :
-
Pmusc estimated by the least square fitting method
- Pplat,aw :
-
End-inspiratory plateau airway pressure
- Pplat,es :
-
End-inspiratory plateau esophageal pressure
- Pres :
-
Resistive pressure
- PEEP:
-
Positive end-expiratory pressure
- PEEPtot :
-
Total PEEP
- PS:
-
Pressure support
- PSbase :
-
Baseline PS
- PSmax :
-
Maximal PS
- PSmin :
-
Minimal PS
- PSV:
-
Pressure support ventilation
- PTP:
-
Pressure–time product
- Rrs :
-
Resistance of the respiratory system
- ROC:
-
Receiver operating characteristics
- V:
-
Volume
- V′:
-
Flow
References
Supinski GS, Morris PE, Dhar S, et al. Diaphragm dysfunction in critical illness. Chest. 2018;153:1040–51.
American Thoracic Society/European Respiratory Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166:518–624.
Iotti GA, Braschi A, Brunner JX, et al. Noninvasive evaluation of instantaneous total mechanical activity of the respiratory muscles during pressure support ventilation. Chest. 1995;108:208–15.
Foti G, Cereda M, Banfi G, et al. End-inspiratory airway occlusion: a method to assess the pressure developed by inspiratory muscles in patients with acute lung injury undergoing pressure support. Am J Respir Crit Care Med. 1997;156:1210–6.
Otis AB, Fenn WO, Rahn H. Mechanics of breathing in man. J Appl Physiol. 1950;2:592–607.
Boles J-M, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29:1033–56.
Ninane V, Leduc D, Kafi SA, et al. Detection of expiratory flow limitation by manual compression of the abdominal wall. Am J Respir Crit Care Med. 2001;163:1326–30.
Abdel Kafi S, Serste T, Leduc D, et al. Expiratory flow limitation during exercise in COPD: detection by manual compression of the abdominal wall. Eur Respir J. 2002;19:919–27.
Lemyze M, Favory R, Alves I, et al. Manual compression of the abdomen to assess expiratory flow limitation during mechanical ventilation. J Crit Care. 2012;27:37–44.
Baydur A, Behrakis PK, Zin WA, et al. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982;126:788–91.
Mauri T, Yoshida T, Bellani G, et al. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016;42:1360–73.
Mojoli F, Iotti GA, Torriglia F, et al. In vivo calibration of esophageal pressure in the mechanically ventilated patient makes measurements reliable. Crit Care. 2016;20:98.
Conti G, Antonelli M, Arzano S, et al. Equipment review. Measurement of occlusion pressures in critically ill patients. Crit Care. 1997;1:89.
Iotti GA, Braschi A, Brunner JX, et al. Respiratory mechanics by least squares fitting in mechanically ventilated patients: applications during paralysis and during pressure support ventilation. Intensive Care Med. 1996;21:406–13.
Berger KI, Sorkin IB, Norman RG, et al. Mechanism of relief of tachypnea during pressure support ventilation. Chest. 1996;109:1320–7.
Rossi A, Gottfried SB, Zocchi L, et al. Measurement of static compliance of the total respiratory system in patients with acute respiratory failure during mechanical ventilation. Am Rev Respir Dis. 1985;131:672–7.
Faul F, Erdfelder E, Lang A-G, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–82.
Peslin R, da Silva J, Chabot F, et al. Respiratory mechanics studied by multiple linear regression in unsedated ventilated patients. Eur Respir J. 1992;5:871–8.
Volta CA, Marangoni E, Alvisi V, et al. Respiratory mechanics by least squares fitting in mechanically ventilated patients: application on flow-limited COPD patients. Intensive Care Med. 2002;28:48–52.
Pesenti A, Pelosi P, Foti G, et al. An interrupter technique for measuring respiratory mechanics and the pressure generated by respiratory muscles during partial ventilatory support. Chest. 1992;102:918–23.
Bellani G, Patroniti N, Weismann D, et al. Measurement of pressure–time product during spontaneous assisted breathing by rapid interrupter technique. Anesthesiology. 2007;106:484–90.
Sassoon CSH, Zhu E, Caiozzo VJ. Assist–control mechanical ventilation attenuates ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med. 2004;170:626–32.
Futier E, Constantin J-M, Combaret L, et al. Pressure support ventilation attenuates ventilator-induced protein modifications in the diaphragm. Crit Care. 2008;12:R116.
Dimussi R, Spadaro S, Mirabella L, et al. Impact of prolonged assisted ventilation on diaphragmatic efficiency: NAVA versus PSV. Crit Care. 2015;20:1.
Bellani G, Grassi A, Sosio S, et al. Plateau and driving pressure in the presence of spontaneous breathing. Intensive Care Med. 2019;45:97–8.
Funding
The study was supported by the departemental funding of the Department of Intensive Care and Anesthesiology, Fondazione Poliambulanza, Brescia, Italy.
Author information
Authors and Affiliations
Contributions
GN, AR and AB contributed to the conception and design of the study; GN, BB, AG, EA, LP, GC, VL contributed to the acquisition of data; GN and LP contributed to the analysis of the data; GN, LP and Salvatore Grasso drafted the manuscript; Nicola Latronico and Massimo Antonelli revised the manuscript; all authors contributed to the interpretation of the data, critically revised the manuscript and approved the final version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The protocol was approved by the local ethical committee (Comitato Etico Provinciale di Brescia, approval number NP2245).
Informed consent
Written informed consent was obtained from the patient. In case of altered consciousness, the Ethics Committees waived the requirement for consent, as in Italy relatives are not regarded as legal representatives of the patient in the absence of a formal designation. Written informed consent was requested from all surviving patients as soon as they regained their mental competency.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Natalini, G., Buizza, B., Granato, A. et al. Non-invasive assessment of respiratory muscle activity during pressure support ventilation: accuracy of end-inspiration occlusion and least square fitting methods. J Clin Monit Comput 35, 913–921 (2021). https://doi.org/10.1007/s10877-020-00552-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00552-5